Introduction
Maxillary sinus cancer is rare and often presents as
a locally advanced disease (1).
Recurrence commonly occurs locoregionally, although a minority of
patients may experience distant metastasis, and the most commonly
involved sites are the lungs and bone (2,3). The
current report discusses the case of a 64-year-old male who
presented with a mass in the left submandibular area at the Kyung
Hee University Hospital at Gangdong in November 2013. Biopsy was
performed and histological analysis identified a poorly
differentiated squamous cell carcinoma. A staging workup was
conducted, including chest X-ray, paranasal sinus computed
tomography (CT), neck CT, chest CT and positron emission tomography
(PET)-CT. After staging workup, it was concluded the patient had a
maxillary sinus squamous cell carcinoma at clinical stage IVA,
which was classified according to the American Joint Committee on
Cancer (AJCC) staging system (4).
The patient received a left partial maxillectomy and a left radical
neck dissection, followed by postoperative chemoradiotherapy (CRT).
After three months of CRT, the patient developed a left adrenal
gland metastasis without locoregional failure. The patient received
a laparoscopic left adrenalectomy and histological analysis
revealed it to be a poorly-differentiated squamous cell carcinoma.
Within one month of surgery, the patient developed multiple
metastases at the left adrenalectomy site, and succumbed to the
disease four months later.
Paranasal sinus cancer is a rare type of tumor,
representing ~3% of head and neck malignancies (1). The most common site of these tumors is
the maxillary sinus (5). Patients
with maxillary sinus cancer tend to be asymptomatic until the tumor
invades the adjacent structures; therefore, they often present with
locally advanced disease (6).
Tumor recurrence commonly occurs within one year of
diagnosis, with locoregional failure (3). Relatively few patients present with
distant metastasis, for which the lungs and bone are the most
commonly involved sites (3). This
report presents a rare case of recurrent maxillary sinus cancer
with only adrenal gland metastasis.
Case report
A 64-year-old male presented with pain in the left
submandibular area and was treated with a three-week course of
antibiotics at the local clinic. However, the patient continued to
experience painful swelling and tenderness in the left
submandibular area and was eventually admitted to the Kyung Hee
University Hospital at Gangdong in November 2013. The patient had
no significant medical history. Waters' view X-ray revealed a
haziness on the left maxillary sinus and bone resorption on the
left buccal vestibular region of no. 26. The patient had
experienced tenderness at the left buccal vestibular region of no.
26 and the left submandibular region. The initial diagnosis was an
odontogenic sinusitis through the dental caries on the palatal root
of no. 26. Tooth no. 26 was extracted and the patient was
prescribed oral antibiotics. Although the patient used the
antibiotics for three weeks, they were still experiencing painful
swelling in the left submandibular area, which had extended to the
left maxillary sinus. Intraoral examination revealed a granulation
tissue was protruding at the tooth no. 26 extraction site, and a
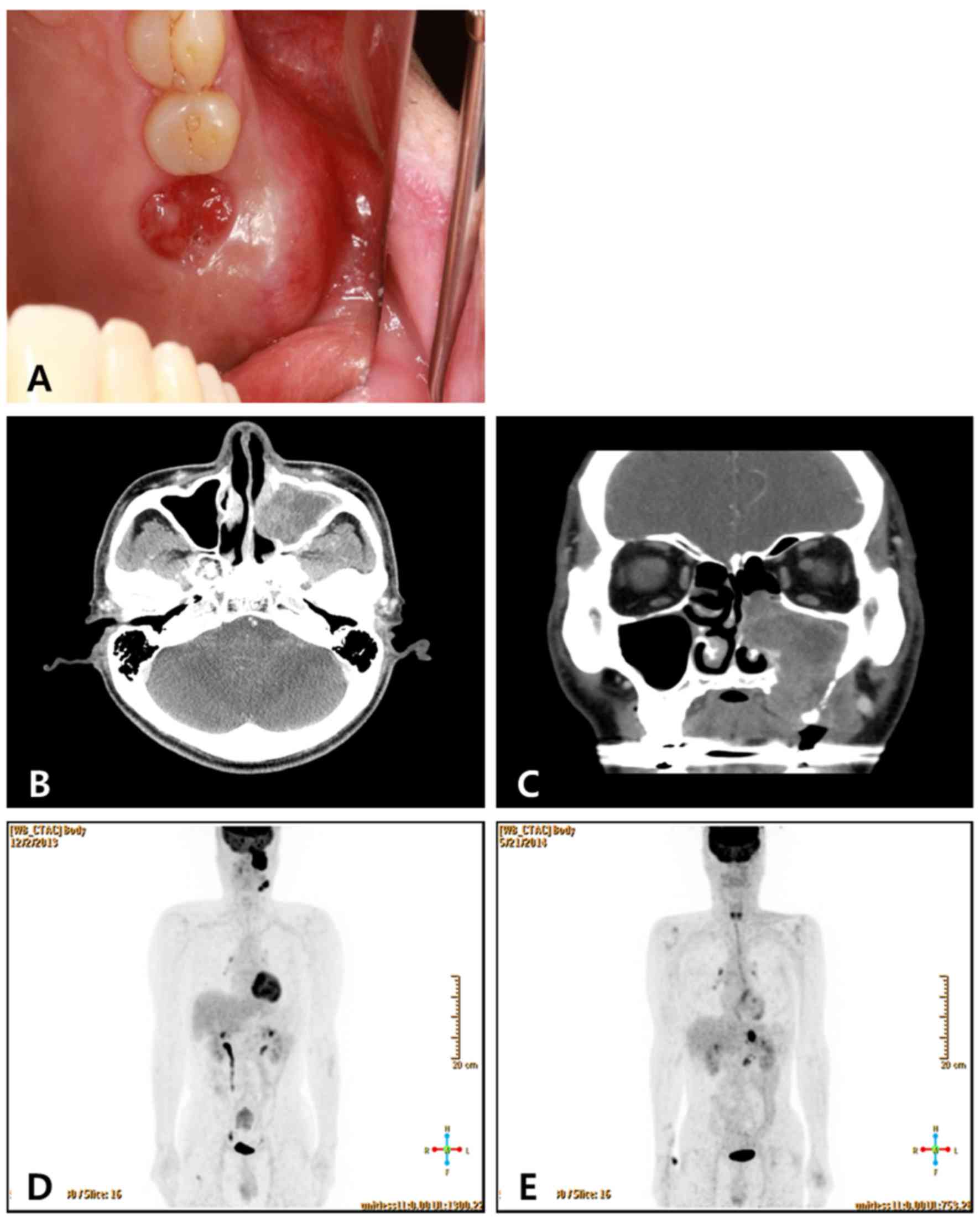
biopsy at that site was subsequently performed (Fig. 1A).
Histological examination of the biopsy tissue sample
revealed a poorly-differentiated squamous cell carcinoma. CT showed
destruction of the left lateral maxillary sinus wall, invasion of
the nasal cavity, destruction of the maxilla's medial inferior wall
as well as destruction of the left oral cavity. In addition,
enlarged lymph nodes in the left neck at level IB and level IIA
were observed. A PET/CT scan was performed, and the lesion was
determined to be confined to the primary site and the ipsilateral
neck lymph nodes (Fig. 1B-D). After
a staging workup, including CT and PET/CT, it was concluded that
the patient had a maxillary sinus squamous cell carcinoma at
clinical stage IVA (cT3N2), according to the AJCC staging system
(4). The patient was then referred
to the maxillofacial surgeon and received a left partial
maxillectomy and ipsilateral radical neck dissection. The
pathological findings indicated poorly-differentiated squamous cell
carcinoma with neck lymph nodes metastasis (9/30). Negative
resection margins were achieved but the safety margin was close;
the patient received adjuvant concurrent CRT.
One month following the completion of CRT, a neck CT
scan was used to assess the primary tumor status. There was no
visible evidence of locoregional failure. After two months of CRT,
the tumor status was re-examined using neck CT and chest CT scans.
The patient had developed a left adrenal gland metastasis without
locoregional failure. PET/CT also revealed that the metastasis was
only present in the left adrenal gland (Fig. 1E). The patient subsequently received
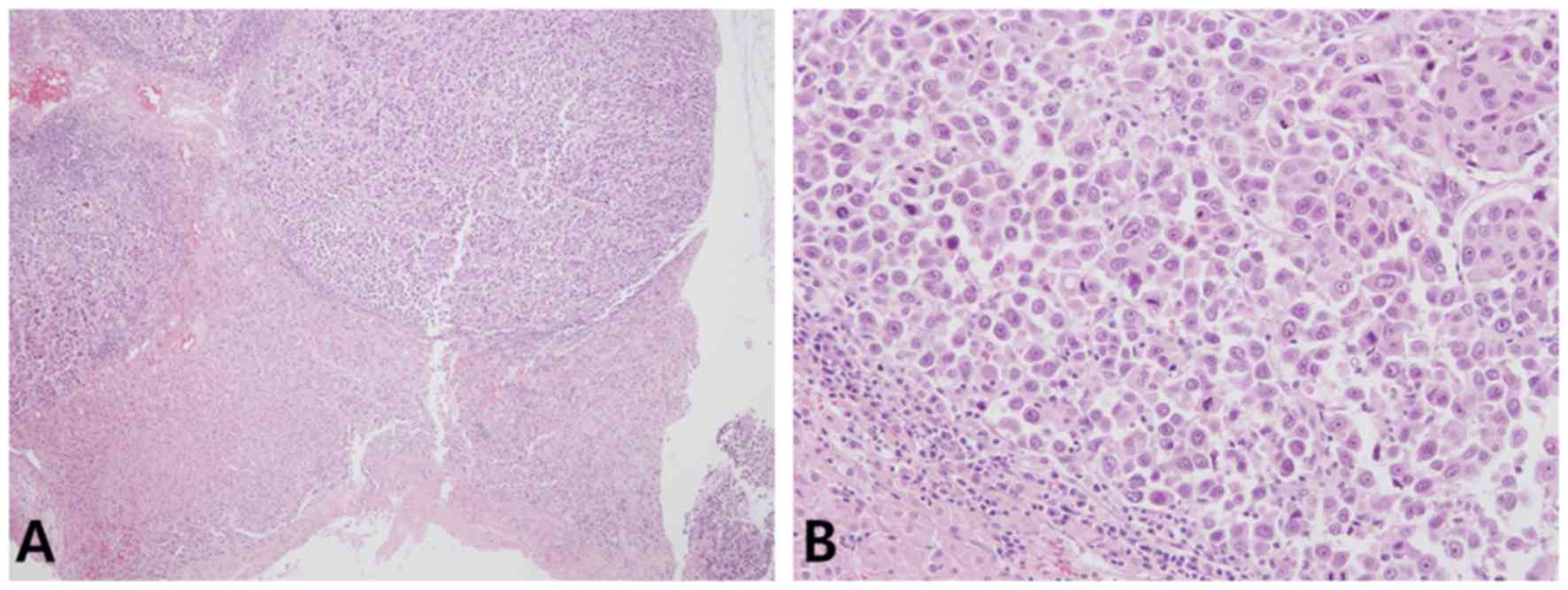
a laparoscopic left adrenalectomy; histological examination
indicated poorly-differentiated squamous cell carcinoma (Fig. 2). One month following this surgery,
the patient experienced abdominal pain and they were examined using
an abdominal-pelvic CT, which demonstrated the presence of multiple
nodules at the left adrenalectomy site. Although the patient was
provided palliative chemotherapy, they succumbed to the disease
four months later.
Discussion
Malignant neoplasms arising from the paranasal
sinuses are rare and the diagnosis of sinus malignancies is
challenging due to the frequently nonspecific symptoms and the deep
position of the structures involved, which are difficult to biopsy
(5). Therefore, paranasal sinus
cancer is typically diagnosed as an advanced T3/T4 stage disease
(7). Nodal metastasis is experienced
by ≤26% of patients (8). In the
present case, the patient exhibited swelling of the left
submandibular area and was experiencing pain, so they were
prescribed a three-week course of oral antibiotics, due to what was
eventually revealed to be a misdiagnosis of odontogenic sinusitis.
The accurate diagnosis was obtained following a biopsy of the
protruding granulation tissue at the tooth extraction site. After
staging work up, the patient was determined to have a locally
advanced maxillary sinus squamous cell carcinoma at stage IVA.
The optimal treatment strategy for locally advanced
paranasal sinus cancer remains undefined (3). Current therapeutic approaches include
surgery, radiation and systemic chemotherapy in a variety of
combinations and sequences (2,3). Prior
studies have reported that a combination of surgery and
radiotherapy can provide an improved rate of overall survival (OS),
when compared with CRT, for locally advanced paranasal sinus cancer
(9,10). Kang et al (11) reported that a combination of surgery
and radiotherapy and/or chemotherapy conferred superior five-year
OS rates, as compared with CRT, for stage III or localized stage IV
maxillary sinus cancer (81.2 vs. 37.9%; log-rank test, P=0.029),
which were analyzed using SPSS software version 16.0 (SPSS, Inc.,
Chicago, IL, USA). The patient in the current report had received a
left partial maxillectomy and ipsilateral radical neck lymph node
dissection followed by postoperative CRT. The patient achieved
complete remission; however, the maxillary sinus cancer rapidly
progressed to the left adrenal gland after three months of CRT. In
the event of isolated adrenal metastasis in lung cancer, or liver
metastasis in colorectal cancer, the patients in question are
considered to have stage IV non-small cell lung cancer or
colorectal cancer, respectively. However, it has previously been
noted that aggressive surgical treatment of the metastasis may
result in long-term survival. Luketich et al (12) reported that excision significantly
prolonged survival time (31 months), as compared with no excision
(8.5 months), in adrenal metastasis of primary non-small cell lung
cancer. In patients with colorectal cancer and liver metastasis,
the five-year survival rate with chemotherapy alone is 5–10%
(13). However, liver resection in
selected patients can result in a five-year survival rate of 30%
(14). In the current case, a
laparoscopic left adrenalectomy was performed for salvage
treatment. Despite this, the maxillary sinus cancer rapidly
progressed and the patient succumbed to the disease four months
later.
Waldron et al (3) evaluated 110 cases of maxillary sinus
cancer with definitive RT (83 patients) or surgery and adjuvant RT
(27 patients). The five-year rates of local progression-free
survival and disease-free survival were 42 and 43%, respectively.
In total, 63 patients developed local r ecurrence, and 25/63 then
underwent salvage surgery with a subsequent five-year
cause-specific survival rate of 31% (3). Therefore, localized recurrence
following surgery and/or CRT may be managed by salvage surgery.
However, further investigations into salvage surgery for isolated
distant metastasis are required.
In conclusion, it is suggested that clinicians must
consider that maxillary sinus cancer may recur only at the distant
site. Salvage surgery alone for isolated distant metastases is not
a sufficient treatment option and postoperative radiotherapy or
chemotherapy must be considered, whether or not residual tumor
tissue is absent. The role of salvage surgery for the isolated
metastasis of paranasal sinus cancer must be investigated
further.
References
|
1
|
Ansa B, Goodman M, Ward K, Kono SA,
Owonikoko TK, Higgins K, Beitler JJ, Grist W, Wadsworth T, El-Deiry
M, et al: Paranasal sinus squamous cell carcinoma incidence and
survival based on surveillance, epidemiology, and end results data,
1973 to 2009. Cancer. 119:2602–2610. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bristol IJ, Ahamad A, Garden AS, Morrison
WH, Hanna EY, Papadimitrakopoulou VA, Rosenthal DI and Ang KK:
Postoperative radiotherapy for maxillary sinus cancer: Long-term
outcomes and toxicities of treatment. Int J Radiat Oncol Biol Phys.
68:719–730. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Waldron JN, O'Sullivan B, Gullane P,
Witterick IJ, Liu FF, Payne D, Warde P and Cummings B: Carcinoma of
the maxillary antrum: A retrospective analysis of 110 cases.
Radiother Oncol. 57:167–173. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Edge SB, Byrd DR, Compton CC, Fritz AG,
Greene FL and Trotti A: AJCC cancer staging manual. 7th. New York,
NY: Springer; 2010
|
|
5
|
Bhattacharyya N: Factors affecting
survival in maxillary sinus cancer. J Oral Maxillofac Surg.
61:1016–1021. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Muir CS and Nectoux J: Descriptive
epidemiology of malignant neoplasms of nose, nasal cavities, middle
ear and accessory sinuses. Clin Otolaryngol Allied Sci. 5:195–211.
1980. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Santos MR, Servato JP, Cardoso SV, de
Faria PR, Eisenberg AL, Dias FL and Loyola AM: Squamous cell
carcinoma at maxillary sinus: Clinicopathologic data in a single
Brazilian institution with review of literature. Int J Clin Exp
Pathol. 7:8823–8832. 2014.PubMed/NCBI
|
|
8
|
Myers LL, Nussenbaum B, Bradford CR,
Teknos TN, Esclamado RM and Wolf GT: Paranasal sinus malignancies:
An 18-year single institution experience. Laryngoscope.
112:1964–1969. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hayashi T, Nonaka S, Bandoh N, Kobayashi
Y, Imada M and Harabuchi Y: Treatment outcome of maxillary sinus
squamous cell carcinoma. Cancer. 92:1495–1503. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Dulguerov P, Jacobsen MS, Allal AS,
Lehmann W and Calcaterra T: Nasal and paranasal sinus carcinoma:
Are we making progress? A series of 220 patients and a systematic
review. Cancer. 92:3012–3029. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kang JH, Cho SH, Kim JP, Kang KM, Cho KS,
Kim W, Seol YM, Lee S, Park HS, Hur WJ, et al: Treatment outcomes
between concurrent chemoradiotherapy and combination of surgery,
radiotherapy, and/or chemotherapy in stage III and IV maxillary
sinus cancer: Multi-institutional retrospective analysis. J Oral
Maxillofac Surg. 70:1717–1723. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Luketich JD and Burt ME: Does resection of
adrenal metastases from non-small cell lung cancer improve
survival? Ann Thorac Surg. 62:1614–1616. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gallinger S, Biagi JJ, Fletcher GG, Nhan
C, Ruo L and McLeod RS: Liver resection for colorectal cancer
metastases. Curr Oncol. 20:e255–e265. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Simmonds PC, Primrose JN, Colquitt JL,
Garden OJ, Poston GJ and Rees M: Surgical resection of hepatic
metastases from colorectal cancer: A systematic review of published
studies. Br J Cancer. 94:982–999. 2006. View Article : Google Scholar : PubMed/NCBI
|