Introduction
Heart failure (HF), one of the most common reasons
for hospitalization in the US Medicare population, remains a major
threat to public health (1). It
affected more than 5 million Americans in 2010 (2). Furthermore, it causes substantial
mortality and morbidity. A previous study indicated that
approximately 20% of people in the world will have HF at some point
in their lifetime (3). Although
diagnostic intensity and treatment is improving, prognosis is still
poor (4). In addition, the rising
incidence of HF is a cause for concern and there are few effective
preventive measures against it (5). Therefore, feasible preventive
measures of HF are of considerable clinical and public health
importance (6).
Potential correlations between HF and different risk
factors have been suggested (7).
Smoking, age and diabetes are well-established risk factors of HF
(8). Moreover, the associations
between HF risk and exogenous factors including diet and lifestyle
characteristics have been reported in numerous epidemiology studies
(9,10). Certain studies report that high
intakes of several specific types of fruits, vegetables and
nutrients may decrease the risk of HF (11).
It is generally accepted that fish has excellent
health benefits for humans (12).
Fish is rich in the long-chain marine ω-3 polyunsaturated fatty
acids (PUFAs), eicosapentaenoic acid (EPA) and docosahexaenoic acid
(DHA), which may lower the cardiovascular disease risk by
decreasing inflammation, oxidative stress and blood pressure, as
well as improving cardiac and endothelial function (13,14).
The relationship between fish intake and HF has received much
attention since 1980. A few prospective cohort studies examined the
potential correlation between fish intake and HF risk (15–19);
however, their findings were controversial. Fish is one of the most
common foods in the world. There is great interest in quantifying
its independent association with HF incidence. To date, no
quantitative assessment concerning the association has been
conducted.
In the present study, we conducted the first
meta-analysis to clarify the potential association between fish
intake and risk of HF on the basis of findings from all published
prospective cohort studies. Our aim was to estimate the relative
risk of high intake versus low intake of fish. We also quantified
the dose-response relationship between fish intake and HF risk.
Materials and methods
Literature search strategy
We conducted the present meta-analysis in accordance
with Meta-analysis of Observational Studies in Epidemiology (MOOSE)
guidelines (20). We performed a
PubMed database search throughout January 2012 for relevant studies
that reported the association between fish intake and risk of HF.
The primary search included the following terms, diet, seafood,
fish, heart failure or HF. The search focused on human studies,
without a restriction on language. In addition, we reviewed the
reference lists of all included articles to obtain relevant
studies.
Inclusion and exclusion criteria
Studies were included in the present meta-analysis
if they met the following criteria; i) they should be prospective
cohort studies in humans; ii) the primary outcome has been clearly
defined as HF; iii) the study has examined the association between
fish intake and HF risk from 1980 to January 2012; iv) the study
has reported point estimates [i.e. relative risks (RR)s or odds
ratios (ORs)] and measures of variability [i.e. 95% confidence
intervals (CIs)] for the highest versus zero/lowest level of fish
intake, or the studies provided sufficient information to estimate
them. To avoid confusion, ‘fish’ in the present analysis included
‘fish’, ‘tuna fish’, ‘tuna and other fish’, ‘fried fish’ and
‘boiled fish’. A summary RR of fried or boiled fish would be
calculated if they were presented individually in more than two
studies. The exclusion criteria were i) duplicates; ii) no usable
data reported; iii) cross-sectional, case-control and ecological
analyses. We identified eligible articles for a full-text review
following an initial screening by title or abstract.
Data extraction
Two of the authors (L-N.H. and F.L.) independently
extracted the information using a standardized data collection form
from the selected studies. Any discrepancy was resolved by
repeating the study review and discussion. The following
information was recorded; name of the first author, year of
publication, study location, study duration, follow-up time, number
of cases, total number of participants, age range of participants,
person-years of follow-up, number of exposed cases, categories of
fish intake, the amount of fish intake for each category, RR or OR,
the corresponding 95% CIs and adjusted confounding factors in the
analysis. If one study reported multiple data sets, we used the
results from the main multivariable model that included the most
adjusted confounders.
We assessed the quality of each study by monitoring
crucial components of the eligible studies; clear definition of
participant characteristics, clear examination of exposure and
outcome, study duration, sufficient duration of follow-up,
person-years of follow-up, no selective loss during follow-up and
control for potential confounding factors. If a study did not
clearly mention one of these key points, we considered that it had
not been performed, therefore it is likely that the reported
characteristics were underestimated.
Statistical analyses
We used the summary relative risk estimate (SRRE)
for the highest compared with the lowest category of fish
consumption. It should be noted that the lowest category included
individuals who did not consume any fish. We used both the fixed-
and random-effects method to estimate the association of HF and
risk ratio of the highest category of fish consumption versus the
lowest category. Statistical heterogeneity across studies was
examined using the Q statistic (significant at P<0.10). The
I2 statistic (values of 75, 50 and 25% were considered
to represent high, medium and low heterogeneity, respectively) was
also calculated to quantitatively measure the inconsistency across
studies (21). Forest plots were
constructed to assess the association between fish intake and HF
risk.
Stratified analyses were conducted to investigate
potential sources of heterogeneity, including geographical region,
gender and cooking method of fish. In addition, we performed a
sensitivity analysis to evaluate the influence of an individual
study on the overall result. Each study was omitted in turn to
assess the robustness of the results. A dose-response analysis was
conducted based on the category data of fish intake, number of
cases, person-years and logarithm of SRRE and its corresponding
standard error. The eligible studies should provide sufficient
information across at least three categories of exposure (22). Among the studies, we assigned a
median of fish intake for each category. For the open-ended upper
category of consumption, the amplitude was assumed the same as the
previous one.
To examine whether publication bias affected the
validity of the summary estimates, we applied Egger’s test and
Begg’s method to evaluate the possible bias combined with a visual
inspection of the funnel plot. Begg’s method is used to test the
rank correction between the standardized effect size and the
variances based on Kendall’s method (23). Egger’s test is a linear regression
approach to measure the estimate divided by its standard error
against the reciprocal of the standard error of the estimate
(24). In other words, Egger’s
method regresses the normalized effect size against precision. All
statistical analyses were performed with STATA Statistical
Software, version 11.0. P<0.05 was considered to indicate a
statistically sigificant result, except where specifically
noted.
Results
Literature search
Fig. 1 shows a flow
chart of our selection process. A total of 1411 records were
retrieved via a PubMed search. Of these, 1224 articles were
excluded following an initial screen of abstracts and titles.
Subsequently, 156 articles were excluded since they were review
articles, did not have relevant exposure or no incidence of HF was
identified. We identified 31 articles by full text review which
evaluated the correlation between fish consumption and HF risk.
Among the excluded 26 articles, one study was excluded as its
participants overlapped with another study (25), a different study was not included
due to the reported association with regard to fish intake and
mortality from HF (26). The
remaining 24 studies were excluded due to their effect sizes and
the corresponding 95% confidence intervals had not been provided or
could not be calculated due to insufficient information. Finally,
seven data sets from five independent prospective cohort studies
were included in our analysis. These studies were published between
1980 and January 2012.
Study characteristics
The characteristics of the five included studies are
listed in Table I. Of the five
studies, two studies were conducted in the US (18,19),
one in Sweden (16), one in The
Netherlands (17) and one in
nationwide clinical centers (15).
The period of follow-up ranged from 9 to 13.3 years. Studies in our
analysis used a Food Frequency Questionnaire (FFQ) based on
self-report or interviewer-administered questionnaires to ascertain
dietary information relating to fish intake, despite food items
differing in the questionnaire across studies. In summary, five
studies comprising 5,273 cases and 144,917 participants were
included in our analysis.
 | Table ICharacteristics of the studies that
analyzed fish consumption and heart failure. |
Table I
Characteristics of the studies that
analyzed fish consumption and heart failure.
| First author, year
(ref.) | Study location | Casesa/subjects | Follow-up
(years)/period | Items | Analytical comparison
(high vs. low intake) | RR (95% CI)/Trend
P-value | Adjustments |
|---|
| Belin RJ, 2011
(15) | USA | 1,858/84,493 | 10.0/1998–2008 | Baked/broiled
fish | ≥5 times/week vs.
<1 time/month | 0.70 (0.51–0.95)
0.022 | Age, smoking, BMI,
ethnicity, education, physical activity, alcohol, hypertension,
diabetes, atrial fibrillation, MI/coronary artery bypass
graft/percutaneous transluminal coronary angioplasty,
time-dependent MI, fiber, fruit/vegetable servings, saturated fat
intake (%), DHA EPA (%), ALA (%), linoleic acid (%), fried food
servings and sodium intake (mg) |
| | | | Fried fish | ≥1 time/week vs.
<1 time/month | 1.48 (1.19–1.84)
0.005 |
| Levitan EB, 2010
(16) | Swedish | 651/36,234 | 9.0/1998–2006 | Fish | ≥3 servings per week
vs. 0 | 0.91 (0.59–1.40)
0.049 | Age, smoking, BMI,
total energy, education, physical activity, living alone,
postmenopausal hormone use, alcohol intake, fiber intake, sodium
intake, intake of red or processed meat, family history of
myocardial infarction before 60 years, self-reported history of
hypertension and high cholesterol |
| Dijkstra SC, 2009
(17) | The Netherlands | 669/5,299 | 11.4/1990–2002 | Fish | ≥20 g/day vs. 0 | 0.96 (0.78–1.18)
0.39 | Age, gender, smoking,
BMI, energy, education, intake of alcohol, total fat, saturated
fat, trans-fat and meat |
| Nettleton JA, 2008
(18) | USA | 1,140/14,153 | 13.3/1987–1998 | Fish | Yes vs. No | 0.99 (0.81–1.22)
NR | Age, gender,
smoking, energy intake, race, education level, physical activity
level, drinking and prevalent disease status |
| Mozaffarian D, 2005
(19) | USA | 955/4,738 | 12/1989–2002 | Not fried fish | ≥5 times/week vs.
<1 time/month | 0.68 (0.45–1.03)
0.009 | Age, gender,
smoking, BMI, energy intake, race, enrollment site, education,
diabetes, prevalent coronary heart disease, stroke/transient
ischemic attack, fried fish or tuna/other fish intake, leisure-time
physical activity, saturated fat, fruits, vegetables and alcohol
intakes |
| | | | Fried fish | 1–2 times/week vs.
<1 time/month | 1.35 (1.12–1.62)
0.005 |
Fish intake and HF risk
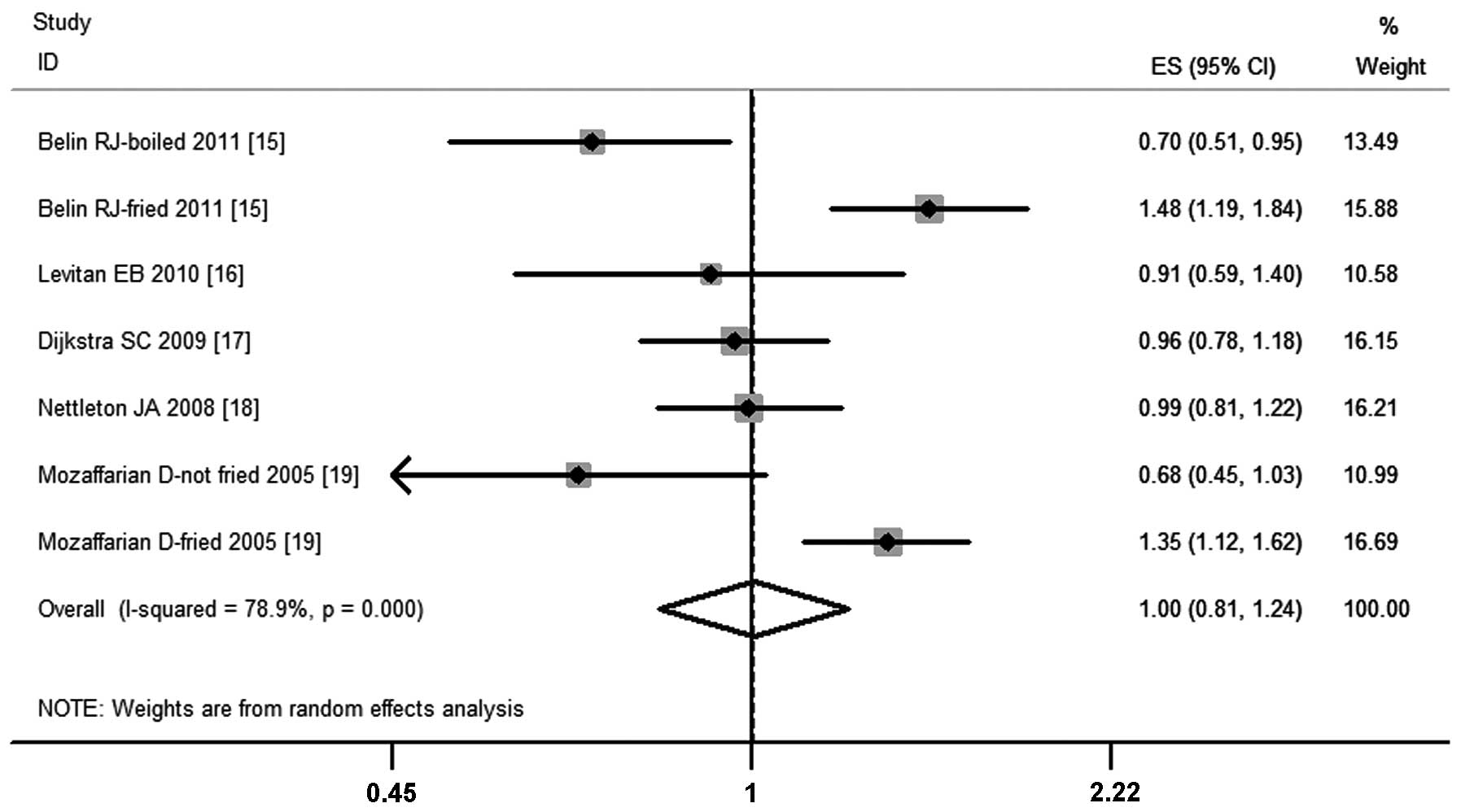
Fig. 2 shows the
pooled results from combing effect sizes for HF using the
random-effects model. Overall, we found no significant association
between fish intake and HF risk (SRRE=1.00; 95% CI, 0.81–1.24).
Substantial heterogeneity was detected across studies (P-value for
heterogeneity <0.0001, I2=78.9%; Fig. 2).
Other correlations
When the studies were stratified by geographical
region, no significant association was observed [USA (18,19):
SRRE=1.01; 95% CI, 0.72–1.41; P-value for heterogeneity=0.004;
I2=81.7%; Europe (16,17):
SRRE=0.95; 95% CI, 0.79–1.15; P-value for heterogeneity=0.827;
I2= 0%]. Notably, there was no variability across the
studies conducted in Europe (P-value for heterogeneity= 0.827;
I2= 0.0%) compared to the studies conducted in the US
(P-value for heterogeneity=0.004; I2=81.7%). Two studies
had only female participants (15,16).
The SRRE of these two studies was 0.99 (95% CI, 0.60–1.65; P-value
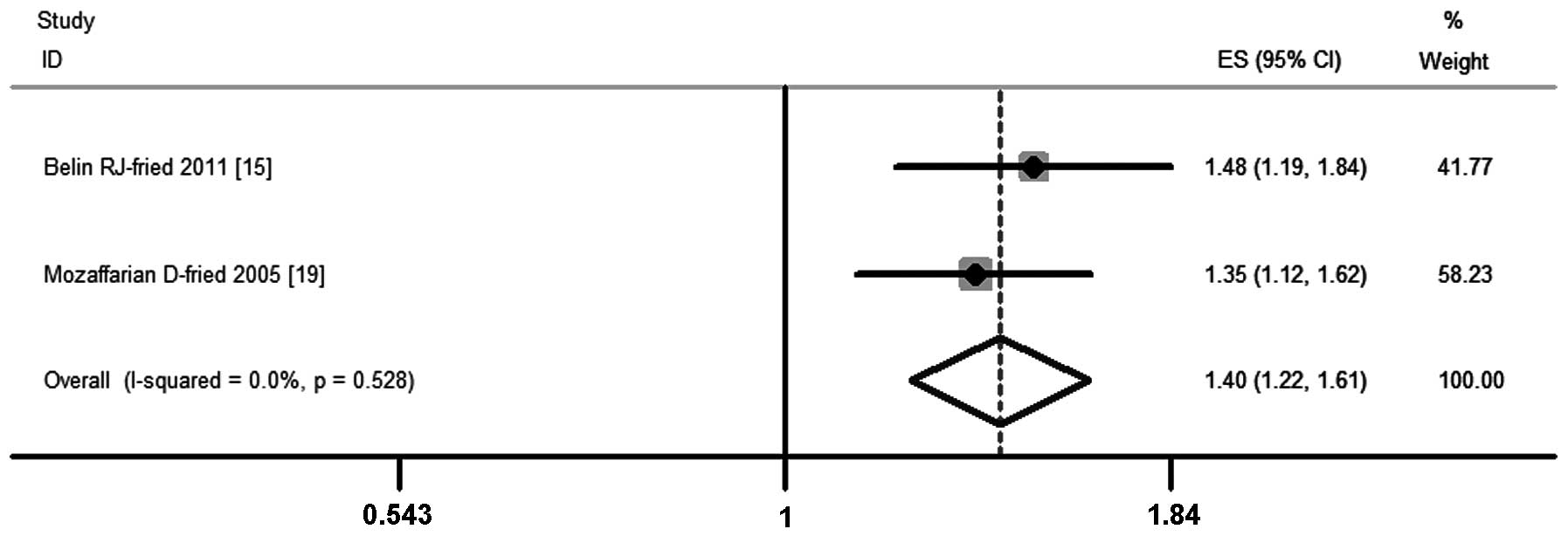
for heterogeneity<0.0001; I2=87.5%). In the cooking
method subgroups we observed a significant positive association
between fried fish consumption and HF (15,19).
The risk of HF markedly increased by 40% on the basis of
comparisons between the highest and lowest quartiles of fish intake
(SRRE=1.40; 95% CI, 1.22–1.61), without any evidence of
heterogeneity (P-value for heterogeneity= 0.528; I2=0%;
Fig. 3).
Sensitivity testing and publication
bias
Further sensitivity testing via the exclusion of a
single study at a time suggested that no single study influenced
the overall results in our meta-analysis, with a narrow range from
0.93 (95% CI, 0.82–1.03; P-value for heterogeneity= 0.001) to 1.05
(95% CI, 0.95–1.15; P-value for heterogeneity=0.001).
Visual inspection of the funnel plot (not shown) did
not suggest substantial asymmetry. There was no statistical
evidence of publication bias based on the Begg’s rank correlation
(P=0.548) and the Egger’s linear test (P=0.126).
HR and fried fish
Dose-response analysis of two studies on fried fish
consumption provide sufficient consistent evidence that the
incidence of HF was elevated when fried fish consumption increased.
Each increment of six fried fish per month corresponded to a 37%
increase of HF rate (RR=1.37; 95% CI, 1.20–1.56). This was
consistent with our combined results on fried fish consumption. We
did not conduct the dose-response analysis of studies on overall
fish intake as there was no connection to the risk of HF in our
analysis.
Discussion
The benefits of fish consumption are thought to be
largely attributable to the antiarrhythmic activity of abundant
PUFAs in fish (12–14). Epidemiological evidence suggests
that the high intake of fish may reduce risks of stroke and
coronary heart disease (CHD) (27,28).
This raises great interest in whether fish intake has any
relationship with HF, a type of cardiovascular disease.
Therefore, we conducted the first meta-analysis for
clarification of the association between fish intake and HF risk.
Five prospective cohort studies comprising 144,917 participants
were included in our analysis. The combined results suggested no
correlation between fish intake and HF incidence. The findings were
similar for subgroups according to geographical region or gender.
Interestingly, we found that a high level of fried fish consumption
was associated with a 40% increased risk of HF.
Heterogeneity is a major concern in meta-analyses. A
marked heterogeneity was observed across the included studies. This
may be caused by variability among the study populations, follow-up
period, analytical methodology, dietary assessment method and
adjustment for confounding factors. Based on subgroups according to
geographical region, gender, method of fish cooking, little
heterogeneity was observed among studies conducted in Europe and
studies that assessed fried fish individually. We were not able to
analyze other subgroups due to the limited data. However, the
results of sensitivity analyses were similar and robust, indicating
that no single study considerably influenced the overall risk
estimate between fish intake and HF. In addition, we observed no
evidence of publication bias in our meta-analysis based on Egger’s
test and Begg’s rank correction.
Our results compare favorably with the majority of
studies included in our analysis, where it was reported that
consuming fish was not associated with HF risk, whereas consumption
of fried fish was associated with a 40% higher risk of HF.
Dose-response analysis of fried fish consumption suggested that a
37% increased risk of HF was caused by an incremental increase of
an average of six fried fish per month.
The underlying mechanism involved in the association
between fried fish consumption and HF is uncertain. One possible
cause is that the net effect of benefit versus risk of fried fish
consumption may be detrimental (29). Although the method of frying does
not decrease the absolute n-3 fatty acid level, frying adds other
fatty acids from the frying oil and the procedure of cooking at
high temperatures may add oxidation products, partially
hydrogenated oils and trans-fatty acids (30–32).
These products may cause the HF risk to increase. In addition, the
association between fried fish intake and HF risk was partly
related to other higher risk clinical and lifestyle factors. The
higher fried fish consumption was markedly correlated with a lower
fiber and higher fruit/vegetable intake (15,19).
A higher fried fish consumption could also cause a higher
prevalence of diabetes, atrial fibrillation, CAD, higher systolic
blood pressure, higher body mass index, higher prevalence of
smoking and higher calorie intake (15). Therefore, these associated risk
factors may contribute to HF. Higher blood pressure, vascular
resistance and cardiac wall motion abnormalities may be the
potential physiological basis by which fried fish intake affects
the risk of HF (33).
Notably, our study has several key strengths. This
is the first meta-analysis to quantitatively assess the
relationship between fish intake and HF. The analysis was based on
five well-established prospective cohorts which had minimized
recall and selection biases. The studies had large sample sizes and
long term follow-up periods that enhanced the statistical power to
estimate the overall association between fish intake and HF risk.
Moreover, in order to control the bias, the included studies were
adjusted for a wide range of potential confounding variables. In
addition, our pooled analysis of five studies involving 144,917
participants was able to detect a more stable association and
provide a more reliable estimation.
There were a number of limitations to our current
meta-analysis when interpreting the results. First, although not
suggested by the Begg’s rank correlation and the Egger’s linear
test, potential bias may be involved considering that the tests for
bias were likely to be underpowered. However, our sensitivity test
showed the findings were robust. Second, substantial heterogeneity
was observed among the studies, although we were able to reveal
that geographic region is a major source of heterogeneity via
subgroup analyses. Third, residual confounders always raise a major
concern in the epidemiology studies. Although most studies included
in our analysis had performed adjustments for a wide range of
dietary and lifestyle variables, we could not exempt the
possibility that other uncontrolled or unmeasured confounding
factors play roles in the summary associations. Fourth, all the
included studies in our analysis were prospective cohort studies.
However, differences among follow-up period, dietary assessment
method and measurement of HF end point, may hinder an estimate of
the true effects of fish or fried fish consumption on HF risk. An
additional limitation is that we were unable to explore potential
differences of associations according to classification of HF. It
remains unclear if findings may vary by subtype.
In summary, it is generally accepted that there is a
great benefit of fish intake. Fish contain numerous essential
nutrients which benefit healthy living. Therefore, fish is
generally considered a healthy diet choice. However, our
meta-analysis on the basis of 144,917 participants suggests no
significant association between fish intake and HF risk and
provides evidence that the incidence of HF might be significantly
increased by consuming a high level of fried fish. Due to limited
data, more studies are required to confirm the findings.
References
|
1.
|
Kozak LJ, DeFrances CJ and Hall MJ:
National hospital discharge survey: 2004 annual summary with
detailed diagnosis and procedure data. Vital Health Stat 13.
162:1–209. 2006.PubMed/NCBI
|
|
2.
|
Lloyd-Jones D, Adams RJ, Brown TM, et al
American Heart Association Statistics Committee and Stroke
Statistics Subcommittee: Executive summary: heart disease and
stroke statistics - 2010 update: a report from the American Heart
Association. Circulation. 121:948–954. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Lloyd-Jones DM, Larson MG, Leip EP, Beiser
A, D’Agostino RB, Kannel WB, Murabito JM, Vasan RS, Benjamin EJ and
Levy D; Framingham Heart Study: Lifetime risk for developing
congestive heart failure: the Framingham Heart Study. Circulation.
106:3068–3072. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Schocken DD: American Society for
Preventive Cardiology. Prev Cardiol. 11:127–128. 2008. View Article : Google Scholar
|
|
5.
|
Yancy CW: Heart failure in African
Americans. Am J Cardiol. 96:3i–12i. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Jhund PS, Macintyre K, Simpson CR, Lewsey
JD, Stewart S, Redpath A, Chalmers JW, Capewell S and McMurray JJ:
Long-term trends in first hospitalization for heart failure and
subsequent survival between 1986 and 2003: a population study of
5.1 million people. Circulation. 119:515–523. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Norton C, Georgiopoulou VV, Kalogeropoulos
AP and Butler J: Epidemiology and cost of advanced heart failure.
Prog Cardiovasc Dis. 54:78–85. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Magaña-Serrano JA, Almahmeed W, Gomez E,
Al-Shamiri M, Adgar D, Sosner P and Herpin D; I PREFER
Investigators: Prevalence of heart failure with preserved ejection
fraction in Latin American, Middle Eastern, and North African
Regions in the I PREFER study (Identification of Patients With
Heart Failure and PREserved Systolic Function: an epidemiological
regional study). Am J Cardiol. 108:1289–1296. 2011.
|
|
9.
|
Wang Y, Tuomilehto J, Jousilahti P,
Antikainen R, Mähönen M, Katzmarzyk PT and Hu G: Lifestyle factors
in relation to heart failure among Finnish men and women. Circ
Heart Fail. 4:607–612. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Cheng S and Vasan RS: Advances in the
epidemiology of heart failure and left ventricular remodeling.
Circulation. 124:e516–e519. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Djoussé L, Driver JA and Gaziano JM:
Relation between modifiable lifestyle factors and lifetime risk of
heart failure. JAMA. 302:394–400. 2009.PubMed/NCBI
|
|
12.
|
Mozaffarian D, Katan MB, Ascherio A,
Stampfer MJ and Willett WC: Trans fatty acids and cardiovascular
disease. N Engl J Med. 354:1601–1613. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Bays H: Clinical overview of Omacor: a
concentrated formulation of omega-3 polyunsaturated fatty acids. Am
J Cardiol. 98:71i–76i. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Mozaffarian D and Rimm EB: Fish intake,
contaminants, and human health: evaluating the risks and the
benefits. JAMA. 296:1885–1899. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Belin RJ, Greenland P, Martin L, Oberman
A, Tinker L, Robinson J, Larson J, Van Horn L and Lloyd-Jones D:
Fish intake and the risk of incident heart failure: the Women’s
Health Initiative. Circ Heart Fail. 4:404–413. 2011.
|
|
16.
|
Levitan EB, Wolk A and Mittleman MA: Fatty
fish, marine omega-3 fatty acids and incidence of heart failure.
Eur J Clin Nutr. 64:587–594. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Dijkstra SC, Brouwer IA, van Rooij FJ,
Hofman A, Witteman JC and Geleijnse JM: Intake of very long chain
n-3 fatty acids from fish and the incidence of heart failure: the
Rotterdam Study. Eur J Heart Fail. 11:922–928. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Nettleton JA, Steffen LM, Loehr LR,
Rosamond WD and Folsom AR: Incident heart failure is associated
with lower whole-grain intake and greater high-fat dairy and egg
intake in the Atherosclerosis Risk in Communities (ARIC) study. J
Am Diet Assoc. 108:1881–1887. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Mozaffarian D, Bryson CL, Lemaitre RN,
Burke GL and Siscovick DS: Fish intake and risk of incident heart
failure. J Am Coll Cardiol. 45:2015–2021. 2005. View Article : Google Scholar
|
|
20.
|
Stroup DF, Berlin JA, Morton SC, Olkin I,
Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA and Thacker
SB: Meta-analysis of observational studies in epidemiology: a
proposal for reporting. Meta analysis Of Observational Studies in
Epidemiology (MOOSE) group. JAMA. 283:2008–2012. 2000. View Article : Google Scholar
|
|
21.
|
Higgins JP and Thompson SG: Quantifying
heterogeneity in a meta-analysis. Stat Med. 21:1539–1558. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Orsini N, Bellocco R and Greenland S:
Generalized least squares for trend estimation of summarized
dose-response data. Stata J. 6:40–57. 2006.
|
|
23.
|
Egger M, Davey Smith G, Schneider M and
Minder C: Bias in meta-analysis detected by a simple, graphical
test. BMJ. 315:629–634. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Begg CB and Mazumdar M: Operating
characteristics of a rank correlation test for publication bias.
Biometrics. 50:1088–1101. 1994. View
Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Levitan EB, Wolk A and Mittleman MA: Fish
consumption, marine omega-3 fatty acids, and incidence of heart
failure: a population-based prospective study of middle-aged and
elderly men. Eur Heart J. 30:1495–1500. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Yamagishi K, Iso H, Date C, Fukui M, Wakai
K, Kikuchi S, Inaba Y, Tanabe N and Tamakoshi A; Japan
Collaborative Cohort Study for Evaluation of Cancer Risk Study
Group: Fish, omega-3 polyunsaturated fatty acids, and mortality
from cardiovascular diseases in a nationwide community-based cohort
of Japanese men and women the JACC (Japan Collaborative Cohort
Study for Evaluation of Cancer Risk) Study. J Am Coll Cardiol.
52:988–996. 2008. View Article : Google Scholar
|
|
27.
|
Bouzan C, Cohen JT, Connor WE,
Kris-Etherton PM, Gray GM, König A, Lawrence RS, Savitz DA and
Teutsch SM: A quantitative analysis of fish consumption and stroke
risk. Am J Prev Med. 29:347–352. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
König A, Bouzan C, Cohen JT, Connor WE,
Kris-Etherton PM, Gray GM, Lawrence RS, Savitz DA and Teutsch SM: A
quantitative analysis of fish consumption and coronary heart
disease mortality. Am J Prev Med. 29:335–346. 2005.PubMed/NCBI
|
|
29.
|
Wilson JF: Balancing the risks and
benefits of fish consumption. Ann Intern Med. 141:977–980. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
30.
|
Warner K: Impact of high-temperature food
processing on fats and oils. Adv Exp Med Biol. 459:67–77. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
31.
|
Aro T, Tahvonen R, Mattila T, Nurmi J,
Sivonen T and Kallio H: Effects of season and processing on oil
content and fatty acids of baltic herring (Clupea harengus
membras). J Agric Food Chem. 48:6085–6093. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
32.
|
Al-Saghir S, Thurner K, Wagner KH, Frisch
G, Luf W, Razzazi- Fazeli E and Elmadfa I: Effects of different
cooking procedures on lipid quality and cholesterol oxidation of
farmed salmon fish (Salmo salar). J Agric Food Chem.
52:5290–5296. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
33.
|
Mozaffarian D, Lemaitre RN, King IB, Song
X, Spiegelman D, Sacks FM, Rimm EB and Siscovick DS: Circulating
long-chain ω-3 fatty acids and incidence of congestive heart
failure in older adults: the cardiovascular health study: a cohort
study. Ann Intern Med. 155:160–170. 2011.
|