Introduction
Squamous cell carcinoma (SCC) is the most frequent
malignant tumour of the head and neck region (1,2).
Funk et al (3) reported
that SCC accounts for 86.3% of head and neck malignancies. Uncommon
malignancies, such as malignant lymphoma (4), adenoid cystic carcinoma (ACC)
(5,6), adenocarcinoma (7) and mucoepidermoid carcinoma (8,9) are
also found in the head and neck region; however, these tumours
account for <5% of the total cases (2).
The rarity of these non-SCCs has prevented the
implementation of evidence-based clinical improvements in their
treatment. The number of malignant tumours has been hypothesized to
increase in conjunction with the progression of medical science
(10). Therefore, it is essential
to expand our understanding of non-SCCs to improve their
prognosis.
The aim of the present study was to investigate the
clinical characteristics of non-SCCs in the head and neck region in
order to improve clinical outcomes.
Materials and methods
Cases
Primary cases of malignant tumours in the head and
neck region treated at the Division of Dentistry and
Oral-Maxillofacial Surgery, Chiba University Hospital, between
January, 1995 and December, 2010, were retrospectively
investigated. All the cases were biopsied for diagnosis by
pathologists and classified according to the World Health
Organization guidelines (1). The
cases were divided into two groups: SCCs and non-SCCs.
Clinicopathological characteristics, including age, gender, primary
lesion site, pathological diagnosis, TNM classification, treatment,
distant metastasis and outcome were retrospectively analyzed using
patient medical records to determine the clinical characteristics
of non-SCCs.
Statistical analysis
The statistical analyses for distant metastasis in
cases of ACC or clinical outcome associated with surgery were
performed using the Fisher’s exact test. The overall survival rate
was assessed using the Kaplan-Meier analysis and the difference was
analyzed using the log-rank test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Patient characteristics
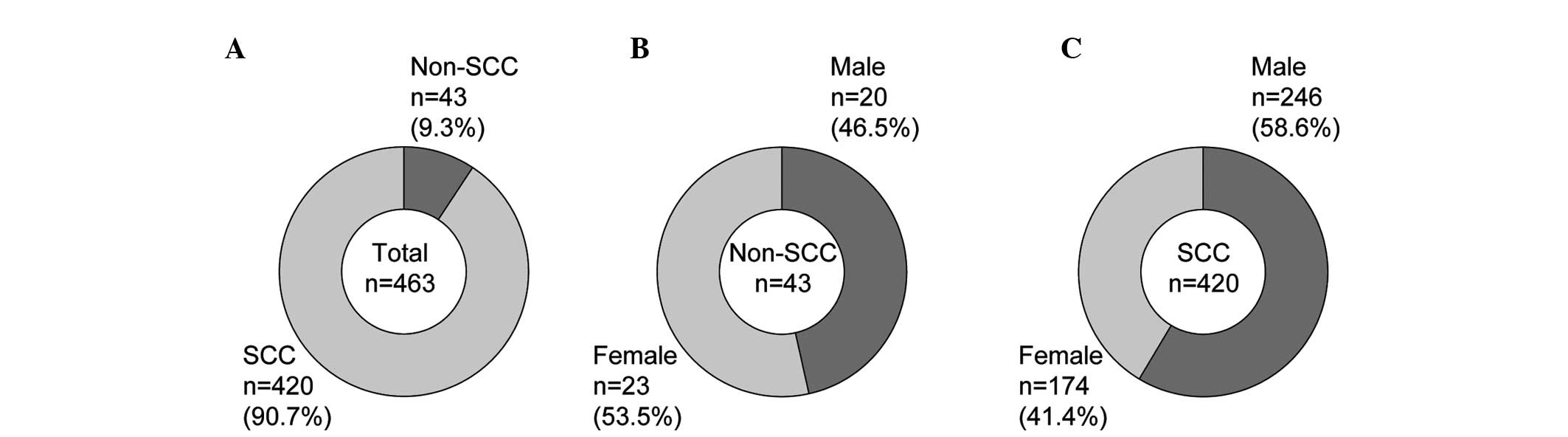
A total of 463 patients were included in this study,
of whom 266 were men and 197 were women. The average age of the men
was 61.6 years (range, 13–85 years) and that of the women 62.1
years (range, 29–94 years). In total, 43 cases (9.3%) were
confirmed as non-SCC (Fig. 1A). Of
the non-SCC cases, 20 (46.5%) were male (Fig. 1B) and the overall average age at
the first visit was 61.8 years (range, 13–92 years). Of the 420 SCC
cases, 246 (58.6%) were male (Fig.
1C) and the average age was 66.2 years (range, 21–94 years).
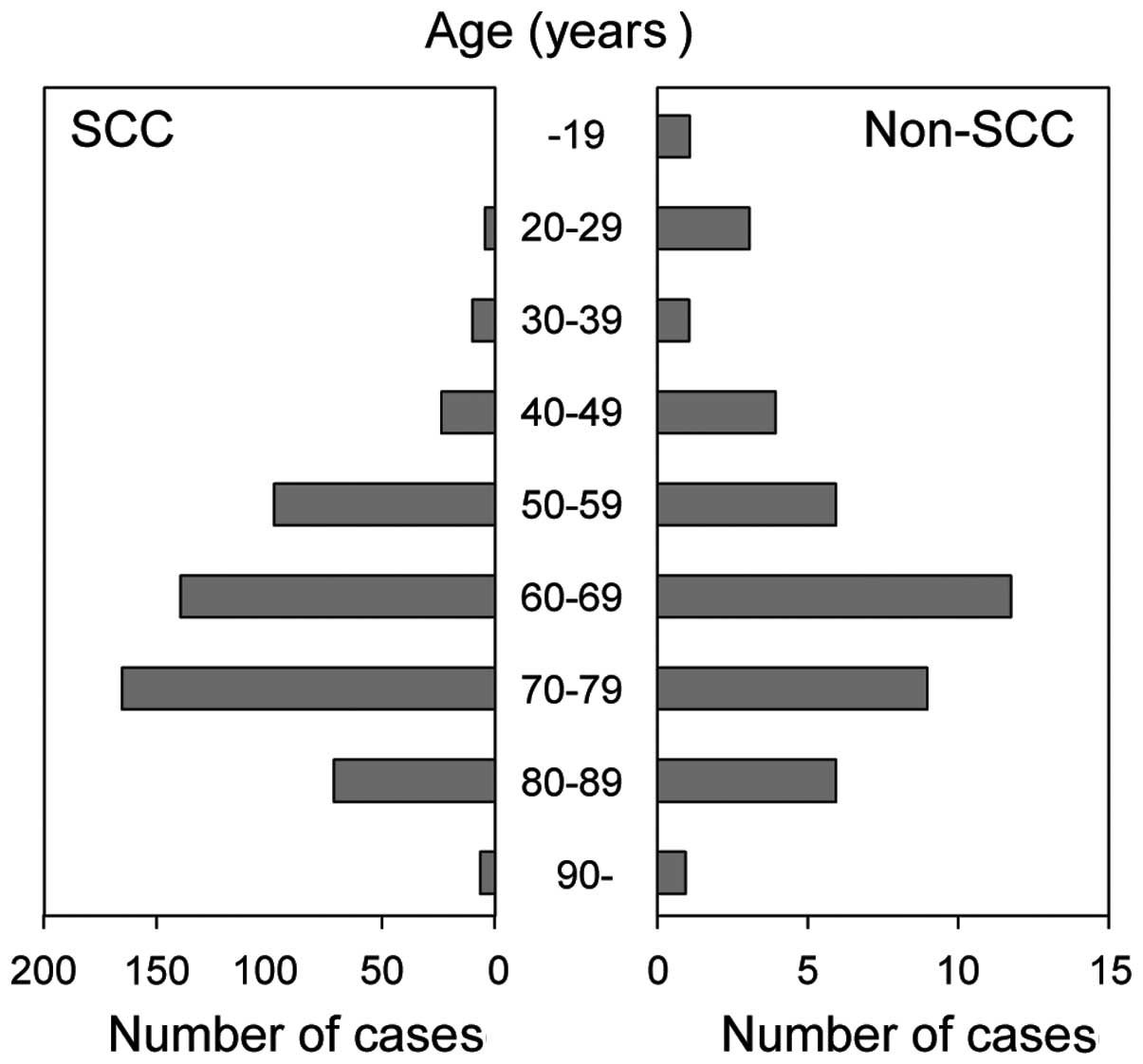
The age distribution analysis revealed that a higher number of SCC
patients were in the age range of 50–80 years. However, the non-SCC
group included younger patients (aged <30 years) as well as
older patients (Fig. 2). These
data indicate that the non-SCC group included more women compared
to the SCC group and that there is a wider age distribution trend
in the non-SCC compared to the SCC group.
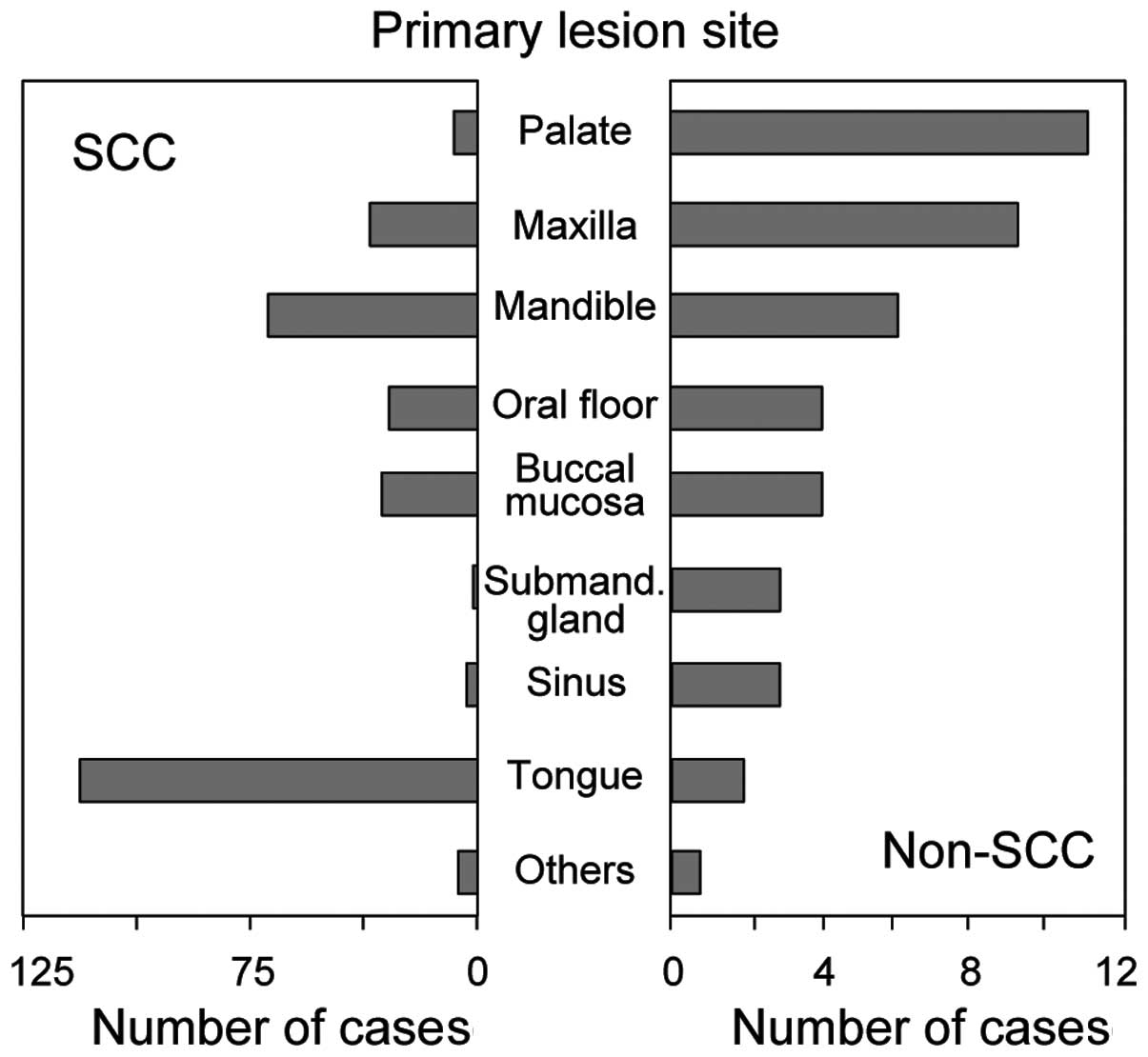
Among the SCC cases, the tongue was the most
frequent primary site, followed by the mandible. However, non-SCCs
occurred most frequently in the palate and maxilla (Fig. 3).
Pathological classification
The pathological classification revealed that ACC
(14 cases) and haematolymphoid tumours (16 cases) were the most
frequently encountered malignancies (Table I). Less frequent neoplasms included
mucoepidermoid carcinoma (2 cases), basal cell adenocarcinoma (1
case), adenocarcinoma (1 case), malignant ameloblastoma (1 case),
small-cell carcinoma (1 case), mucosal malignant melanoma (4
cases), rhabdomyosarcoma (2 cases) and synovial sarcoma (1 case).
Patients with haematolymphoid tumours were referred to the Division
of Internal Medicine for treatment. Therefore, ACC was the most
frequently encountered non-SCC malignancy treated at our
Department.
 | Table IList of non-squamous cell carcinomas
investigated in the present study. |
Table I
List of non-squamous cell carcinomas
investigated in the present study.
| Pathological
classification | No. of cases | 5-year survival,
n/totala (%) | Incidence of distant
metastasis, n/total (%) |
|---|
| Salivary gland
carcinomas |
| Adenoid cystic
carcinoma | 14 | 8/11 (73) | 9/14 (64) |
| Mucoepidermoid
carcinoma | 2 | 2/2 (100) | 0/2 (0) |
| Adenocarcinoma | 1 | 0/1 (0) | 1/1 (100) |
| Basal cell
adenocarcinoma | 1 | 1/1 (100) | 0/1 (0) |
| Odontogenic
carcinoma |
| Malignant
ameloblastoma | 1 | 1/1 (100) | 0/1 (0) |
| Neuroendocrine
tumors |
| Small-cell
carcinoma, neuroendocrine type | 1 | 0/1 (0) | 1/1 (100) |
| Haematolymphoid
tumors |
| Diffuse large B-cell
lymphoma | 10 | 4/8 (50) | -b |
| Extranodal marginal
zone B-cell lymphoma of MALT | 2 | 2/2 (100) | - |
| Extranodal NK/T-cell
lymphoma | 2 | 2/2 (100) | - |
| Anaplastic
large-cell lymphoma | 1 | 1/1 (100) | - |
| Plasmacytoma | 1 | 0/0 | - |
| Mucosal malignant
melanoma | 4 | 2/4 (50) | 4/4 (100) |
| Soft tissue
tumors |
|
Rhabdomyosarcoma | 2 | 0/2 (0) | 2/2 (100) |
| Synovial
sarcoma | 1 | 0/1 (0) | 0/1 (0) |
| Total | 43 | 22/33 (67) | |
Treatment and outcomes
Surgery was mainly selected as the primary
treatment, except for malignant lymphoma, with chemotherapy or
radiotherapy administered as necessary. Conversely, malignant
lymphoma was mainly treated with chemotherapy and/or radiotherapy
(Table II). In cases with local
recurrence or distant metastasis, additional surgery, chemotherapy
and/or radiotherapy were administered.
 | Table IITherapeutic approach in the primary
treatment. |
Table II
Therapeutic approach in the primary
treatment.
| No. of therapies for
primary lesion |
|---|
|
|
|---|
| Type of tumor | S | S+C | S+R | S+C+R | C | R | C+R |
|---|
| Salivary gland
carcinomas (n=17)a | 13 | 0 | 3 | 1 | 0 | 0 | 0 |
| Malignant
ameloblastoma (n=1) | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Small-cell carcinoma
(n=1) | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| Haematolymphoid
tumors (n=16) | 1 | 0 | 1 | 1 | 7 | 3 | 3 |
| Mucosal malignant
melanoma (n=4) | 0 | 1 | 0 | 1 | 1 | 0 | 1 |
| Soft tissue tumors
(n=3) | 1 | 0 | 0 | 1 | 1 | 0 | 0 |
The correlation between surgical treatment and
outcome was analyzed in non-SCC cases, except for malignant
lymphoma. Four patients did not undergo surgery and they all
succumbed to the disease within 5 years (Table III). Conversely, 14 of the 19
patients (74%) who underwent surgery survived for >5 years. The
5-year survival rate was significantly higher among patients who
underwent surgery compared to those who did not (P=0.014) (Table IV).
 | Table IIIComparison of 5-year survival rate
between non-squamous cell carcinomas patients treated with and
without surgery. |
Table III
Comparison of 5-year survival rate
between non-squamous cell carcinomas patients treated with and
without surgery.
| 5-year survived
patients |
|---|
|
|
|---|
| Pathological
classification | Surgery, n/total
(%) | No surgery, n/total
(%) |
|---|
| Adenoid cystic
carcinoma | 0/1 (0) | 8/10 (80) |
| Mucoepidermoid
carcinoma | None | 2/2 (100) |
| Basal cell
adenocarcinoma | None | 1/1 (100) |
| Adenocarcinoma | None | 0/1 (0) |
| Malignant
ameloblastoma | None | 1/1 (100) |
| Small-cell
carcinoma | None | 0/1 (0) |
| Mucosal malignant
melanoma | 0/2 (0) | 2/2 (100) |
| Sarcoma | 0/1 (0) | 0/1 (0) |
| Total | 0/4 (0) | 14/19 (74) |
 | Table IVComparison of outcome between primary
treatment with and without surgery in non-squamous cell carcinomas,
excluding malignant lymphoma. |
Table IV
Comparison of outcome between primary
treatment with and without surgery in non-squamous cell carcinomas,
excluding malignant lymphoma.
| Surgery |
|---|
|
|
|---|
| Outcome | Yes | No | P-value |
|---|
| Surviveda | 14 | 0 | 0.014b |
| Deceased | 5 | 4 | |
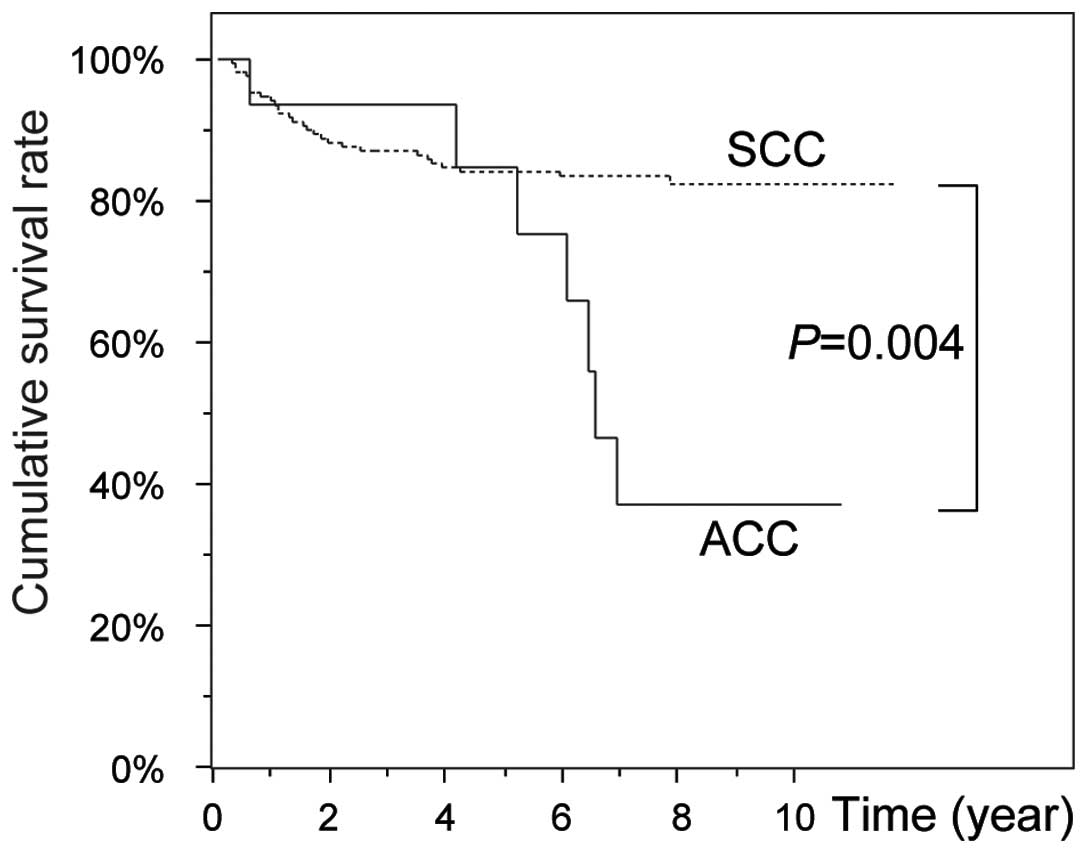
The 5-year survival rates were ≤50% for patients
with adenocarcinoma, small-cell carcinoma, mucosal malignant
melanoma, rhabdomyosarcoma and synovial sarcoma (Table I).
Salivary gland carcinomas
One ACC patient refused treatment. The remaining 13
ACC patients underwent surgery and additionally received
radiotherapy or chemotherapy, as required. Among the 5 surviving
ACC patients, 2 have survived for >5 years, while 6 of the 9
deceased ACC patients survived for >5 years after treatment.
Thus, 8 of the 11 cases (73%) remained alive at the 5-year
observation time point (Table I).
Subsequently, the survival rate decreased significantly, resulting
in a 10-year cumulative survival rate of 38% (Fig. 4). The cumulative survival rates at
the 5-year observation time point between ACC and SCC patients were
similar. However, the subsequent decrease in the ACC was more
noticeable compared to the decrease in the SCC survival rate
(P=0.004; Fig. 4).
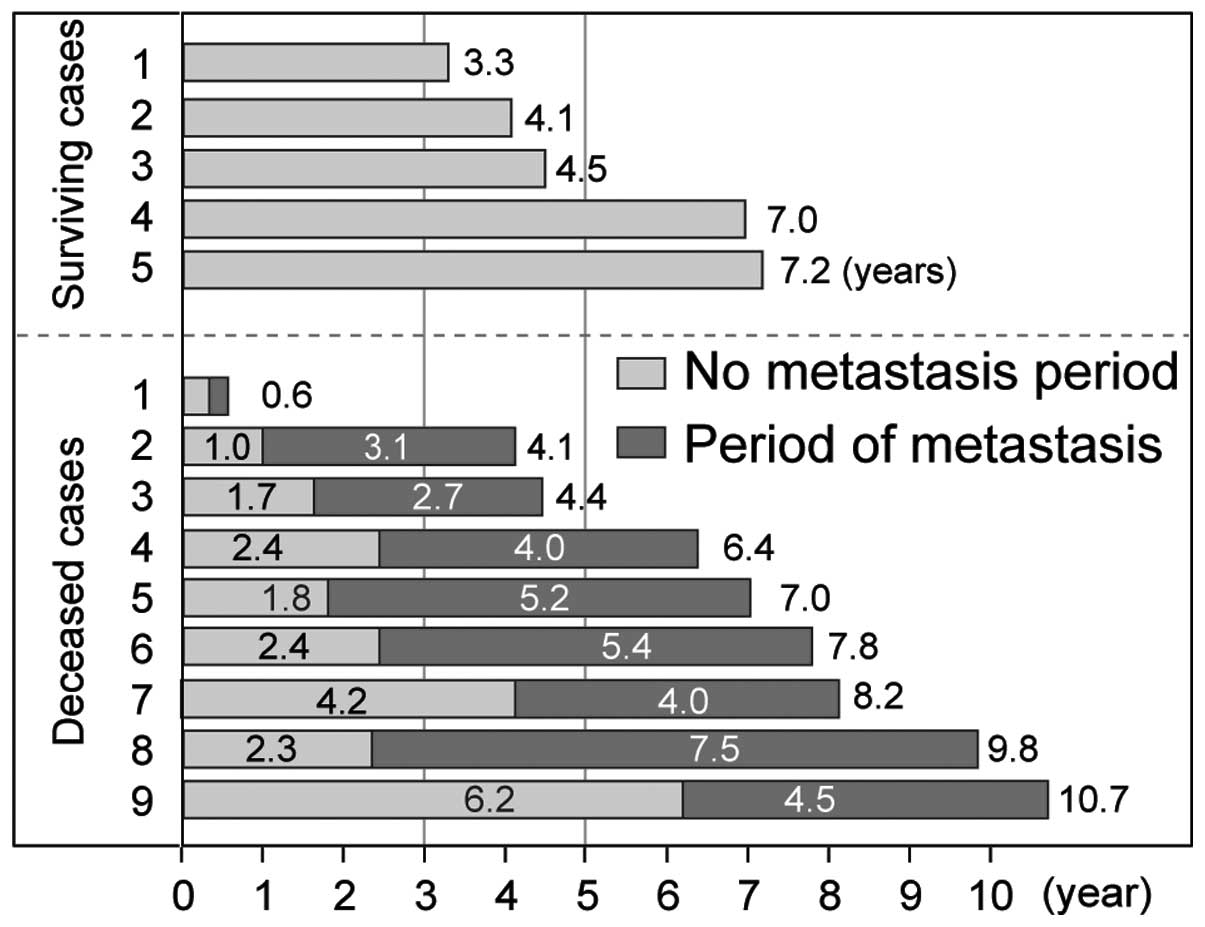
Distant metastasis was not observed in any of the
surviving patients. Distant metastases were observed in 9 of the 14
ACC cases, 6 of which occurred within 3 years following primary
treatment (Fig. 5). Lung
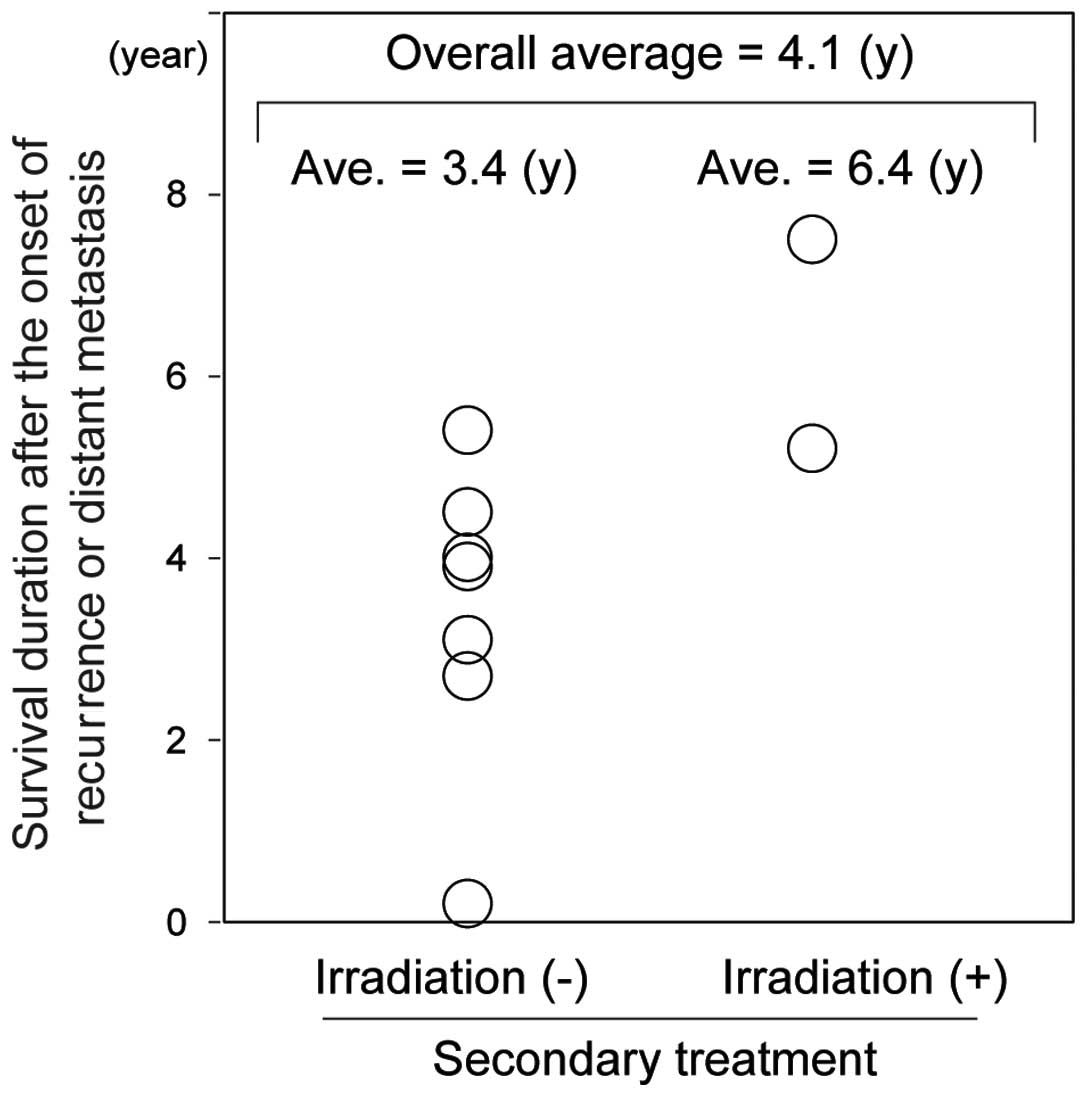
metastasis occurred in all patients with metastasis (Table V). The overall average survival
duration following local recurrence or distant metastasis was 4.1
years and the survival duration was 3.4 and 6.4 years when treated
with and without radiotherapy, respectively (Fig. 6). Distant metastasis was observed
in 22 of the 420 SCC patients; thus, ACC exhibited a significantly
higher incidence of distant metastasis compared to SCC (P<0.001)
(Table VI). The ACC patient
information is summarized in Table
VII to clarify the association between clinicopathological
factors and distant metastasis. The data demonstrated that the
distant metastasis rate was significantly higher in T3+T4 when
compared to that in T1+T2 cases (P=0.021). In addition, distant
metastasis occurred in all the patients who experienced regional
lymph node metastasis. Distant metastasis was frequently observed
in the sinus (100%), submandibular gland (100%) and oral floor
(75%), but was comparably rare in the palate (33%) (Table VII). There was no significant
association between distant metastasis and histological type.
 | Table VSummary of adenoid cystic carcinoma
cases. |
Table V
Summary of adenoid cystic carcinoma
cases.
| Case | Gender (age) | Primary lesion
site | TNM
classification | Type | Treatment | Distant metastasis
(years) | Outcome
(years) |
|---|
|
|---|
| Primary | Secondary |
|---|
| 1 | M (85) | Oral floor | T2N0M0 | T+Cr | S (resection) | No | No | A (3.3) |
| 2 | F (49) | Palate | T2N0M0 | T | S (resection +
ND) | No | No | A (4.1) |
| 3 | F (64) | Palate | T1N0M0 | T | S (resection +
ND) | No | No | A (4.5) |
| 4 | F (53) | Palate | T1N0M0 | Sol | S (resection +
ND) | No | No | A (7.0) |
| 5 | M (71) | Palate | T1N0M0 | T+Cr | S (resection +
ND) | No | No | A (7.2) |
| 6 | F (40) | Sinus | T4N0M0 | Sol | S (resection + ND)
+ R (66 Gy) | C (5FU + CDDP) | Lung, liver
(0.3) | D (0.6) |
| 7 | F (64) | Palate | T4N0M0 | T+Cr | S (resection + ND)
+ C (CDDP) + R (66 Gy) | C (docetaxel +
5FU) | Lung (1.0) | D (4.1) |
| 8 | F (67) | Oral floor | T2N0M0 | T+Cr | Refusal | Refusal | Lung (1.6) | D (4.4) |
| 9 | M (58) | Oral floor | T2N0M0 | T | S (resection +
ND) | C (CDDP + 5FU) | Lung (2.4) | D (6.4) |
| 10 | F (48) | Sinus | T3N1M0 | T | S (resection +
ND) | C (CDDP +
docetaxel) + R (64.8Gy) | Lung, vertebrae
(1.8) | D (7.0) |
| 11 | F (28) | Submand. gland | T4N2M0 | Cr | S (resection + ND)
+ R (66 Gy) | C (CDDP + 5FU) | Lung (2.4) | D (7.8) |
| 12 | M (34) | Oral floor | T3N1M0 | T | S (resection +
ND) | S (neumonectomy) +
C (CDDP + 5FU) | Lung, brain
(4.2) | D (8.2) |
| 13 | M (67) | Submand. gland | T4N0M0 | Cr | S (resection +
ND) | S (neumonectomy) +
R (50 Gy) | Lung (2.3) | D (9.8) |
| 14 | F (55) | Palate | T3N0M0 | Sol | S (resection + ND)
+ R (66 Gy) | C (cetuximab + 5FU
+ CDDP) | Lung (6.2) | D (10.7) |
 | Table VIComparison of distant metastasis
incidence between adenoid cystic carcinoma and squamous cell
carcinoma. |
Table VI
Comparison of distant metastasis
incidence between adenoid cystic carcinoma and squamous cell
carcinoma.
| Pathological
classification | Distant
metastasis | P-value |
|---|
|
|---|
| Yes | No |
|---|
| Adenoid cystic
carcinoma | 9 | 5 | <0.001a |
| Squamous cell
carcinoma | 22 | 398 | |
 | Table VIICorrelation of clinicopathological
factors with distant metastasis in adenoid cystic carcinoma. |
Table VII
Correlation of clinicopathological
factors with distant metastasis in adenoid cystic carcinoma.
| Distant
metastasis | |
|---|
|
| |
|---|
| Clinical
factors | Yes (%) | No (%) | P-valuea |
|---|
| TNM
classification |
| T: T1 (n=3) | 0 (0) | 3 (100) | |
| T2 (n=4) | 2 (50) | 2 (50) | |
| T3 (n=3) | 3 (100) | 0 (0) | |
| T4 (n=4) | 4 (100) | 0 (0) | |
| T1+T2 (n=7) | 2 (29) | 5 (71) | 0.021b |
| T3+T4 (n=7) | 7 (100) | 0 (0) | |
| N: N0 (n=11) | 6 (55) | 5 (45) | 0.258c |
| N1+N2 (n=3) | 3 (100) | 0 (0) | |
| Primary lesion
site |
| Oral floor
(n=4) | 3 (75) | 1 (25) | |
| Sinus (n=2) | 2 (100) | 0 (0) | |
| Submandibular
gland (n=2) | 2 (100) | 0 (0) | |
| Palate (n=6) | 2 (33) | 4 (67) | |
| Histological
type |
| Tubular (n=5) | 3 (60) | 2 (40) | |
| Tubular/cribriform
(n=4) | 2 (50) | 2 (50) | |
| Cribriform
(n=2) | 2 (100) | 0 (0) | |
| Solid (n=3) | 2 (67) | 1 (33) | |
In addition, there were 2 cases of mucoepidermoid
carcinoma, 1 advanced case of adenocarcinoma and 1 case of basal
cell adenocarcinoma. The 2 cases with mucoepidermoid carcinoma were
treated with surgery, including neck dissection, and the patients
have remained alive for 7 and 11 years, respectively, with no
evidence of recurrence or metastasis (Table VIII). The advanced
adenocarcinoma case was staged as T3N2bM0 (Table VI). The patient underwent surgical
tumour resection and neck dissection. Additional treatments, such
as adjuvant chemotherapy and radiotherapy were planned; however,
neither was administered due to the patient’s poor overall
condition. After 8 months, multiple lymph node metastases were
detected in the neck. The patient did not consent to further
treatment and eventually succumbed to the disease 17 months after
her first visit.
 | Table VIIISummary of uncommon malignancies. |
Table VIII
Summary of uncommon malignancies.
| Cases | Gender (age) | Primary lesion
site | TNM
classification | Treatment | Distant
metastasis | Outcome
(years) |
|---|
|
|---|
| Primary | Secondary |
|---|
| Mucoepidermoid
carcinoma | F (54) | Mandible | T2N0M0 | S (resection +
ND) | No | No | A (7.9) |
| Mucoepidermoid
carcinoma | F (68) | Buccal mucosa | T2N0M0 | S (resection +
ND) | No | No | A (9.9) |
| Basal cell
adenocarcinoma | M (66) | Buccal mucosa | T2N0M0 | S (resection +
ND) | No | No | A (7.1) |
| Adenocarcinoma | F (84) | Tongue | T3N2bM0 | S (resection +
ND) | No | No | D (1.4) |
| Malignant
ameloblastoma | M (55) | Mandible | T3N0M0 | S (resection) | S (resection +
ND) | No | A (13.0) |
| Small-cell
carcinoma, neuroendocrine type | M (65) | Maxilla | T3N0M0 | S (resection + ND)
+ C (PI+PE) + R (66 Gy) | S (resection) | Supraclavicular
fossa, underam (0.9 years) | D (1.4) |
Haematolymphoid tumours
Three patients underwent surgery, were diagnosed
with malignant lymphoma and were referred to the Internal Medicine
Department. For the other malignant lymphoma cases, biopsy or image
analyses were used for diagnosis and the patients were directly
referred to Internal Medicine. All the malignant lymphoma cases
were non-Hodgkin lymphomas, with 13 cases of B-cell neoplasms and 3
cases of natural killer or T-cell (NK/T) neoplasms (Table IX). Chemotherapy or radiotherapy
was the main therapeutic option for patients with malignant
lymphoma (Tables II and IX). At the 5-year observation time
point, 5 of the 11 malignant lymphoma cases (45%) had survived
(Table I). The median observation
period for surviving patients and the survival period for deceased
patients were 6.0 and 3.6 years, respectively. Of the NK/T-cell
lymphoma patients, 2 succumbed to the disease and 1 has remained
alive for 5 years without recurrence. The surviving NK/T-cell
lymphoma patient is a 28-year-old woman who was treated with
radiotherapy (50 Gy) and 3 courses of dexamethasone, etoposide,
ifosfamide and carboplatin (DeVIC).
 | Table IXSummary of haematolymphoid
tumors. |
Table IX
Summary of haematolymphoid
tumors.
| Cases | Gender (age) | Lesion site | Pathological
diagnosis | Pathological
classification | Treatment | Outcome | Observation
period/survival period (years) |
|---|
| 1 | M (71) | Upper gingiva | DLBCL | B | C | Alive | 4.3 |
| 2 | M (81) | Sinus | DLBCL | B | C+R | Alive | 6.1 |
| 3 | M (20) | Lower | DLBCL | B | C+R | Alive | 5.9 |
| 4 | F (92) | Submandibular | DLBCL | B | C | Alive | 8.9 |
| 5 | F (69) | Lower gingiva | DLBCL | B | S+C+R | Alive | 8.6 |
| 6 | F (61) | Palate | DLBCL | B | C | Alive | 1.1 |
| 7 | M (84) | Maxilla | DLBCL | B | R | Deceased | 1.1 |
| 8 | F (54) | Upper gingiva | DLBCL | B | C | Deceased | 1.2 |
| 9 | F (45) | Lower gingiva | DLBCL | B | C | Deceased | 1.8 |
| 10 | F (84) | Maxilla | DLBCL | B | C | Deceased | 1.5 |
| 11 | F (83) | Palate | MALT lymphoma | B | R | Alive | 5.1 |
| 12 | F (73) | Oral floor | MALT lymphoma | B | R | Alive | 12.0 |
| 13 | M (71) | Mandible | Plasmacytoma | B | S | Alive | 3.0 |
| 14 | F (28) | Upper gingiva | Extranodal
NK/T-cell lymphoma (nasal type) | NK/T | C+R | Alive | 5.3 |
| 15 | M (74) | Palate | Extranodal
NK/T-cell lymphoma (nasal type) | NK/T | C | Deceased | 7.3 |
| 16 | M (75) | Maxilla | ALCL | NK/T | S+R | Deceased | 8.6 |
Other malignancies
A case of small-cell carcinoma (neuroendocrine type)
was treated by surgery (tumour resection and neck dissection) and
concurrent chemoradiotherapy, which comprised 5 courses of
cisplatin + etoposide (PE) and 1 course of cisplatin + irinotecan
(PI), with 66 Gy of radiotherapy (Table VIII). This malignancy is common
in the lung but extremely rare in the head and neck region
(11,12). Since PE and PI are considered to be
the standard treatment for SCC of the lung, they were selected for
this case. However, the patient succumbed to the disease 18 months
after his first visit.
In total, 4 cases of malignant melanoma were treated
(Table X). All the patients
succumbed to the disease at 2, 3, 8 and 10 years after diagnosis.
The 2 patients who survived the longest had undergone tumour
resection with regional neck dissection, combined with chemotherapy
or concurrent chemoradiotherapy. Surgical treatment was suggested
to the remaining 2 patients, who experienced a shorter survival.
However, both patients refused surgery and opted for chemotherapy
or concurrent chemoradiotherapy.
 | Table XSummary of mucosal malignant
melanoma. |
Table X
Summary of mucosal malignant
melanoma.
| Cases | Gender (age) | Primary lesion
site | TNM
classification | Treatment | Metastasis
(years) | Outcomes
(years) |
|---|
| 1 | F (67) | Palate | T3N0M0 | S (tumor resection
+ ND) + C (3 courses of DTIC) | Lung (1.6),
bronchus (7.5) | D (8.0) |
| 2 | F (77) | Maxilla | T3N0M0 | C (2 courses of
DTIC) + R (45 Gy) | Lung (1.5) | D (2.1) |
| 3 | M (74) | Maxilla | T3N0M0 | S (tumor resection
+ ND) + C (DAV ×3, CDDP-DTIC ×1, DAC-tam-feron ×4)+ R (51 Gy) | Lung (1.0) | D (9.4) |
| 4 | M (77) | Buccal mucosa | T2N0M0 | C (DAV-feron
×4) | Lung (2.2) | D (3.0) |
A total of 2 rhabdomyosarcoma patients and 1
synovial sarcoma patient visited our Department (Table XI). The outcomes for the
rhabdomyosarcoma cases were poor. The first rhabdomyosarcoma
patient was a 13-year-old boy. The CT scan revealed multiple
metastases in the lungs, suggesting that surgical treatment was not
feasible. Thus, the patient was immediately transferred to the
Pediatrics Department for chemotherapy. The patient finally
succumbed to respiratory dysfunction 9 months after his first
visit. The second rhabdomyosarcoma patient was a 61-year-old woman
who was treated with surgery and chemoradiotherapy. The treatment
achieved effective control of the local lesion; however, distant
lung metastasis occurred and compromised the patient’s general
condition. It should be noted that both rhabdomyosarcoma patients
succumbed to their disease within 2 years after their first
visits.
 | Table XIDetailed information of soft tissue
tumors. |
Table XI
Detailed information of soft tissue
tumors.
| Cases | Gender (age) | Primary lesion
site | Treatment | Metastasis
(years) | Outcome
(years) |
|---|
|
Rhabdomyosarcoma | M (13) | Palate | C (CY + VCR + CDDP
+ THP-ADR) | Lung (0) | D (0.7) |
|
Rhabdomyosarcoma | F (61) | Buccal mucosa | S (resection + ND)
+ C (CDDP + 5FU) + R (40 Gy) | Lung (0.3) | D (1.9) |
| Synovial
sarcoma | M (66) | TMJ | S (resection +
ND) | No | D (2.0; HCC) |
The synovial sarcoma patient was a 66-year-old man
treated with surgery. Although there was no evidence of recurrence,
the patient died of hepatocellular carcinoma 2 years after
surgery.
Discussion
The incidence of SCC is higher compared to that of
non-SCC (2), a fact also confirmed
by our study (90.7 vs. 9.3%, respectively). In addition, our data
revealed that the clinical outcomes of certain non-SCC cases were
not satisfactory when compared to those of SCC cases, indicating
that, although non-SCCs are minor diseases from the perspective of
epidemiology, these cases should be managed carefully. A possible
explanation as to why treatment of head and neck non-SCCs is
difficult may lie with their low frequency. Therefore, the
accumulated clinical observations provided in the present study may
be of great value. All clinicians should disclose information on
the head and neck non-SCC cases they encounter in order to share
this limited information and improve clinical outcomes.
The cumulative survival rates were found to be
significantly worse in ACC compared to those in SCC patients
(P=0.004; Fig. 4). The
unsatisfactory outcome of ACC may be due to the early and high
incidence of distant metastasis. In the present study, 6 metastases
occurred within 3 years after primary treatment and all the
patients who experienced distant metastasis eventually succumbed to
the disease. Conversely, distant metastasis was not observed in any
of the surviving cases. The distant metastasis rate of ACC was
significantly higher compared to that of SCC (Table VI). Our data revealed that tumour
size is the most significant risk factor for distant metastasis.
Therefore, timely diagnosis and treatment are essential in ACC
cases. Although no definitive clinical approach for preventing
distant metastasis has been established, it was previously reported
that surgery with postoperative radiotherapy significantly improved
the outcomes (13). Additionally,
Lin et al (14) reported
that postoperative radiotherapy reduced the recurrence rate in
patients with a negative resection margin. In the present study,
the effect of postoperative irradiation on recurrence in
margin-negative cases was not confirmed. The overall average
survival duration following local recurrence or distant metastasis
was 4.1 years, indicating that metastasized tumours progress slowly
or secondary treatment may suppress tumour development to a certain
extent. It is also crucial to maintain the quality of life
following recurrence or distant metastasis in ACC patients. Of the
cases with metastasis, 2 out of 9 underwent radiotherapy for
distant lesions and the average survival duration was 6.4 years
(Fig. 6). Therefore, radiotherapy
for metastatic disease should be considered as the primary
therapeutic option.
A number of cases with haematolymphoid tumours were
also observed. All the cases were non-Hodgkin lymphomas, comprising
13 B-cell neoplasms and 3 NK/T-cell neoplasms. NK/T-cell lymphoma
is generally aggressive and is associated with a poor outcome
(15,16). Of the patients with 3 NK/T-cell
lymphoma, 2 succumbed to the disease and 1 has survived for 5 years
without any evidence of recurrence. Cyclophosphamide, doxorubicin,
vincristine and prednisone therapy followed by radiotherapy is
currently the established standard treatment for localized
non-Hodgkin lymphoma (17).
However, as the outcome of localized NK/T-cell lymphoma (nasal
type) treated with this therapy is not satisfactory, concurrent
chemoradiotherapy as a therapeutic option has been investigated in
Japan. A phase I/II trial of concurrent chemoradiotherapy (DeVIC
and 50 Gy irradiation) for localized nasal NK/T-cell lymphoma was
conducted and the authors concluded that this regimen should be
recommended as a first-line treatment for this type of malignancy
(18). The surviving NK/T-cell
lymphoma patient in our study was a 28-year-old woman who initially
presented with a stage I localized lesion in her upper gingiva. The
patient was immediately referred to our Department for prompt
treatment and received radiotherapy (50 Gy) and 3 courses of DeVIC.
These findings indicate that initiating treatment at an early stage
is crucial and that concurrent chemoradiotherapy should be
recommended hereafter for NK/T-cell lymphomas.
In the present study, there were 4 cases of mucosal
malignant melanoma. Two of the patients (50%) exhibited long-term
survival; however, all the patients eventually succumbed to their
disease. Malignant melanoma of the head and neck is difficult to
cure. Of the deceased patients, 2 died within 3 years after
treatment, whereas the remaining 2 patients survived for a
significantly longer period. A 74-year-old male patient survived
for 10 years, despite developing distant metastases in the lung and
brain. In addition, a 67-year-old female patient survived
disease-free for ~8 years until distant metastasis to her lung and
bronchus occurred. Both patients underwent surgery, including neck
dissection, indicating that resection of the primary lesion and
regional lymph nodes may prolong survival. However, distant
metastasis, mainly to the lungs, hampers the management of head and
neck malignant melanoma.
Rhabdomyosarcoma is a malignant soft tissue tumour
of skeletal muscle origin that is most commonly encountered in the
head and neck region (19).
Rhabdomyosarcoma frequently occurs in childhood, particularly in
individuals aged <15 years. Indeed, in the present study, of the
2 rhabomyosarcoma patients, 1 was a 13-year-old boy. Both
rhabdomyosarcoma patients developed distant lung metastasis and
succumbed to their disease within 2 years of their first visits. In
a review of sarcomas of the oral and maxillofacial region,
Yamaguchi et al (20)
reported that 3 of 5 rhabdomyosarcoma cases died within 3 years
after treatment and that distant metastasis occurred in the
deceased but not in the surviving and disease-free patients. These
observations strongly indicate that distant metastasis is a major
complication contributing to the poor outcome in patients with
rhabdomyosarcoma and malignant melanoma.
Overall, the data of the present study indicate that
non-SCC patients frequently develop distant metastasis to the lung
and that the survival rate was significantly higher in the non-SCC
patients who underwent surgery compared to those who did not.
Furthermore, we hypothesized that the poor outcomes may be due to
the limited amount of clinical information available regarding
these rare malignancies. However, the present study was limited by
the fact that it was a single-center study with a limited number of
non-SCC cases. Therefore, the continued accumulation of information
from various clinical trials and other studies is required for
improving the clinical outcomes of non-SCCs patients.
In conclusion, our data indicated that non-SCC
malignant tumours of the head and neck are relatively rare.
However, non-SCC malignant tumours are a clinically significant
entity, as their management is generally difficult. Timely
treatment and control of distant metastasis are essential and
surgical treatment should be prioritized in non-SCC cases in order
to improve the outcomes in such patients.
Abbreviations:
|
SCC
|
squamous cell carcinoma
|
References
|
1
|
Slootweg PJ and Eveson JW: Tumours of the
oral cavity and oropharynx. World Health Organization
Classification of Tumours (Pathology and Genetics of Head and Neck
Tumours). Barnes L, Eveson JW, Reichart P and Sidransky D: IARC
Press; Lyon: pp. 163–165. 2005
|
|
2
|
Krolls SO and Hoffman S: Squamous cell
carcinoma of the oral soft tissues: a statistical analysis of
14,253 cases by age, sex, and race of patients. J Am Dent Assoc.
92:571–574. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Funk GF, Karnell LH, Robinson RA, Zhen WK,
Trask DK and Hoffman HT: Presentation, treatment, and outcome of
oral cavity cancer: a National Cancer Data Base report. Head Neck.
24:165–180. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kemp S, Gallagher G, Kabani S, Noonan V
and O’Hara C: Oral non-Hodgkin’s lymphoma: review of the literature
and World Health Organization classification with reference to 40
cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
105:194–201. 2008.
|
|
5
|
Al-Sukhun J, Lindqvist C, Hietanen J,
Leivo I and Penttilä H: Central adenoid cystic carcinoma of the
mandible: case report and literature review of 16 cases. Oral Surg
Oral Med Oral Pathol Oral Radiol Endod. 101:304–308. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Khan AJ, DiGiovanna MP, Ross DA, et al:
Adenoid cystic carcinoma: a retrospective clinical review. Int J
Cancer. 96:149–158. 2001. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
Parashar P, Baron E, Papadimitriou JC, Ord
RA and Nikitakis NG: Basal cell adenocarcinoma of the oral minor
salivary glands: review of the literature and presentation of two
cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 103:77–84.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
do Prado RF, Lima CF, Pontes HA, Almeida
JD, Cabral LA and Carvalho YR: Calcifications in a clear cell
mucoepidermoid carcinoma: a case report with histological and
immunohistochemical findings. Oral Surg Oral Med Oral Pathol Oral
Radiol Endod. 104:e40–e44. 2007.PubMed/NCBI
|
|
9
|
Corcione L, Giordano G, Gnetti L, Multinu
A and Ferrari S: Oncocytic mucoepidermoid carcinoma of a
submandibular gland: a case report and review of the literature.
Int J Oral Maxillofac Surg. 36:560–563. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sciubba JJ: Oral cancer. The importance of
early diagnosis and treatment. Am J Clin Dermatol. 2:239–251.
2001.
|
|
11
|
Terada T: Small cell carcinoma of the oral
cavity (cheek mucosa): a case report with an immunohistochemical
and molecular genetic analysis. Int J Clin Exp Pathol. 6:780–787.
2013.PubMed/NCBI
|
|
12
|
Shenoy N, Sholapurkar AA, Pai KM and Pal
K: Small cell carcinoma of the oral cavity: report of a rare case.
J Calif Dent Assoc. 37:399–401. 2009.PubMed/NCBI
|
|
13
|
Shen C, Xu T, Huang C, Hu C and He S:
Treatment outcomes and prognostic features in adenoid cystic
carcinoma originated from the head and neck. Oral Oncol.
48:445–449. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lin YC, Chen KC, Lin CH, Kuo KT, Ko JY and
Hong RL: Clinicopathological features of salivary and non-salivary
adenoid cystic carcinomas. Int J Oral Maxillofac Surg. 41:354–360.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Schmitt C, Sako N, Bagot M, Huang Y,
Gaulard P and Bensussan A: Extranodal NK/T-cell lymphoma: toward
the identification of clinical molecular targets. J Biomed
Biotechnol. 2011:7908712011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Coha B, Vucinic I, Mahovne I and
Vukovic-Arar Z: Extranodal lymphomas of head and neck with emphasis
on NK/T-cell lymphoma, nasal type. J Craniomaxillofac Surg.
42:149–152. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Miller TP, Dahlberg S, Cassady JR, et al:
Chemotherapy alone compared with chemotherapy plus radiotherapy for
localized intermediate- and high-grade non-Hodgkin’s lymphoma. N
Engl J Med. 339:21–26. 1998.PubMed/NCBI
|
|
18
|
Yamaguchi M, Tobinai K, Oguchi M, et al:
Concurrent chemoradiotherapy for localized nasal natural
killer/T-cell lymphoma: an updated analysis of the Japan clinical
oncology group study JCOG0211. J Clin Oncol. 30:4044–4046. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Miloglu O, Altas SS, Buyukkurt MC, Erdemci
B and Altun O: Rhabdomyosarcoma of the oral cavity: a case report.
Eur J Dent. 5:340–343. 2011.PubMed/NCBI
|
|
20
|
Yamaguchi S, Nagasawa H, Suzuki T, et al:
Sarcomas of the oral and maxillofacial region: a review of 32 cases
in 25 years. Clin Oral Investig. 8:52–55. 2004.PubMed/NCBI
|