Introduction
Angiolymphoid hyperplasia with eosinophilia (ALHE),
also known as epithelioid hemangioma, is rare type of benign
vascular hyperplastic lesion (1).
This disease usually presents with pink-red/brown, dome-shaped,
dermal papules or nodules on the head or neck, particularly near
the ears and on the scalp (2). The
lesion(s) may be associated with pain or pruritus. Uncommon
symptoms include pulsation and spontaneous bleeding. It is unclear
whether ALHE is a reactive or neoplastic disease. In its active
phase, it can be misdiagnosed as an angiosarcoma; however,
eosinophilia is not a usual feature of malignant angiosarcoma
(3). Pyogenic granuloma (PG) is a
small, eruptive, usually solitary, sessile or pedunculated, friable
papule. The lesion is common in children and occurs most often on
an exposed surface. PG bleeds easily with the slightest trauma and,
if removed superficially, may promptly recur. Recurring lesions may
have one or numerous satellite lesions (2).
Case report
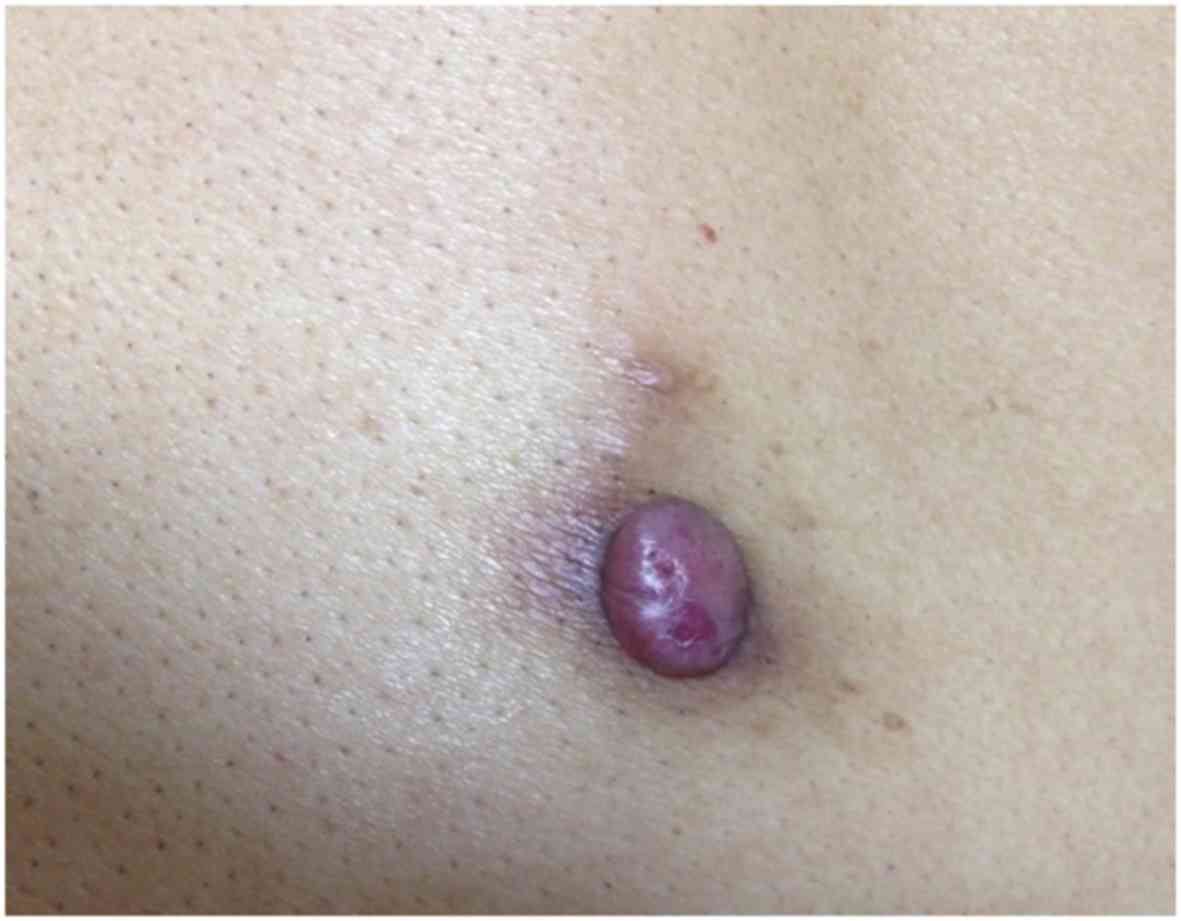
A 47-year-old East Asian male patient inadvertently
noticed a protuberant, mildly pruritic, reddish colored nodule near
the scapular region of the back present for the past 6 months. The
patient was admitted to the Dermatology Department of Shenzhen
Zhongshan Urological Hospital (Shenzhen, China) in November 2015.
The patient gave history of accidental bleeding and blood scab
formation from the nodule following trivial trauma such as rubbing
of the skin. There was no history of fever, night sweats, weight
loss or decreased appetite.
The general physical examination was unremarkable.
Over the vicinage of scapular region was a round, reddish colored,
protuberant nodule ~1.8×1 cm in size, which was firm in consistency
with smooth overlying surface (Fig.
1). Surrounding the nodule, few prominent pilosebaceous
follicles over a reddish brown base were observed. There was no
axillary or inguinal lymphadenopathy and no hepatosplenomegaly.
Routine blood investigations revealed Hb: 141 g/l, WBC:
6.3×109/l, eosinophil count: 0.52×109/l
(reference range, 0.02–0.52×109/l), eosinophil count %:
8.3% (0.4–0.8%). The coagulation profile provided the following
values: PT: 13.2S, PT%: 98%, APTT: 29S, TT: 15S, Fib2.71 g/l. Liver
and renal function tests were normal.
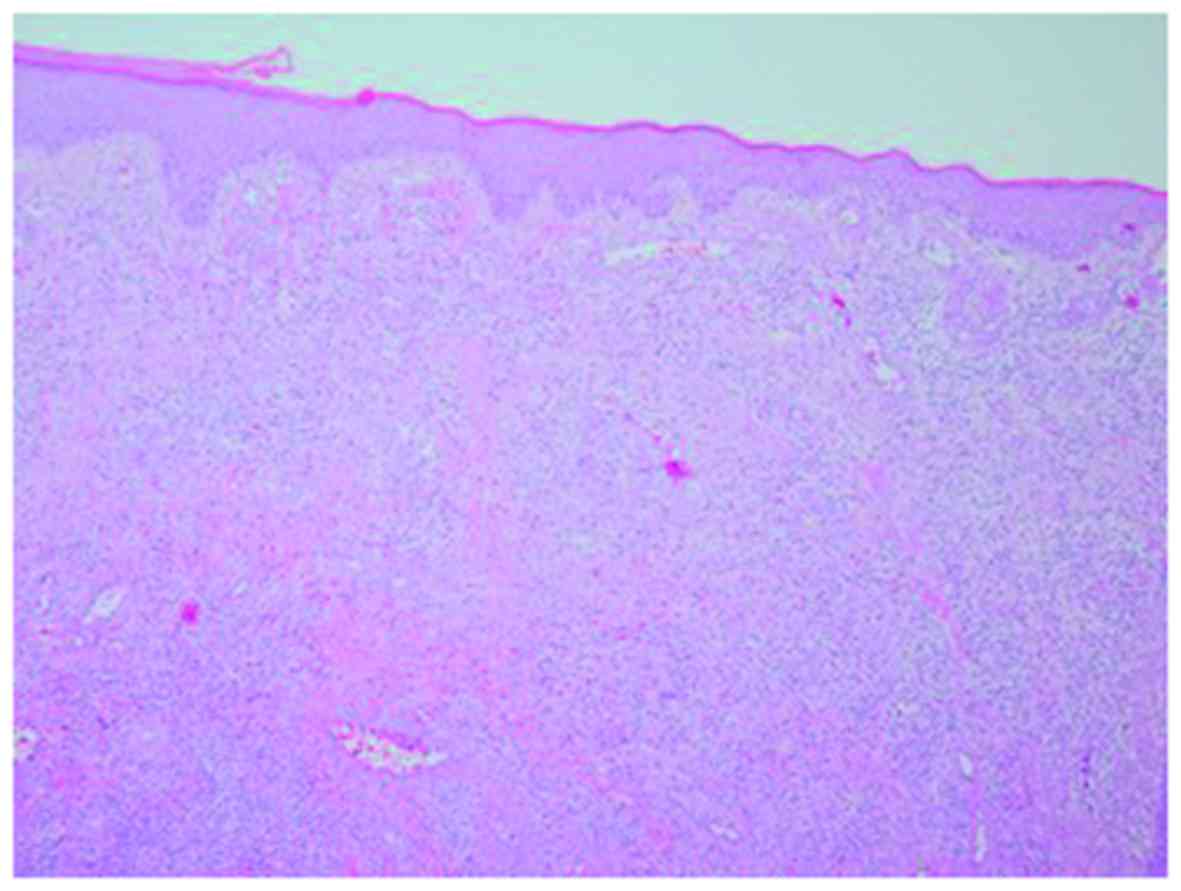
Histopathological examination of the nodule revealed
squamous epithelial hyperplasia, epithelial hyperplasia of the
blood vessels, significant fibroplasia, and granulomatous tissue
formation with a large number of eosinophils, plasmacytes and
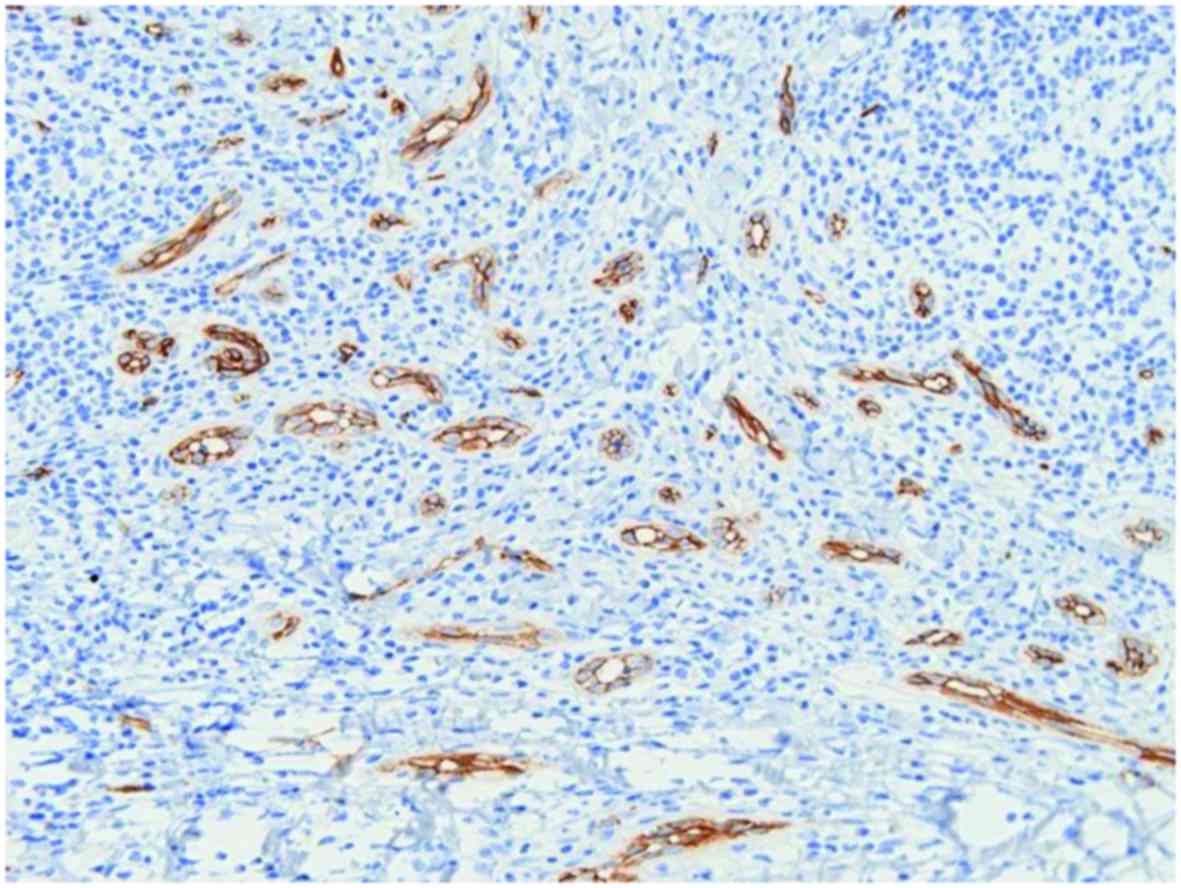
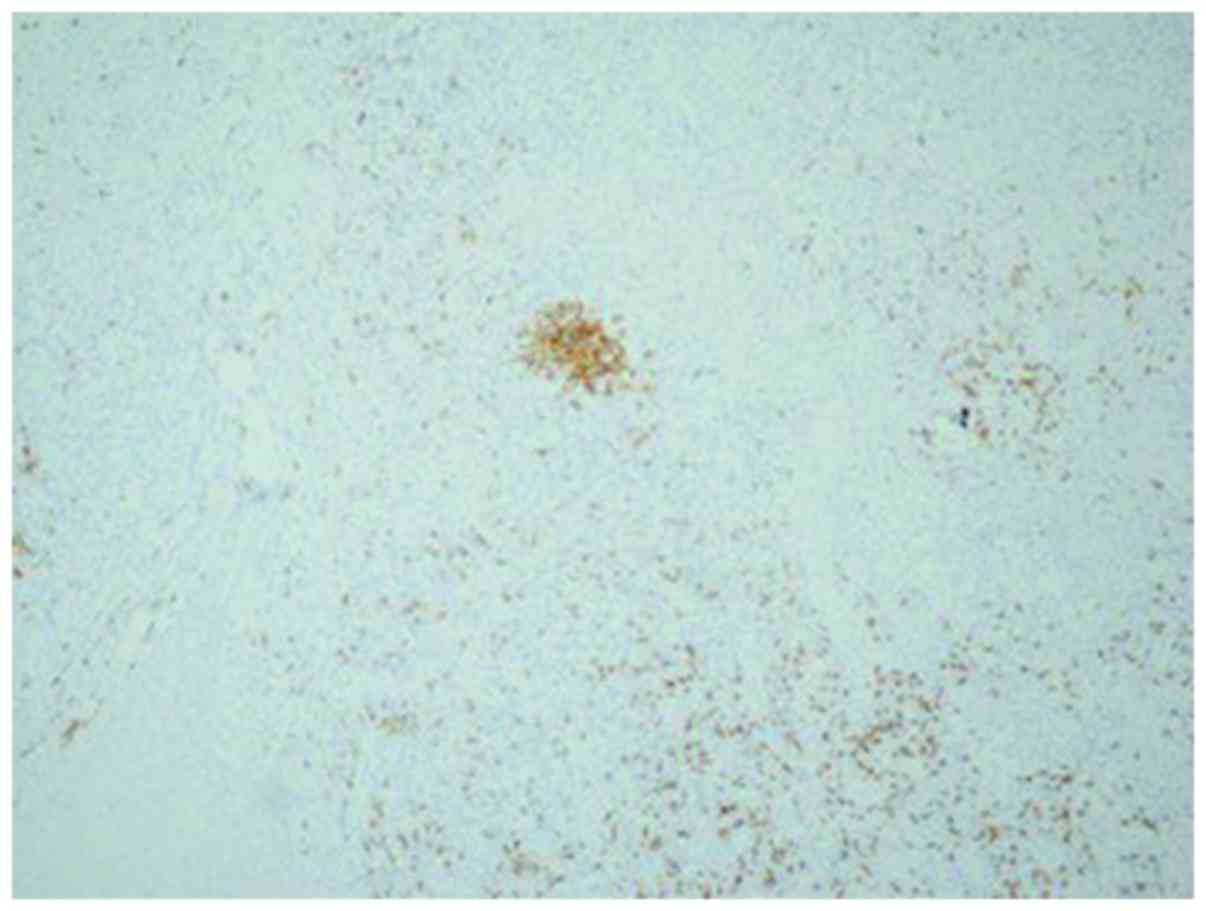
lymphocytes infiltrating the stroma (Fig. 2). CD34 was positive (Fig. 3) in proliferative blood vessels while
the perivascular lymphocytes exhibited CD20 positivity (Fig. 4). The diagnosis of ALHE was
determined on the basis of clinicopathological correlation.
Discussion
ALHE was first described by Wells and Whimster
(4) in 1969, and the etiology and
pathogenesis remains unclear. Certain scholars had considered
benign tumor vascular tissue hyperplasia, or possible blood vessel
reactive hyperplasia to external injury, infection (HTLV/HHV8), or
symptoms of renin or high estrogen (5–7). The
study observed that may be benign or malignant abnormal T
lymphocyte proliferation (8,9). ALHE and Kimura's disease were
originally considered to be the same entity, but are now considered
to be separate disease processes (3).
To date, ALHE cases have been reported worldwide,
but the incidence is currently unknown. ALHE is uncommon but not
rare, and presents most commonly in patients of Asian populations
followed by Caucasians; ALHE may also be more common in Japan than
in other countries. ALHE is more common in females; however, a male
predominance has been noted in a prior Asian study (10). ALHE presents most commonly in
patients aged 20–50 years, with mean age of onset of 30–33 years.
Overall, ~85% of lesions occur in the skin of the head and neck,
with the majority on or near the ear, forehead or scalp (10). The typical clinical manifestations
include pink-brown papules or nodules, single or multiple and 2–3
cm in diameter. AHLE may also occur in the mouth, trunk and
extremities, and the vulva (1,2); rare
sites of involvement include the hands, breast, shoulder and oral
mucosa (11). However, prior case
reports have described incidents of ALHE affecting the penis
(11) and the conjunctiva (12).
A diagnosis of ALHE was determined based on the
clinical characteristics at manifestation and the histopathological
features. The differential diagnosis included Kimura's disease,
pyogenic granuloma (PG), Kaposi's sarcoma, lymphocytoma cutis,
squamous cell carcinoma and angiosarcoma, among others. With the
exception of Kimura's disease, other diseases with these
pathological features are easy to distinguish from ALHE.
Pathologically, both ALHE and Kimura's disease exhibit lymphocytic
and acidophilic cell infiltration. However, there are important
differences in the histopathology of ALHE and Kimura's disease.
ALHE lesions typically present in the dermis and have
histocyte-like or epithelioid vascular endothelial cells, an uneven
thickness of the blood vessels and branching vascular hyperplasia.
Conversely, the pathological changes in Kimura's disease occur
primarily in the subcutaneous tissue, and have a characteristic
lymphoid follicular structure (13,14).
Herein is reported a case of ALHE, which occurs in
the back only rarely. On visual inspection, the patient's lesion
resembled a PG, whereas on palpation the texture was soft. Lymphoid
follicles, eosinophils and branching vascular hyperplasia were not
observed in the surrounding environment. A definitive diagnosis was
reached following pathological examination. In the event a patient
is admitted with an isolated convex neoplasm on the back, with
features of hyperplasia scar tissue, occasional bleeding and
acidophilic cells in the peripheral blood, the differential
diagnosis must consider the possibility of ALHE.
ALHE has a generally favorable prognosis with a low
associated mortality rate. The recommended treatment is surgical
resection, and ~33% of patients experience post-surgical recurrence
(15). This type of disease is
sensitive to deep tissue X-ray irradiation and electron beam
therapy, but these methods carry the risk of inducing a malignant
transformation. For patients unable to receive surgery or
radiotherapy, glucocorticoid treatments are indicated. No cases of
relapse were observed in patients during the follow-up period,
following the complete surgical removal of the lesion.
Acknowledgements
The present study was supported by the Science and
Technology Planning Project of Shenzhen, China (grant no.
JCYJ20150402165325173).
References
|
1
|
Rapini RP, Bolognia JL and Jorizzo JL:
Dermatology: 2-Volume. 2nd. Mosby Elsevier; St. Louis: 2007
|
|
2
|
James WD, Elston D and Berger T: Andrew's
diseases of the skin: Clinical Dermatology. Elsevier Health Sci.
2011.
|
|
3
|
Chitrapu P, Patel M, Readinger A and
Menter A: Angiolymphoid hyperplasia with eosinophilia. Proc (Bayl
Univ Med Cent). 27:336–337. 2014.PubMed/NCBI
|
|
4
|
Wells GC and Whimster IW: Subcutaneous
angiolymphoid hyperplasia with eosinophilia. Br J Dermatol.
81:1–14. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kaur T, Sandhu K, Gupta S, Kanwar AJ and
Kumar B: Treatment of angiolymphoid hyperplasia with eosinophilia
with the carbon dioxide laser. J Dermatolog Treat. 15:328–330.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Miller CJ, Ioffreda MD and Ammirati CT:
Mohs micrographic surgery for angiolymphoid hyperplasia with
eosinophilia. Dermatol Surg. 30:1169–1173. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hollo P, Marschalko M, Sikos G, Harsing J
and Horvath A: Angiolymphoid hyperplasia with eosinophilia in
pregnancy. J Eur Acad Dermatol Venereol. 19:645–646. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kempf W, Haeffner AC, Zepter K, Sander CA,
Flaig MJ, Mueller B, Panizzon RG, Hardmeier T, Adams V and Burg G:
Angiolymphoid hyperplasia with eosinophilia: Evidence for a T-cell
lymphoproliferative origin. Hum Pathol. 33:1023–1029. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shankar S and Russell-Jones R:
Co-existence of lichen amyloidosus and angiolymphoid hyperplasia
with eosinophilia. Clin Exp Dermatol. 29:363–365. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rajendran R, Padmakumar SK, Kothawar S and
Nair B: Angiolymphoid hyperplasia with eosinophilia (ALHE). J Oral
Maxillofac Pathol. 9:24–26. 2005. View Article : Google Scholar
|
|
11
|
Dewan P, Francis ND, Lear JT and Bunker
CB: Angiolymphoid hyperplasia with eosinophilia affecting the
penis. Br J Dermatol. 159:755–757. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Huang M, Lloyd WC III and O'Hara M:
Angiolymphoid hyperplasia with eosinophilia: An unusual
presentation in a child. J AAPOS. 12:302–304. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Filo V, Ferák I and Borecká D: Multiple
unilateral reddish tumors on the ear and forehead in a woman with
early syphilis. Angiolymphoid hyperplasia (ALHE) with eosinophilia
coexisting with early latent syphilis. Arch Dermatol. 130:371–374.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Moy RL, Luftman DB, Nguyen QH and Amenta
JS: Estrogen receptors and the response to sex hormones in
angiolymphoid hyperplasia with eosinophilia. Arch Dermatol.
128:825–828. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mukherjee B, Kadaskar J, Priyadarshini O,
Krishnakumar S and Biswas J: Angiolymphoid hyperplasia with
eosinophilia of the orbit and adnexa. Ocul Oncol Pathol. 2:40–47.
2015. View Article : Google Scholar : PubMed/NCBI
|