Introduction
Improving the oncological and functional outcome of
laparoscopic radical prostatectomy (LRP) is crucial, as the
patients' quality of life is significantly affected by the severity
and duration of postoperative urinary incontinence. Since LRP is
considered to be technically challenging, a relatively long time
elapsed between its first application and its establishment as the
treatment of choice for organ-confined prostate cancer (1). Early multi-institutional studies in
Japan found the recovery of urinary function following LRP to be
slower compared to that following retropubic radical prostatectomy
(RRP) (2,3). The operative procedures used to
improve the recovery of urinary continence following radical
prostatectomy include preserving the fascia covering the levator
ani muscle (4), preserving the
bladder neck (4), preserving
neurovascular bundles (NVBs) (5),
securing a longer functional urethra (6,7),
reconstructing the posterior musculofascial plate (PMPR) (8–10),
suspending the vesicourethral anastomosis (11) and performing an anterior
reconstruction (12).
Since December, 2008, when performing LRPs, we have
been routinely preserving the fascia covering the levator ani
muscle, preserving the bladder neck, securing a functional urethral
length by using a lateral-view dissection technique (13) and suspending the vesicourethral
anastomosis. However, as these four procedures did not appear to
improve the recovery of urinary continence in LRP, in Feburary,
2010, we initiated the application of a PMPR procedure. Our
procedure differs from the original Rocco stitch (8,9) in
the aspects described below. Firstly, we used a running suture to
connect the Denonvilliers' fascia (DF) with the fibrous tissue
underneath the urethra (median fibrous raphe, MFR). Secondly, at
the beginning of the vesicourethral anastomosis, the bladder wall
was stitched 1–2 cm dorsocephalad to the bladder neck (at positions
1 and 11 o'clock on the bladder neck) and the musculofascial plate
was stitched at 5 and 7 o'clock positions on the urethra instead of
using Rocco's second-layer stitch. Although it was previously
reported that urinary continence was not improved by PMPR (14), in the present study we demonstrated
that urinary continence was recovered significantly earlier in
patients undergoing LRPs with our modified PMPR. We also evaluated
the postoperative cystograms and compared the bladder shapes
between patients undergoing LRP with PMPR and those undergoing LRP
without PMPR.
Patients and methods
Patients
LRP is being performed at our institute since 2000.
In the present study, we evaluated 32 patients undergoing LRP
(retroperitoneal approach) who were operated on by a single surgeon
(K.I.) between December, 2008 and September, 2011. Maximal
preservation of the fascia covering the levator ani muscle, bladder
neck preservation, apical dissection using a lateral view to secure
functional urethral length and decrease the positive surgical
margin at the apex, and suspension of the vesicourethral
anastomosis by suturing to the puboprostatic ligaments were
performed during all LRPs since December, 2008 (group A, n=13); our
modified PMPR procedure was added to these previous procedures from
January, 2010 onwards (group B, n=19). In group B, there was no
change in the other operative procedures intended to expedite
continence recovery. For all the patients included this study, the
indication for LRP was T1–2 N0M0 prostate cancer. Clinical staging
was determined by digital rectal examination and transrectal
urtrasonography. Computed tomography and magnetic resonance imaging
were performed in all the patients for the evaluation of lymph node
metastasis and extracapsular extension of the prostate cancer.
Radionuclide bone scanning was routinely performed in patients with
prostate-specific antigen (PSA) levels ≥10 mg/dl.
Surgical procedure
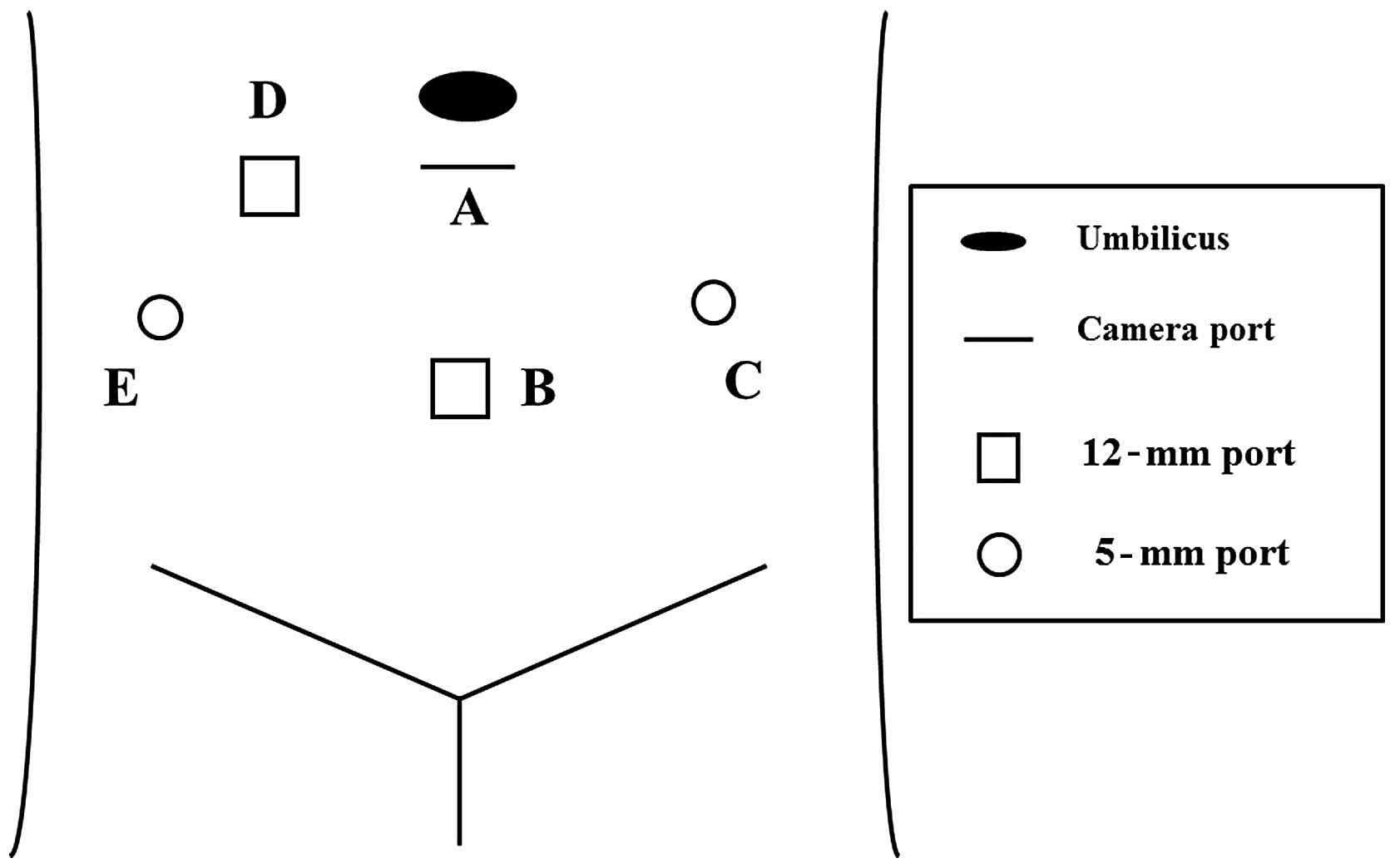
Five port sites were created as shown in Fig. 1. Obturator lymph node dissection
was performed in all the patients. Following lymph node dissection,
the junction of the endopelvic fascia was bluntly incised as
previously described (4). The
fascia covering the levator ani muscle was carefully preserved to
prevent muscle damage. The puboprostatic ligaments were severed
close to the prostate to preserve their length, since they were
later used for the anterior suspension of the vesicourethral
anastomosis. The dorsal vein complex (DVC) was ligated twice using
2-0 absorbable sutures (Polysorb, 3/8, 32-mm needle; Covidien,
Mansfield, MA, USA). The bladder neck was maximally preserved in
all the patients. Following complete dissection of the posterior
bladder neck, the vas deferens and seminal vesicles were identified
and dissected. The seminal vesicles were retracted ventrally to
expose the posterior DF. The DF was incised horizontally and the
perirectal fat was exposed. In selected patients, the NVB was
preserved. In the nerve-sparing technique, heat injury was avoided
by using metal clips on blood vessels rather than an electronic
coagulator. Following dissection of the dorsal side of the
prostate, the DVC was incised with cold scissors and the urethra
was exposed. Subsequently, the anterior side of the urethra was
incised and the urethral catheter was exposed. At apical
dissection, particularly dissection of the dorsal side of the
prostatic apex, the lateral-view approach (13) was used, as it enabled maximizing
the functional urethral length and avoiding the incorrect incision
of the prostatic apex. After the prostate was removed from the
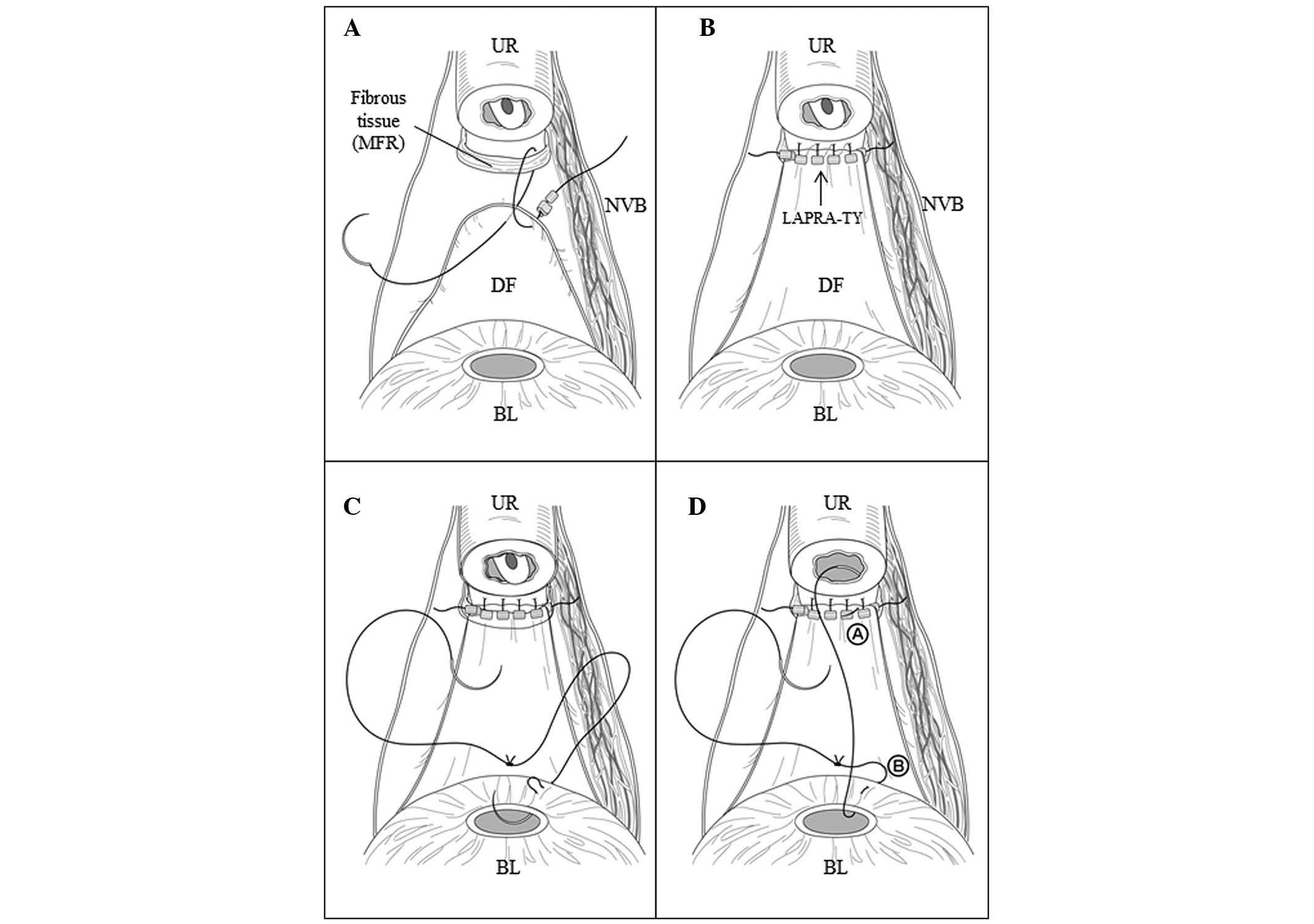
rectal bed, a running suture was placed between the DF and the
fibrous tissue under the urethra (MFR) (Fig. 2). The MFR is connected to the
cranial aspect of the rectourethralis muscle (RUM) and the RUM is
connected to the dorsal aspect of the rhabdosphincter (RS). A
vesicourethral anastomosis was then performed by placing
double-armed running sutures (∼8 sutures) with 2-0 absorbable
sutures (Polysorb, 5/8, 27-mm needle). Two 2-0 absorbable ligatures
were tied and used for the anastomosis. At the beginning of the
anastomosis, the first stitches (at 1 and 11 o'clock on the bladder
neck) were placed 1–2 cm dorsocephalad to the bladder neck (first
through the seromuscular layer and then through the full thickness
of the bladder neck) (Fig. 2). At
the 5 and 7 o'clock positions of the urethra the stitches were
placed through the urethral mucosa as well as the the reconstructed
musculofascial plate. The middle of the running suture was secured
with several LAPRA-TY® clips (Ethicon Inc., Bridgewater,
NJ, USA). We attempted to push the needles thinly through the
anterior urethra (15) and anchor
them to the fascia covering the DVC to avoid laceration of the
urethra. The double-armed running sutures were finally ligated at
the anterior side of the urethra. For the anterior suspension, the
vesicourethral anastomosis was then secured at the 1 and 11 o'clock
positions of the puboprostatic ligament by using 2-0 absorbable
sutures (Polysorb, 5/8, 27-mm needle). The anastomosis was
confirmed to be watertight prior to the two pelvic drainage tubes
being passed through the 5-mm ports and into the two iliac
fossae.
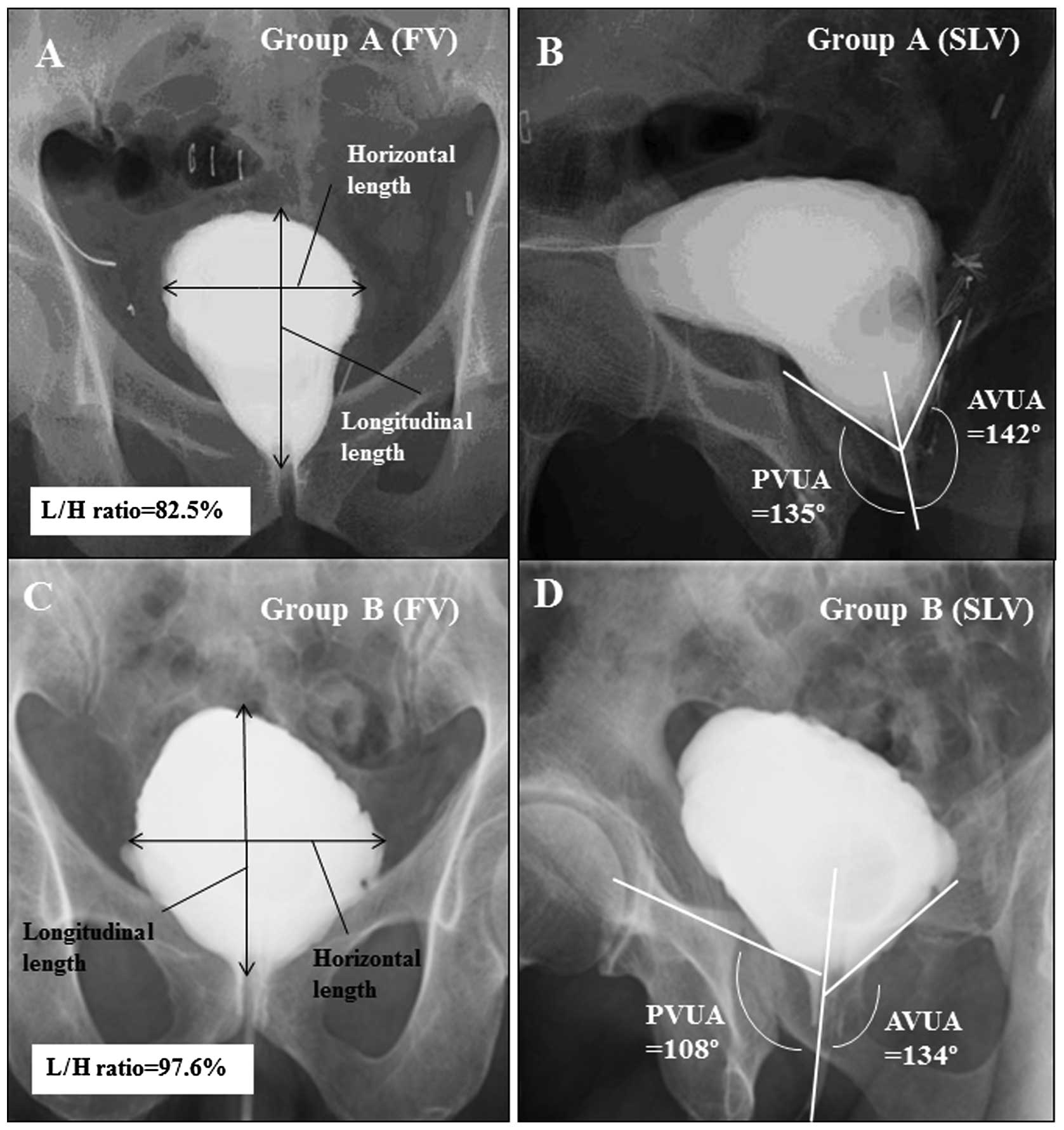
Postoperative cystography
Cystography was performed on postoperative day 5 or
6. A total of 100 ml of saline solution containing contrast media
was infused into the bladder and front-view and
45°-semilateral-view images were captured. Provided there was no
leakage or only a minor leakage at the anastomosis, the balloon
catheter was removed. If leakage was detected, cystography was
again performed 4 or 7 days later, according to the severity of the
leakage. The ratio between the longitudinal and horizontal length
(L/H ratio) was measured in the front-view cystogram (Fig. 3); the anterior vesicourethral angle
(AVUA) and the posterior vesicourethral angle (PVUA) were measured
in the semilateral-view cystogram (Fig. 3). If the catheter removal was
delayed due to leakage at the anastomosis, the final cystography
session was used for the evaluation.
Factors for evaluation
The factors evaluated are listed in Tables I and II. The clinical and pathological stages
were determined using the 2002 version of the TNM staging system.
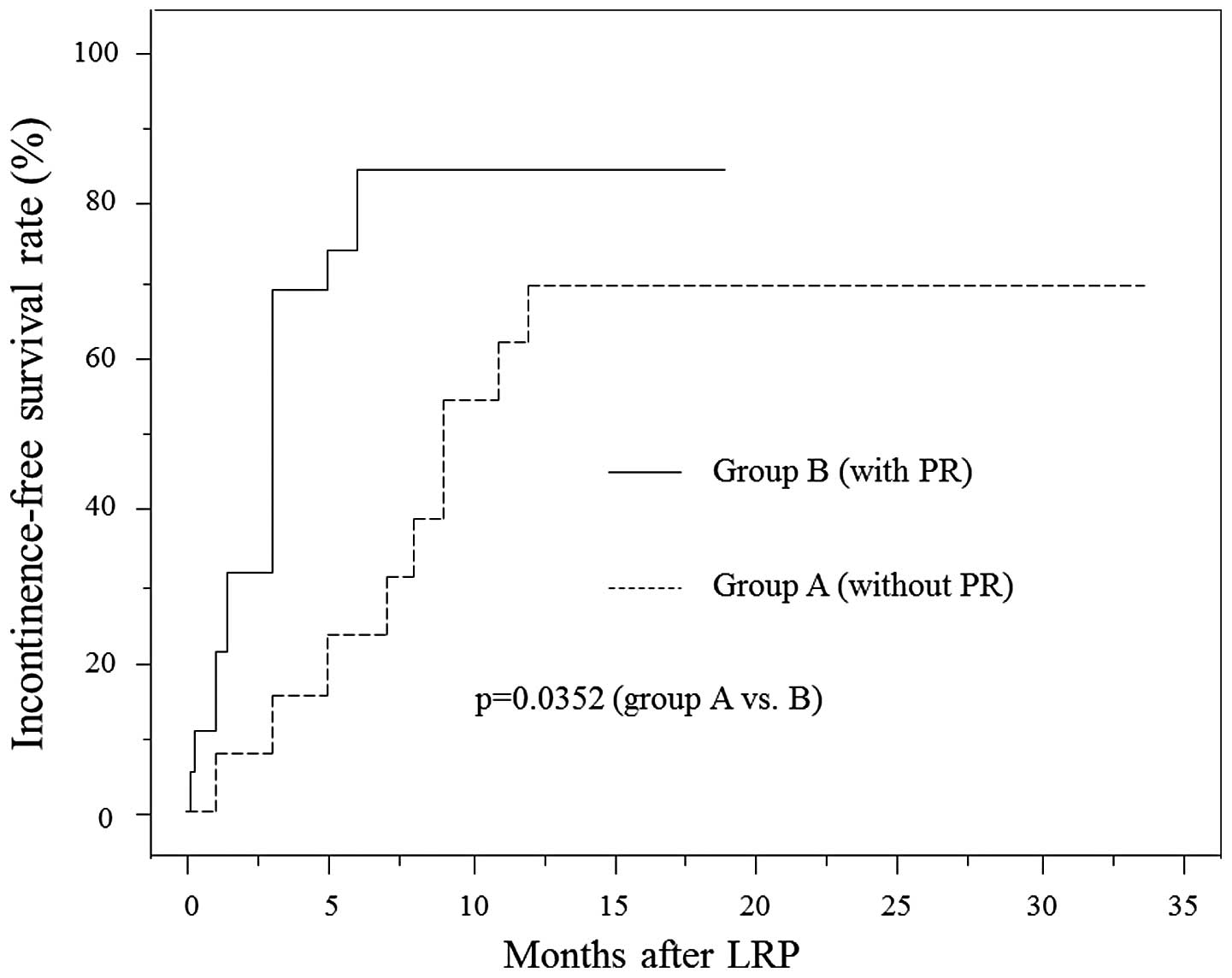
The daily pad usage (number of pads) at 1, 3, 6 and 12 months after
LRP was used to evaluate the recovery of continence and
incontinence-free survival rate was determined by the Kaplan-Meier
method. The urinary function and urinary bother were also evaluated
using the University of California-Los Angeles Prostate Cancer
Index scoring system (16).
 | Table I.Comparison of preoperative background
between groups A and B. |
Table I.
Comparison of preoperative background
between groups A and B.
| Variables | Group A (n=13) | Group B (n=19) | P-value |
|---|
| Age (years) | 66.2±4.5 | 67.1±4.2 | 0.4778a |
| PSA level
(ng/ml) | 7.4±2.1 | 8.4±5.6 | 0.6590a |
| Clinical T stage
(1c/2a/2b/2c) | 4/7/2/0 | 12/4/3/0 | 0.1330b |
| Gleason's grade
(biopsy) | | | 0.4636b |
| 3+3 | 2 | 8 | |
| 3+4 | 7 | 7 | |
| 4+3 | 2 | 2 | |
| 4+4 | 2 | 2 | |
 | Table II.Comparison of perioperative surgical
results between groups A and B. |
Table II.
Comparison of perioperative surgical
results between groups A and B.
| Variables | Group A (n=13) | Group B (n=19) | P-value |
|---|
| Operating time
(min) | 337±67 | 321±29 | 0.9084b |
| Blood lossa (ml) | 1042±1022 | 897±569 | 0.9515b |
| Specimen weight
(g) | 36.0±15.9 | 34.0±12.2 | 0.8479b |
| pT stages
(pT2a/2b/2c/3a/3b) | 3/1/5/3/1 | 3/3/12/1/0 | 0.2945c |
| Gleason sum
(5/6/7/8/9) | 1/0/9/1/2 | 0/5/13/1/0 | 0.0961c |
| Surgical margin
(−/+) | 11/2 | 15/4 | 0.6866c |
| Nerve sparing
(+/−) | 4/9 | 8/11 | 0.5153c |
| Oral food intake
(POD) | 1.6±0.5 | 1.2±0.4 | 0.0302b |
| Catheter removal
(POD) | 8.4±3.0 | 8.2±2.4 | 0.9388b |
| Hospital stay
(POD) | 14.7±3.4 | 13.8±4.1 | 0.4836b |
Statistical analysis
The results are presented as means ± standard
deviation and the values of the variables of the different groups
were compared using the Mann-Whitney U test. The independence of
fit of categorical data was analyzed using the Chi-square test.
Incontinence-free survival curves were constructed using the
Kaplan-Meier method and the differences between these curves were
assessed using the log-rank test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Preoperative factors
The preoperative factors did not differ
significantly between groups A and B (Table I). The only perioperative factor
that differed significantly between the two groups was the time
until the initiation of oral food intake (Table II). The percentage of patients with
leakage of the vesicourethral anastomosis that prevented removal of
the urethral catheter did not differ significantly between groups A
and B (23.1 vs. 33.3%, P>0.05).
Postoperative cystography
The representative postoperative cystograms are
presented in Fig. 3. The L/H ratio
was significantly higher in group B (93.9±11.2%) compared to that
in group A (78.8±14.6%) (P=0.0028) and the PVUA in group B
(117±11°) was significantly narrower compared to that in group A
(129±9°) (P=0.0062). The AVUA in group B (138±10°) appeared to be
narrower compared to that in group A (145±8°), although the
difference was not statistically significant (P= 0.0689).
Recovery of urinary continence
The number of pads used daily was significantly
lower in group B compared to that in group A at 1 month (4.4±2.0
vs. 2.3±2.1, P= 0.0141), 3 months (2.3±1.4 vs. 0.7±1.3, P= 0.0026)
and 6 months (1.1±1.0 vs. 0.3±0.9, P=0.0048) after LRP, but not at
12 months (0.5±0.9 vs. 0.2±0.5, P=0.4778) after LRP. The time
required to achieve a daily pad usage of ≤1 was significantly
shorter in group B compared to that in group A (data not shown). At
12 months after LRP, the percentage of patients with a daily pad
usage of ≤1 was 76.9% in group A and 94.7% in group B. The time
required to achieve a pad-free status (0 pads/day) was
significantly shorter in group B (P=0.0352) (Fig. 4).
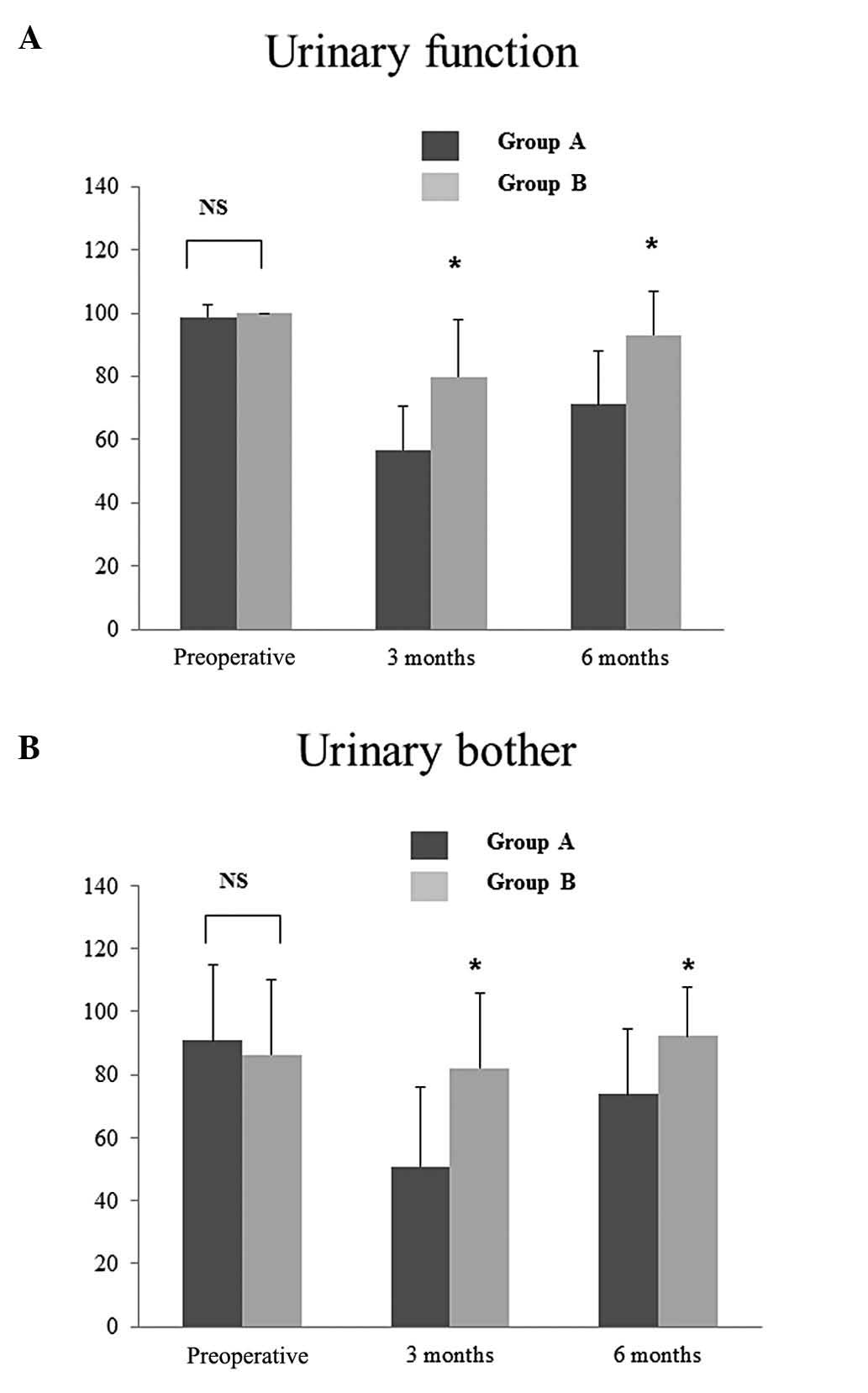
Urinary function and urinary bother
The preoperative urinary function score and the
preoperative urinary bother score did not differ significantly
between the two groups (Fig. 5),
although the urinary function scores at 3 and 6 months after LRP
were significantly higher in group B compared to those in group A
(Fig. 5A) (P=0.0013 at 3 months
and P=0.0007 at 6 months). These urinary function scores appeared
to reflect the daily pad usage at those times. The urinary bother
scores at 3 and 6 months after LRP were significantly higher in
group B compared to those in group A (Fig. 5B) (P=0.0023 at 3 months and
P=0.0061 at 6 months).
Discussion
Achieving early recovery of urinary continence
following radical prostatectomy is crucial and early clinical
studies evaluating continence recovery following LRP reported that
recovery was slower compared to that following RRP (2,3).
Although skilled laparoscopic surgeons have achieved excellent
results regarding urninary continence following LRP, more
experience (number of cases) is generally required to aquire a
stable surgical technique in LRP compared to RRP or robot-assisted
laparoscopic radical prostatectomy (RALP) (17–19).
It is crucial for laparoscopic surgeons to develop simple surgical
procedures that improve urinary continence recovery following LRP.
In the present study, our modified PMPR procedure was added to
previous operative procedures with the intent to expedite
continence recovery and significantly improved urinary continence.
Nguyen et al (7) reported
that their PMPR procedure restored the functional urethral length
and led to early continence recovery. In that study, the functional
urethral length determined by endorectal ultrasonography was
decreased by 12.0–15.6 mm following prostatectomy and PMPR restored
the urethral length by a mean of 2.0 mm in patients undergoing LRP
or RALP. The dorsal aspect of the RS is attached to the RUM
(20). There is fibrous tissue
between the RUM and the dorsal side of the prostatic apex, referred
to as MFR. The DF is connected to the RUM (20) and suturing the DF to the MFR
restores the musculofascial plate. Therefore, the membranous
urethra that lies within the RS is fixed to the musculofascial
plate through the RS. The PMPR recreates the ‘fixation point’,
restores the functional urethral length and may improve sphincteric
function. Rocco and Rocco (21)
also demonstrated the significance of the second layer of the
original Rocco's plate reconstruction and reported that the
functional urethral length may also be improved by the second-layer
stitch and that the external sphincter may be returned to its
original preoperative position.
The development of our modified PMPR procedure was
prompted by two observations regarding the findings in
postoperative cystograms prior to 2010: first, a significant number
of patients undergoing LRP in our institute exhibited a higher
longitudinal length of the bladder (compared to the horizontal
length) in the front-view postoperative cystogram; and second, a
significant number of those patients exhibited a slender
funnel-shaped bladder neck (wide AVUA and PVUA) in the
semilateral-view cystograms. These radiological findings appeared
to be different from those in patients undergoing open RRP. Since
the dissected area around the bladder is likely to be more limited
in a laparoscopic compared to that in an open procedure (due to the
relative lack of blunt dissection) and the bladder is not
particularly mobile, the bladder neck may be difficult to pull down
caudally during vesicourethral anastomosis in LRP, leading to the
slender funnel-shaped bladder neck. Therefore, we hypothesized that
early continence recovery may be achieved if the shape of the
bladder following vesicourethral anastomosis, particularly that of
bladder neck, is improved. When the dorsal upper side of the
bladder is pulled down caudally by suturing the DF to the MFR, the
longitudinal length of the bladder in the front-view cystogram may
be shortened and the PVUA may decrease. Moreover, this procedure
may relieve the anastomotic tension at the vesicourethral
anastomosis. Our PMPR resulted in a lower L/H ratio and a narrower
PVUA, compared to those in patients undergoing LRP without PMPR. In
addition to the previously confirmed restoration of the functional
urethral length by PMPR (7), the
improvement of the PVUA may be one of reasons leading to early
continence recovery. Since the percentage of patients with leakage
from the vesicourethral anastomosis did not differ significantly
between the two groups in the present study, the leakage did not
appear to be associated with continence recovery.
One of the differences between our PMPR and the
Rocco stitch is that we used a running suture to attach the DF to
the MFR. The running suture stabilizes the attachment, making its
rupture unlikely. Coelho et al (22) reported that urinary continence
following RALP may be improved by PMPR using a running suture to
attach the DF to the MFR. In that study, the continence rates at 1
and 4 weeks after RALP were higher in patients with PMPR compared
to those in patients without PMPR. Another difference between our
procedure and Rocco's procedure is the second-layer suture. As
shown in Fig. 2, the bladder was
stitched 1–2 cm dorsocephalad to the bladder neck and the
reconstructed musculofascial plate at the begining of the
vesicourethral anastomosis instead of using the second-layer suture
in Rocco's method. The purpose of this stitch was to approximate
the bladder wall to the MFR 1–2 cm dorsocephalad to the bladder
neck. We hypothesized that this procedure eliminated the need for
Rocco's second-layer stitch, approximated points ‘A’ and ‘B’
(Fig. 2) and simplified the
operative procedure. In the study conducted by Coelho et al
(22), the posterior lip of the
bladder neck (full thickness) and the vesicoprostatic muscle
(23) were sutured to the
posterior urethral edge and the reconstructed median raphe. The
procedure described in that study is similar to ours.
In the present study, urinary continence was
recovered earlier in patients with compared to those without PMPR,
despite the similar clinical backgrounds and perioperative factors
of the two groups. Since we did not modify other surgical
procedures intented to improve continence recovery, our PMPR
procedure appeared to exert a significant effect on the recovery of
urinary continence. Previous studies reported that PMPR improves
the recovery of urinary continence (7–10,22).
In RALP, however, PMPR was not identified as an independent
predictor of the early recovery of urinary continence in a
multivariate analysis (14). Sano
et al (24) suggested that
the magnified stereoscopic view and maneuverable instruments in
RALP may allow for the preservation of the sphincteric/supporting
musculature and, therefore, that PMPR may not be an independent
factor in the multivariate analysis. The authors of that study also
suggested that plate reconstruction may be beneficial for early
continence recovery following standard LRP in a community hospital
(i.e., without the extensive fascia preservation possible in RALP).
In addition, the percentage of patients with NVB preservation is
high among RALP cases (14). Nerve
preservation is reportedly a significant factor contributing to
early continence recovery (25,26).
The high rate of nerve preservation may be one of reasons due to
which PMPR is not an independent predictor for the early continence
recovery following RALP. In our cases, a nerve-sparing procedure
was performed in 37.5% of the patients (bilateral, 3.1% and
unilateral, 34.4%) and the percentage of nerve preservation was
similar between groups A and B.
This study has several weak points. First, it is a
non-randomized retrospective study conducted in a single institute.
Second, the study spanned five years, during which time it is
possible that the surgeon's surgical skills improved significantly.
However, LRP was initiated in our institute in 2000 and the surgeon
started performing LRPs as a main operator in 2004. Therefore, it
is likely that the surgical skills had already become stable by
2008. Third, the patient sample was limited and more patients
undergoing LRP with our method should be evaluated to confirm our
results. The evaluation of postoperative cystograms indicated that
the improvement in the PVUA is a possible reason for the improved
continence recovery associated with our PMPR procedure.
In conclusion, although several factors contribute
to the recovery of urinary continence, our PMPR procedure combined
with the modification of the vesicourethral anastomosis, was shown
to improve the PVUA and exert a positive effect on the recovery of
urinary continence following LRP.
References
|
1.
|
Guillonneau B, Cathelineau X, Barret E,
Rozet F and Vallancien G: Laparoscopic radical prostatectomy:
technical and early oncological assessment of 40 operations. Eur
Urol. 36:14–20. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Egawa S, Arai Y, Kawakita M, Matsuda T, et
al: Surgical outcome of laparoscopic radical prostatectomy: summary
of early multiinstitutional experience in Japan. Int J Clin Oncol.
8:97–103. 2003. View Article : Google Scholar
|
|
3.
|
Namiki S, Egawa S, Baba S, et al: Recovery
of quality of life in year after laparoscopic or retropubic radical
prostatectomy: a multi-institutional longitudinal study. Urology.
65:517–523. 2005.
|
|
4.
|
Azuma H, Ibuki N, Inamoto T, et al:
Utility of transrectal ultrasonography guidance and seven key
elements of operative skill for early recovery of urinary
continence after laparoscopic radical prostatectomy. Int J Oncol.
38:293–304. 2011. View Article : Google Scholar
|
|
5.
|
Curto F, Benijts J, Pansadoro A, et al:
Nerve sparing laparoscopic radical prostatectomy: our technique.
Eur Urol. 49:344–352. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Coakley FV, Eberhardt S, Kattan MW, Wei
DC, Scardino PT and Hricak H: Urinary continence after radical
retropubic prostatectomy: relationship with membranous urethral
length on preoperative endorectal magnetic resonance imaging. J
Urol. 168:1032–1035. 2002. View Article : Google Scholar
|
|
7.
|
Nguyen L, Jhaveri J and Tewari A: Surgical
technique to overcome anatomical shortcoming: balancing
post-prostatectomy continence outcomes of urethral sphincter
lengths on preoperative magnetic resonance imaging. J Urol.
179:1907–1911. 2008. View Article : Google Scholar
|
|
8.
|
Rocco F, Carmignani L, Acquati P, et al:
Restoration of posterior aspect of rhabdosphincter shortens
continence time after radical retropubic prostatectomy. J Urol.
175:2201–2206. 2006. View Article : Google Scholar
|
|
9.
|
Rocco B, Gregori A, Stener S, et al:
Posterior reconstruction of the rhabdosphincter allows a rapid
recovery of continence after transperitoneal videolaparoscopic
radical prostatectomy. Eur Urol. 51:996–1003. 2007. View Article : Google Scholar
|
|
10.
|
Rocco F, Carmignani L, Acquati P, et al:
Early continence recovery after open radical prostatectomy with
restoration of the posterior aspect of the rhabdosphincter. Eur
Urol. 52:376–383. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Noguchi M, Kakuma T, Suekane S, Nakashima
O, Mohamed ER and Matsuoka K: A randomized clinical trial of
suspension technique for improving early recovery of urinary
continence after radical retropubic prostatectomy. BJU Int.
102:958–963. 2008. View Article : Google Scholar
|
|
12.
|
Tewari A, Jhaveri J, Rao S, et al: Total
reconstruction of the vesico-urethral junction. BJU Int.
101:871–877. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Sasaki H, Miki J, Kimura T, et al: Lateral
view dissection of the prostato-urethral junction to reduce
positive apical margin in laparoscopic radical prostatectomy. Int J
Urol. 16:664–669. 2009. View Article : Google Scholar
|
|
14.
|
Menon M, Muhletaler F, Campos M and
Peabody JO: Assessment of early continence after reconstruction of
the periprostatic tissues in patients undergoing computer assisted
(robotic) prostatectomy: results of a 2 group parallel randomized
controlled trial. J Urol. 180:1018–1023. 2008. View Article : Google Scholar
|
|
15.
|
Ozu C, Hagiuda J, Nakagami Y, et al:
Radical retropubic prostatectomy with running vesicourethral
anastomosis and early catheter removal: our experience. Int J Urol.
16:487–492. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Kakehi Y, Kamoto T, Ogawa O, et al:
Development of Japanese version of the UCLA Prostate Cancer Index:
a pilot validation study. Int J Clin Oncol. 7:306–311.
2002.PubMed/NCBI
|
|
17.
|
Guillonneau B, Rozet F, Barret E,
Cathelineau X and Vallancien G: Laparoscopic radical prostatectomy:
assessment after 240 procedures. Urol Clin North Am. 28:189–202.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Kavoussi LR: Laparoscopic radical
prostatectomy: irrational exuberance? Urology. 58:503–505. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Ahlering TE, Skarecky D, Lee D and Clayman
RV: Successful transfer of open surgical skills to a laparoscopic
environment using a robotic interface: initial experience with
laparoscopic radical prostatectomy. J Urol. 170:1738–1741. 2003.
View Article : Google Scholar
|
|
20.
|
Soga H, Takenaka A, Murakami G and
Fujisawa M: Topographical relationship between urethral
rhabdosphincter and rectourethralis muscle: a better understanding
of the apical dissection and the posterior stitches in radical
prostatectomy. Int J Urol. 15:729–732. 2008. View Article : Google Scholar
|
|
21.
|
Rocco B and Rocco F: Re: Assessment of
early continence after reconstruction of the periprostatic tissues
in patients undergoing computer assisted (robotic) prostatectomy:
results of a 2 group parallel randomized controlled trial: M.
Menon, F. Muhletaler, M. Campos and J. O. Peabody. J Urol.
2008.180:1018–1023, J Urol 181: 1500–1501; author reply 1501,
2009.
|
|
22.
|
Coelho RF, Chauhan S, Orvieto MA, et al:
Influence of modified posterior reconstruction of the
rhabdosphincter on early recovery of continence and anastomotic
leakage rates after robot-assisted radical prostatectomy. Eur Urol.
59:72–80. 2011. View Article : Google Scholar
|
|
23.
|
Walz J, Burnett AL, Costello AJ, et al: A
critical analysis of the current knowledge of surgical anatomy
related to optimization of cancer control and preservation of
continence and erection in candidates for radical prostatectomy.
Eur Urol. 57:179–192. 2010. View Article : Google Scholar
|
|
24.
|
Sano T, Nakashima M, Haitani T, Kajita Y
and Shichiri Y: Posterior musculofascial plate reconstruction
promotes early restoration of continence and prevents severe
incontinence in patients undergoing laparoscopic radical
prostatectomy. Int J Urol. 19:475–479. 2012. View Article : Google Scholar
|
|
25.
|
Burkhard FC, Kessler TM, Fleischmann A,
Thalmann GN, Schumacher M and Studer UE: Nerve sparing open radical
retropubic prostatectomy - does it have an impact on urinary
continence? J Urol. 176:189–195. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Nandipati KC, Raina R, Agarwal A and Zippe
CD: Nerve-sparing surgery significantly affects long-term
continence after radical prostatectomy. Urology. 70:1127–1130.
2007. View Article : Google Scholar
|