Introduction
Gastrointestinal stromal tumors (GISTs) are rare
tumors that may arise from any site of the GI tract and are
generally associated with abdominal pain, GI bleeding, or a
palpable mass. However, a small intestinal GIST rarely causes
hemorrhagic shock. We herein report a case of hemorrhagic shock
with excessive bleeding caused by an ileal GIST that was managed by
emergency surgery. The patient provided written informed consent
for the publication of this case report.
Case report
A 67-year-old male patient presented to the
Department of Gastroenterology of the Ibaraki Medical Center, Tokyo
Medical University (Ami, Japan) in July 18, 2014, with dizziness
and blood in the stool. The patient's medical history included
treatment for hypertension by a local physician. The findings of
the subsequent physical examination were unremarkable, except for
low blood pressure (97/60 mmHg) and mild pallor of the palpebral
conjunctiva. Laboratory data revealed mild anemia (hemoglobin, 10.2
g/dl) and increased blood urea nitrogen (34.1 mg/dl). Upper
endoscopy revealed no hemorrhagic lesion of the duodenum, stomach,
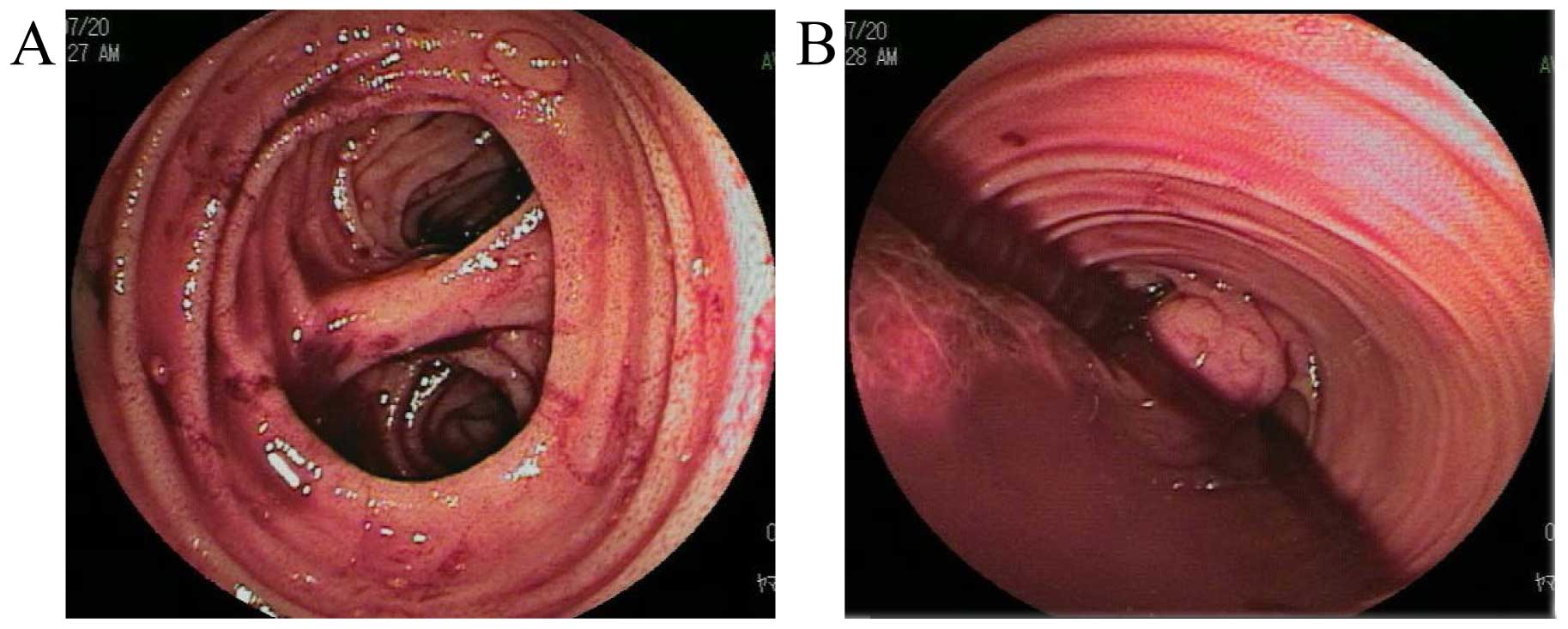
or esophagus. Colonoscopy revealed fresh blood with clotting
discharged from the proximal side of the ileocecal valve; no
hemorrhagic lesion of the colon or rectum was identified. Abdominal
contrast-enhanced computed tomography (CT) revealed extravasation
of the contrast medium into the small intestine (Fig. 1). The intestinal bleeding continued,
and the patient eventually developed hemorrhagic shock (blood
pressure, 76/42 mmHg; hemoglobin 4.5 g/dl). Hence, 22 units of red
blood cells stored in mannitol-adenine-phosphate and 10 units of
fresh-frozen plasma were administered. Subsequent double-balloon
enteroscopy (DBE) revealed a Meckel's diverticulum and a submucosal
tumor with excessive bleeding at 60 and 100 cm proximal to the
ileocecal valve, respectively (Fig.
2). Endoscopic hemostasis was not possible, as the enteroscope
could not approach the tumor. Following DBE marking near the tumor,
emergency partial resection of the ileum, including the tumor and
the Meckel's diverticulum, was performed 2 h from developing
hemorrhagic shock in July 20, 2014. There were no signs of
lymphadenopathy, peritoneal dissemination, or liver metastasis. The
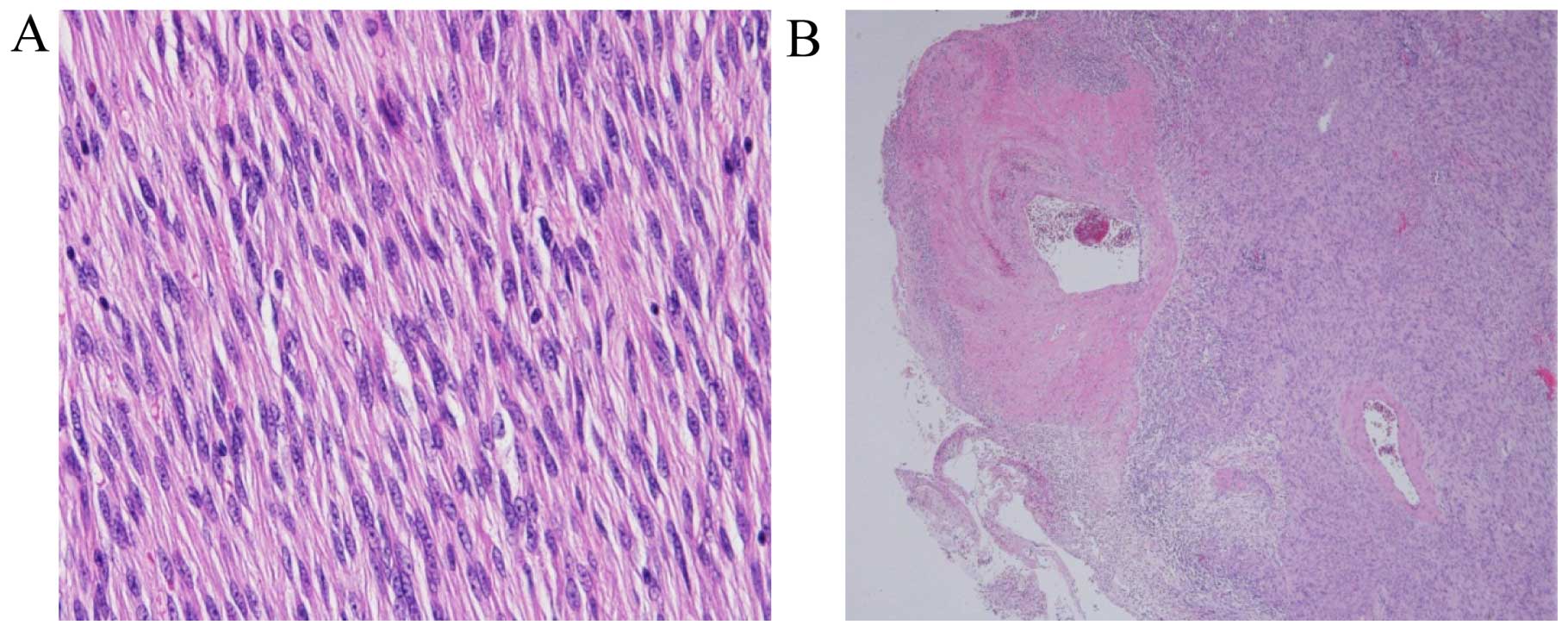
excised tumor (1.3×0.8 cm) exhibited ulcerative mucosal changes
(Fig. 3). Sectioning of the tumor
revealed a solid and grayish white tissue. Histological examination
of the excised tumor revealed proliferation of spindle-shaped cells
in the submucosa to the subserosa of the ileum and a ruptured
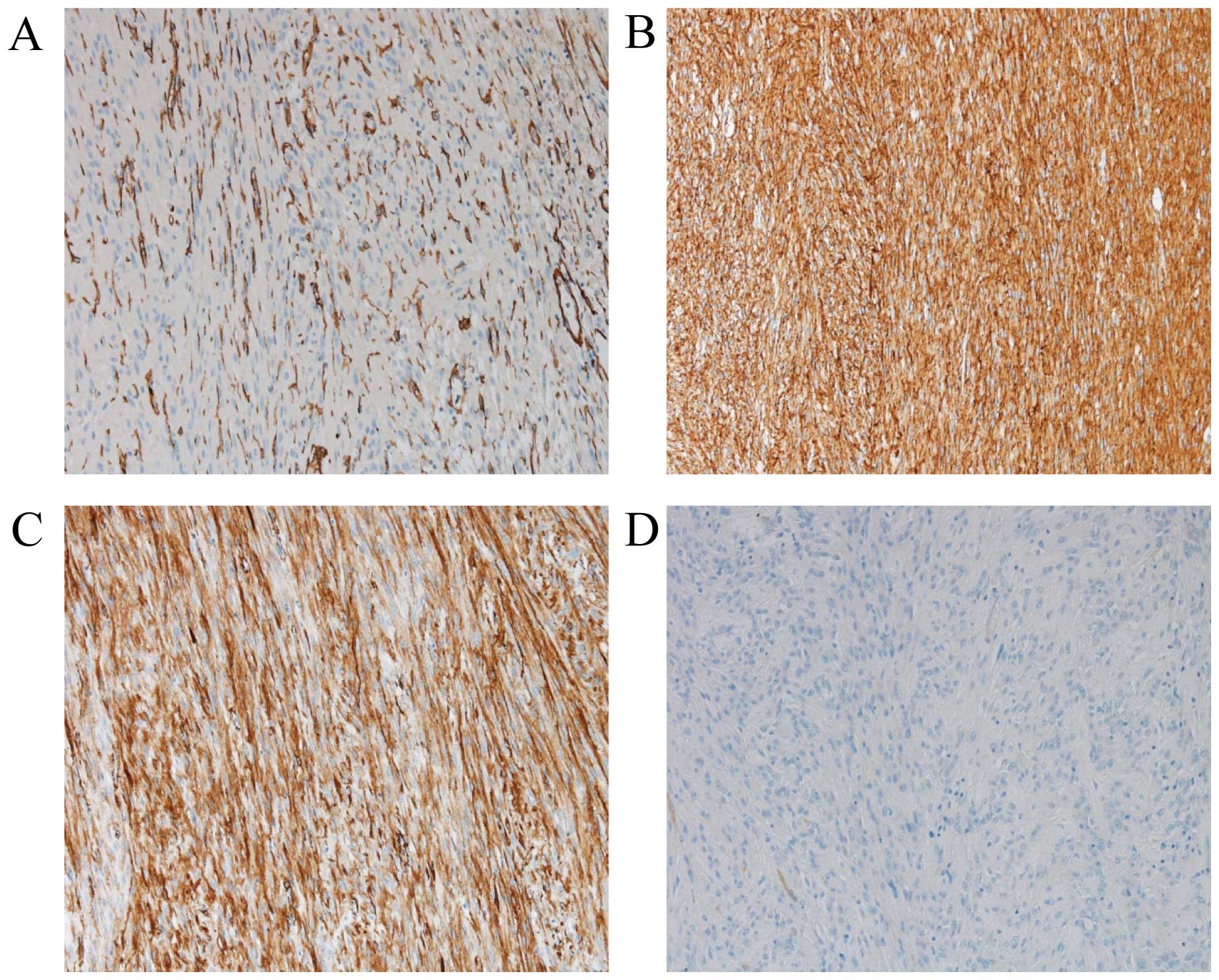
intratumoral artery at the tumor surface (Fig. 4). Immunohistochemical staining of the
tumor was positive for CD34, KIT and α-smooth muscle actin, but
negative for S-100 protein (Fig. 5).
The MIB-1 labeling index using Ki-67 was 1.0–5.0%. The tumor size
and the immunohistological findings supported the diagnosis of a
low-risk GIST of the ileum (1). The
patient had an uneventful recovery, was discharged on postoperative
day 14 and has been monitored at our outpatient clinic for 14
months after the surgery.
Discussion
GISTs constitute ~0.2–0.5% of all GI tract tumors,
with ~70% of the cases occurring in the stomach, 20% in the small
intestine, and <10% in the colon, rectum, or esophagus (2,3). The
clinical presentation of GISTs is variable and the most frequent
symptoms are abdominal pain, GI bleeding, or a palpable mass. In
GISTs arising in any site, including the stomach, duodenum, small
intestine, colon and rectum, Sorour et al (4) reported that GI bleeding was the most
serious symptom. However, with respect to small intestinal GISTs,
abdominal pain (35.5%) is the most frequent symptom, while
hemorrhagic shock (6.4%) is relatively rare (5). In the present case, the patient
developed hemorrhagic shock; thus, upper endoscopy, colonoscopy,
abdominal contrast-enhanced CT, and DBE were performed to
investigate the source of the hemorrhage. Abdominal CT plays an
important role in the diagnosis of small intestinal GISTs,
particularly contrast-enhanced CT in cases with excessive bleeding
(6,7).
In the present case, abdominal contrast-enhanced CT revealed that
the hemorrhagic source was the small intestine, although no tumor
was detected. DBE is an efficacious procedure for the diagnosis and
treatment of small intestinal disease. The most common clinical
indications of GISTs include obscure bleeding, abdominal pain,
anemia, chronic diarrhea and inflammatory bowel disease (8). Robles et al (9) reported that the histological detection
rate of GISTs by DBE biopsy was 71.4%. The first-line treatment for
small intestinal GISTs with excessive bleeding remains debatable
(10,11). The endoscopic treatment by DBE is very
limited in massive GIST bleeding, but it may be possible, delaying
or averting emergency surgery (9). In
the present case, DBE was unable to avert emergency surgery, but
located the level of the bleeding and guided resection.
Interventional digital subtraction angiography has been reported to
be effective for GISTs with bleeding (12). Basile et al (13) reported that interventional
radiological procedures for the detection of bleeding GISTs of the
small intestine were superior to other diagnostic approaches. In
the present case, we performed emergency partial resection of the
ileum, including the GIST, as i) the patient had developed
hemorrhagic shock and ii) an interventional radiology specialist
was unable to urgently respond in our hospital.
There are certain differences in the follow-up
examinations after surgery for GISTs between the guidelines of the
National Comprehensive Cancer Network (NCCN) and the Japanese
Society of Clinical Oncology (JSCO) (14,15). After
surgical resection of all tumors, the NCCN guidelines recommend
abdominal and pelvic CT imaging every 3–6 months for 3–5 years.
However, the JSCO guidelines recommend CT testing every 6–12 months
for GISTs with low or very low risk for recurrence, and every 4–6
months for GISTs with a high or intermediate risk or clinically
malignant. Our patient has been monitored by CT scans every 6
months in our outpatient clinic, as recommended by the JSCO
guidelines.
In conclusion, DBE is an efficacious procedure for
identify the source of bleeding in the small intestine. Moreover,
immediate emergency surgery should be considered for cases of small
intestinal GISTs with excessive bleeding.
Acknowledgements
The authors would like to thank Enago (www.enago.jp) for the English language review.
References
|
1
|
Fletcher CD, Berman JJ, Corless C,
Gorstein F, Lasota J, Longley BJ, Miettinen M, O'Leary TJ, Remotti
H, Rubin BP, et al: Diagnosis of gastrointestinal stromal tumors: A
consensus approach. Hum Pathol. 33:459–465. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Connolly EM, Gaffney E and Reynolds JV:
Gastrointestinal stromal tumors. Br J Surg. 90:1178–1186. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Joensuu H: Gastrointestinal stromal tumor
(GIST). Ann Oncol. 17(Suppl 10): 280–286. 2006. View Article : Google Scholar
|
|
4
|
Sorour MA, Kassem MI, Ghazal Ael-H,
El-Riwini MT and Abu Nasr A: Gastrointestinal stromal tumors (GIST)
related emergencies. Int J Surg. 12:269–280. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Constantin VD, Socea B, Popa F, Carâp AC,
Popescu G, Vlădescu T, Ceauşu Z, Berteşteanu ŞV and Ceauşu MC: A
histopathological and immunohistochemical approach of surgical
emergencies of GIST. An interdisciplinary study. Rom J Morphol
Embryol. 55(2 Suppl): 619–627. 2014.PubMed/NCBI
|
|
6
|
Choi H: Imaging modalities of
gastrointestinal stromal tumors. J Surg Oncol. 104:907–914. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sandrasegaran K, Rajesh A, Rushing DA,
Rydberg J, Akisik FM and Henley JD: Gastrointestinal stromal
tumors: CT and MRI findings. Eur Radiol. 15:1407–1414. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Akarsu M, Akkaya Özdinç S, Celtik A and
Akpınar H: Diagnostic and therapeutic efficacy of double-balloon
endoscopy in patients with small intestinal diseases: Single-center
experience in 513 procedures. Turk J Gastroenterol. 25:374–380.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Robles EP, Delgado PE, Conesa PB, Andrés
BM, Guggiana MF, Mateos EA, Caballero MF, Agudo JL, Martínez SC,
Latorre R, et al: Role of double-balloon enteroscopy in malignant
small bowel tumors. World J Gastrointest Endosc. 7:652–658.
2015.PubMed/NCBI
|
|
10
|
Gerson LB, Fidler JL, Cave DR and Leighton
JA: ACG clinical guideline: Diagnosis and management of small bowel
bleeding. Am J Gastroenterol. 110:1265–1287; quiz 1288. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ohmiya N, Nakagawa Y, Nagasaka M, Tahara
T, Shibata T, Nakamura M, Hirooka Y, Goto H and Hirata I: Obscure
gastrointestinal bleeding: Diagnosis and treatment. Dig Endosc.
27:285–294. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chen YT, Sun HL, Luo JH, Ni JY, Chen D,
Jiang XY, Zhou JX and Xu LF: Interventional digital subtraction
angiography for small bowel gastrointestinal stromal tumors with
bleeding. World J Gastroenterol. 20:17955–17961. 2014.PubMed/NCBI
|
|
13
|
Basile A, Certo A, Ascenti G, Lamberto S,
Cannella A and Medina JG: Interventional radiology in the
preoperative management of stromal tumors causing intestinal
bleeding. Radiol Med. 106:376–381. 2003.(In English, Italian).
PubMed/NCBI
|
|
14
|
von Mehren M, Randall RL, Benjamin RS,
Boles S, Bui MM, Casper ES, Conrad EU III, DeLaney TF, Ganjoo KN,
George S, et al: Gastrointestinal stromal tumors, version 2.2014. J
Natl Compr Canc Netw. 12:853–862. 2014.PubMed/NCBI
|
|
15
|
Nishida T, Hirota S, Yanagisawa A, Sugino
Y, Minami M, Yamamura Y, Otani Y, Shimada Y, Takahashi F and Kubota
T: GIST Guideline Subcommittee: Clinical practice guidelines for
gastrointestinal stromal tumor (GIST) in Japan: English version.
Int J Clin Oncol. 13:416–430. 2008. View Article : Google Scholar : PubMed/NCBI
|