Introduction
Well-differentiated thyroid cancer is the most
common endocrine tumor, and its prevalence is increasing worldwide
(1). The majority of thyroid cancer
cases (~85%) are papillary thyroid carcinoma (PTC) (2). A number of PTC variants have been
described, including classical, follicular, oncocytic, solid, tall
cell, columnar cell, diffuse sclerosing and cribriform (3,4). Among
these variants, the conventional or classical type is the most
common and accounts for ≤54.2% of all PTC cases in certain reported
series (5–8). The follicular variant is the second most
common subtype and constitutes 4.9–41.2% PTC cases in different
series (7–12). Since the follicular variant of PTC
(FV-PTC) was first described by Crile and Hazard in 1953 (13), FV-PTC has been increasingly diagnosed
and accounts for 41–53% of PTC cases (7,14).
As FV-PTC exhibits a mixed histopathological picture
of PTC and follicular thyroid carcinoma (FTC), certain
investigators have hypothesized that FV-PTC has specific
characteristics from the two types. Numerous studies have since
investigated the clinical behavior of FV-PTC and the classical type
of PTC (C-PTC) and compared the two; however, certain results were
contradictory. In different studies, the incidence of aggressive
clinical features was identified as higher, similar or lower in
FV-PTC compared to C-PTC (5,7,8,10,12,15–20).
Meta-analysis is a powerful tool for summarizing the
results of different studies by producing a single estimate of the
major effect with enhanced precision. A major advantage of a
meta-analysis is the increase in sample size, which may reduce the
probability that a random error will produce false-positive or
false-negative associations.
A meta-analysis was performed to quantify and
compare the clinical parameters of C-PTC and FV-PTC and provide
some guidance on the management and prognosis of FV-PTC. The
following clinicopathological parameters were evaluated: Age,
gender, tumor size, multifocality, capsular invasion, vascular
invasion, extrathyroidal extension, lymph node metastasis,
lymphocytic and/or Hashimoto's thyroiditis, clinical stage,
BRAF mutation and recurrence.
Materials and methods
Selection criteria
Studies that examined the associations of FV-PTC and
C-PTC with clinicopathological parameters were searched for. The
following criteria were considered when selecting the studies: i)
Studies published in English between January 1, 2003 and August 31,
2014. ii) The criteria of C-PTC include classical, conventional and
pure PTC. iii) Clinicopathological parameters with detailed data on
C-PTC and FV-PTC tissue were included from the same studies that
assessed different types of carcinoma, such as primary, follicular,
anaplastic and medullary carcinomas. iv) Only studies analyzing at
least two of the above categories of clinicopathological data and
containing ≥5 cases reported FV-PTC and C-PTC. v) When multiple
studies were published by the same investigators or groups, the
newest or most informative single study was selected. The following
studies were excluded: i) Review studies without original data; ii)
absent or inappropriately reported clinicopathological data; iii)
single or pure case reports; iv) animal research; and v) familial
research studies.
Collection of published studies
A literature search was carried out using the PubMed
database (http://www.ncbi.nlm.nih.gov/pubmed). The search term
combination was ‘follicular variant of papillary thyroid carcinoma’
OR ‘FV-PTC’ OR ‘FVPTC’ OR ‘FPTC’ OR ‘F-PTC.’ Relevant studies were
selected on the basis of the summary analysis. Any duplication of
data was carefully avoided by examining the names of all the
authors and different medical centers involved in each publication.
Overlapping studies or data and studies that were unrelated to the
meta-analysis were excluded. Two investigators (J. Yang and Y.P.
Gong) used the EndNote reference tool to independently screen and
select studies. All the procedures conformed to the guidelines for
the meta-analysis of observational studies in epidemiology
(21).
Data analyses and statistical
methods
Review Manager (version 5.1; http://tech.cochrane.org/revman) was used to perform
all the statistical analyses, including the calculation of the
summary odds ratio (OR) or the mean difference (MD) with a 95%
confidence interval (CI), using a random- or fixed-effect model for
all the analyses. The choice of each individual statistical method
depended on whether the measured event was dichotomous or
continuous, whereas the choice of a random- or fixed-effect model
depended on the tests for heterogeneity. The heterogeneity of the
studies was assessed using the χ2 test of heterogeneity
and the I2 measure of inconsistency. When the
heterogeneity in the χ2 test showed a P-value of
<0.10 or when the I2 measure was >50%, the
random-effect model was chosen, otherwise the fixed-effect model
was used. The 95% CI was constructed around the effect size to
establish its significance.
For the OR of dichotomous events, if the 95% CI of
an OR included 1, the two groups were not considered statistically
different, otherwise they were considered statistically different.
For the MD of continuous events, if the 95% CI crossed the null
point (zero), then the possibility that the difference should be
attributed to chance could not be ruled out. When the null point
fell outside the 95% CI of an MD, the observed difference was
considered statistically significant. The potential publication
bias was assessed using Begg's funnel plot and Egger's test by
Stata 12.0 software (Stata Corporation, College Station, TX, USA).
P<0.05 was considered to indicate a statistically significant
difference.
Results
Clinicopathological parameters
Fig. 1 summarizes the
study selection process. A total of 495 abstracts and titles were
obtained using a PubMed search, of which 81 were published before
January 1, 2003 and 1 duplicate study was excluded. Of the
remaining 413, 112 full-text studies were deemed relevant and were
examined in detail. Eventually, following the application of all
the inclusion and exclusion criteria, 36 studies (7,8,10,12,14,16,17,19,20,22–48)
fulfilled the eligibility criteria. The main features of the
eligible studies are summarized in Table
I. In each category of clinicopathological parameters, some
heterogeneity was present. In terms of tumor size, multifocality,
capsular invasion, vascular invasion, extrathyroidal extension and
lymph node metastasis, their heterogeneity was assessed using
χ2 tests and the P-value was <0.10 (or I2
measures were >50%). The random-effect models were selected, but
for the remaining parameters, fixed-effect models were used. The
combined results of the meta-analysis and the heterogeneity test
are shown in Table II.
 | Table I.Characteristics of individual studies
included in the meta-analysis. |
Table I.
Characteristics of individual studies
included in the meta-analysis.
|
|
| Patients, no. | Mean age (years) ±
SD and/or ≥ (>) 45, no. (%) | Mean tumor size
(mm) ± SD and/or ≥ (>)10, no. (%) |
|
|---|
|
|
|
|---|
| First author,
year | Country | FV-PTC | C-PTC | FV-PTC | C-PTC | FV-PTC | C-PTC | (Refs.) |
|---|
| Abrosimov,
2007a | Japan | 34 | 148 | NA | NA | >10±11
(32.4) | >10±71
(47.3) | (22) |
| Brzezianska,
2007 | Poland | 8 | 14 | 49 (20.4) | 47.57 (17) | NA | NA | (23) |
|
|
|
|
| ≥45±5 (62.5) | ≥45±7 (50.0) |
|
|
|
| Burningham,
2005 | USA | 46 | 114 | 46
(17)b | 47
(26)b | 15
(19)b | 10
(16)b | (19) |
| Chang, 2006 | China | 85 | 170 | NA | NA | 27 (18.4) | 23 (13.0) | (10) |
| Costa, 2008 | Portugal | 17 | 16 | 37 (10) | 45 (25) | 34 (25) | 35 (15) | (24) |
| Daglar-Aday,
2013 | Turkey | 36 | 72 | 44.94 (15.21) | 52.88 (17.11) | NA | NA | (25) |
| Darr, 2011 | USA | 6 | 7 | 43 (15) | 44 (14) | >20±5
(16.7) | >20±6
(14.3) | (26) |
| Dettmer, 2013 | USA | 17 | 27 | 50.9 (17.73) | 47.8 (15.58) | NA | NA | (27) |
| Di Cristofaro,
2006 | France | 24 | 26 | 38.5 (13) | 43.3 (17.3) | 21.5 (8.5) | 25.7 (11.3) | (28) |
| Eloy, 2011 | Portugal | 31 | 42 | 42.73 (12.94) | 39 (17.75) | 22.3 (18) | 22.4 (17.1) | (29) |
|
|
|
|
| ≥45±15 (48.4) | ≥45±14 (33.3) | >10±23
(74.2) | >10±32
(76.2) |
|
| Ertek, 2012 | Turkey | 56 | 42 | 39.1 (10.6) | 46.7 (12.9) | 34.7 (31.7) | 13.9 (12.2) | (14) |
| Espadinha,
2009 | Portugal | 17 | 21 | 35.41 (25.37) | 39.24 (25.17) | NA | NA | (30) |
|
|
|
|
| ≥45±6 (35.3) | ≥45±14 (33.3) |
|
|
|
| Gao, 2012 | China | 25 | 84 | ≥45±13 (52) | ≥45±54 (64.3) | >10±20 (80) | >10±61
(72.6) | (31) |
| Hagag, 2006 | Israel | 92 | 99 | 46 (19.18) | 44 (9.95) | 22 (19.2) | 20 (9.9) | (20) |
|
|
|
|
| ≥45±52 (56.5) | ≥45±54 (54.5) |
|
|
|
| Hunt, 2004 | USA | 16 | 8 | 50.38 (11.63) | 46.75 (11.5) | 30.1 (23.7) | 15.6 (13.7) | (32) |
|
|
|
|
| ≥45±11 (68.8) | ≥45±5 (62.5) | >10±11
(68.8) | >10±4 (50) |
|
| Igci, 2013 | Turkey | 10 | 11 | 38.5 (12.75) | 50.09 (19.61) | 30.6 (16.9) | 30.6 (16.6) | (33) |
|
|
|
|
| ≥45±5 (50) | ≥45±4 (36.4) | >10±9 (90) | >10±11
(100) |
|
| Igci, 2014 | Turkey | 25 | 15 | 46.76 (13.72) | 48.73 (15.66) | 14.4 (9.7) | 16.4 (10) | (34) |
|
|
|
|
| ≥45±15 (60) | ≥45±9 (60) | ≥10±16 (64) | ≥10±9 (60) |
|
| Ito, 2008 | Japan | 100 | 1,313 | >55±41 (41) | >55±403
(30.7) | >40±6 (6) | >40±158
(12) | (35) |
| Lang, 2006 | China | 67 | 308 | 38.5
(14–83)c | 42.0
(11–81)c | 25
(10–85)c | 25
(10–100)c |
(8) |
| Lassalle, 2011 | France | 5 | 11 | 39 (8.06) | 44.45 (18.05) | 22.4 (8.4) | 17.7 (7.8) | (36) |
| Lee, 2011 | Korea | 30 | 30 | 49.27 (12.8) | 47.83 (9.65) | 17.4 (9.6) | 9.7 (6.4) | (37) |
| Lim, 2013 | Korea | 85 | 2,947 | 45
(13–84)c | 47
(24–74)c | 8.2
(0.5–)c | 10
(2–65)c | (38) |
| Liu, 2010 | USA | 73 | 114 | NA | NA | NA | NA | (39) |
| Min, 2013 | Korea | 58 | 312 | >45±44
(75.9) | >45±172
(55.1) | >10±15
(25.9) | >10±101
(32.4) | (40) |
| Nechifor-Boila,
2013 | Romania | 90 | 98 | 27 (6.1) | 26.3 (5.5) | 27 (16) | 21 (11) | (41) |
| Oler, 2009 | Brazil | 47 | 73 | ≥45±23 (53.5) | ≥45±31 (43.7) | ≥10±35 (74.5) | ≥10±50 (70.4) | (42) |
| Ozdemir, 2011 | Turkey | 90 | 354 | 43.98 (12.46) | 45.82 (12.24) | 16.9 (13.9) | 10.6 (9.7) | (17) |
|
|
|
|
|
|
| >10±55
(61.1) | >10±127
(35.9) |
|
| Passler, 2003 | Austria | 37 | 117 | 46.4
(10.9–74.8)c | 47.5
(18.1–79.3)c | 17.9 (17.6) | 24.2 (21) | (12) |
| Rivera, 2009 | USA | 63 | 43 | >45±30
(47.6) | >45±14
(32.6) | ≥40±22 (35.5) | ≥40±2 (4.7) | (43) |
| Schulten, 2012 | Saudi Arabia | 42 | 115 | NA | NA | NA | NA | (44) |
| Sheu, 2010 | Germany | 30 | 10 | 46.4 (15.4) | 48.1 (14.0) | 28.5 (18.1) | 26.2 (18.8) | (45) |
| Slosar, 2009 | USA | 60 | 37 | NA | NA | ≥10±56 (93.3) | ≥10±30 (81.1) | (46) |
| Trovisco, 2005 | Portugal | 54 | 69 | 41.5 (19.11) | 37.2 (17.44) | 27 (13.6) | 32 (21) | (47) |
| Wreesmann,
2004 | USA | 17 | 25 | 40
(25–75)c | 41
(20–77)c | 25
(8–65)c | 20
(6–45)c | (48) |
| Yuksel, 2008 | Turkey | 41 | 158 | >40±31
(75.6) | >40±37
(23.4) | 16.5 (10.8) | 13.4 (10) | (16) |
| Zidan, 2003 | Israel | 100 | 143 | 44
(17–81)c | 43
(11–78)c | 35
(3–100)c | 34
(4–90)c |
(7) |
 | Table II.Meta-analyses of the
clinicopathological parameters between FV-PTC and C-PTC. |
Table II.
Meta-analyses of the
clinicopathological parameters between FV-PTC and C-PTC.
| Clinicopathological
characteristics | Included study,
n | Heterogeneity
test | Effects model
selection | OR/MD (95%
confidence interval) | Combined effect
test | Statistical
significance | Egger's test |
|---|
|
|
|
|---|
| χ2 | P-value | I2,
% | Z | P-value | P-value |
|---|
| Female | 33 | 29.61 | 0.59 | 0 | Fixed | 1.09
(0.93–1.29) | 1.06 | 0.29 | No | 0.707 |
| Age, years |
|
|
|
|
|
|
|
|
|
|
|
Mean | 19 | 31.36 | 0.03 | 43 | Fixed | −0.61
(−1.75–0.53)a | 1.05 | 0.29 | No | 0.413 |
|
≥45 | 11 | 8.90 | 0.54 | 0 | Fixed | 1.45
(1.11–1.90) | 2.69 | <0.01 | Yes | 0.754 |
| Tumor size, mm |
|
|
|
|
|
|
|
|
|
|
|
Mean | 17 | 50.72 | <0.01 | 68 | Random | 2.88
(0.26–5.51)a | 2.15 | 0.03 | Yes | 0.485 |
|
≥10 | 10 | 21.73 | 0.01 | 59 | Random | 1.25
(0.77–2.03) | 0.92 | 0.36 | No | 0.473 |
| Multifocality | 17 | 40.85 | <0.01 | 61 | Random | 0.88
(0.64–1.24) | 0.77 | 0.44 | No | 0.522 |
| CI | 6 | 14.60 | 0.01 | 66 | Random | 0.82
(0.48–1.39) | 0.74 | 0.46 | No | 0.577 |
| VI | 9 | 31.84 | <0.01 | 75 | Random | 1.38
(0.56–3.42) | 0.69 | 0.49 | No | 0.555 |
| EE | 18 | 56.75 | <0.01 | 70 | Random | 0.40
(0.25–0.64) | 3.86 | <0.01 | Yes | 0.609 |
|
LNM | 23 | 65.94 | <0.01 | 67 | Random | 0.35
(0.25–0.49) | 6.12 | <0.01 | Yes | 0.450 |
| LT
or/and HT | 9 | 13.94 | 0.08 | 43 | Fixed | 0.79
(0.61–1,02) | 1.82 | 0.07 | No | 0.419 |
| CS
(I+II) | 12 | 10.29 | 0.50 | 0 | Fixed | 1.17
(0.90–1.52) | 1.16 | 0.25 | No | 0.605 |
|
BRAF mutation | 13 | 8.15 | 0.77 | 0 | Fixed | 0.19
(0.15–0.24) | 13.34 | <0.01 | Yes | 0.247 |
|
Recurrence | 8 | 5.46 | 0.60 | 0 | Fixed | 0.52
(0.34–0.80) | 2.98 | <0.01 | Yes | 0.991 |
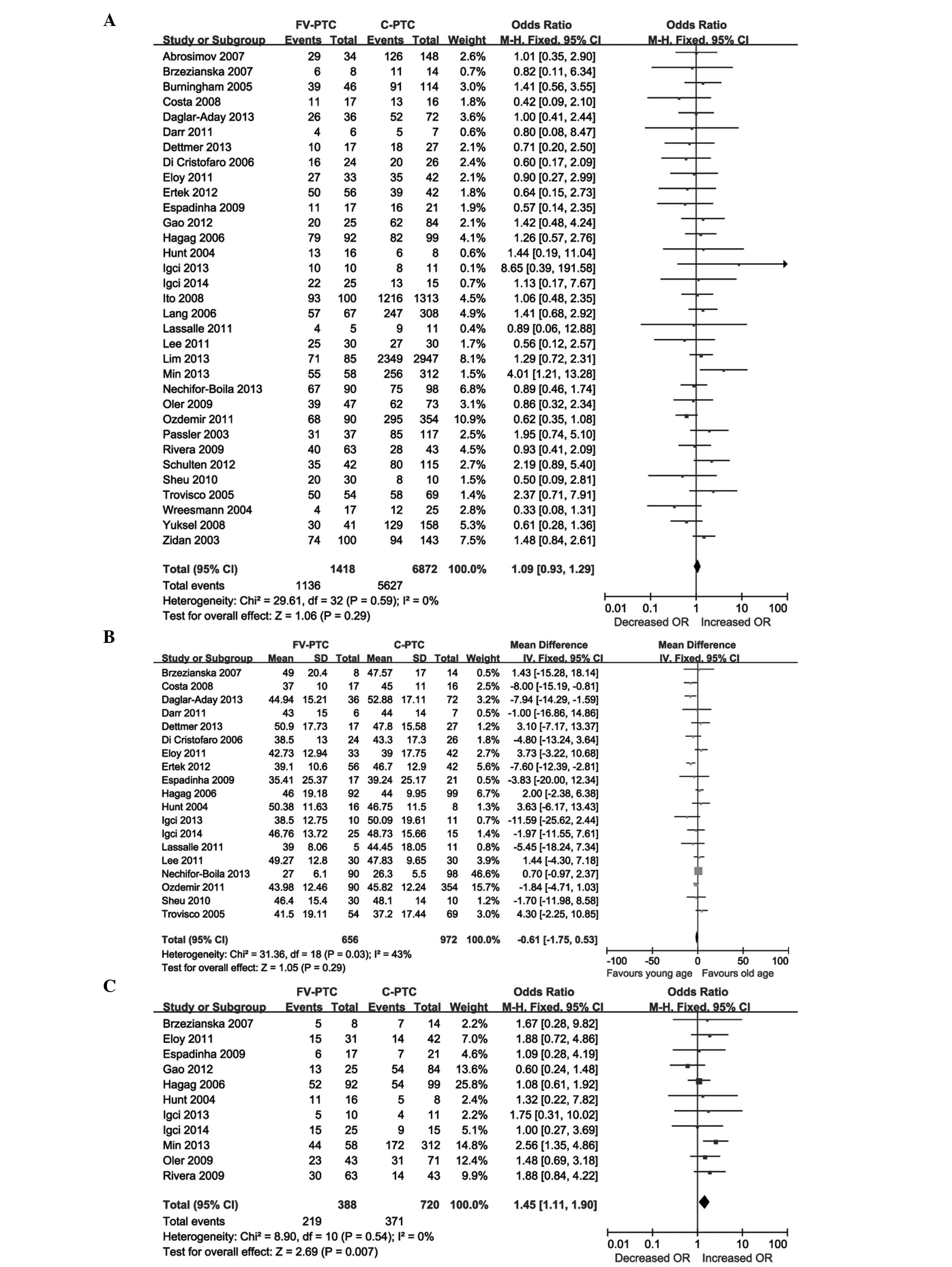
Gender
In total, 33 studies were comparable in terms of
gender. The prevalence of females among patients with FV-PTC and
C-PTC was 80.1 (1,136/1,418) and 81.9% (5,627/6,872), respectively,
and the difference was not statistically significant (OR, 1.09; 95%
CI, 0.93–1.29; P=0.29; Fig. 2A). No
statistical heterogeneity was detected among the studies
(χ2=29.61, P=0.59, I2=0%).
Age
Nineteen studies included mean age in the patient
clinical data. The mean age of patients with FV-PTC ranged from 27
to 50.9 years, whereas those of the patients with C-PTC ranged from
26.3 to 52.88 years, and the difference was not significant (MD,
−0.61; 95% CI, −1.75–0.53; P=0.29; Fig.
2B). No statistical heterogeneity was identified among the
studies (χ2=31.36, P=0.03, I2=43%). In
addition, 11 studies presented the prevalence of patients aged ≥45
years, which overall was 56.4 (219/388) and 51.5% (371/720) in
patients with FV-PTC and C-PTC, respectively, and the difference
was statistically significant (OR, 1.45; 95% CI, 1.11–1.90;
P=0.007; Fig. 2C). There was no
significant statistical heterogeneity among the studies
(χ2=8.90, P=0.54, I2=0%).
Tumor size
Seventeen studies presented clinical data that
included mean tumor size. The mean tumor size of patients with
FV-PTC ranged from 14.4 to 34.7 mm, whereas that of patients with
C-PTC ranged from 9.7 to 35.0 mm; this difference was statistically
significant (MD, 2.88; 95% CI, 0.26–5.51; P=0.03; Fig. 2D). Significant statistical
heterogeneity was present among the studies (χ2=50.73,
P<0.0001, I2=68%). Ten studies presented the
prevalence of the tumor size of patients with FV-PTC and C-PTC
being ≥10 mm, which overall was 63.4 (251/396) and 45.8%
(496/1,084), respectively, and the difference was not significant
(OR, 1.25; 95% CI, 0.77–2.03; P=0.36; Fig. 2E). There was significant statistical
heterogeneity among the studies (χ2=21.73, P=0.010,
I2=59%).
Multifocality
In 17 studies that analyzed multifocality, the
overall percentage of patients with multifocality in FV-PTC and
C-PTC was 31.6 (257/813) and 30.7% (1,411/4,593), respectively, and
the difference was not statistically significant (OR, 0.88; 95% CI,
0.64–1.22; P=0.44; Fig. 2F). No
statistical heterogeneity was detected among the studies
(χ2=40.85, P=0.0006, I2=61%).
Capsular invasion
In 6 studies that assessed the capsular invasion of
the tumor, the percentages of patients with capsular invasion in
FV-PTC and C-PTC were 28.1 (115/409) and 30.2% (281/932),
respectively, and the difference was not statistically significant
difference (OR, 0.82; 95% CI, 0.48–1.39; P=0.46; Fig. 2G). There was no statistical
heterogeneity among the studies (χ2=14.60, P=0.01,
I2=66%).
Vascular invasion
In 9 studies, the percentages of cases with vascular
invasion in FV-PTC and C-PTC were reported; these were 19.8
(85/430) and 12.2% (86/704), respectively, and the difference was
not significant (OR, 1.38; 95% CI, 0.56–3.42; P=0.49; Fig. 2H). Significant statistical
heterogeneity was detected among the studies (χ2=31.84,
P<0.0001, I2=75%).
Extrathyroidal extension
Eighteen studies presented the prevalence of cases
with extrathyroidal extension in FV-PTC and C-PTC, which overall
was 15.1 (144/951) and 46.1% (2,157/4,682), respectively, and the
difference was statistically significant (OR, 0.40; 95% CI,
0.25–0.64; P=0.0001; Fig. 2I).
Significant statistical heterogeneity was detected among the
studies (χ2=56.75, P<0.00001, I2=70%).
Lymph node metastasis
Twenty-three studies reported the prevalence of
lymph node metastasis in patients with FV-PTC and C-PTC, which
overall was 22.8 (257/1,125) and 46.4% (2,965/6,386), respectively,
and this difference was statistically significant (OR, 0.35; 95%
CI, 0.25–0.49; P<0.00001; Fig.
2J). Significant statistical heterogeneity was detected among
the studies (χ2=65.94, P<0.00001,
I2=67%).
Lymphocytic and/or Hashimoto's
thyroiditis
Nine studies presented the prevalence of lymphocytic
and/or Hashimoto's thyroiditis in patients with FV-PTC and C-PTC.
The overall prevalence was 19.8 (97/490) and 30.0% (1,279/4,261),
respectively, and the difference was not statistically significant
(OR, 0.79; 95% CI, 0.61–1.02; P=0.07; Fig. 2K). There was no significant
statistical heterogeneity among the studies (χ2=13.94,
P=0.08, I2=43%).
Clinical stage
Twelve studies included clinical stage in their
analyses. The stage of the tumor was I or II in 422/527 (80.1%)
patients with FV-PTC and in 913/1,195 (76.4%) patients with C-PTC;
the difference was not statistically significant (OR, 1.17; 95% CI,
0.0–1.52; P=0.25; Fig. 2L). There was
no significant statistical heterogeneity among the studies
(χ2=10.29, P=0.50, I2=0%).
BRAF mutation
Thirteen studies presented the prevalence of
BRAF mutation in patients with FV-PTC and C-PTC, which
overall was 23.8 (116/487) and 71.7% (2,734/3,814), respectively,
and the difference was statistically significant (OR, 0.19; 95% CI,
0.15–0.24, P<0.00001; Fig. 2M).
There was no significant statistical heterogeneity among the
studies (χ2=8.15, P=0.77, I2=0%).
Recurrence
Eight studies evaluated the recurrence of tumor
while following up patients with FV-PTC and C-PTC for varying
periods. The overall percentage of recurrence was 9.4 (31/329) and
15.8% (129/814), respectively, and the difference was statistically
significant (OR, 0.52; 95% CI, 0.34–0.80; P=0.003; Fig. 2N). There was no significant
statistical heterogeneity among the studies (χ2=5.46,
P=0.60, I2=0%).
Publication bias
Funnel plots and Begg's test were performed to
access the publication bias. All the Begg's funnel plots did not
show evident asymmetry (Begg's funnel plots not shown), and the
results of Egger's test were confirmed for the comparison of
clinical parameters of FV-PTC and C-PTC (all P>0.05 for Egger's
test; Table II). The results of
Begg's funnel plot and Egger's test did not show any publication
bias.
Discussion
Following a systematic review of the recent
literature, it was observed that FV-PTC has been increasingly
diagnosed in recent years, and an increasing amount of research is
being performed concerning FV-PTC. The majority of studies
comparing the clinicopathological behavior of FV-PTC and C-PTC have
limitations, such as inclusion of relatively few cases,
incomprehensive categories of clinical parameters and
single-institution bias. Thus, their conclusions were mutually
conflicting. Therefore, it is necessary to acquire a more
comprehensive view of FV-PTC from population-based studies, and a
meta-analysis can achieve this. To the best of our knowledge, this
is the first study of a meta-analysis comparing the
clinicopathological behavior of FV-PTV and C-PTC.
The findings reveal that the following
clinicopathological parameters are significantly different between
patients with FV-PTC and those with C-PTC: Patient age (≥45 years),
mean tumor size, extrathyroidal extension, lymph node metastasis,
BRAF mutation and recurrence. By contrast, no significant
differences were identified in gender, mean age, tumor size (≥10
mm), multifocality, capsular invasion, vascular invasion,
lymphocytic and/or Hashimoto's thyroiditis, and clinical stage.
Patients with FV-PTC and C-PTC have similarly high
prevalence of females, and this finding is consistent with nearly
all the relevant studies. When analyzing age and tumor size, the
meta-analysis was performed in two ways. The mean age of patients
with FV-PTC was similar to that of patients with C-PTC, but the
former were more likely to be ≥45 years old. The number of patients
with FV-PTC and C-PTC in the analysis of mean age was 656 and 972
(total 1,628) respectively, which is a larger population of
patients in the analysis of age ≥45 years being 219 and 371 (total
590). Logically, the mean age analysis may be more reliable. The
findings were not consistent in the mean tumor size and the
prevalence of tumor size ≥10 mm. The mean tumor size of patients
with FV-PTC was larger than that of the patients with C-PTC, which
is in agreement with the results of studies by Chang et al
(10), Ozdemir et al (17), Burningham et al (19), Jain et al (49) and Kim et al (50). Ozdemir et al (17) and Kim et al (50) also reported that compared to C-PTC,
FV-PTC has more benign sonographic features, a lower incidence of a
sonographically malignant grade and a lower diagnostic rate of PTC
on fine-needle aspiration biopsy (FNAB). Thus, the lower rate of
suspicious findings in FV-PTC lesions may have caused evaluation of
larger FV-PTC lesions by FNAB, resulting in the detection of these
lesions at a later stage. In addition, FV-PTC lesions may have
become larger when patients with FV-PTC underwent surgery. However,
the present study identified that the prevalence of tumor size ≥10
mm was similar between the two types. By contrast, Tielens et
al (5) reported that tumor size
of FV-PTC tends to be smaller than that of C-PTC. The present study
showed similar prevalence of multifocality, capsular invasion,
vascular invasion, lymphocytic and/or Hashimoto's thyroiditis, and
clinical stage between patients with FV-PTC and C-PTC.
The prevalence of the above results has been
controversial. Passler et al (12) suggested that there was a significantly
higher prevalence of multifocality in patients with FV-PTC compared
to patients with C-PTC, but the opposite was reported by Gao et
al (31) and Trovisco et
al (47). Certain studies
reported a higher prevalence of capsular invasion and vascular
invasion in the FV-PTC (10,20,51),
whereas others did not (17,43,47).
Although the majority of the C-PTCs do not have a tumor capsule,
patients with C-PTC (28.1%) and patients with FV-PTC (30.2%) showed
a similar high prevalence of capsular invasion of tumor in the
present meta-analysis. As C-PTC is more inclined to show
infiltrative growth, the tumor easily invades the capsule once
containing the tumor capsule. When histopathologically comparing
the presence of concomitant lymphocytic and/or Hashimoto's
thyroiditis in patients with FV-PTC and C-PTC, Tielens et al
(5) reported a higher rate in the
former, whereas Yuksel et al (16) reported a higher rate in the
latter.
Nearly all the relevant literature on clinical
stages shows the same ratio of clinical stage I + II in patients
with FV-PTC and C-PTC, thereby suggesting that clinical stages of
patients with FV-PTC and C-PTC are similar. The present
meta-analysis reveals that the incidence of associated
extrathyroidal extension, lymph node metastases, BRAF
mutation and recurrence is significantly lower in patients with
FV-PTC compared to patients with C-PTC. As described in the
majority of the studies, the frequencies of extrathyroidal
extension and lymph node metastases are lower in patients with
FV-PTC compared to patients with C-PTC; however, a few studies
reported opposing findings (20,24).
Consistently, all the relevant studies on the BRAF gene
shows the lower ratio of BRAF mutation in patients with
FV-PTC compared to patients with C-PTC. The majority of
meta-analysis studies showed that the BRAF mutation was
associated with the majority of vital clinicopathological
characteristics in PTC, and the BRAF mutation may be used as
an important prognostic marker of patients with PTC (52–56).
However, when analyzing FV-PTC and C-PTC respectively, Gao et
al (31) and Oler et al
(42) identified that the BRAF
mutation was associated with the clinicopathological
characteristics in patients with C-PTC, but not in patients with
FV-PTC.
After the similar follow-up periods, the rate of
recurrence in patients with FV-PTC was significantly lower than
that in the patients with C-PTC, which may be associated with the
above finding that patients with FV-PTC are at a lower risk of
extrathyroidal extension, lymph node metastases or BRAF
mutation. Aggressive clinicopathological behavior of patients with
PTC is associated with old age, and include the following: Presence
of extrathyroidal extension, lymph node metastases, advanced
clinical stages and BRAF mutation. Therefore, poor prognosis
in patients with PTC is associated with certain aggressive
clinicopathological characteristics. Therefore, patients with
FV-PTC have an improved prognosis compared to patients with C-PTC.
However, it may be affected by treatment factors such as type of
surgery, I-131 ablation and use of external radiotherapy.
Patients with FV-PTC have a lower prevalence of
extrathyroidal extension, lymph node metastases, BRAF
mutation and recurrence compared to patients with C-PTC. The mean
tumor size is larger and the incidence of patients aged ≥45 years
are higher in the former. Thus, as reported in a previous study
(8) and in the present meta-analysis,
patients with FV-PTC exhibit a more favorable clinicopathological
behavior and improved prognosis compared to patients with C-PTC.
Thus, the lower incidence of extrathyroidal extension, lymph node
metastases, BRAF mutation and recurrence would appear to be
distinct clinicopathological behavior of FV-PTC. Patients with
FV-PTC and C-PTC are clearly two different groups. As was also
reported by Yu et al (57) and
Chang et al (10), the
clinicopathological behavior of FV-PTC is unique and represents an
intermediate entity between C-PTC and FTC. Different approaches may
be used for their clinical management. More invasive treatment
strategies, such as total thyroidectomy or central lymph node
dissection, may be considered in patients with C-PTC presenting
extrathyroidal extension, lymph node metastasis or BRAF
mutation to decrease recurrence.
The present study has several limitations. One
primary limitation is that reporting of FV-PTC is not a standard
practice in certain hospitals, leading to a reporting bias. There
may be an interpretational difference among pathologists, as FV-PTC
may be confused with FTC. Additionally, stratified analyses of
summary data from the reported studies could not be performed, and
the present study was unable to identify the diverse sources of
heterogeneity of the effect size. In addition, multiple outcome
variables require cautious interpretation as the outcomes may be
interrelated. For instance, the patients with extrathyroidal
extension tend to have a more advanced clinical stage and a higher
risk of recurrence than those with no extension. However, this
limitation is unlikely to have a significant impact on the present
study as the sample size in the meta-analysis is sufficiently
large.
The meta-analysis suggested that, patients with
FV-PTC present more favorable clinicopathological behaviors and
improved prognosis than patients with C-PTC. Patients with FV-PTC
and C-PTC may be managed differently, and the two types of PTC
should be clearly distinguished in future retrospective or
prospective studies. For instance, it may not be necessary for
patients with FV-PTC to undertake the invasive strategies that are
appropriate in patients with C-PTC, if the FV-PTC is diagnosed
prior to or during surgery. However, more valuable studies on a
large cohort of cases are required to evaluate the
clinicopathological behavior in patients with FV-PTC and patients
with C-PTC.
Acknowledgements
The present study was supported by a grant from the
Department of Sichuan Province, Science and Technology Support
Program (no. 2013SZ0041).
References
|
1
|
Howlader N, Noone AM, Krapcho M, Garshell
J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,
Mariotto A, Lewis DR, Chen HS, Feuer EJ and Cronin KA: SEER Cancer
Statistics Review. 1975–2011, National Cancer Institute; Bethesda,
MD: http://seer.cancer.gov/csr/1975_2011/September
17–2014
|
|
2
|
Sipos JA and Mazzaferri EL: Thyroid cancer
epidemiology and prognostic variables. Clin Oncol (R Coll Radiol).
22:395–404. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Carcangiu ML, Zampi G, Pupi A, Castagnoli
A and Rosai J: Papillary carcinoma of the thyroid = A
clinicopathologic study of 241 cases treated at the University of
Florence, Italy. Cancer. 55:805–828. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Albores-Saavedra J and Wu J: The many
faces and mimics of papillary thyroid carcinoma. Endocr Pathol.
17:1–18. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tielens ET, Sherman SI, Hruban RH and
Ladenson PW: Follicular variant of papillary thyroid carcinoma: a
clinicopathologic study. Cancer. 73:424–431. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sebastian SO, Gonzalez JM, Paricio PP,
Perez JS, Flores DP, Madrona AP, Romero PR and Tebar FJ: Papillary
thyroid carcinoma: prognostic index for survival including the
histological variety. Arch Surg. 135:272–277. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zidan J, Karen D, Stein M, Rosenblatt E,
Basher W and Kuten A: Pure versus follicular variant of papillary
thyroid carcinoma: clinical features, prognostic factors, treatment
and survival. Cancer. 97:1181–1185. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lang BH, Lo CY, Chan WF, Lam AK and Wan
KY: Classical and follicular variant of papillary thyroid
carcinoma: a comparative study on clinicopathologic features and
long-term outcome. World J Surg. 30:752–758. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lam AK, Lo CY and Lam KS: Papillary
carcinoma of thyroid: A 30-yr clinicopathological review of the
histological variants. Endocr Pathol. 16:323–330. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chang HY, Lin JD, Chou SC, Chao TC and
Hsueh C: Clinical presentations and outcomes of surgical treatment
of follicular variant of the papillary thyroid carcinomas. Jpn J
Clin Oncol. 36:688–693. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lin HW and Bhattacharyya N: Clinical
behavior of follicular variant of papillary thyroid carcinoma:
presentation and survival. Laryngoscop. 120:712–716. 2010.
View Article : Google Scholar
|
|
12
|
Passler C, Prager G, Scheuba C, Niederle
BE, Kaserer K, Zettinig G and Niederle B: Follicular variant of
papillary thyroid carcinoma: a long-term follow-up. Arch Surg.
138:1362–1366. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Crile GJ and Hazard JB: Relationship of
the age of the patient to the natural history and prognosis of
carcinoma of the thyroid. Ann Surg. 138:33–38. 1953. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ertek S, Yilmaz NC, Cicero AF, Vurupalmaz
O, Demiroz AS and Erdogan G: Increasing diagnosis of thyroid
papillary carcinoma follicular variant in south-east Anatolian
region: comparison of characteristics of classical papillary and
follicular variant thyroid cancers. Endocr Pathol. 23:157–160.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
LiVolsi VA and Asa SL: The demise of
follicular carcinoma of the thyroid gland. Thyroid. 4:233–236.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yuksel O, Kurukahvecioglu O, Ege B, Ekinci
O, Aydin A, Poyraz A, Tezel E and Taneri F: The relation between
pure papillary and follicular variant in papillary thyroid
carcinoma. Endocr Regul. 42:29–33. 2008.PubMed/NCBI
|
|
17
|
Ozdemir D, Ersoy R, Cuhaci N, Arpaci D,
Ersoy EP, Korukluoglu B, Guler G and Cakir B: Classical and
follicular variant papillary thyroid carcinoma: comparison of
clinical, ultrasonographical, cytological and histopathological
features in 444 patients. Endocr Pathol. 22:58–65. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Cheng S, Serra S, Mercado M, Ezzat S and
Asa SL: A high-throughput proteomic approach provides distinct
signatures for thyroid cancer behavior. Clin Cancer Res.
17:2385–2394. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Burningham AR, Krishnan J, Davidson BJ,
Ringel MD and Burman KD: Papillary and follicular variant of
papillary carcinoma of the thyroid: Initial presentation and
response to therapy. Otolaryngol Head Neck Surg. 132:840–844. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hagag P, Hod N, Kummer E, Cohenpour M,
Horne T and Weiss M: Follicular variant of papillary thyroid
carcinoma: clinical-pathological characterization and long-term
follow-up. Cancer J. 12:275–282. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Stroup DF, Berlin JA, Morton SC, Olkin I,
Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA and Thacker
SB: Meta-analysis of observational studies in epidemiology: a
proposal for reporting. Meta-analysis of observational studies in
epidemiology (MOOSE) group. JAMA. 283:20082012. View Article : Google Scholar
|
|
22
|
Abrosimov A, Saenko V, Meirmanov S,
Nakashima M, Rogounovitch T, Shkurko O, Lushnikov E, Mitsutake N,
Namba H and Yamashita S: The cytoplasmic expression of MUC1 in
papillary thyroid carcinoma of different histological variants and
its correlation with cyclin D1 overexpression. Endocr Pathol.
18:68–75. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Brzezianska E, Pastuszak-Lewandoska D,
Wojciechowska K, Migdalska-Sek M, Cyniak-Magierska A, Nawrot E and
Lewinski A: Investigation of V600E BRAF mutation in papillary
thyroid carcinoma in the Polish population. Neuro Endocrinol Lett.
28:351–359. 2007.PubMed/NCBI
|
|
24
|
Costa AM, Herrero A, Fresno MF, Heymann J,
Alvarez JA, Cameselle-Teijeiro J and Garcia-Rostan G: BRAF mutation
associated with other genetic events identifies a subset of
aggressive papillary thyroid carcinoma. Clin Endocrinol (Oxf).
68:618–634. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Daglar-Aday A, Toptas B, Ozturk T, Seyhan
F, Saygili N, Eronat AP, Akadam-Teker B, Yilmaz-Aydogan H, Aksoy F
and Ozturk O: Investigation of BRAF V600E mutation in papillary
thyroid carcinoma and tumor-surrounding nontumoral tissues. DNA
Cell Biol. 32:13–18. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Darr EA, Patel AD, Yu G, Komorowski Z,
McCormick S, Tiwari R, Schantz SP and Geliebter J: Reduced Cx43 gap
junction plaque expression differentiates thyroid carcinomas from
benign disease. Arch Otolaryngol Head Neck Surg. 137:1161–1165.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Dettmer M, Perren A, Moch H, Komminoth P,
Nikiforov YE and Nikiforova MN: Comprehensive MicroRNA expression
profiling identifies novel markers in follicular variant of
papillary thyroid carcinoma. Thyroid. 23:1383–1389. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Di Cristofaro J, Marcy M, Vasko V, Sebag
F, Fakhry N, Wynford-Thomas D and De Micco C: Molecular genetic
study comparing follicular variant versus classic papillary thyroid
carcinomas: association of N-ras mutation in codon 61 with
follicular variant. Hum Pathol. 37:824–830. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Eloy C, Santos J, Soares P and
Sobrinho-Simoes M: The preeminence of growth pattern and
invasiveness and the limited influence of BRAF and RAS mutations in
the occurrence of papillary thyroid carcinoma lymph node
metastases. Virchows Arch. 459:265–276. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Espadinha C, Santos JR, Sobrinho LG and
Bugalho MJ: Expression of iodine metabolism genes in human thyroid
tissues: evidence for age and BRAFV600E mutation dependency. Clin
Endocrinol (Oxf). 70:629–635. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Gao WL, Wie LL, Chao YG, Wie L and Song
TL: Prognostic prediction of BRAF (V600E) and its relationship with
sodium iodide symporter in classic variant of papillary thyroid
carcinomas. Clin Lab. 58:919–926. 2012.PubMed/NCBI
|
|
32
|
Hunt JL, Fowler M, Lomago D, Niehouse L,
Sasatomi E, Swalsky P and Finkelstein S: Tumor suppressor gene
allelic loss profiles of the variants of papillary thyroid
carcinoma. Diagn Mol Pathol. 13:41–46. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Igci YZ, Erkilic S, Igci M and Arslan A:
MCM3 Protein expression in follicular and classical variants of
papillary thyroid carcinoma. Pathol Oncol Res. 20:87–91. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Igci YZ, Erkilic S and Arslan A: Septin 7
immunoexpression in papillary thyroid carcinoma: a preliminary
study. Pathol Res Pract. 210:426–431. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Ito Y, Hirokawa M, Uruno T, Kihara M,
Higashiyama T, Takamura Y, Miya A, Kobayashi K, Matsuzuka F and
Miyauchi A: Prevalence and biological behaviour of variants of
papillary thyroid carcinoma: experience at a single institute.
Pathology. 40:617–622. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Lassalle S, Hofman V, Ilie M, Bonnetaud C,
Puissegur MP, Brest P, Loubatier C, Guevara N, Bordone O, Cardinaud
B, Lebrigand K, Rios G, Santini J, Franc B, Mari B, Al Ghuzlan A,
Vielh P, Barbry P and Hofman P: Can the microRNA signature
distinguish between thyroid tumors of uncertain malignant potential
and other well-differentiated tumors of the thyroid gland? Endocr
Relat Cancer. 18:579–594. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Lee S, Han BK, Ko EY, Oh YL, Choe JH and
Shin JH: The ultrasonography features of hyalinizing trabecular
tumor of the thyroid are more consistent with its benign behavior
than cytology or frozen section readings. Thyroid. 21:253–259.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Lim JY, Hong SW, Lee YS, Kim BW, Park CS,
Chang HS and Cho JY: Clinicopathologic implications of the BRAF
(V600E) mutation in papillary thyroid cancer: a subgroup analysis
of 3130 cases in a single center. Thyroid. 23:1423–1430. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Liu Z, Liu D, Bojdani E, El-Naggar AK,
Vasko V and Xing M: IQGAP1 plays an important role in the
invasiveness of thyroid cancer. Clin Cancer Res. 16:6009–6018.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Min HS, Lee C and Jung KC: Correlation of
immunohistochemical markers and BRAF mutation status with
histological variants of papillary thyroid carcinoma in the Korean
population. J Korean Med Sci. 28:534–541. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Nechifor-Boila A, Borda A, Sassolas G,
Hafdi-Nejjari Z, Borson-Chazot F, Lifante J, C, Sturm N, Laverriere
MH, Berger N and Decaussin-Petrucci M: Immunohistochemical markers
in the diagnosis of papillary thyroid carcinomas: The promising
role of combined immunostaining using HBME-1 and CD56. Pathol Res
Pract. 209:585–592. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Oler G and Cerutti JM: High prevalence of
BRAF mutation in a Brazilian cohort of patients with sporadic
papillary thyroid carcinomas: correlation with more aggressive
phenotype and decreased expression of iodide-metabolizing genes.
Cancer. 115:972–980. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Rivera M, Tuttle RM, Patel S, Shaha A,
Shah JP and Ghossein RA: Encapsulated papillary thyroid carcinoma:
a clinico-pathologic study of 106 cases with emphasis on its
morphologic subtypes (histologic growth pattern). Thyroid.
19:119–127. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Schulten HJ, Salama S, Al-Mansouri Z,
Alotibi R, Al-Ghamdi K, Al-Hamour OA, Sayadi H, Al-Aradati H,
Al-Johari A, Huwait E, Gari M, Al-Qahtani MH and Al-Maghrabi J:
BRAF mutations in thyroid tumors from an ethnically diverse group.
Hered Cancer Clin Pract. 10:102012. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Sheu SY, Grabellus F, Schwertheim S, Worm
K, Broecker-Preuss M and Schmid KW: Differential miRNA expression
profiles in variants of papillary thyroid carcinoma and
encapsulated follicular thyroid tumours. Br J Cancer. 102:376–382.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Slosar M, Vohra P, Prasad M, Fischer A,
Quinlan R and Khan A: Insulin-like growth factor mRNA binding
protein 3 (IMP3) is differentially expressed in benign and
malignant follicular patterned thyroid tumors. Endocr Pathol.
20:149–157. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Trovisco V, Soares P, Preto A, de Castro
IV, Lima J, Castro P, Maximo V, Botelho T, Moreira S, Meireles AM,
Magalhaes J, Abrosimov A, Cameselle-Teijeiro J and Sobrinho-Simoes
M: Type and prevalence of BRAF mutations are closely associated
with papillary thyroid carcinoma histotype and patients' age but
not with tumour aggressiveness. Virchows Arch. 446:589–595. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Wreesmann VB, Ghossein RA, Hezel M,
Banerjee D, Shaha AR, Tuttle RM, Shah JP, Rao PH and Singh B:
Follicular variant of papillary thyroid carcinoma: genome-wide
appraisal of a controversial entity. Genes Chromosomes Cancer.
40:355–364. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Jain M, Khan A, Patwardhan N, Reale F and
Safran M: Follicular variant of papillary thyroid carcinoma: a
comparative study of histopathologic features and cytology results
in 141 patients. Endocr Pract. 7:79–84. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Kim DS, Kim JH, Na DG, Park SH, Kim E,
Chang KH, Sohn CH and Choi YH: Sonographic features of follicular
variant papillary thyroid carcinomas in comparison with
conventional papillary thyroid carcinomas. J Ultrasound Med.
28:1685–1692. 2009.PubMed/NCBI
|
|
51
|
Salajegheh A, Petcu EB, Smith RA and Lam
AK: Follicular variant of papillary thyroid carcinoma: a diagnostic
challenge for clinicians and pathologists. Postgrad Med J.
84:78–82. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Lee JH, Lee ES and Kim YS:
Clinicopathologic significance of BRAF V600E mutation in papillary
carcinomas of the thyroid: a meta-analysis. Cancer. 110:38–46.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Kim TH, Park YJ, Lim JA, Ahn HY, Lee EK,
Lee YJ, Kim KW, Hahn SK, Youn YK, Kim KH, Cho BY and Park do J: The
association of the BRAF (V600E) mutation with prognostic factors
and poor clinical outcome in papillary thyroid cancer: a
meta-analysis. Cancer. 118:1764–1773. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Tufano RP, Teixeira GV, Bishop J, Carson
KA and Xing M: BRAF mutation in papillary thyroid cancer and its
value in tailoring initial treatment: a systematic review and
meta-analysis. Medicine (Baltimore). 91:274–286. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Li C, Lee KC, Schneider EB and Zeiger MA:
BRAF V600E mutation and its association with clinicopathological
features of papillary thyroid cancer: a meta-analysis. J Clin
Endocrinol Metab. 97:4559–4570. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Liu X, Yan K, Lin X, Zhao L, An W, Wang C
and Liu X: The association between BRAF V600E mutation and
pathological features in PTC. Eur Arch Otorhinolaryngol. 271:Jan
4–2014.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Yu XM, Schneider DF, Leverson G, Chen H
and Sippel RS: Follicular variant of papillary thyroid carcinoma is
a unique clinical entity: a population-based study of 10,740 cases.
Thyroid. 23:1263–1268. 2013. View Article : Google Scholar : PubMed/NCBI
|