Introduction
Colorectal cancer (CRC) is a common malignancy of
the gastrointestinal tract, which is fourth in incidence and second
in terms of cancer-related mortality in America (1). Several factors and genes are associated
with the process of tumor angiogenesis, invasion, growth and
metastasis in CRC. A number of stage III/IV patients succumb to
metastasis and stage II patients to recurrence, particularly in the
liver, lungs and lymph nodes (2).
Despite the advances in identifying high-risk factors for
recurrence in stage II CRC patients, the benefit from chemotherapy
administration remains uncertain (3–5).
Over the last few decades, microsatellite
instability (MSI) has been identified as a biomarker in previous
clinical trials (4,5), which demonstrated that patients with MSI
treated with 5-fluorouracil exhibited a significant survival
benefit compared with the non-MSI and the surgery alone groups.
Numerous tumor cell-derived factors and microenvironment molecules,
such as chemokines, are involved in cancer cell metastasis and
migration (6,7). Chemokines (8–10 kDa) are chemotactic
cytokines that cause directed migration of numerous cells,
including leukocytes, and are induced by inflammatory cytokines,
growth factors and pathogenic stimuli. The chemokine-receptor axis
allows cells to move towards high local concentrations of
chemokines during inflammation, as well as the homeostatic
transport of lymphocytes and dentritic cells. To date, >50
chemokines and 20 seven-transmembrane-domain receptors, which
belong to G-protein coupled families, have been identified. One
receptor may generally bind to more than one cytokines. A number of
human cancers characterized by leukocyte infiltration possess a
complex chemokine network that affects tumor cell growth, survival,
infiltration, migration and angiogenesis.
Latest research demonstrated that the expression of
the majority of chemokines and their receptors, such as
CXCL10/CXCR3, CXCL12/CXCR4, CCL21/CCR7 and CCL25/CCR9, is
associated with CRC. Dwinell et al (8) reported that CXCR3 is not present in
normal colonic epithelial cells, but in mononuclear cells in the
lamina propria. Kawada et al (9) observed that CXCL10 enhances CRC cell
survival and gelatinase expression in culture and upregulates cell
surface expression of CXCR3. Furthermore, CXCL10 has been found to
be overexpressed in several cases of CRC as a Ras target gene
(10), although Jiang et al
(11) reported opposite findings. It
appears that chemokines exert their tumor-associated activies by
inducing immune-stimulating and angiostatic effects and
constituting the tumor microenviroment. However, the precise role
of CXCL10/CXCR3 in solid cancers remains poorly understood.
The aim of the present study was to investigate
CXCL10 and CXCR3 expression in stage II CRC, in order to determine
its clinicopathological significance and role in disease recurrence
and optimise postoperative treatment in patients with stage II
CRC.
Patients and methods
Patients and materials
A series of 401 stage II CRC patients who underwent
radical resection at Tianjin Medical University Cancer Institute
and Hospital between 2005 and 2009 were included in this study.
None of the patients had received preoperative neoadjuvant
chemotherapy or radiotherapy. The patients were divided into two
groups, the recurrence group (RG) and the non-recurrence group
(NRG). We collected paraffin-embedded samples from 71 recurrent
cases, 12 non-recurrent cases and 10 normal tissue samples. All the
samples were independently reviewed by two pathologists and the
histological diagnoses were classified according to the 2010 World
Health Organization Classification of Digestive System Tumors
(12). The recurrence risk factors of
stage II CRC according to the guidelines of the National
Comprehensive Cancer Network included poor differentiation, lymph
node or blood vessel infiltration, intestinal obstruction, <12
lymph nodes retrieved, perineural invasion, partial perforation and
positive resection margin. The term inflammatory adhesions refers
to tumors found to be attached to the surrouding tissues during
surgery, although no cancer cell infiltration is later identified
on pathological examination.
Immunohistochemical analysis
Tumor samples were collected from the Tianjin
Medical University Cancer Institute and Hospital (Tianjin, China),
fixed in formalin, embedded in paraffin and sectioned at 4 µm. A
polyclonal rabbit anti-human CXCL10 antibody (cat. no. (C-20)
sc-6226; dilution, 1:120; Santa Cruz Biotechnology, Inc., Santa
Cruz, CA, USA) and polyclonal rabbit anti-human CXCR3 antibody
(cat. no. sc-101500; dilution, 1:200) were separately added to the
sections following deparaffinization, hydration, antigen repair and
endogenous peroxidase blocking. Immunoperoxidase staining was
performed with the two-step EnVision™ method (DakoCytomation,
Glostrup, Denmark) according to the manufacturer's instructions and
visualized with 3,3′-diaminobenzidine (Sigma, St. Louis, MO, USA).
The phosphate-buffered saline buffer was used to prepare negative
control samples. Cell membrane and cytoplasmic staining were
measured for these antibodies. Two pathologists independently
counted the positive cells. The 4-tiered scoring system
(−/+/++/+++), which took into account the percentage of positive
cells and staining intensity, was used in our evaluation. The
expression level of a certain target was determined according to
the respective median values of a tumor indicator. Lower than the
median was defined as ‘low expression’ and higher as ‘strong
expression’.
Follow-up
Follow-up data were collected through telephone
communication and from the database of the Medical Records
Department of our hospital. The time interval from the operative
date to clinical relapse was defined as the disease-free survival
(DFS), and to death or last follow-up as overall survival (OS).
Statistical analysis
All the data were analyzed using SPSS 17.0 software
(SPSS Inc., Chicago, IL, USA). The t-test and analysis of variance
were used for numerical variables and the χ2 test for
qualitative variables. For survival analysis, survival curves were
generated by the Kaplan-Meier method. The univariate survival
analysis was performed using the log-rank test and the multivariate
Cox proportional hazards model was used to identify the independent
prognostic factors. P<0.05 was considered to indicate
statistically significant differences.
Results
Clinicopathological
characteristics
A total of 229 male and 172 female patients, aged
7–87 years (mean age, 60.5 years), were initially included in the
study. Of these, 54.86% (220/401) had colon cancer, 45.89%
(181/401) had rectal cancer. Patients with colon cancer exhibited a
survival advantage compared with those with rectal cancer
(P=0.026). The general classification was ulcerated type in
288/401, elevated type in 111/401, colloid type in 1/401 and
infiltrative type in 1/401. The pathological results of all kinds
of carcinomas were adenoma, histologically classified as tubular
(n=198), papillary (n=15), mucinous (n=25) and mixed (n=54). Of the
401 cases, 22 were classified as well-differentiated, 335 as
moderately differentiated and 44 as poorly differentiated. A
maximum diameter of >10 cm was observed in 4.99% (20/401) of the
cases, with a significantly different DFS compared with cases with
smaller tumors (P<0.051). In 91 cases, inflammatory adhesions to
the surrounding tissues were identified, which statistically
significantly affected OS (P=0.024), but not DFS (P=0.214). A
backward Cox's proportional hazards regression analysis of the
clinicopathological parameters yielded a hazard ratio of 1.823 (95%
confidence interval: 1.093–3.039; P=0.013) for adhesion-positive
compared with adhesion-negative patients. Patients with more risk
factors exhibited shorter DFS and OS (P<0.05). The multivariate
Cox analysis indicated that location, tumor size and the number of
high-risk factors were independent variables (P=0.013, 0.033 and
0.036), as was the presence of inflammatory adhesions, and were all
significant prognostic factors for poor OS (Table IA and B). Colon cancer patients with
larger tumors who had >1 high-risk factor and inflammatory
adhesions were more likely to succumb to the disease.
 | Table I.Comparison of clinicopathological
characteristics in stage II colorectal cancer patients undergoing
potentially curative resection. |
Table I.
Comparison of clinicopathological
characteristics in stage II colorectal cancer patients undergoing
potentially curative resection.
| A,
Clinicopathological characteristics |
|
|
|
|
|
|
|
|---|
|
|---|
|
|
| Survival status | Recurrence
status |
|---|
|
|
|
|
|
|---|
| Variables | Total (n=401) | Alive (n=325) | Deceased (n=76) | P-valuea | No recurrence | Recurrence | P-valuea |
|---|
| Gender |
|
|
| 0.320 |
|
| 0.681 |
| Male | 229 | 182 | 47 |
| 167 | 62 |
|
|
Female | 172 | 143 | 29 |
| 128 | 44 |
|
| Age, years |
|
|
| 0.341 |
|
| 0.721 |
| ≤60 | 199 | 166 | 33 |
| 149 | 50 |
|
|
>60 | 202 | 159 | 43 |
| 146 | 56 |
|
| Location |
|
|
| 0.026b |
|
| 0.101 |
|
Colon | 220 | 187 | 33 |
| 169 | 51 |
|
|
Rectum | 181 | 138 | 43 |
| 125 | 54 |
|
| General
classification |
|
|
| 0.551 |
|
| 0.515 |
|
Ulcerated | 288 | 229 | 59 |
| 206 | 82 |
|
|
Elevated | 111 | 94 | 17 |
| 87 | 24 |
|
|
Other | 2 | 2 | 0 |
| 2 | 0 |
|
| Tumor size, cm |
|
|
| 0.031b |
|
| 0.051 |
|
≤10 | 381 | 312 | 69 |
| 283 | 98 |
|
|
>10 | 20 | 13 | 7 |
| 8 | 12 |
|
| Stage |
|
|
| 0.179 |
|
| 0.441 |
|
IIA | 71 | 59 | 12 |
| 55 | 16 |
|
|
IIB | 323 | 262 | 61 |
| 236 | 87 |
|
|
IIC | 7 | 4 | 3 |
| 4 | 3 |
|
| Recurrence risk
factors |
|
|
| 0.009b |
|
|
<0.001b |
|
None | 75 | 63 | 12 |
| 56 | 19 |
|
| 1 | 276 | 229 | 47 |
| 208 | 68 |
|
| ≥2 | 50 | 33 | 17 |
| 31 | 19 |
|
| Preoperative
CEA |
|
|
| 0.838 |
|
| 0.205 |
|
Abnormal | 28 | 23 | 5 |
| 18 | 10 |
|
|
Normal | 373 | 302 | 71 |
| 277 | 96 |
|
| Anemia |
|
|
| 0.731 |
|
| 0.952 |
| No | 300 | 242 | 58 |
| 221 | 79 |
|
|
Yes | 101 | 83 | 18 |
| 74 | 27 |
|
| Family history |
|
|
| 0.528 |
|
| 0.295 |
| No | 327 | 263 | 64 |
| 235 | 90 |
|
|
Yes | 74 | 62 | 12 |
| 58 | 16 |
|
| Inflammatory
adhesions |
|
|
| 0.024b |
|
| 0.214 |
| No | 310 | 258 | 52 |
| 232 | 78 |
|
|
Yes | 91 | 67 | 24 |
| 63 | 28 |
|
|
| B, Uni- and
multivariate Cox proportional hazards model for overall survival in
stage II colorectal cancer patients |
|
| Variables | B | SE | Wald |
P-valuea | Exp (B) | 95% CI |
|
| Location | −0.622 | 0.250 | 6.184 | 0.013b | 0.537 | 0.329–0.877 |
| Tumor size | 0.455 | 0.213 | 4.562 | 0.033b | 1.577 | 1.038–2.395 |
| Recurrence risk
factors | 0.432 | 0.206 | 4.395 | 0.036b | 1.540 | 1.029–2.307 |
| Inflammatory
adhesion | 0.600 | 0.261 | 5.298 | 0.013b | 1.823 | 1.093–3.039 |
From the follow-up data, we identified 106 patients
with relapse or metastasis, with a median DFS of 21.8 months and a
median OS of 39.6 months. The follow-up time ranged from 2 to 36
months. Of the 401 patients, 286 survived without evidence of
cancer, 39/401 remained alive with recurrent lesions, 67/401
succumbed to CRC and 9/401 succumbed due to other causes.
Inflammatory adhesions
In the RG, only the presence of inflammatory
adhesions was associated with OS (P=0.025) (Table II). However, there was no such
association with the remaining characteristics. A total of 28
(28/106) of the relapsed patients exhibited inflammatory adhesions
surrounding the tumor and the majority survived for <3 years
[67.86 (19/28)]. The median survival time of relapsed patients with
adhesions was 26.63 months, while in the NRG it was 61.67 months.
It is considered that adhesion had been reported previously to OS.
It was concluded that the presence of inflammatory adhesions in a
proportion of the patients was not associated with recurrence, but
was closely associated with OS; however, for patients who presented
with adhesions as well as recurrence, the prognosis was worse.
 | Table II.Correlation between the
clinicopathological characteristics of relapsed patients and
overall survival. |
Table II.
Correlation between the
clinicopathological characteristics of relapsed patients and
overall survival.
|
Characteristics |
P-valuea |
|---|
| Imflammatory
adhesions | 0.025b |
| General
classification | 0.314 |
| Recurrence risk
factors | 0.194 |
| Tumor size | 0.516 |
| Gender | 0.487 |
| Age | 0.931 |
| N stage | 0.266 |
| Preoperative CEA
level | 0.218 |
| Preoperative Hb
level | 0.295 |
| Tumor location | 0.309 |
| Family history | 0.859 |
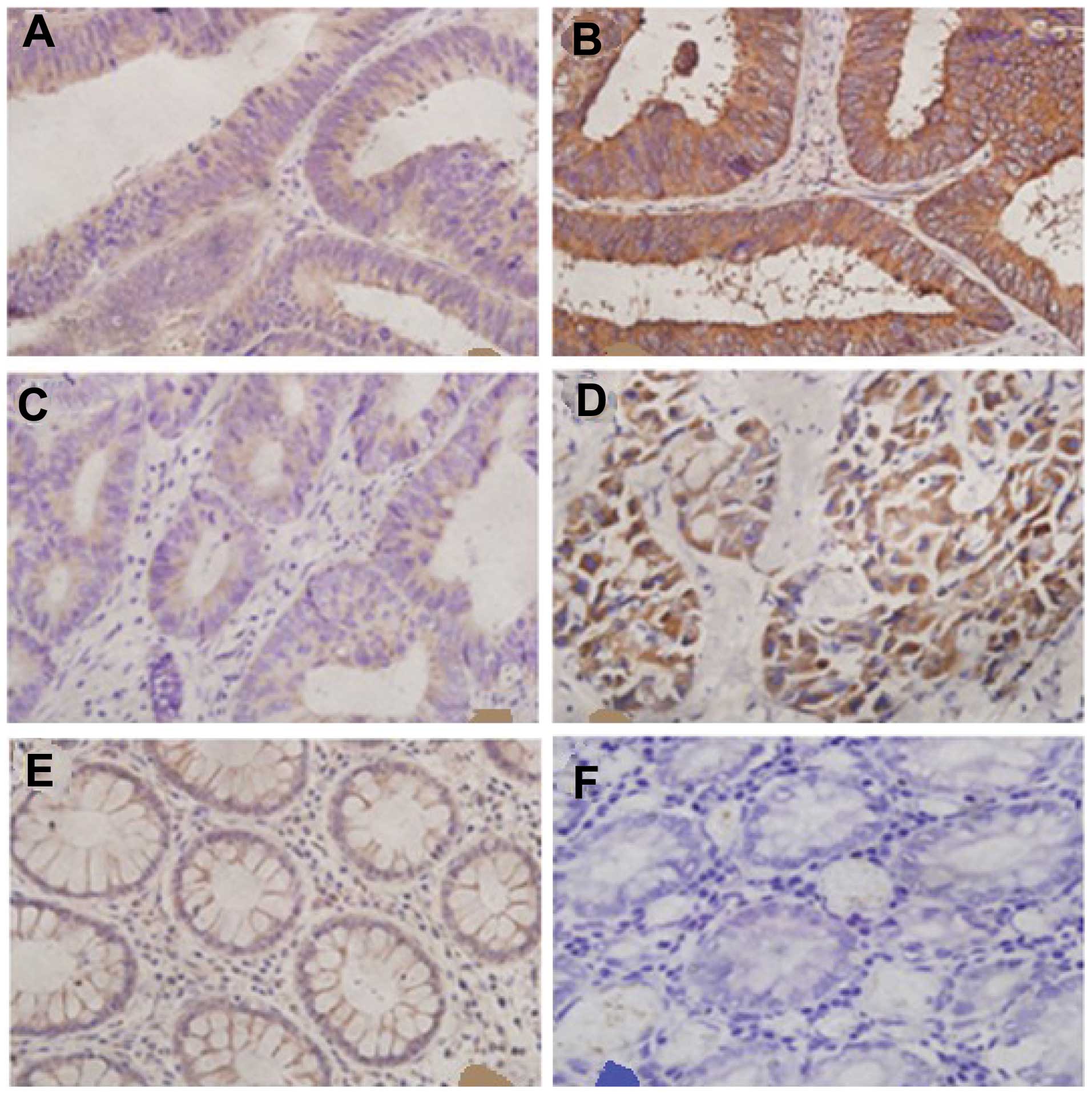
Immunohistochemistry (IHC) in CRC
Immunostaining with anti-CXCL10 or -CXCR3 was
considered to be antibody-specific by using the immunising peptide
for each antibody as the target. In order to elucidate the
association between clinical characteristics and the CXCL10/CXCR3
axis, we examined 143 CRC specimens and 10 peritumoral tissues at a
distance of ≥5 cm from the resection margin (normal intestinal
epithelia). CXCL10 and CXCR3 exhibited distinct characteristics in
each group (Fig. 1).
As determined by IHC, CXCL10 was poorly expressed in
36 out of 72 cases (50.0%) in NRG and 19 out of 71 cases (26.76%)
in RG, as well as strongly expressed in 10 out of 72 cases (13.89%)
in the NRG and 27 out of 71 cases (38.03%) in the RG. We also found
that 48 samples (66.67%) exhibited low CXCR3 expression in the NRG
and 21 samples (29.58%) in the RG, whereas 12 cases (16.90%)
exhibited high CXCR3 expression in the RG and 2 (2.78%) in the NRG.
In the normal group, none of the normal tissue samples expressed
CXCR3, whereas 6 samples poorly expressed CXCL10. The remaining
pathological sections were not stained by the specific antibodies
(Tables III and IV). There was a significant difference
beween normal tissues and CRC RG or NRG in terms of CXCL10 and
CXCR3 expression (P<0.05).
 | Table III.Immunostaining for CXCL10 and CXCR3
expression in normal and CRC tissues. |
Table III.
Immunostaining for CXCL10 and CXCR3
expression in normal and CRC tissues.
|
| CXCL10 | CXCR3 |
|---|
|
|
|
|
|---|
| Variable | Negative | Low | Strong | Negative | Low | Strong |
|---|
| CRC (n=143) | 51 | 55 | 37 | 60 | 69 | 14 |
| Normal tissue
(n=10) | 4 | 6 | 0 | 10 | 0 | 0 |
|
P-valuea |
| 0.145 |
|
| 0.002b |
|
 | Table IV.Immunostaining for CXCL10 and CXCR3
in colorectal cancer (negative expression samples are absent). |
Table IV.
Immunostaining for CXCL10 and CXCR3
in colorectal cancer (negative expression samples are absent).
| Variable | Recurrence group
(n=71) | Non-recurrence
group (n=72) |
P-valuea |
|---|
| CXCL10 |
|
| 0.001b |
| Low
expression | 19 | 36 |
|
| Strong
expression | 27 | 10 |
|
| CXCR3 |
|
|
<0.001b |
| Low
expression | 21 | 48 |
|
| Strong
expression | 12 | 2 |
|
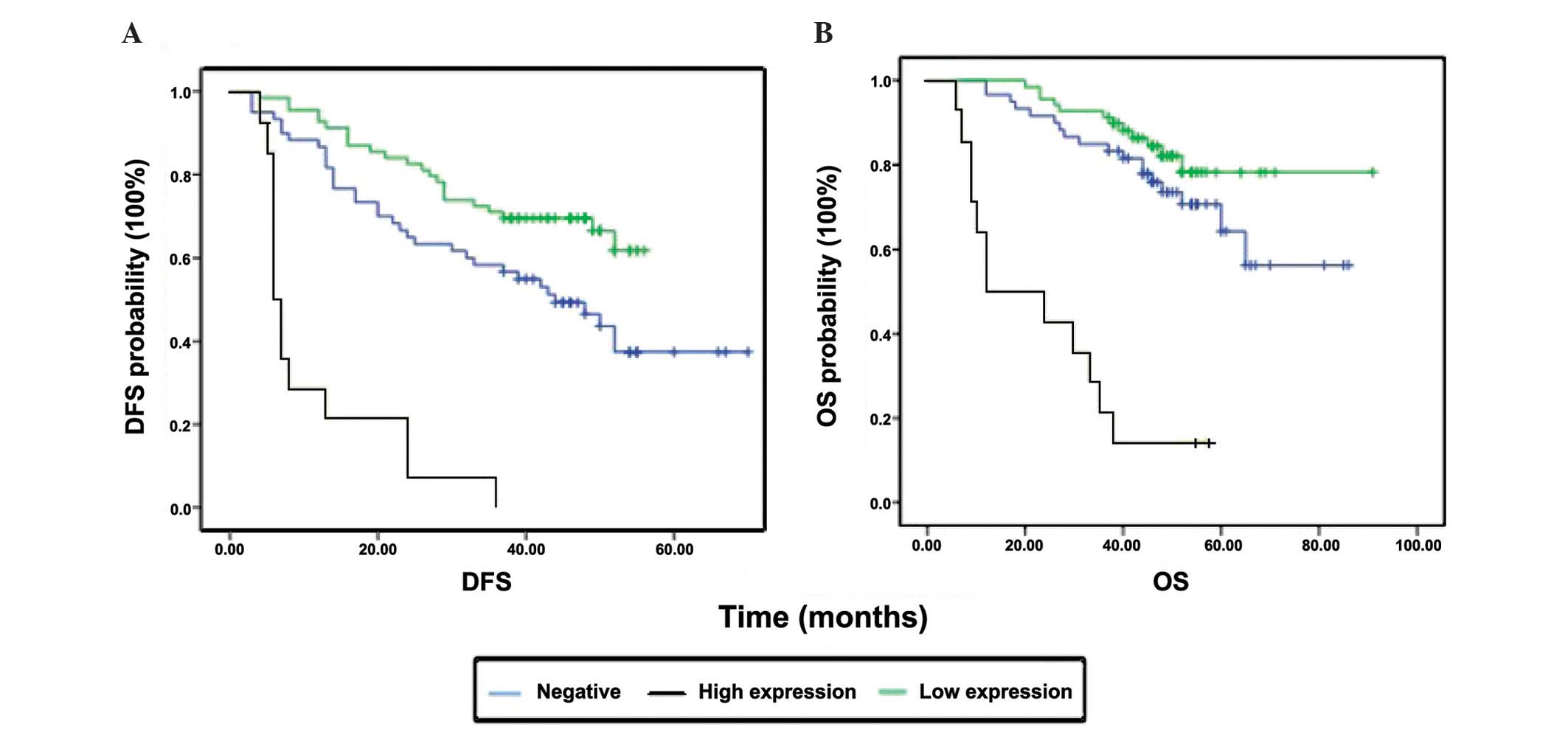
Effect of clinicopathological
characteristics and biomarker expression on survival
The univariate variables were discussed and analyzed
at the beginning of this research. We aimed to determine the
association between prognosis and the expression of CXCL10 or CXCR3
with the assistance of Kaplan-Meier plots. High expression of CXCR3
was found to be associated with shorter OS and DFS (both P-values
<0.0001; Fig. 2, Table V). However, CXCL10 expression was
significantly associated with DFS (P<0.0001), but not with OS
(P=0.181) (Table V). Further analysis
demonstrated that general classification and the presence of
inflammatory adhesions were correlated with CXCR3
(χ2=7.074, P=0.029) and CXCL10 (χ2=4.863,
P=0.088). The fact that ulcerated CRCs stained deeper compared with
elevated CRCs may be attributed to CXCR3, as one of the common
inflammatory cytokines, being involved in ulcer-related
inflammation.
 | Table V.Association between CXCL10/CXCR3 and
prognosis |
Table V.
Association between CXCL10/CXCR3 and
prognosis
|
| DFSa | OSa |
|---|
|
|
|
|
|---|
| Variables | Mean ± SE |
P-valueb | Mean ± SE |
P-valueb |
|---|
| CXCR3
expression |
|
<0.001c |
|
<0.001b |
|
Negative | 42.46±3.30 |
| 67.12±3.75 |
|
|
Low | 44.96±2.02 |
| 79.52±3.05 |
|
|
High | 11.29±2.59 |
| 25.21±4.52 |
|
| CXCL10
expression |
|
<0.001c |
| 0.181 |
|
Negative | 46.47±3.41 |
| 68.46±4.29 |
|
|
Low | 51.93±3.48 |
| 59.83±2.54 |
|
|
High | 28.66±3.25 |
| 61.79±5.62 |
|
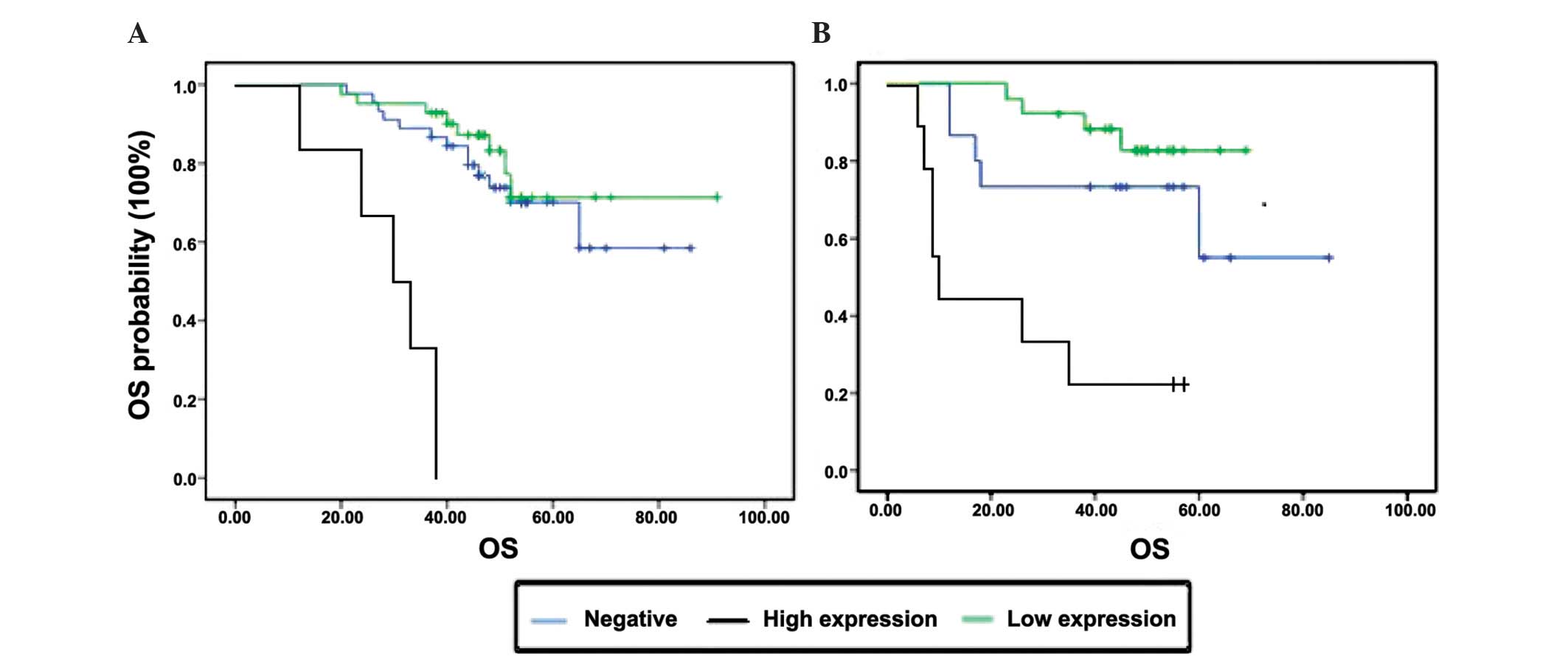
Effect of inflammatory adhesions and
CXCR3 expression on survival
Of the 401 stage II CRC patients, 91 had
inflammatory adhesions, of whom 28 patients developed disease
recurrence (Table IA). All the
recurrent tumors with inflammatory adhesions were collected for
IHC. In view of the results of the log-rank test, we found that the
presence of inflammatory adhesions was associated with OS and CXCR3
expression; therefore, the statistical significance of the
association was investigated. Under the same conditions of cancer
surrounded by adhesions, patients with lower CXCR3 expression
exhibited a better OS. However, patients with the same expression
level of CXCR3 and different inflammatory adhesion status exhibited
no differences in terms of OS (P>0.05). On multivariate
analysis, only CXCR3 expression (P=0.003) was found to be an
independent factor predicting a poorer prognosis (Fig. 3).
Discussion
In this study, we first analyzed the
clinicopathological characteristics of stage II CRC and found that
colon cancer, a higher number of risk factors, the presence of
inflammatory adhesions and tumor size were associated with OS and
were independent variables; the presence of inflammatory adhesions,
in particular, was found to be a significant factor for recurrent
patients. Subsequently, we further investigated the association
between the CXCL10/CXCR3 axis and inflammatory adhesions and
observed that strong CXCL10 or CXCR3 expression in stage II CRC
patients predicted short DFS and OS, particularly CXCR3 expression,
which exhibited statistical significance. Furthermore, CXCR3 was
found to be closely associated with inflammatory adhesions and OS.
We suggest that CXCR3 is a strong indicator of relapse in stage II
CRC patients; in addition, CXCR3 was a long-term prognostic
biomarker for relapsed stage II patients. The chemokine axis
CXCL10/CXCR3 may be the molecular mechanism underlying the
development of inflammatory adhesions.
The morbidity and mortality of CRC are on the
increase worldwide. Chemokines, as inflammatory cytokines, were
first investigated in the context of hematological diseases
(13), such as primary
thrombocythemia, leukemia, multiple myeloma and von Willebrand
syndrome. The association of chemokines with cancer has been
attracting increasing attention. Schimanski et al (14) and Ottaiano et al (15) used IHC to detect CXCL12/CXCR4
expression in CRC and reported significantly higher expression in
stage III/IV compared with stage I/II disease, suggesting that high
expression was associated with lymph node and distant metastasis.
Similar findings were reported for CCR7 in CRC (16,17),
breast cancer (18) and pancreatic
cancer (19). Chemokines in tumors
mainly function in two ways: They either alter tumor cell actin
aggregation, increase or decrease the formation of pseudopodia and
affect tumor cell migration, or they promote the secretion of
certain cytokines, such as metalloproteinases, degrade the
extracellular matrix, damage the endothelial cells and alter
vascular permeability, thereby affecting the process of invasion or
metastasis.
CXCL10 belongs to the ELR (Glu-Leu-Arg)
motif-negative subfamily and acts as an angiogenesis inhibitor; it
has also been characterized as a prognostic marker predicting
clinical outcome in uterine cervical cancer (20) and melanoma (21). It has been demonstrated that CXCL10
exerts its antitumor effect through its immune-stimulating and
angiostatic properties. Of note, the additional roles of CXCL10 in
the tumor microenvironment are also important. CXCL10 may activate
RhoA and Racl and trigger migration of cancer cells (22). The CXCL10/CXCR3-mediated chemotaxis
was found to promote lymph node metastasis in CRC by Kawada et
al (9). As one of the first
immune defense components, CXCL10 levels increase sharply in the
liver, lungs and lymph nodes in CRC by combining to its specific
receptor CXCR3. In order to elucidate the mechanism of action,
previous researchers constructed a CRC cell metastasis model and
found that cells from both primary and metastatic lesions expressed
increased levels of CXCL10 and CXCR3 (23,24); they
confirmed that tumor cells are able to activate and increase the
level of lymphocytes in the microenviroment, upregulate the
expression of interferon-γ and promote secretion of chemokine axes
such as CXCL10/CXCR3, which is a cascade reaction. The underlying
molecular mechanism may be CXCL10 promoting the CRC cells to
secrete matrix metalloproteinases (MMPs) by inhibiting
extracellular signal-regulated kinase 1/2 (ERK1/2) phosphorylation
and repressing the ERK signaling pathway. The MMPs may initiate
other metastasis-related pathways or alter the adhesive properties
of cancer cells, directly promoting invasion. Metzner et al
(25) previously analyzed the
expression of chemokines in melanoma cells by flow cytometric
measurements, ELISA and reverse transcription polymerase chain
reaction; they hypothesized that constitutive chemokine expression
enables an autocrine growth mechanism in epidermoid carcinoma
cells. Numorous studies have demonstrated that CRC cells have the
ability to secrete CXCL10 and CXCR3, whereas normal epithelial
cells may not express CXCR3. In the present study, although CXCL10
as well as CXCR3 differed between RG and NRG, CXCL10 did not
statistically significantly affect DFS or OS. As mentioned above,
we hypothesized that the main function of CXCL10 expressed by stage
II CRC cells is to promote the secretion of CXCR3 in an autocrine
manner and initiate a cascade reaction, promoting invasion and
distant migration of malignant carcinoma cells.
Regardless of the local or systemic inflammatory
response, cancer-associated inflammation, another studying point,
appears to be associated with tumor formation, progression and
metastasis and may be of prognostic value in patients with CRC. Hu
et al (26) found that
microbiota in the gastrointestinal tract may enhance the expression
of chemokine CCL5 and induce CCL5-mediated inflammation, which in
turn promotes epithelial cell proliferation through local
activation of the interleukin 6 (IL-6) pathway, leading to
tumorigenesis. Components of the gut microbiota may be associated
with individual susceptibility. Through measuring IL-6, IL-10,
neutrophil-lymphocyte ratio, neutrophil count and other
inflammatory factors, it was previously demonstrated that elevated
circulating IL-6 concentration is associated with tumor necrosis
(27). The key pathway may be Wnt
signaling recognized by the transcription factor nuclear factor-κB
(28). There are no studies on the
latent function of peritumoral imflammatory adhesions; however, the
association between CXCR3 and inflammation is clear. Dysregulation
of CXCR3 expression has been found in viral infections (29), autoimmune diseases (30), allergy and asthma. To the best of our
knowledge, the present study is the first to provide supportive
evidence for the hypothesis that CRC prognosis is associated with
the presence of inflammatory adhesions and CXCR3 expression. In
turn, the CXCL10/CXCR3 axis may participate in the peritumoral
inflammatory response and promote tumor progression.
In conclusion, we observed that CXCL10 and CXCR3 are
upregulated in recurrent CRC tissues. CXCR3 expression may be used
as one of the predictors of prognosis in postoperative stage II CRC
patients. The cause of adhesion formation remains unclear, but may
pertain to the upregulated expression of CXCR3. Therefore,
postoperative stage II CRC patients exhibiting strong expression of
CXCR3 should be closely followed up.
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chambers AF, Groom AC and MacDonald IC:
Dissemination and growth of cancer cells in metastatic sites. Nat
Rev Cancer. 2:563–572. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
3
|
Benson AB III, Schrag D, Somerfield MR,
Cohen AM, Figueredo AT, Flynn PJ, Krzyzanowska MK, Maroun J,
McAllister P, Van Cutsem E, et al: American Society of Clinical
Oncology recommendations on adjuvant chemotherapy for stage II
colon cancer. J Clin Oncol. 22:3408–3419. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ribic CM, Sargent DJ, Moore MJ, et al:
Tumor microsatellite-instability status as a predictor of benefit
from fluorouracil-based adjuvant chemotherapy for colon cancer. N
Engl J Med. 349:247–257. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sargent DJ, Marsoni S, Monges G, Thibodeau
SN, Labianca R, Hamilton SR, French AJ, Kabat B, Foster NR, Torri
V, et al: Defective mismatch repair as a predictive marker for lack
of efficacy of fluorouracil-based adjuvant therapy in colon cancer.
J Clin Oncol. 28:3219–3226. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zlotnik A: Chemokines in neoplastic
progression. Semin Cancer Biol. 14:181–185. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Balkwill F: Cancer and the chemokine
network. Nat Rev Cancer. 4:540–550. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dwinell MB, Lügering N, Eckmann L and
Kagnoff MF: Regulated production of interferon-inducible T-cell
chemoattractants by human intestinal epithelial cells.
Gastroenterology. 120:49–59. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kawada K, Hosogi H, Sonoshita M, Sakashita
H, Manabe T, Shimahara Y, Sakai Y, Takabayashi A, Oshima M and
Taketo MM: Chemokine receptor CXCR3 promotes colon cancer
metastasis to lymph nodes. Oncogene. 26:4679–4688. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhang R, Zhang H, Zhu W, Pardee AB, Coffey
RJ Jr and Liang P: Mob-1, a Ras target gene, is overexpressed in
colorectal cancer. Oncogene. 14:1607–1610. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jiang Z, Xu Y and Cai S: CXCL10 expression
and prognostic significance in stage II and III colorectal cancer.
Mol Biol Rep. 37:3029–3036. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Li ZS and Li Q: The latest 2010 WHO
classification of tumors of digestive system. Zhonghua Bing Li Xue
Za Zhi. 40:351–354. 2011.(In Chinese). PubMed/NCBI
|
|
13
|
Matsuda T, Seki T, Ogawara M, Miura R,
Yokouchi M and Murakami M: Levels of beta-thromboglobulin and
platelet factor 4 in various diseases (author's transl). J Jpn
Hematol Soc. 43:871–878. 1980.(In Japanese).
|
|
14
|
Schimanski CC, Schwald S, Simiantonaki N,
Jayasinghe C, Gönner U, Wilsberg V, Junginger T, Berger MR, Galle
PR and Moehler M: Effect of chemokine receptors CXCR4 and CCR7 on
the metastatic behavior of human colorectal cancer. Clin Cancer
Res. 11:1743–1750. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ottaiano A, Franco R, Aiello Talamanca A,
Liguori G, Tatangelo F, Delrio P, Nasti G, Barletta E, Facchini G,
Daniele B, et al: Overexpression of both CXC chemokine receptor 4
and vascular endothelial growth factor proteins predicts early
distant relapse in stage II–III colorectal cancer patients. Clin
Cancer Res. 12:2795–2803. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Correale P, Rotundo MS, Botta C, Del
Vecchio MT, Ginanneschi C, Licchetta A, Conca R, Apollinari S, De
Luca F, Tassone P, et al: Tumor infiltration by T lymphocytes
expressing chemokine receptor 7 (CCR7) is predictive of favorable
outcome in patients with advanced colorectal carcinoma. Clin Cancer
Res. 18:850–857. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Li J, Sun R, Tao K and Wang G: The
CCL21/CCR7 pathway plays a key role in human colon cancer
metastasis through regulation of matrix metalloproteinase-9. Dig
Liver Dis. 43:40–47. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Cabioglu N, Yazici MS, Arun B, Broglio KR,
Hortobagyi GN, Price JE and Sahin A: CCR7 and CXCR4 as novel
biomarkers predicting axillary lymph node metastasis in T1 breast
cancer. Clin Cancer Res. 11:5686–5693. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Nakata B, Fukunaga S, Noda E, Amano R,
Yamada N and Hirakawa K: Chemokine receptor CCR7 expression
correlates with lymph node metastasis in pancreatic cancer.
Oncology. 74:69–75. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sato E, Fujimoto J, Toyoki H, Sakaguchi H,
Alam SM, Jahan I and Tamaya T: Expression of IP-10 related to
angiogenesis in uterine cervical cancers. Br J Cancer.
96:1735–1739. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Antonicelli F, Lorin J, Kurdykowski S, et
al: CXCL10 reduces melanoma proliferation and invasiveness in vitro
and in vivo. Br J Dermatol. 164:720–728. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Robledo MM, Bartolome RA, Longo N,
Rodríguez-Frade JM, Mellado M, Longo I, van Muijen GN,
Sánchez-Mateos P and Teixidó J: Expression of functional chemokine
receptors CXCR3 and CXCR4 on human melanoma cells. J Biol Chem.
276:45098–45105. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zipin-Roitman A, Meshel T, Sagi-Assif O,
Shalmon B, Avivi C, Pfeffer RM, Witz IP and Ben-Baruch A: CXCL10
promotes invasion-related properties in human colorectal carcinoma
cells. Cancer Res. 67:3396–3405. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kawada K, Hasegawa S, Murakami T, Itatani
Y, Hosogi H, Sonoshita M, Kitamura T, Fujishita T, Iwamoto M,
Matsumoto T, et al: Molecular mechanisms of liver metastasis. Int J
Clin Oncol. 16:464–472. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Metzner B, Hofmann C, Heinemann C, Zimpfer
U, Schraufstätter I, Schöpf E and Norgauer J: Overexpression of
CXC-chemokines and CXC-chemokine receptor type II constitute an
autocrine growth mechanism in the epidermoid carcinoma cells KB and
A431. Oncol Rep. 6:1405–1410. 1999.PubMed/NCBI
|
|
26
|
Hu B, Elinav E, Huber S, Strowig T, Hao L,
Hafemann A, Jin C, Wunderlich C, Wunderlich T, Eisenbarth SC, et
al: Microbiota-induced activation of epithelial IL-6 signaling
links inflammasome-driven inflammation with transmissible cancer.
Proc Natl Acad Sci USA. 110:9862–9867. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Guthrie GJ, Roxburgh CS, Richards CH,
Horgan PG and McMillan DC: Circulating IL-6 concentrations link
tumour necrosis and systemic and local inflammatory responses in
patients undergoing resection for colorectal cancer. Br J Cancer.
109:131–137. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Vaiopoulos AG, Athanasoula KCH and
Papavassiliou AG: NF-κB in colorectal cancer. J Mol Med (Berl).
1029–1037. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
de Niet A, de Bruijne J, Plat-Sinnige MJ,
Takkenberg RB, van Lier RA, Reesink HW and van Leeuwen EM:
Upregulation of CXCR3 expression on CD8+ T cells due to
the pervasive influence of chronic hepatitis B and C virus
infection. Hum Immunol. 74:899–906. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Björkander S, Heidari-Hamedani G, Bremme
K, Gunnarsson I and Holmlund U: Peripheral monocyte expression of
the chemokine receptors CCR2, CCR5 and CXCR3 is altered at
parturition in healthy women and in women with systemic lupus
erythematosus. Scand J Immunol. 77:200–212. 2013. View Article : Google Scholar : PubMed/NCBI
|