Introduction
Primary patellar tumors are uncommon and may present
with anterior knee pain and/or swelling (1). Recently, Casadei et al
(2) reported that the most
frequent benign patellar tumor is giant cell tumor (GCT), followed
by chondroblastoma and aneurysmal bone cyst (ABC). GCT accounts for
4–5% of all primary bone tumors and usually affects the ends of
long bones (3). This is the report
of a rare case of GCT of the patella in a young adult woman and a
brief review of the relevant literature. Written informed consent
was obtained from the patient for publication of this case report
and accompanying images.
Case report
A 25-year-old woman presented with a 1-year history
of occasional right anterior knee pain. Two weeks prior to visiting
our hospital, the patient had been experiencing increasing anterior
knee pain following a stumble. The physical examination revealed
mild swelling and slight tenderness in the anterior aspect of the
right knee. However, we did not observe any skin adhesion, local
heat, redness, or limitation of the knee joint range of motion.
Furthermore, no joint effusion was noted. The laboratory data were
within normal limits, except for a marginal elevation of alkaline
phosphatase levels. The patient's past medical history was
unremarkable.
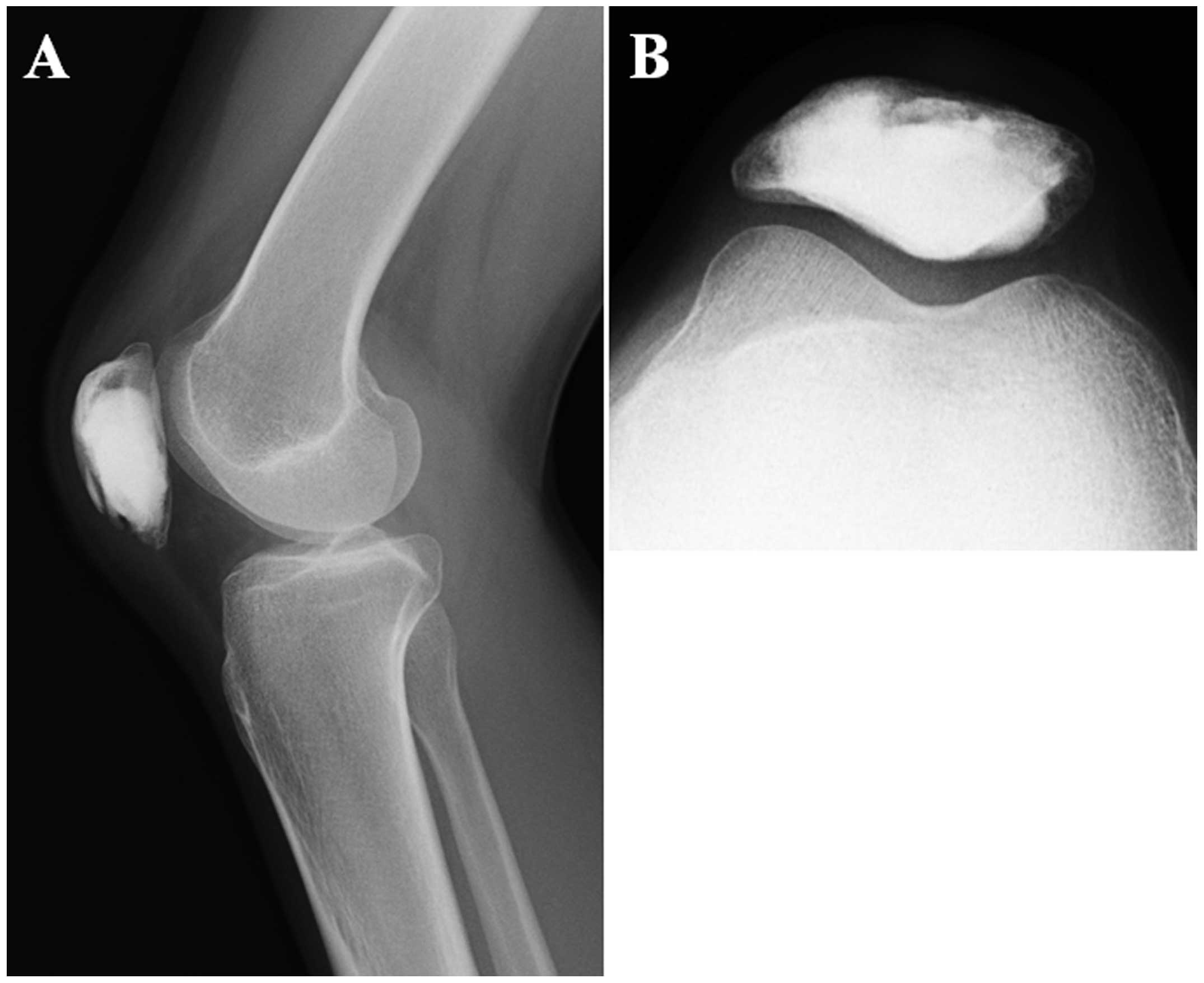
Plain radiographs revealed a well-defined, lytic
lesion in the inferior and central portion of the patella (Fig. 1). There was no periosteal reaction.
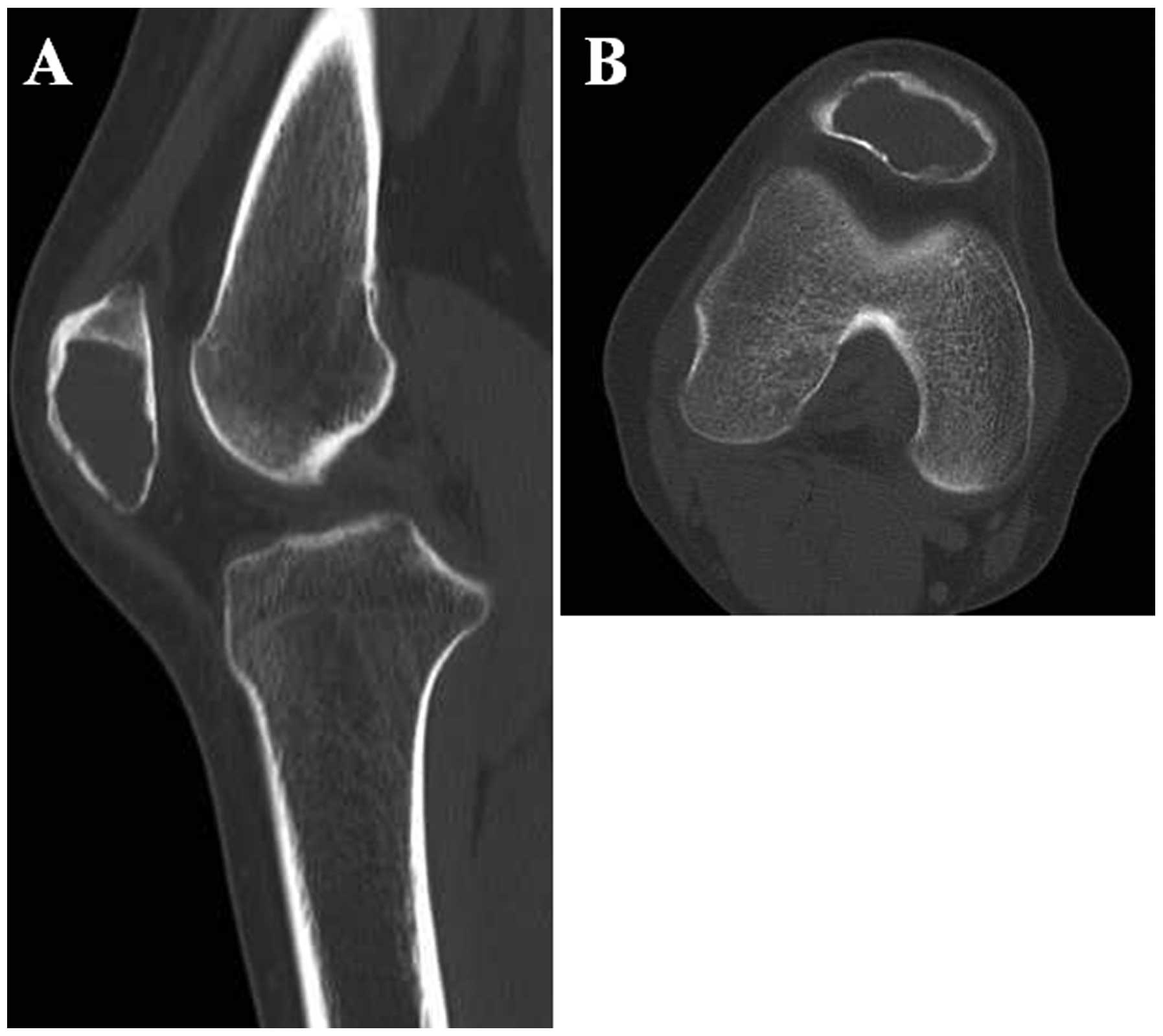
Computed tomographic (CT) scans demonstrated an intraosseous lytic
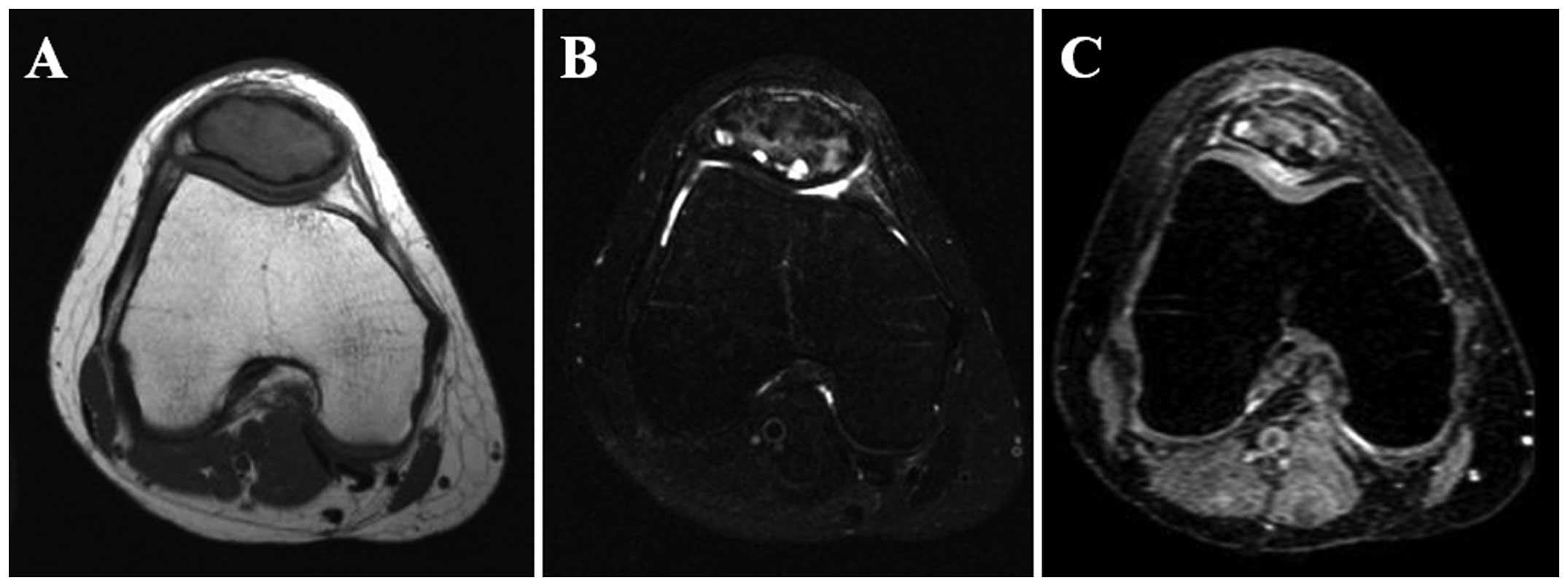
lesion with associated cortical thinning (Fig. 2). On magnetic resonance imaging
(MRI), the lesion exhibited slightly higher signal intensity
compared to skeletal muscle on T1-weighted sequences (Fig. 3A) and heterogeneous signal
intensity on T2-weighted spectral presaturation with inversion
recovery sequences (Fig. 3B).
Contrast-enhanced fat-suppressed T1-weighted sequences demonstrated
a heterogeneously strong enhancement of the lesion (Fig. 3C). There was no obvious soft tissue
or intra-articular extension. Technetium-99m hydroxymethylene
diphosphonate bone scintigraphy revealed no abnormal uptake, except
for the right patella (Fig. 4).
Based on these findings, a benign bone tumor was suggested,
including GCT in the differential diagnosis.
An incisional biopsy was performed and a rapid
intraoperative pathological diagnosis was GCT of the bone. The
patient subsequently underwent radical intralesional curettage with
a high-speed burr. Following curettage, 70% phenol was applied
meticulously to the inner surface of the cavity with a cotton swab
for a period of 5 min. The cavity was then filled with 99.5%
ethanol for 5 min. After extensive washing with normal saline
solution, the cavity was filled with calcium phosphate cement
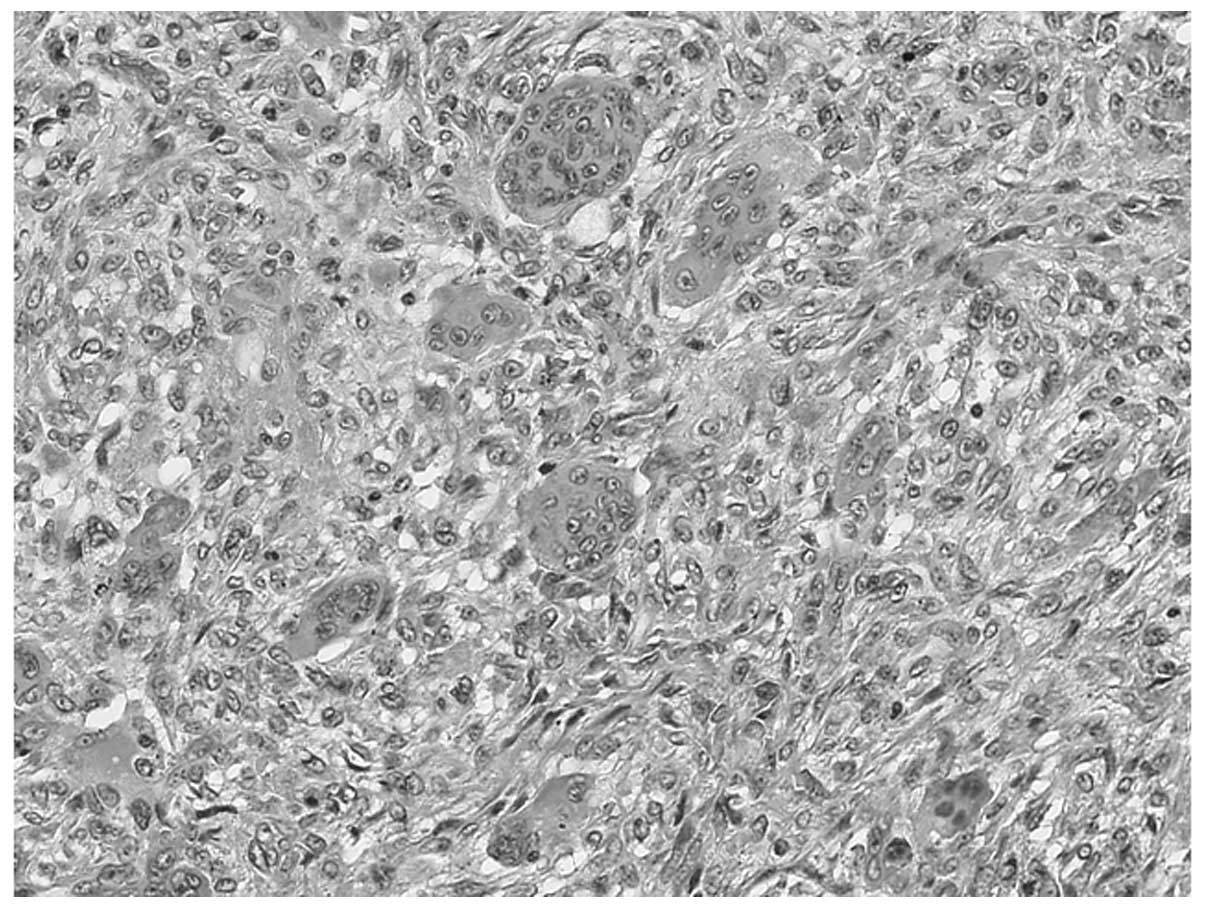
(Biopex®; Pentax, Tokyo, Japan). Microscopically, the
tumor consisted of round or spindle-shaped mononuclear cells
admixed with numerous osteoclastic giant cells (Fig. 5). Foci of hemorrhage, hemosiderin
deposits and aggregates of foamy histiocytes were also found.
Mitotic figures were present among the mononuclear cells, but there
were no atypical mitoses identified. These findings confirmed the
diagnosis of GCT of the bone.
The postoperative course was uneventful. The patient
returned to normal activities within 1 month after surgery. At 16
months follow-up, the patient was asymptomatic and there was no
evidence of local recurrence (Fig.
6) or distant metastasis.
Discussion
GCT is a benign but locally aggressive bone tumor
that is composed of mononuclear cells and osteoclast-like giant
cells. GCT typically affects the ends (epiphyses) of long bones,
particularly the distal femur and proximal tibia. GCT has a peak
incidence in the third or fourth decade of life, with a marginal
female predominance (3). Pain is
the most common symptom. The majority of patients note swelling of
the affected region. Pathological fractures are seen in 5–10% of
the patients (3). Traditionally,
GCT has been treated surgically with curettage and placement of
bone graft or cement. Local recurrence occurs in 15–25% of the
patients (4), depending on the
thoroughness of the curettage and the nature of the adjuvant
therapy. Malignant transformation occurs in <1% of all GCTs
(3). The histogenesis of GCT has
not been fully elucidated.
Patellar tumors represent an uncommon etiology of
anterior knee pain and their diagnosis is often delayed (5). Benign lesions are more frequent
compared to malignant tumors (1,
2, 6). The most common benign tumor is GCT,
followed by chondroblastoma and ABC (2). Metastases are the most frequent
malignant tumors of the patella and primary malignant lesions
predominantly include osteosarcoma, hemangioendothelioma and
lymphoma (2). We previously
reported a case of osteosarcoma of the patella mimicking GCT with
secondary ABC in a middle-aged patient (7).
The differential diagnosis of the present case may
include chondroblastoma and hemangioma. Chondroblastoma accounts
for <1% of all bone tumors and most frequently occurs in the
second decade of life, with a male predominance (8). Radiographically, chondroblastoma
usually presents as a well-defined, round or oval lytic lesion.
Periosteal reaction is absent in the patella. Calcification is
observed in 19% of the cases (2),
which is less compared to other skeletal sites. CT may be useful in
revealing tiny, scattered calcifications. Peritumoral edema may be
seen on MRI. Chondroblastoma is usually smaller in size compared to
GCT (1). On the other hand, 10
cases of hemangioma in the patella have been reported to date,
representing ∼2% of all patellar tumors (2). Periosteal reaction, calcification and
septation are absent in the patella. On MRI, bone hemangioma
typically exhibits increased signal intensity on T1- and
T2-weighted sequences, possibly due to the fat content of the
lesion (9). In the present case,
it was difficult to distinguish these 2 conditions from GCT on the
basis of imaging characteristics alone.
The surgical treatment for patellar GCT includes
curettage with bone graft and patellectomy (6, 10,
11). Total patellectomy has been
recommended as the preferred treatment for aggressive benign
lesions with cortical breakthrough (6). Recently, Malhotra et al
(12) reported a case of
aggressive GCT of the patella and its management with wide
resection and reconstruction of the extensor mechanism using a
patellar allograft. We performed radical curettage with adjuvant
phenol and ethanol and injectable calcium phosphate cement
grafting. This treatment was considered to be appropriate for our
patient. Sixteen months after surgery, the patient was free of
symptoms and there was no clinical or radiographic evidence of
local recurrence.
In summary, we have described a rare case of
patellar GCT in a young adult patient. Patellar tumors, such as
GCT, should be considered in the differential diagnosis of
persistent unexplained knee pain, particularly in young adult
patients.
References
|
1
|
Singh J, James SL, Kroon HM, Woertler K,
Anderson SE, Jundt G and Davies AM: Tumour and tumour-like lesions
of the patella - a multicentre experience. Eur Radiol. 19:701–712.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Casadei R, Kreshak J, Rinaldi R, Rimondi
E, Bianchi G, Alberghini M, Ruggieri P and Vanel D: Imaging tumors
of the patella. Eur J Radiol. 82:2140–2148. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Athanasou NA, Bansal M, Forsyth R, Reid RP
and Sapi Z: Giant cell tumor of boneWorld Health Organization
Classification of Tumours of Soft Tissue and Bone. Fletcher CDM,
Bridge JA, Hogendoorn PCW and Mertens F: 4th. IARC Press; Lyon: pp.
321–324. 2013
|
|
4
|
Chakarun CJ, Forrester DM, Gottsegen CJ,
Patel DB, White EA and Matcuk GR Jr: Giant cell tumor of bone:
review, mimics, and new developments in treatment. Radiographics.
33:197–211. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Saglik Y, Yildiz Y, Basarir K, Tezen E and
Guner D: Tumours and tumour-like lesions of the patella: a report
of eight cases. Acta Orthop Belg. 74:391–396. 2008.PubMed/NCBI
|
|
6
|
Mercuri M and Casadei R: Patellar tumors.
Clin Orthop Relat Res. 389:35–46. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Aoki M, Nishio J, Iwasaki H, Masaki M,
Kawakami Y, Nishino T, Ohjimi H, Tamura K, Nabeshima K and Naito M:
Osteosarcoma of the patella mimicking giant cell tumor: imaging
features with histopathological correlation. Anticancer Res.
34:2541–2545. 2014.PubMed/NCBI
|
|
8
|
Kilpatrick SE and Romeo S:
ChondroblastomaWorld Health Organization Classification of Tumours
of Soft Tissue and Bone. Fletcher CDM, Bridge JA, Hogendoorn PCW
and Mertens F: 4th. IARC Press; Lyon: pp. 262–263. 2013
|
|
9
|
Vilanova JC, Barcelo J, Smirniotopoulos
JG, Perez-Andres R, Villalon M, Miro J, Martin F, Capellades J and
Ros PR: Hemangioma from head to toe: MR imaging with pathologic
correlation. Radiographics. 24:367–385. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ferguson PC, Griffin AM and Bell RS:
Primary patellar tumors. Clin Orthop Relat Res. 336:199–204. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yoshida Y, Kojima T, Taniguchi M, Osaka S
and Tokuhashi Y: Giant-cell tumor of the patella. Acta Med Okayama.
66:73–76. 2012.
|
|
12
|
Malhotra R, Sharma L, Kumar V and Nataraj
AR: Giant cell tumor of the patella and its management using a
patella, patellar tendon, and tibial tubercle allograft. Knee Surg
Sports Traumatol Arthrosc. 18:167–169. 2010. View Article : Google Scholar : PubMed/NCBI
|