Introduction
Invasive bladder cancers usually metastasize to the
lymph nodes, liver, lung and bone. Furthermore, aggressive local
invasion into adjacent structures is also commonly observed
(1). However, the occurrence of
rectal stricture due to infiltration by bladder cancer is
relatively rare. We herein report the case of a patient who
presented with an aggressive bladder cancer that resulted in rectal
infiltration and partial obstruction.
Case report
A 69-year-old man was referred to the Tokyo Medical
University Ibaraki Medical Center (Inashiki, Japan) with chief
complaints of urinary incontinence and pollakiuria. The patient
also had thin stools and edema of the left lower extremity. The
patient had a history of hypertension and a family history of
prostate and gastric cancer occurring in his father and daughter,
respectively.
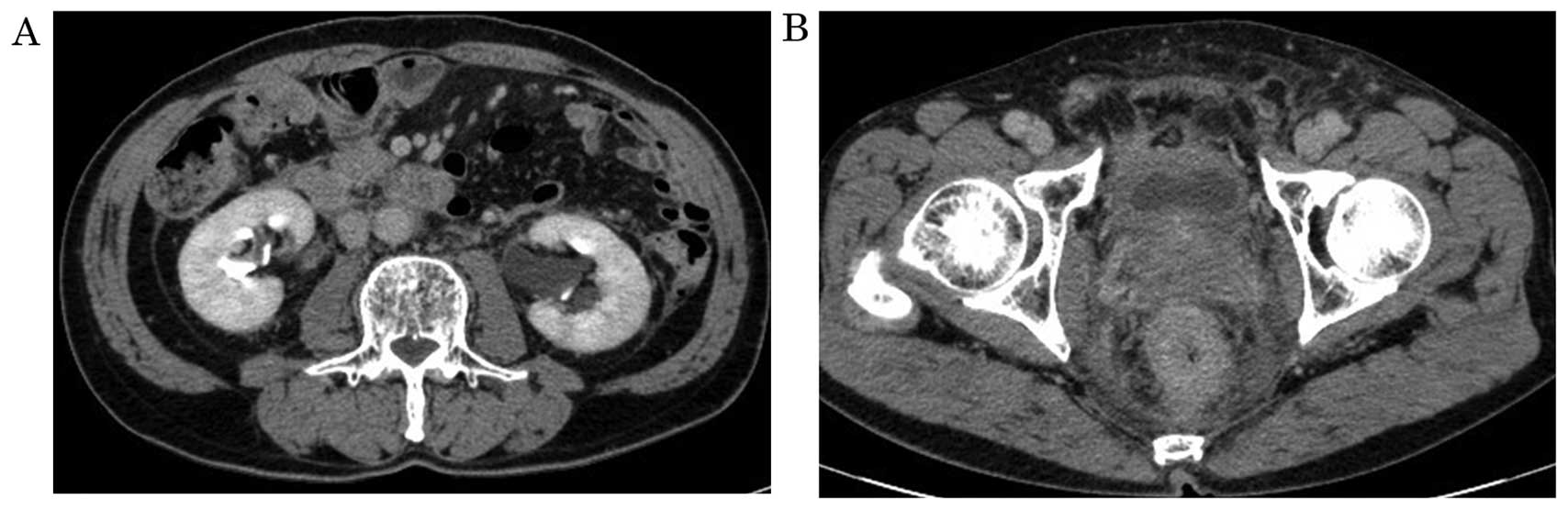
Computed tomography (CT) and magnetic resonance
imaging (MRI) revealed bilateral hydronephrosis and thickening of
the wall of the rectum and the posterolateral wall of the bladder.
Enlargement of the left obturator lymph nodes was also observed,
suggesting the presence of lymph node metastasis (Figs. 1 and 2).
The laboratory test results were as follows: Normal
blood count; creatinine level, 1.16 mg/dl; estimated glomerular
filtration rate, 48.9 ml/min/1.73 m2; carcinoembryonic
antigen (CEA) level, 5.6 ng/ml (normal range, <5.0 ng/ml); and
carbohydrate antigen (CA) 19-9 level, 460.1 U/ml (normal range,
<37.0 U/ml). Urinalysis revealed the presence of 1–4 white and
0–1 red blood cells per high-power field in the urine. Furthermore,
the urine cytology was class IIIb. Cystoscopic examination revealed
small papillary tumors and a pale thickened bladder mucosa at the
retrotrigonum of the bladder, involving the ureteral orifices
bilaterally. These results suggested extrinsic invasion of the
bladder by the tumor. Rectal examination indicated a narrowed
rectal lumen, with an intact rectal mucosa. Colonoscopy revealed a
narrow rectal lumen with an edematous mucosa, suggesting extrinsic
compression. Transurethral biopsy of the papillary lesions and the
thickened bladder wall revealed the presence of grade 2 urothelial
carcinoma with glandular differentiation (Fig. 3). Transrectal bladder needle biopsy
suggested that the bladder cancer cells had infiltrated the rectal
wall.
Three courses of gemcitabine and cisplatin (GC)
chemotherapy were administered and this therapy continued to
demonstrate effectiveness post-treatment. A CT scan revealed an
improvement in the thickened bladder and rectal walls (Fig. 4). The CEA and CA19-9 levels were also
reduced to 2.3 ng/ml and 66.1 U/ml, respectively. The symptom of
thin stools also subsided. At the last follow-up 6 months after
chemotherapy, the disease status was stable.
Informed consent was obtained form the patient
regarding the publication of the case details.
Discussion
Prostate cancer is reported to be the most common
cause of rectal obstruction among urogenital cancers (2). However, annular constriction of the
rectum secondary to bladder cancer has rarely been reported. There
are three main characteristics of an annular rectal constriction
caused by an infiltrating bladder cancer: The majority of the
patients are male, the tumor is of high grade and stage, and the
prognosis is poor (3–6). The characteristics of the patient in
the present case, who was diagnosed with grade 2 stage IV
urothelial carcinoma, were consistent with the previously reported
cases.
The mechanism underlying annular rectal stricture
caused by bladder cancer remains unknown. Stillwell et al
(3) reported two cases of male
patients with annular constrictions of the rectum and they
hypothesized that a locally aggressive cancer of the bladder neck
or trigonum may break through the Denonvilliers' fascia and
encircle the rectum. Langenstroer et al (4) described another case with similar
rectal obstruction that developed 3 years after cystoprostatectomy;
they suggested that surgical deposition of cancer cells may be the
cause of the rectal obstruction.
Kobayashil et al (5) reported three cases of male patients
exhibiting annular constriction of the rectum due to the
infiltration by a bladder cancer. All these cases exhibited
progressive spread of tumor cells involving the bladder wall. The
infiltrating tumor, encroaching both ureteral orifices, resulted in
reduced bladder capacity. The CT results showing thickened lateral
pedicles without involvement of the perirectal fat layer were
intriguing. Therefore, Kobayashil et al (5) hypothesized that cancer cells of this
type were able to easily spread along the lateral pedicles to reach
the posterior rectal wall and then infiltrate the rectal wall.
In the present case, the CT findings of the
enlargement of the left obturator lymph nodes, without the
involvement of the perirectal fat layer, were of interest. These
results differed from those of the surgical deposition of cancer
cells that caused rectal constriction. Therefore, we hypothesized
that, consistent with the report by Kobayashil et al
(5), the cancer cells in this study
may have spread along the lateral pedicles to reach the posterior
rectal wall prior to penetrating it.
Almost all reported cases of annular rectal
constrictions caused by an infiltrating bladder cancer are
associated with a poor prognosis. By contrast, our patient
responded well to GC chemotherapy. Therefore, immediate initiation
of an appropriate chemotherapy following diagnosis may be
beneficial and achieve a good response, given that a complete
response to treatment may not be feasible.
In conclusion, annular rectal constriction is a rare
complication of bladder cancer and is associated with a poor
prognosis. It is important that physicians consider the possibility
of an annular rectal constriction caused by an infiltrating bladder
cancer when patients with bladder cancer complain of thin stools
and the clinical examination reveals narrowing of the rectal lumen.
Immediate chemotherapy initiation should be considered in such
cases.
Acknowledgements
The authors would like to thank Enago (www.enago.jp) for reviewing the English language of
the original manuscript.
References
|
1
|
Tabbara WS and Mehio AR: Metastatic
patterns of bladder carcinoma. Prog Clin Biol Res 162A. 145–160.
1984.
|
|
2
|
Fry DE, Amin M and Harbrecht PJ: Rectal
obstruction secondary to carcinoma of the prostate. Ann Surg.
189:488–492. 1979.PubMed/NCBI
|
|
3
|
Stillwell TJ, Rife CC and Lieber MM:
Bladder carcinoma presenting with rectal obstruction. Urology.
34:238–240. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Langenstroer P, Zacharias A, Almagro U and
Dewire D: Annular constriction of the rectum secondary to
transitional cell carcinoma of the bladder. Urology. 47:442–444.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kobayashi S, Kato H, Iijima K, Kinebuchi
Y, Igawa Y and Nishizawa O: Annular rectal constriction due to
infiltration by bladder cancer. Hinyokika Kiyo. 52:569–572.
2006.PubMed/NCBI
|
|
6
|
Abol-Enein H, El-Baz M, Abd El-Hameed MA,
Abdel-Latif M and Ghoneim MA: Lymph node involvement in patients
with bladder cancer treated with radical cystectomy: A
patho-anatomical study-a single center experience. J Urol.
172:1818–1821. 2004. View Article : Google Scholar : PubMed/NCBI
|