Introduction
Cutaneous ureterostomy is a type of urinary
diversion involving simple surgical procedures and requiring the
least invasive surgical approach, making it suitable for elderly
patients and those with a poor performance status. However,
cutaneous ureterostomy is generally retroperitoneally constructed.
Therefore, the ureter cannot be lifted to the abdominal wall in
cases with a limited available ureter length. Thus, selection of a
different type of urinary diversion is crucial. We succeeded in
constructing a cutaneous ureterostomy in patients with a shorter
ureter length by transperitoneal construction using the transverse
mesocolon, as was previously described (1).
In the present study, in order to demonstrate that
the treatment outcome of transperitoneally constructed cutaneous
ureterostomy using the transverse mesocolon is not inferior to that
of conventional retroperitoneal cutaneous ureterostomy, a
comparative investigation was conducted between patients who were
treated with the two procedures during the same time period.
Materials and methods
Cases
A total of 160 cases of urinary diversion were
performed between March, 2004 and November, 2011 at our
institution. Among these, cutaneous ureterostomy was performed in
26 cases and conventional retroperitoneal construction in 15 cases
(15 ureters), while transperitoneal construction was performed in
11 cases and 18 ureters. Seven of the transperitoneal
ureterocutaneostomy cases were bilateral and all the cases of
retroperitoneal ureterocutaneostomy were unilateral. In this study
we aimed to describe the transperitoneal ureterocutaneostomy
technique using the transverse mesocolon and the outcomes of this
procedure in comparison to the conventional technique.
Technique
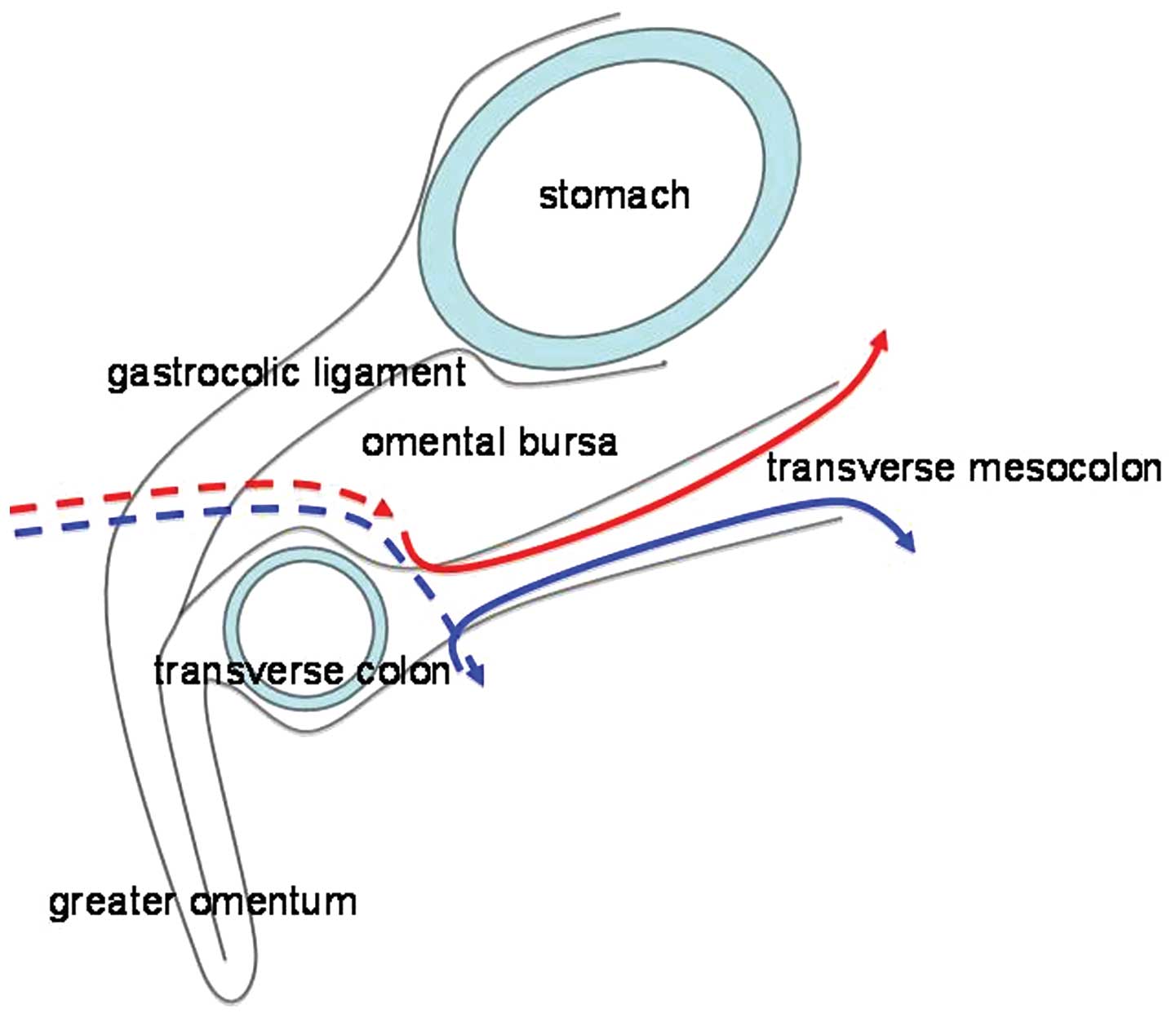
During the procedure, on the right side the
transverse colon is caudally mobilized in the same manner as when
performing a right radical nephrectomy and the retroperitoneum is
incised on the outer side of the descending part of the duodenum.
The right ureter is then identified and mobilized. An incision is
made into the serosa of the transverse mesocolon close to the area
of attachment of the transverse colon, while the great omentum is
moved caudally. The subserous part of the transverse mesocolon is
detached and a space is created which allows the ureter to pass
from this area towards the area of the retroperitoneal incision,
similar to creating a tunnel (Fig. 1,
red solid line). The right ureter is passed from the root of
the transverse mesocolon towards the area to which the transverse
colon is attached in this space and the transverse mesocolon is
then fixed to the connective tissue surrounding the ureter.
Subsequently, the gastrocolic ligament is penetrated from the
ventral side towards the area to which the transverse colon is
attached, in order to construct a space for the ureter to pass
through (Fig. 1, red broken line).
The ureter is passed through this area and fixed to its surrounding
tissues.
On the left side, the mesocolon is incised between
the abdominal aorta and the inferior mesenteric vein at the level
of the Treitz suspensory ligament, as during a left radical
nephrectomy. The retroperitoneum is reached and the left ureter is
identified, mobilized and pulled inside the abdominal cavity. An
incision is made on the serosa of the transverse mesocolon near the
area to which the transverse colon is attached, while the greater
omentum is moved cranially. From this area, the subserous part of
the transverse mesocolon is detached towards the mesocolon incision
area, similar to creating a tunnel and a space is created for the
ureter to pass through (Fig. 1, blue
solid line). Subsequently, the gastrocolic ligament and the
transverse mesocolon are penetrated from the ventral side towards
the area of the small incision near the attachment site of the
transverse mesocolon, in order to construct a space for the ureter
to pass through (Fig. 1, blue broken
line). The ureter is passed from the root of the transverse
mesocolon towards the gastrocolic ligament in this space and fixed
to its surrounding connective tissue. Subsequently, the ureters are
lifted bilaterally to the abdominal wall and a ureteral stoma is
constructed. If both the available right and left ureters are
short, a ureteral stoma is constructed by a median xiphoid process.
Furthermore, for cases in which there is a limited available length
for either the right or left ureter, a ureteral stoma may be
constructed near the lateral border of the rectus abdominis muscle
under the costal arch. An excess 3 cm of the ureter, plus the
length from the renal hilus to the abdominal wall, as measured by
computed tomography, is a sufficient ureter length for the new
construct.
Statistical analysis
The treatment outcome of cutaneous ureterostomy
cases constructed transperitoneally using the transverse mesocolon
and that of cases constructed retroperitoneally using the
conventional method performed within the same period, were
retrospectively evaluated. Decisions regarding adverse events were
made based on the Common Terminology Criteria for Adverse Events
(CTCAE) v4.0 (2). The Student’s
t-test, Chi-square test or Friedman’s test were used for the
statistical analysis.
Results
Clinical characteristics according to the
cutaneous ureterostomy type
The transperitoneal ureterocutaneostomy cases
included 5 males and 6 females, with a median age of 81 years
(range, 62–94 years) and a median body mass index (BMI) of 22.3
(range, 17.1–26.3). The underlying pathology was bladder cancer in
6 patients, bladder cancer with unilateral ureteral cancer in 2
patients, prostate cancer in 2 patients and vaginal cancer in 1
patient (Table I). Out of the 8
patients with bladder cancer, 1 had stage 0is disease, 1 had stage
I disease, 2 had stage II disease, 2 had stage III disease and 2
had stage IV disease, based on the clinical staging system. All 3
patients with prostate or vaginal cancer had stage IV disease. The
cutaneous ureterostomy was performed prior to total cystectomy with
or without urethrectomy in 7 patients and a cutaneous ureterostomy
was performed without cystectomy in 4 cases, 1 of which underwent a
colostomy at the same time. Together with total cystectomy,
unilateral nephroureterectomy was performed in 2 patients with
ureteral cancer. Furthermore, 2 patients had previously undergone
unilateral nephroureterectomy or nephrectomy due to ureteral cancer
or nephrophthisis. A significant difference was observed regarding
age between the groups that underwent the different surgical
procedures (P=0.032), with no significant differences regarding the
BMI or the follow-up period (P=0.516 and 0.197, respectively).
 | Table I.Clinical characteristics of the
patients according to the cutaneous ureterostomy type. |
Table I.
Clinical characteristics of the
patients according to the cutaneous ureterostomy type.
| Characteristics | Transperitoneal | Retroperitoneal | P-value |
|---|
| Total no. of
patients | 11 | 15 | |
| Gender | | | |
| Male | 5 | 10 | |
| Female | 6 | 5 | |
| Age (years) | | | |
| Median (range) | 81 (62–94) | 71 (51–84) | 0.032 |
| 80> | 4 | 11 | |
| 80≤ | 7 | 4 | |
| BMI | | | |
| Median (range) | 22.3 (17.1–26.3) | 22.8 (18.4–26.5) | 0.516 |
| Underlying
disease | | | |
| Bladder cancer | 6 | 5 | |
| Bladder cancer +
ureteral cancer | 2 | 2 | |
| Bladder cancer +
renal pelvic cancer | 0 | 1 | |
| Bladder cancer +
prostate cancer | 0 | 2 | |
| Bladder cancer +
atrophic kidney | 0 | 3 | |
| Prostate
cancer | 2 | 0 | |
| Prostate cancer +
atrophic kindey | 0 | 2 | |
| Vaginal cancer | 1 | 0 | |
| Operation | | | |
| Ureterostomy
alone | 3 | 1 | |
| + cystectomy | 5 | 5 | |
| + cystectomy +
nephroureterectomy | 2 | 8 | |
| + colostomy | 1 | 0 | |
| + pelvic
exenteration + nephroureterectomy + colostomy | 0 | 1 | |
| Follow-up period
(months) | | | |
| Median (range) | 8.3 (1.0–58.7) | 20.1 (3.5–83.3) | 0.197 |
| Survival | | | |
| Alive | 4 | 6 | |
| Deceased | 7 | 9 | |
Postoperative complications according to
the cutaneous ureterostomy type
Ileus developed in 1 (9.1%) bilateral
transperitoneal ureterocutaneostomy case and in 1 (6.7%)
retroperitoneal cutaneous ureterostomy case, which improved with
conservative therapy alone (CTCAE v.4.0 grade 2). No significant
difference was observed between the surgical procedures regarding
ileus (P=0.827) (Table II).
 | Table II.Postoperative complications according
to cutaneous ureterostomy type. |
Table II.
Postoperative complications according
to cutaneous ureterostomy type.
| Complications | Transperitoneal | Retroperitoneal | P-value |
|---|
| Ileus | 1 | 1 | 0.827 |
| Acute | 3 | 8 | 0.199 |
| pyelonephritis | | | |
| within 3
months | 3 | 8 | |
| after 3 months | 2 | 7 | |
Acute pyelonephritis
Acute pyelonephritis developed in 3 (27.3%)
transperitoneal ureterocutaneostomy cases, 2 of which were
bilateral. The catheter remained in place in all 3 cases. Acute
pyelonephritis developed in 8 (53.3%) retroperitoneal
ureterocutaneostomy cases, with the catheter remaining in place in
all the cases. All the patients showed improvement with the
administration of antibiotics alone (CTCAE v.4.0 grade 3). No
significant difference was observed between the two surgical
procedures regarding the incidence of acute pyelonephritis
(P=0.199).
Catheter-free status according to the
cutaneous ureterostomy type
Transperitoneal ureterocutaneostomy was performed in
7 bilateral and 4 unilateral cutaneous ureterostomy cases, totaling
11 cases and 18 ureters. A double-barrel-type stoma was constructed
in the center of the upper abdomen in 3 of these cases. All 15
cases undergoing retroperitoneal ureterocutaneostomy were
unilateral. No significant difference was observed between surgical
procedures regarding the catheter-free status of each individual
case (P=0.393) (Table III). No
significant difference was observed between surgical procedures
regarding the catheter-free status according to the renal units
(P=0.525). In addition, no significant difference was observed
between surgical procedures regarding the catheter-free status
according to the renal units and in those patients in whom it was
attempted to obtain a catheter-free status (P=0.437) (Table III).
 | Table III.Catheter-free status according to the
cutaneous ureterostomy type. |
Table III.
Catheter-free status according to the
cutaneous ureterostomy type.
| Type | Transperitoneal | Retroperitoneal | P-value |
|---|
| Ureter | | | |
| Total | 18 | 15 | |
| Right | 2 | 8 | |
| Left | 2 | 7 | |
| Bilateral | 7 | 0 | |
| Stomal side | | | |
| Right | 5 | 8 | |
| Left | 3 | 7 | |
| Middle | 3 | 0 | |
| Catheter-free
(cases) | | | |
| Yes | 3 | 2 | 0.393 |
| No | 8 | 13 | |
| Catheter-free (renal
units) | | | |
| Yes | 4 | 2 | 0.525 |
| No | 14 | 13 | |
| Attempted
catheter-free (renal units) | | | |
| Yes | 4 | 2 | 0.437 |
| No | 4 | 5 | |
Renal function [blood urea nitrogen (BUN)
and serum creatinine (Cr) values] according to the cutaneous
ureterostomy type (Table IV)
In the transperitoneal ureterocutaneostomy cases,
the median rate of change between the serum Cr value prior to
surgery and that on the last follow-up day was 97.1% (58.1–148.5)
and the median rate of change between the serum Cr value at the
early postoperative examination and that on the last follow-up day
was 97.1% (78.0–116.3). Moreover, the median rate of change between
the BUN value prior to surgery and that on the last follow-up day
was 86.4% (58.2–161.0) and the median rate of change between the
BUN value at the early postoperative period and that on the last
follow-up day was 111.1% (73.4–169.4). No significant difference
was observed in the serum Cr or BUN values prior to surgery, at the
early postoperative examination or on the last follow-up day.
Discussion
Cutaneous ureterostomy is usually constructed
retroperitoneally in cases where there is a sufficient ureter
length available. However, urinary diversion in cases of limited
available ureter length and when the use of the digestive tract is
preferably avoided has been challenging. To address this problem,
we developed a method of construction using a shorter ureter
compared to the conventional retroperitoneal ureterocutaneostomy,
by transperitoneally constructing the cutaneous ureterostomy using
the transverse mesocolon (1). This
method is also suitable for cases with anatomical abnormalities,
such as extreme obesity, although these cases have a sufficient
available ureter length. In this study, in order to prove that the
clinical outcome of the transperitoneal ureterocutaneostomy is not
inferior to that of the conventional retroperitoneal
ureterocutaneostomy, a comparison was conducted between the
clinical outcomes of patients who underwent the two different
procedures during the same period.
First, postoperative adverse events were
investigated. The major advantage of retroperitoneal
ureterocutaneostomy is that all operations may be completed in the
retroperitoneum. Accordingly, surgical complications accompanying
opening the abdominal cavity, such as ileus, may be avoided. In
cases in which the transperitoneal technique was applied, the
transverse mesocolon was used in addition to opening the abdominal
cavity. Therefore, the incidence of ileus was likely to be higher
compared to the cases where the transverse mesocolon was not used.
However, in the present study, ileus only developed in 1 patient,
who recovered with conservative treatment alone and there was no
significant difference compared to the retroperitoneal cases
(P=0.827). As regards acute pyelonephritis, Yoshimura et al
reported that the incidence within 3 months following surgery and
thereafter was 19.7 and 11.5%, respectively (3), whereas according to Kim et al,
the incidence was 22.2 and 11.1%, respectively (4). In this study, the incidence of acute
pyelonephritis among cases treated with the transperitoneal
technique was 27.3% (3 out of the 11 cases) within 1 month from
surgery and 18.2% (2 out of the 11 cases) from 3 months onwards. No
significant difference was observed between the surgical procedures
regarding the occurrence of acute pyelonephritis during the same
period (P=0.199); however, the incidence was slightly higher
compared to that with conventional techniques (3,4). In
all cases, a catheter was present at the onset of acute
pyelonephritis in the two surgical procedures. Thus, it is
hypothesized that the incidence of acute pyelonephritis may be
reduced if a catheter-free status is achieved.
The catheter-free status was then investigated. The
rate of catheter-free status was 22.2% (4 out of the 18 ureters) in
patients treated with the transperitoneal technique and 13.3% (2
out of the 15 ureters) in those treated with the retroperitoneal
technique, demonstrating no significant difference between the
surgical procedures (P=0.393). Regarding ureterocutaneostomy, if a
single stoma and catheter-free status are achieved bilaterally,
this technique may be comparable to an ileal conduit. This is a
technique that has received little attention internationally;
however, a catheter-free status was achieved in 80–90% of cases by
urologists in Japan (5–7). According to a previous study by Terai
et al regarding double barrel- and barrel-type stoma, 84% of
stomas and ipsilateral kidneys and 81% of the contralateral kidneys
achieved a catheter-free status; therefore, a catheter-free status
was achieved in 79% of all cases (6). However, for cases exhibiting stoma
stenosis, rendering ureteral catheter placement essential, the
quality of life of the patient may be compromised due to the
possible onset of complications, such as urinary tract infections
and renal dysfunction. In the present study, there was no
significant difference between the surgical procedures regarding
the median follow-up period (P=0.197). However, the median
follow-up period of transperitoneal ureterocutaneostomy cases was
only 8.3 months, almost half of that observed in retroperitoneal
ureterocutaneostomy cases, which was 20.1 months. The purpose of
the transperitoneal technique in several cases was to secure the
urinary tract and ease the symptoms of the patient during
palliative care. Accordingly, this procedure was a type of urinary
diversion performed during the palliative operation; therefore, a
catheter-free status was not our intent in all cases. Furthermore,
securing a sufficient amount of urine is necessary at the early
postoperative period for cases where securing the urinary tract is
required for chemotherapy; therefore, a catheter-free status was
not attempted in these cases. Moreover, certain chemotherapeutic
regimens require placement of a catheter and attempting to achieve
a catheter free-status may lead to a delay in the initiation of
chemotherapy, a decrease in renal function and the administration
of an insufficient volume of anticancer drugs, due to the
hydronephrosis that occurs at least temporarily. The risk of
pyelonephritis may also increase and renal function may decrease in
the long-term. Therefore, we did not attempt to achieve a
catheter-free status in all the cases, since our priority was to
ensure sufficient renal function and allow the administration of
adequate volume of anticancer drugs during the early postoperative
period. We only attempted to provide a catheter-free status in
cases with predicted long-term survival.
Due to the the reasons mentioned previously, the
catheter-free status was attempted in 6 (8 ureters, since 2 cases
were bilateral) out of the 11 cases (18 ureters) treated by
transperitoneal cutaneous ureterostomy. Among these, a
catheter-free status was achieved in 4 cases and 4 ureters (1 case
was a bilateral cutaneous ureterostomy with a catheter-free status
achieved on one side). Accordingly, any evaluation considering only
the cases in which a catheter-free status was attempted revealed a
success rate of 50% (4 out of 8 ureters).
A catheter-free status was not attempted in all
cases of retroperitoneal cutaneous ureterostomy due to the same
reasons mentioned above. Out of the 15 cases (15 ureters) who
underwent retroperitoneal ureterocutaneostomy, a catheter-free
status was attempted in 7 cases and 7 ureters. Of these, a
catheter-free status was achieved in 2 cases and 2 ureters (28.6%).
These results lead to the conclusion that a catheter-free status is
feasible even when the cutaneous ureterostomy is transperitoneally
constructed. Furthermore, no significant difference was observed
between the surgical procedures regarding the catheter-free status.
However, the rate of attaining a catheter-free status was lower
among the conventional retroperitoneal ureterocutaneostomy cases.
Therefore, it is considered necessary to conduct a ureterostomy
according to the Toyoda method (5), which was also adopted by Terai et
al (6), or the Hirokawa method
(7), in order to avoid the need
for an indwelling catheter due to future stoma stenosis.
As regards renal function, no significant changes
(BUN and serum Cr values) were observed in the transperitoneal
ureterocutaneostomy cases at the postoperative, early postoperative
(1 month after surgery) and the final follow-up examinations
(P=0.739 and 0.078). Therefore, there was no significant effect on
the renal function when the ureter was run transperitoneally using
the transverse colon. The incidence of acute pyelonephritis was
slightly higher with the transperitoneal technique, compared to
studies on conventional retroperitoneal ureterocutaneostomy, with a
lower rate of catheter-free status. However, renal function did not
decrease between the preoperative and postoperative examinations.
Adopting a procedure to avoid the stenosis of the stoma may likely
lead to an increase in the catheter-free status rate and decrease
the occurrence of acute pyelonephritis.
In conclusion, transperitoneal cutaneous
ureterostomy using the transverse mesocolon is a surgical procedure
that should be considered for urinary diversions in cases with a
limited available ureter length and in which use of the digestive
tract is preferably avoided.
References
|
1.
|
Furubayashi N, Nakamura M, Hishikawa K,
Fukuda A, Matumoto T and Hasegawa Y: Cutaneous ureterostomy using
the transverse mesocolon. Int J Urol. 19:174–176. 2012. View Article : Google Scholar
|
|
2.
|
Common Terminology Criteria for Adverse
Events (CTCAE): v4.0. http://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm#ctc_40.
|
|
3.
|
Yoshimura K, Maekawa S, Ichioka K, Terada
N, Matsuta Y, Okubo K and Arai Y: Tubeless cutaneous ureterostomy:
the Toyoda method revisited. J Urol. 165:785–788. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Kim CJ, Wakabayashi Y, Sakano Y, Johnin K,
Yoshiki T and Okada Y: Simple technique for improving tubeless
cutaneous ureterostomy. Urology. 65:1221–1225. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Toyoda Y: A new technique for catheterless
cutaneous ureterostomy. J Urol. 117:276–278. 1977.PubMed/NCBI
|
|
6.
|
Terai A, Yoshimura K, Ueda N, Utsunomiya
N, Kohei N and Arai Y: Clinical outcome of tubeless cutaneous
ureterostomy by the Toyoda method. Int J Urol. 13:891–895. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Hirokawa M, Iwasaki A, Yamazaki A, Asakura
S, Nozaki A and Yamagishi T: Improved technique of tubeless
cutaneous ureterostomy and results of permanent urinary diversion.
Eur Urol. 16:125–132. 1989.PubMed/NCBI
|