Introduction
Squamous cell carcinoma (SCC) accounts for 5–10% of
diagnosed cancers of unknown primary (CUP) site (1). As reported, the primary site is
detected in antemortem examinations in only 25% of patients
(2) and median survival is
predicted to be 6–9 months (3). A
limited number of studies have described retroperitoneal CUP with
primary site detected in the esophagus during follow-up, and even
fewer studies have observed long progression-free survival (PFS)
and overall survival (OS). In the present case study, we report a
59-year-old female patient with SCC presenting as large
retroperitoneal mass with primary site in the esophagus detected
subsequently. This patient was treated with chemotherapy, and had
PFS of 18 months and OS of 28 months. Of note, a search of the
literature using Medline, EMBASE and the Web of Science, until
August 2012, yielded no similar reports.
Case report
A 59-year-old female patient was referred to a
hospital with a 4-month history of persistent waist pain in August
2008. She was diagnosed with lumbar muscle strain. The patient
ingested traditional Chinese medicine. However, the pain became
more severe in the following three months and the patient was not
able to lie back without strong opioid analgesics and lost 7 kg
during this period of time. In November 2008, the patient was
admitted to a second hospital. Physical examinations revealed
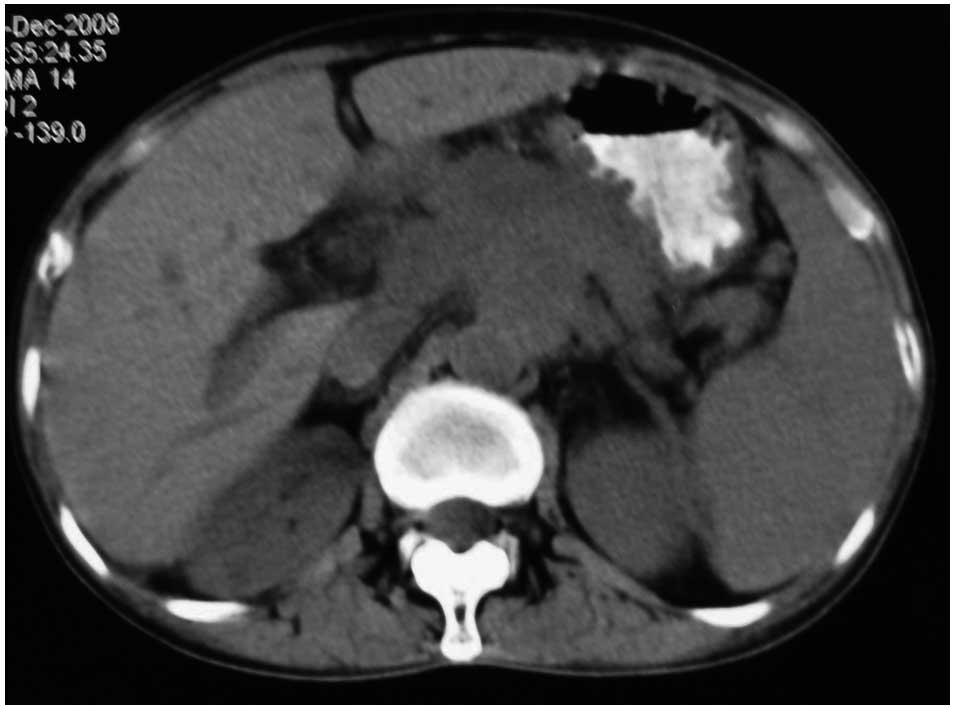
nothing abnormal and the abdominal computed tomography (CT) scan
showed that a large mass occupied the entire retroperitoneal cavity
(Fig. 1). Positron emission
tomography/computed tomography (PET/CT) showed a mass in the
retroperitoneal cave, which was considered as lymph nodes blending
together into a large mass, with an average standardized uptake
value (SUV) of 5.5. Due to the limited conditions, the patient did
not undergo biopsy and was diagnosed as having retroperitoneal
occupation.
For further diagnosis and therapy, the patient was
finally hospitalized at our Department on November 12th, 2008.
Physical examination showed a mild tenderness in the middle of the
upper abdomen. No other positive signs were found including
palpable inguinal or cervical lymph nodes. Blood tests were normal
other than an elevation of carcinoembryonic antigen (CEA) to 7.2
ng/ml (normal ≤5.0 ng/ml) and carbohydrate antigen-199 (CA199) to
88.8 U/ml (normal ≤35.0 U/ml). The abdominal CT showed a large mass
with no clear boundaries fixed to the retroperitoneal cavity and
enveloping the abdominal aorta as well as other vascular elements.
No other lesions were detected by gastro-esophageal endoscopy,
nasopharyngeal CT, chest CT or cervix and urology-gynecologic
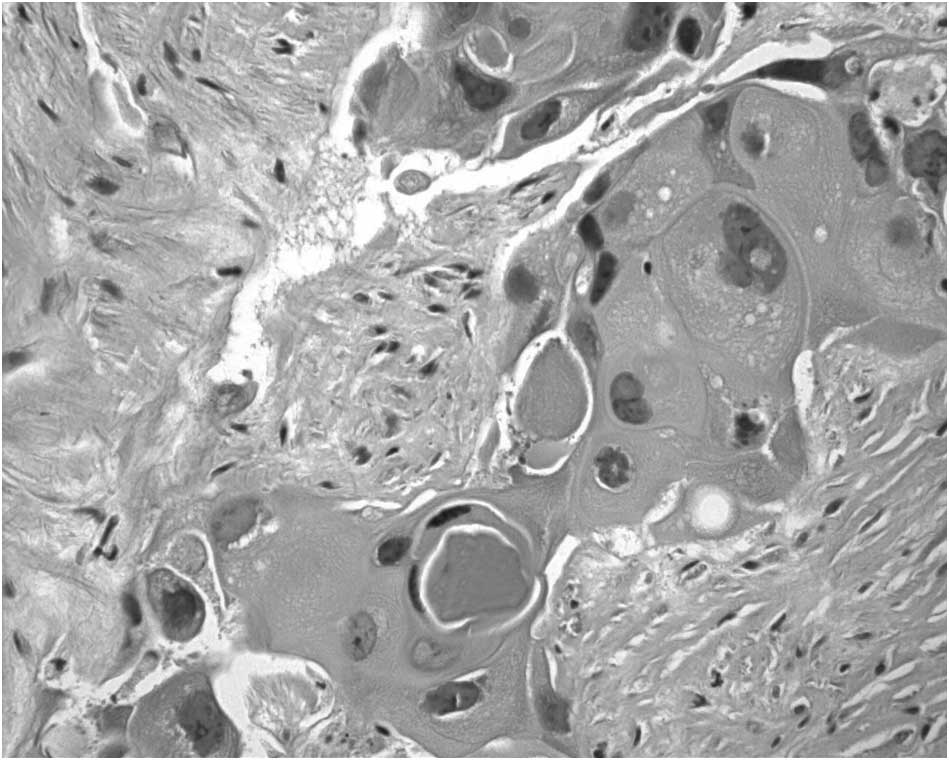
ultrasonography. An ultrasound guided puncture biopsy was
conducted. The pathological examinations suggested proliferation of
squamous cancer cells forming intercellular bridges and keratin
pearls (Fig. 2).
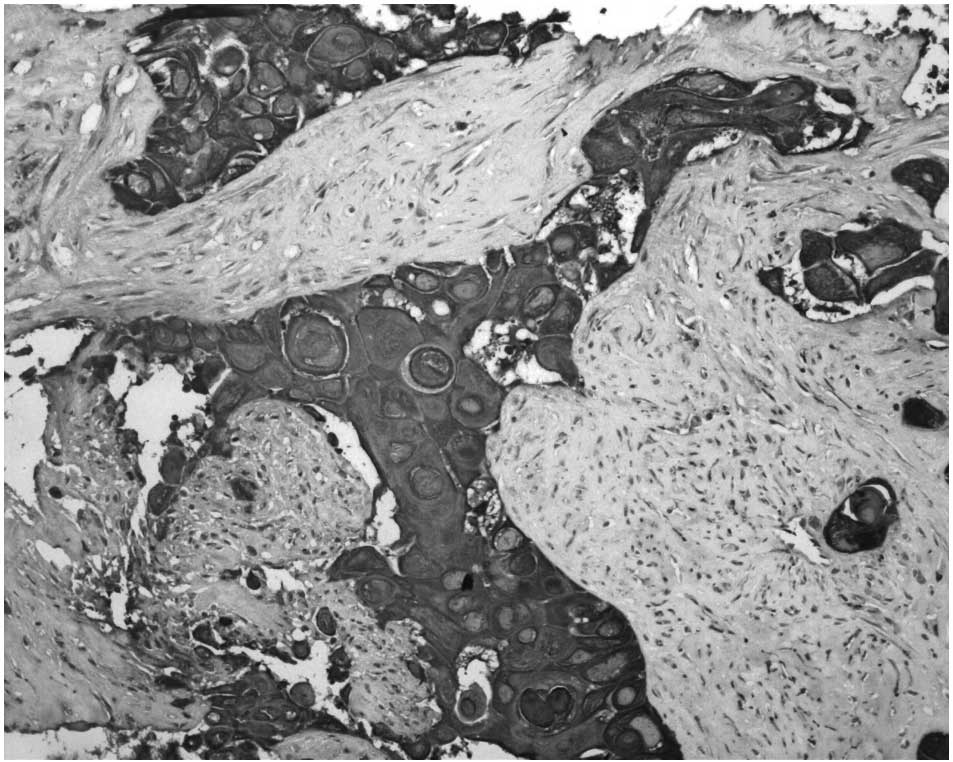
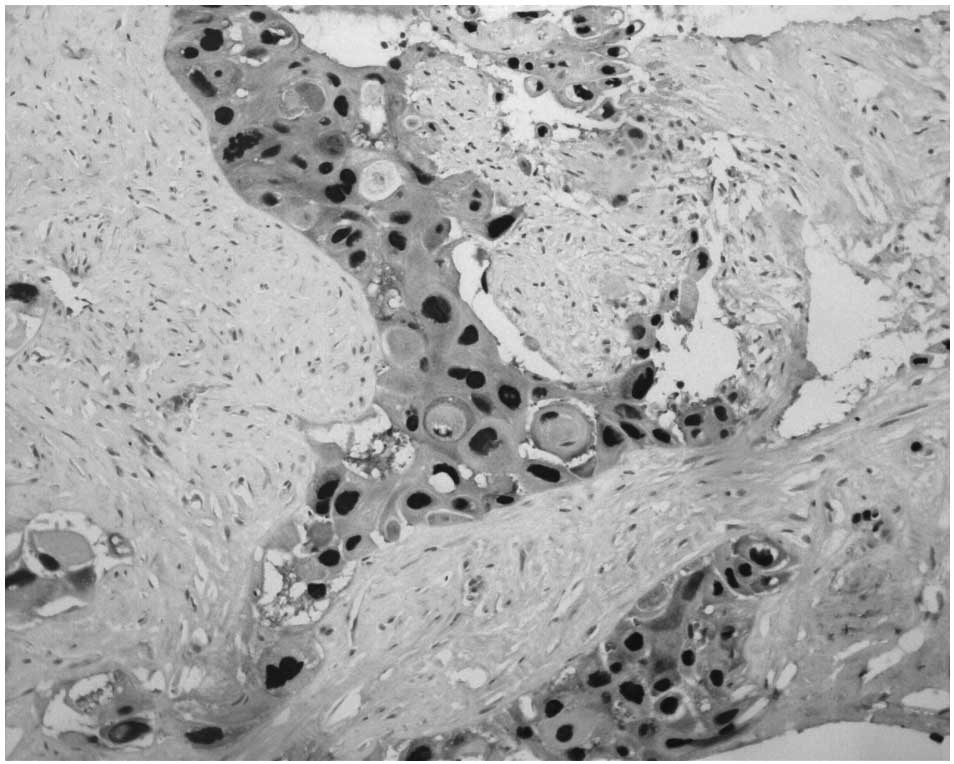
Immunohistochemical staining showed positive for cytokeratin (CK)
14 (Fig. 3) and p63 (Fig. 4), which contributed to the
diagnosis of SCC. Since no specific primary lesion was detected,
the patient was ultimately diagnosed as retroperitoneal metastatic
SCC of unknown primary site.
Subsequent to sound discussion among the
multidisciplinary team (MDT), surgery and radiotherapy were not
recommended at the time as the tumor was fixed to the entire
retroperitoneal cavity, which had no clear boundaries and enveloped
the abdominal aorta as well as other vascular elements. Thus
chemotherapy was selected as the first-line treatment. From
December 19th 2008, the patient underwent six 21-day cycles of
chemotherapy of cisplatin (25 mg/m2/day on days 2–4),
paclitaxel (80 mg/m2/day on days 1 and 8) and
5-fluorouracil (500 mg/m2/day on days 1–3). After one
cycle of chemotherapy, the waist pain was completely relieved.
Serum levels of CEA and CA199 decreased to normal levels. At the
end of the second cycle, clinical partial response of the lesion
was confirmed by abdominal CT (Fig.
5) and clinical complete response (CCR) after six cycles
(Fig. 6). Due to hematological
toxicity paclitaxel was cancelled on day 8 in cycles 2 and 6. Grade
3/4 toxicities (Common Toxicity Criteria, version 3.0) involving
nausea/vomiting, neutropenia, hair loss and peripheral
neurotoxicity were observed.
The patient was followed up for 18 months, during
which she led a normal life. Periodical clinical and instrumental
examinations showed no signs of tumor recurrence or metastasis
until September 2010, when she was referred to a hospital,
complaining of recent onset of dysphagia. Esophago
gastroduodenoscopy showed a mass in the middle-low esophageal
lumen. Biopsy of the mass was performed and histological
examination revealed SCC. Following detailed examinations, no other
lesions were found and the diagnosis was clarified as CUP with the
subsequent primary site identified in the esophagus. Subsequent
treatment strategies were discussed among the MDT. Surgery was not
recommended as the metastatic site had already been identified.
However, the patient was weak and could not tolerate the toxicity
of the chemotherapy. Thus, she underwent radiotherapy of the tumor
and the regional lymph nodes. Following radiotherapy, stable
disease was confirmed. The patient was kept free of disease
progression for 3 months. In March 2011, the patient was referred
to hospital complaining of more severe dysphagia. No chemotherapy
or radiotherapy was considered due to her condition. Supportive
care was provided, and the patient succumbed to the disease one
month later, with OS of 28 months.
Discussion
CUP is defined as histologically proven metastatic
malignant tumor whose primary site cannot be identified during
pretreatment evaluation, accounting for 5–10% of the malignancies
diagnosed (4). There are four
major types of CUP and SCC comprising 5–10% of malignancies
compared to 55–60% for adenocarcinoma (ADC) (1). As previously reported, in only 25% of
patients the primary site is detected in antemortem examinations
(2). A previous study with almost
1,000 patients revealed that lung and pancreatic cancers were the
most frequent primary sites identified (almost half of all cases),
although esophageal cancer was not observed (5). Numerous sites of involvement are
observed in 26% of CUP patients, while the most common isolated
sites are liver (24%) and lung (12%), followed by lymph nodes (11%)
(6). Esophageal primary cancer
also presents with lymph node involvement, with cervical lymph
nodes (30–49.5%) being more common than abdominal ones (8–12%)
(7,8). Thus, it is rare to observe squamous
CUP presenting with solitary retroperitoneal lymph node metastasis.
Detection of the primary site in the esophagus 18 months later is
extremely rare. In fact, a search of published studies on Medline,
EMBASE and the Web of Science, until October 2011, yielded no
similar studies to the present one.
Prognosis of CUP is poor and median survival is
predicted to be 6–9 months (3).
Previous studies discussed multidisciplinary treatment of advanced
esophageal carcinoma, which showed that palliative resection was
not recommended and induction chemotherapy followed by
chemoradiotherapy (CRT) was feasible (9,10).
Neither of these studies focused on the treatment of
retroperitoneal lymph node metastasis of SCC. Since the mass had no
clear boundaries and enveloped important vascular elements, surgery
and radiotherapy were not recommended. Thus, a platinum-based
chemotherapy regimen was chosen according to the National
Comprehensive Cancer Network (NCCN 2008 version 1.1) guidelines.
Moreover, the PFS and OS in advanced esophageal squamous cell
carcinoma (ESCC) following first-line chemotherapy were not
satisfied, with ranges of 4.5–6.1 and 7.4–11.5 months, respectively
(Table I) (11–15).
Compared with patients in those studies, the outcome of the patient
in our case was improved, with PFS of 18 months and OS of 28
months.
 | Table IPFS and OS in advanced ESCC after
first-line chemotherapy. |
Table I
PFS and OS in advanced ESCC after
first-line chemotherapy.
| Authors (Refs.) | Date | Country | Total sample
size | Size of SCC | Chemotherapy
drugs | PFS | OS |
|---|
| Cao (11) | 2009 | China | 48 | 46 | Nedaplatin,
paclitaxel | 6.1 m | 11.5 m |
| Shim (12) | 2010 | Korea | 38 | 38 | Cisplatin,
5-fluorouracil | 4.5 m | 7.4 m |
| Honda (13) | 2010 | Japan | 41 | 41 | Doxirubicin,
cisplatin, 5-fluorouracil | 153 d | 306 d |
| Kim (14) | 2010 | Korea | 39 | 39 | Docetaxel,
cisplatin | 5 m | 8.3 m |
| Overman (15) | 2010 | USA | 117 | 17 | Docetaxel, cisplatin,
5-fluorouracil | 5.3 m | 8.9 m |
Therefore, it is likely that the different
biological characteristics resulting in a different outcome between
carcinomas with reverse sequence of the primary site and metastatic
site played a role. Findings of an early study (16) showed that the percentage of the
osseous involvement was much lower in lung cancer presenting as CUP
than that in known primary cancers, which was opposite to findings
in pancreatic and prostatic cancers (16). However, investigations of
esophageal cancers in the studies searched were not identified.
Thus, more relevant studies investigating the role of the
biological characteristics in the prognosis of such cancers should
be conducted.
The hypothesis of whether a complete response
following first-line therapy is beneficial to OS was considered.
Keskin et al(17) reported
findings on 410 patients with locally advanced breast cancer who
had undergone surgery following neoadjuvant chemotherapy. A longer
PFS was noted in patients achieving pathological complete response
(pCR) after neoadjuvant chemotherapy, although no increase in OS
was observed. Results from the TECHNO trial of the AGO and GBG
study groups revealed that among the patients with human epidermal
growth factor receptor 2 (HER-2)-overexpressing breast cancer, pCR
after neoadjuvant among anti-HER2 therapy in combination with
chemotherapy followed by maintenance trastuzumab had an improved
long-term outcome (18). Apart
from the aforementioned studies on breast cancer patients who
received preoperative chemotherapy, a previous study (19) reported findings on 31 patients of
esophageal cancer with distant lymph node metastasis. Only four of
these 19 patients survived for >3 years and half of the
survivors were those who showed CCR after definitive CRT (19). In their study, Yamamoto et
al(20) reported a patient of
advanced ESCC treated with chemotherapy with docetaxel,
5-fluorouracil and cisplatin. CCR was confirmed after 2 cycles of
chemotherapy and OS of 4 years was observed. However, no
large-scale studies on palliative chemotherapy as mentioned above
were identified, thus, more clinical studies regarding this
mechanism are required.
In summary, to the best of our knowledge, this is
the first case of esophageal SCC initially presenting as metastatic
site of a large retroperitoneal mass. Clinical complete response
was confirmed following first-line chemotherapy. PFS of 18 months
and OS of 28 months were observed. Thus, the different biological
characteristics and/or complete response to chemotherapy may
contribute to the relatively long PFS and OS. Nevertheless,
large-scale studies are required to determine the mechanism of
action.
References
|
1.
|
Oien KA: Pathologic evaluation of unknown
primary cancer. Semin Oncol. 36:8–37. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Hillen HF: Unknown primary tumours.
Postgrad Med J. 76:690–693. 2000. View Article : Google Scholar
|
|
3.
|
Pavlidis N, Briasoulis E, Hainsworth J and
Greco FA: Diagnostic and therapeutic management of cancer of an
unknown primary. Eur J Cancer. 39:1990–2005. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Greco FA and Hainsworth JD: Tumors of
unknown origin. CA Cancer J Clin. 42:96–115. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Pentheroudakis G, Golfinopoulos V and
Pavlidis N: Switching benchmarks in cancer of unknown primary: from
autopsy to microarray. Eur J Cancer. 43:2026–2036. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
van de Wouw AJ, Janssen-Heijnen ML,
Coebergh JW and Hillen HF: Epidemiology of unknown primary tumours;
incidence and population-based survival of 1285 patients in
Southeast Netherlands, 1984–1992. Eur J Cancer. 38:409–413.
2002.PubMed/NCBI
|
|
7.
|
Akiyama H, Tsurumaru M, Udagawa H and
Kajiyama Y: Radical lymph node dissection for cancer of the
thoracic esophagus. Ann Surg. 220:364–373. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Chen J, Liu S, Pan J, et al: The pattern
and prevalence of lymphatic spread in thoracic oesophageal squamous
cell carcinoma. Eur J Cardiothorac Surg. 36:480–486. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Kelsen DP, Winter KA, Gunderson LL, et al:
Long-term results of RTOG trial 8911 (USA Intergroup 113): a random
assignment trial comparison of chemotherapy followed by surgery
compared with surgery alone for esophageal cancer. J Clin Oncol.
25:3719–3725. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Ruhstaller T, Templeton A, Ribi K, et al:
Intense therapy in patients with locally advanced esophageal cancer
beyond hope for surgical cure: a prospective, multicenter phase II
trial of the Swiss Group for Clinical Cancer Research (SAKK 76/02).
Onkologie. 33:222–228. 2010. View Article : Google Scholar
|
|
11.
|
Cao W, Xu C, Lou G, et al: A phase II
study of paclitaxel and nedaplatin as first-line chemotherapy in
patients with advanced esophageal cancer. Jpn J Clin Oncol.
39:582–587. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Shim HJ, Cho SH, Hwang JE, et al: Phase II
study of docetaxel and cisplatin chemotherapy in
5-fluorouracil/cisplatin pretreated esophageal cancer. Am J Clin
Oncol. 33:624–628. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Honda M, Miura A, Izumi Y, et al:
Doxorubicin, cisplatin, and fluorouracil combination therapy for
metastatic esophageal SCC. Dis Esophagus. 23:641–645. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Kim JY, Do YR, Park KU, et al: A
multi-center phase II study of docetaxel plus cisplatin as
first-line therapy in patients with metastatic squamous cell
esophageal cancer. Cancer Chemother Pharmacol. 66:31–36. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Overman MJ, Kazmi SM, Jhamb J, et al:
Weekly docetaxel, cisplatin, and 5-fluorouracil as initial therapy
for patients with advanced gastric and esophageal cancer. Cancer.
116:1446–1453. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Nystrom JS, Weiner JM,
Heffelfinger-Juttner J, Irwin LE, Bateman JR and Wolf RM:
Metastatic and histologic presentations in unknown primary cancer.
Semin Oncol. 4:53–58. 1977.PubMed/NCBI
|
|
17.
|
Keskin S, Muslumanoglu M, Saip P, et al:
Clinical and pathological features of breast cancer associated with
the pathological complete response to anthracycline-based
neoadjuvant chemotherapy. Oncology. 81:30–38. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Untch M, Fasching PA, Konecny GE, et al:
Pathologic complete response after neoadjuvant chemotherapy plus
trastuzumab predicts favorable survival in human epidermal growth
factor receptor 2-overexpressing breast cancer: results from the
TECHNO trial of the AGO and GBG study groups. J Clin Oncol.
29:3351–3357. 2011. View Article : Google Scholar
|
|
19.
|
Okamura S, Fujiwara H, Shiozaki A, et al:
Long-term survivors of esophageal carcinoma with distant lymph node
metastasis. Hepatogastroenterology. 58:421–425. 2011.PubMed/NCBI
|
|
20.
|
Yamamoto Y, Ikeda M, Takashima M, et al: A
case of a patient with stage IVa esophageal cancer surviving over 4
years by combination chemotherapy with docetaxel, 5-FU and
cisplatin, without operation. Gan To Kagaku Ryoho. 38:1321–1324.
2011.(In Japanese).
|