Introduction
Schwannoma (neurilemmoma) is a type of tumor that
originates from Schwann cells, which produce the insulating myelin
sheath covering peripheral nerves. Schwannomas are also referred to
as Schwann cell tumors and are benign, solitary, relatively
slow-growing nerve sheath tumors (1). Theoretically, schwannomas may develop
in any peripheral nerve. The most common site of schwannomas is the
head and neck region, accounting for ~25–35% of all cases (2). In 3–4% of the patients, schwannomas of
the head and neck are incidentally discovered at autopsy (3). Apart from cranial nerves, schwannomas
may be observed in other sites, such as the tongue (4), stomach (5), colon (6), knee (7)
and penis (8); however, it is highly
unusual for schwannomas to be encountered in the genital tract.
Transformation into a malignant tumor is rarely
encountered in schwannomas, and the reasons have not yet been fully
elucidated. Schwannomas may transform into a type of malignant
tumor referred to as neurofibrosarcoma.
The clinical manifestations of schwannomas differ
according to tumor location and tumor size and they are mostly
atypical. The majority of head and neck schwannomas are vestibular
schwannomas, and tumors of the vestibulocochlear nerve may be
associated with tinnitus and epicophosis. Complete surgical removal
is considered to be the standard approach to the treatment of the
vast majority of this type of tumor, due to its encapsulated nature
(9).
We herein present a case of schwannoma located in
the vagina in a 48-year-old woman, which was incidentally
discovered.
Case report
A 48-year-old female patient, gravida 2 para 2,
presented to the Handan First Hospital (Handan, China) in June 2016
with a main complaint of vaginal dilation persisting for ~1 year.
The last menstrual period was in July 11, 2016. Apart from
menstruation, the patient had not observed any vaginal bleeding or
other vaginal discharge over the course of the disease. The
findings on physical examination were as follows: Temperature
36.8°C, heart rate 78 beats/min, respiratory rate 20 breaths/min,
and blood pressure 125/80 mmHg. Gynecological examination revealed
a nodular mass located in the left posterior vaginal wall, in the
upper part of the vagina. The size of the mass was 3.5×2.5 cm, and
it was fixed (non-mobile), with a hard texture, clear boundary,
smooth surface and irregular shape. The cervix, uterus and
bilateral attachments did not exhibit any abnormalities on
palpation. Transvaginal ultrasonography revealed a low-echo mass on
the left side of the vagina, sized 3.7×2.7×2.7 cm. The liver and
kidney function tests, chest X-ray and electrocardiogram were all
normal. To determine the nature of the lesion, the patient
underwent exploratory surgery through the transvaginal approach
under epidural anesthesia. The intraoperative findings were as
follows: The lesion was located in the left posterior wall of the
vagina and it appeared to be nodular, consisting of three smaller
fused nodules, sized 1×0.5, 1×2 and 0.5×0.5 cm. The mass had a
clear boundary from the surrounding tissues, its surface was smooth
and it was encapsulated. The mass was removed in a piecemeal manner
and on cross-section the tumor exhibited yellowish areas and its
texture was soft. On gross examination, the resected tissues were
gray or grayish yellow in color, the size ranged from 0.5×0.3×0.2
to 3.2×1.5×0.5 cm, and the texture was soft and partly tough. On
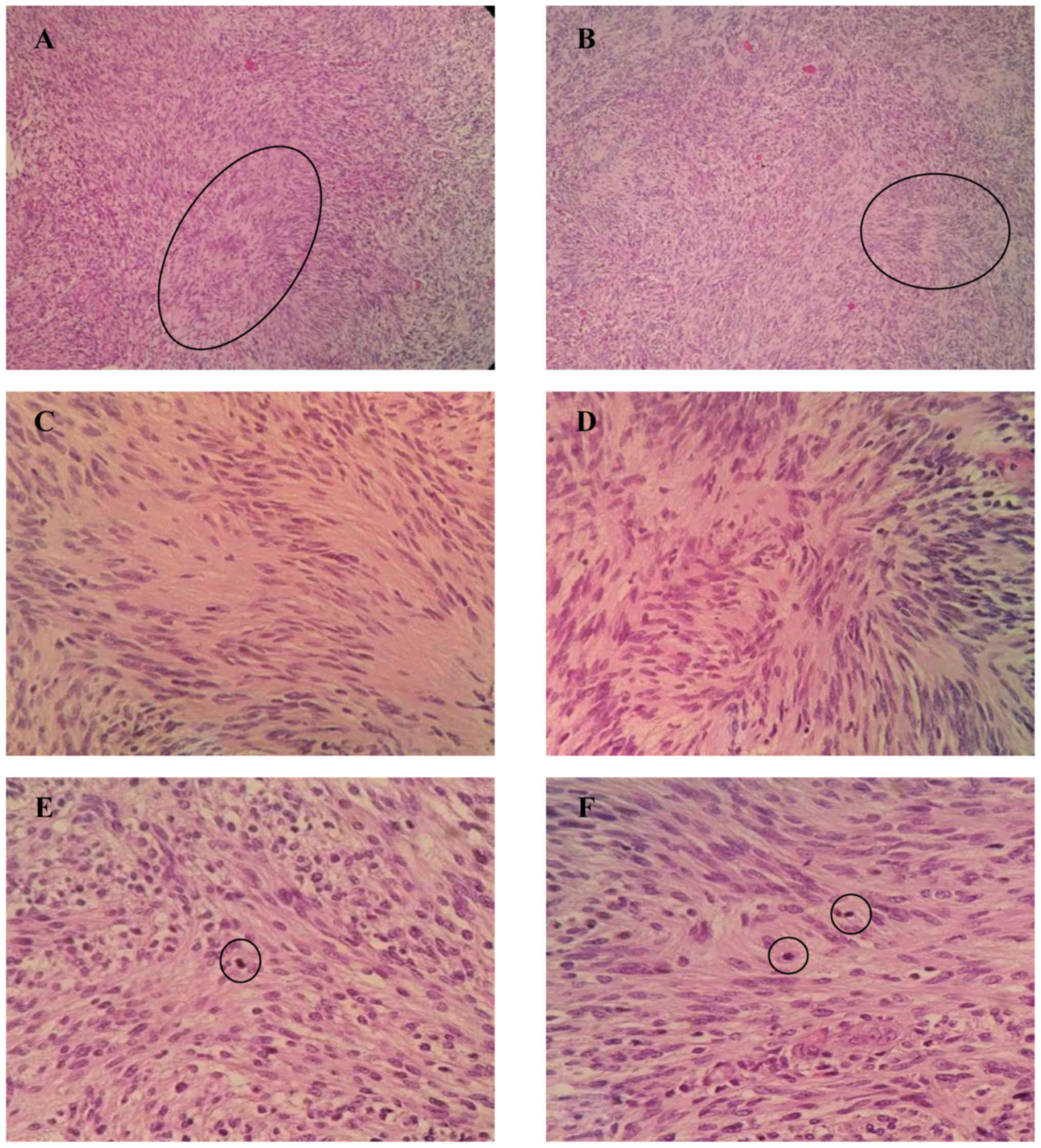
microscopic examination following hematoxylin and eosin (H&E)
staining, hypercellular and hypocellular areas (Antoni type A and
B, respectively) with Verocay bodies were identified. The tumor
cells were long, spindle-shaped, and mildly atypical, and were
densely arranged in bundles, palisades and whirlpools, with a
mitotic count of 3/10 high-power fields (HPFs). No necrosis or
mucoid degeneration was identified on microscopic examination. The
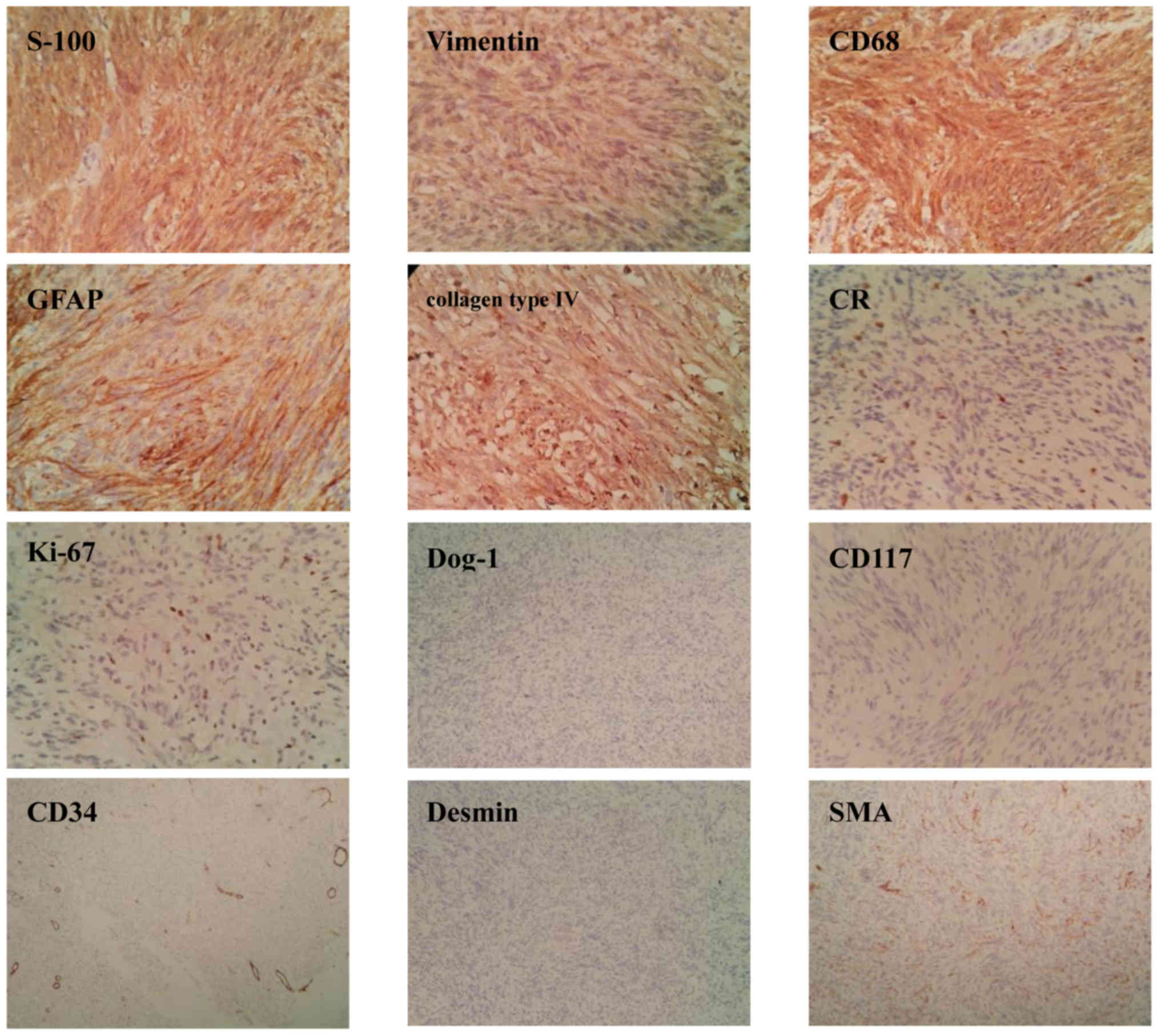
histological appearance on H&E staining is shown in Fig. 1. On immunohistochemical examination,
the tumor cells were positive for vimentin (3+), S-100 (3+), CD68
(3+), glial fibrillary acidic protein (GFAP; 3+), collagen type IV
(3+), calretinin (+) and Ki-67 (10%); discovered on GIST-1 (DOG-1),
CD117, CD34, CD99, desmin, smooth muscle actin (SMA) and
cytokeratin were all negative. All immunohistochemistry reagents
were purchased from Maxim Biotechnologies (Fuzhou, China). The
immunohistochemical staining results are presented in Fig. 2. Taken together, these
characteristics were consistent with a pathological diagnosis of
benign cellular schwannoma. Due to the presence of active cell
growth and mitotic figures, follow-up was recommended. The patient
recovered quickly following complete margin-negative surgical
resection, and there has been no recurrence or metastasis during
the 1-year follow-up (last follow-up visit, May 2017).
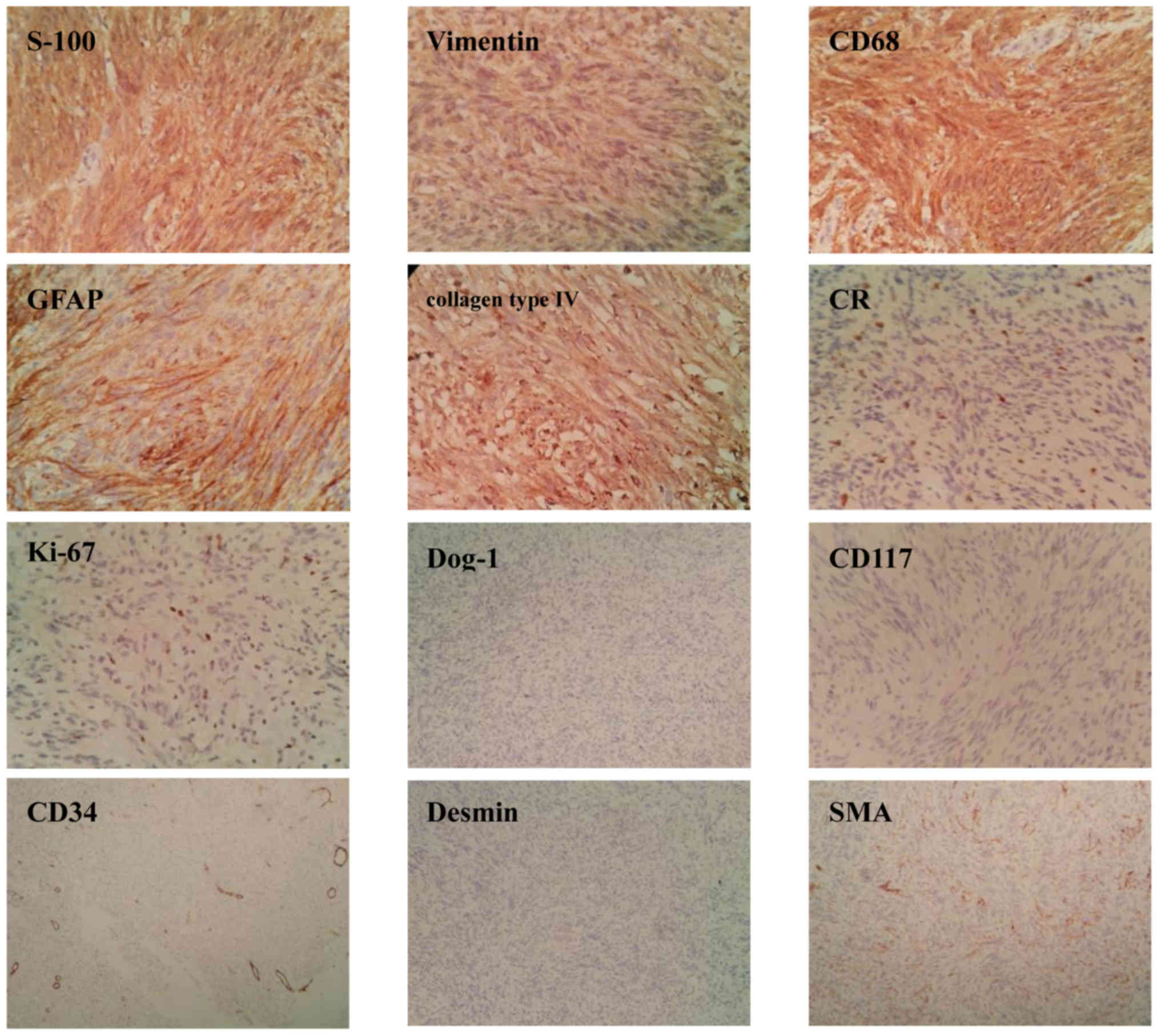 | Figure 2.Immunostaining of the tumor section
with hematoxylin counterstaining; original magnification, ×200. The
tumor cells were strongly positive for S-100, vimentin, CD68, GFAP
and collagen type IV in Antoni A areas (3+, brownish-yellow
cytoplasmic staining). CR was weakly positive (1+, nuclear
staining). The Ki-67 proliferation index was 10%. However, DOG-1,
CD117, CD34 and desmin were all negative. SMA was positive in the
vessels. GFAP, glial fibrillary acidic protein; CR, calretinin;
DOG-1, discovered on GIST-1; SMA, smooth muscle actin. |
Discussion
Cellular schwannoma, which is a benign peripheral
nerve tumor with unknown histogenesis, has a predilection for the
upper limbs and the head and neck region in children and young
women (10). This type of tumor
often grows slowly and is almost always solitary, encapsulated,
circumscribed and eccentrically located. For vaginal schwannomas,
early detection may be difficult due to the slow growth over time
and unspecific clinical manifestations. The majority of the cases
are asymptomatic and most of these tumors are incidentally
discovered on imaging examinations (computed tomography, magnetic
resonance imaging). Histologically, two main patterns, namely
Antoni type A and B, are observed. Immunohistochemical examination
is necessary for the definitive diagnosis of this type of
tumor.
In the present case, the patient was a
perimenopausal middle-aged woman. The symptoms were mild, without
bleeding, pain or irritation, so the mass was not detected over a
long period. A variety of clinical manifestations of vaginal
schwannoma are reported, with late symptoms often occurring due to
the increasing size of the tumor and depending on its location
(11). Other clinical symptoms
include vaginal pain when the tumor is large, and urinary retention
and/or constipation if the tumor compresses the bladder outlet
and/or rectum, respectively (12–15). Our
patient had a tumor measuring ~3 cm and experienced a sensation of
vaginal tenesmus. The diagnosis of this type of tumor relies on
pathological examination of the surgically excised specimens
revealing the classic schwannoma Antoni A and B areas. Antoni A
areas are characteristically hypercellular, composed of spindle
tumor cells (elongated Schwann cells) arranged in sheets,
exhibiting a fascicular pattern and nuclear palisading arranged
around a collagenous hyalinised core (Verocay bodies). The
structure of Antoni type A areas is considered as a prominent
characteristic for histopathological diagnosis. Antoni B areas are
hypocelullar and are composed of small round cells within a myxoid
stroma; the tumor cells in this area appear to be more disorganized
compared with Antoni type A areas. This type is prone to cystic
degeneration. In our patient, H&E staining revealed that
spindle cells were regularly arranged in whirlpools or palisades.
The nuclear atypia was mild, and the mitotic count was 3/10 HPFs
under the microscope. No necrosis or degenerative changes were
observed. Therefore, the diagnosis of schwannoma may be made based
on the histopathological characteristics described above. However,
immunohistochemical staining is essential for confirming the
diagnosis and distinguishing schwannoma from other homologous
tumors. Schwannomas display strong and diffuse immunoreactivity for
S-100 protein, vimentin and GFAP, and are negative for CD117,
DOG-1, CD34 and SMA, which are findings suggestive of its neural
origin. The patient in the present case received timely complete
surgical resection and has had no recurrence during the follow-up
period. Surgical resection was previously reported to be the only
curative treatment for schwannoma (9,16). As
schwannomas are mostly benign with a good prognosis, aggressive
surgery is not considered necessary.
Differential diagnosis: i) Leiomyoma is a benign
tumor of smooth muscle (usually originating in the uterus or
digestive tract). The tumor cells are spindle-shaped and are
arranged in a weaving pattern. The nuclei are egg-shaped, round and
blunt on both ends. Leiomyoma very rarely exhibits malignant
transformation, except for cases where the nuclear mitotic count is
1–4/10 HPFs. On immunohistochemistry, the tumor cells are
SMA-positive. ii) Interstitialoma is a benign tumor located in the
digestive tract. The spindle cells form swirls and fascicles, with
occasional palisading, and many have oval nuclei surrounded by
perinuclear halos or vacuoles. On immunohistochemistry, the cells
are CD117-, DOG-1- and CD34-positive. iii) Malignant schwannoma.
There is a significant distinction between benign and malignant
schwannomas. In malignant schwannomas, the tumor cells form
clusters and may invade into the lumen of blood vessels. These
tumors are highly cellular, with areas of necrosis commonly seen in
the tumor parenchyma, and significant mitotic activity (≥4 mitotic
figures/10 HPFs). The expression of SOX10, neurofibromin and p16 is
completely absent, epidermal growth factor receptor and S-100 may
be weakly positive, and the Ki-67 proliferation index is >20%
(17). iv) Neurofibroma is a
peripheral nerve sheath tumor. The tumor is composed of slender
spindle cells arranged in wavy, fascicular and circinate pattern,
with collagen fibers or myxoid substance in the tumor stroma. The
tumor lacks Antoni A and B areas and there is no calretinin
expression. v) Solitary fibroma is a rare mesenchymal tumor
composed of two parts, namely a hypercellular and a hypocellular
region, in which collagen fibers exhibit unequal thickness and
different shapes. The mitotic count is <3/10 HPFs. CD34, CD99,
epithelial membrane antigen and B-cell lymphoma-2 are usually
positive.
In conclusion, we herein present a rare case of
vaginal schwannoma incidentally detected in a patient presenting
only with mild discomfort. As this is a common disease, but a rare
location, differential diagnosis of schwannoma from other vaginal
tumors is crucial. Based on the histopathological and
immunohistochemical characteristics, particularly staining for
S-100, CD117, DOG-1, CD34, SMA and Ki-67, the diagnosis of
schwannoma may be confirmed, even if the location of the tumor is
unusual. Transvaginal surgical resection is curative, as in the
present case. The recurrence rate and the risk of malignant
transformation are exceptionally low in such cases.
Glossary
Abbreviations
Abbreviations:
|
SMA
|
smooth muscle actin
|
|
GFAP
|
glial fibrillary acidic protein
|
|
CR
|
calretinin
|
References
|
1
|
Hilton DA and Hanemann CO: Schwannomas and
their pathogenesis. Brain Pathol. 24:205–220. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Berlucchi M, Piazza C, Blanzuoli L,
Battaglia G and Nicolai P: Schwannoma of the nasal septum: a case
report with review of the literature. Eur Arch Otorhinolaryngol.
257:402–405. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hanemann CO and Evans DG: News on the
genetics, epidemiology, medical care and translational research of
Schwannomas. J Neurol. 253:1533–1541. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Abreu I, Roriz D, Rodrigues P, Moreira A,
Marques C and Alves FC: Schwannoma of the tongue-A common tumour in
a rare location: A case report. Eur J Radiol Open. 4:1–3. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Romdhane H, Cheikh M, Mzoughi Z, Slama SB,
Ennaifer R and Belhadj N: Gastric Schwannoma: A Case Report. Clin
Pract. 6:8492016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wang WB, Chen WB, Lin JJ, Xu JH, Wang JH
and Sheng QS: Schwannoma of the colon: A case report and review of
the literature. Oncol Lett. 11:2580–2582. 2016.PubMed/NCBI
|
|
7
|
Öz TT, Aktaş B, Özkan K, Özturan B, Kilic
B and Demiroğlu M: A Case of Schwannoma of the Common Peroneal
Nerve in the Knee. Orthop Rev (Pavia). 9:68252017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Loeser A, Katzenberger T, Meuller JG,
Riedmiller H and Gerharz EW: Solitary schwannoma of the glans
penis. Urology. 70:1007.e5–1007.e6. 2007. View Article : Google Scholar
|
|
9
|
Biswas D, Marnane CN, Mal R and Baldwin D:
Extracranial head and neck schwannomas-a 10-year review. Auris
Nasus Larynx. 34:353–359. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hornick JL and Fletcher CD: Cellular
neurothekeoma: Detailed characterization in a series of 133 cases.
Am J Surg Pathol. 31:329–340. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Terada S, Suzuki N, Tomimatsu N and
Akasofu K: Vaginal schwannoma. Arch Gynecol Obstet. 251:203–206.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Obeidat BR, Amarin ZO and Jallad MF:
Vaginal schwannoma: A case report. J Reprod Med. 52:341–342.
2007.PubMed/NCBI
|
|
13
|
Park JW, Hwang SO, Choi SJ, Lee BI, Park
JH and Song E: Incidental diagnosis of vaginal schwannoma in a
patient with thigh pain. Obstet Gynecol Sci. 57:86–88. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sharma NS and Lynch MJ: Intrapelvic
neurilemmoma presenting with bladder outlet obstruction. Br J Urol.
82:9171998. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Samarakoon L, Weerasekera A, Sanjeewa R
and Kollure S: Giant presacral schwannoma presenting with
constipation: A case report. J Med Case Reports. 6:2852012.
View Article : Google Scholar
|
|
16
|
Melvin WS and Wilkinson MG: Gastric
schwannoma. Clinical and pathologic considerations. Am Surg.
59:293–296. 1993.PubMed/NCBI
|
|
17
|
Pekmezci M, Reuss DE, Hirbe AC, Dahiya S,
Gutmann DH, von Deimling A, et al: Morphologic and
immunohistochemical features of malignant peripheral nerve sheath
tumors and cellular schwannomas. Mod Pathol. 28:187–200. 2015.
View Article : Google Scholar : PubMed/NCBI
|