Introduction
Osteochondromas are usually extra-articular, as they
predominantly originate from the metaphysis of long bones. However,
intra-articular osteochondromas may also occur, causing pain and
discomfort and restricting the range of motion (1). Osteochondroma of the femoral neck is
rare. It has been described in patients with bursitis, sciatic
nerve compression, femoroacetabular impingement, and fracture at
the stalk of the tumor (2–5). Determining the optimal treatment may be
difficult due to the high risk of avascular necrosis (AVN)
following surgical excision due to the lesion's location. We herein
report a rare case of an intra-articular osteochondroma involving
the posteroinferior aspect of the femoral neck associated with
secondary synovial osteochondromatosis (SOC) of the hip joint in a
25-year-old woman, who was successfully treated with arthroscopic
surgery.
Case report
A 25-year-old woman was referred to the Department
of Orthopaedics Surgery of Chonbuk National University Hospital
(Jeonju, Korea) for pain in the right inguinal region and a limping
gait for 6 months. The pain was exacerbated upon standing and
sitting. The patient had been receiving conservative treatment
including rest, non-steroidal anti-inflammatory drugs and physical
therapy at an outside hospital; however, the symptoms persisted.
Physical examination of the right hip revealed a limited range of
motion, with flexion 70°, extension 30°, external rotation 30° and
internal rotation 10°. The Patrick's test was positive. The results
of the laboratory tests were within normal limits.
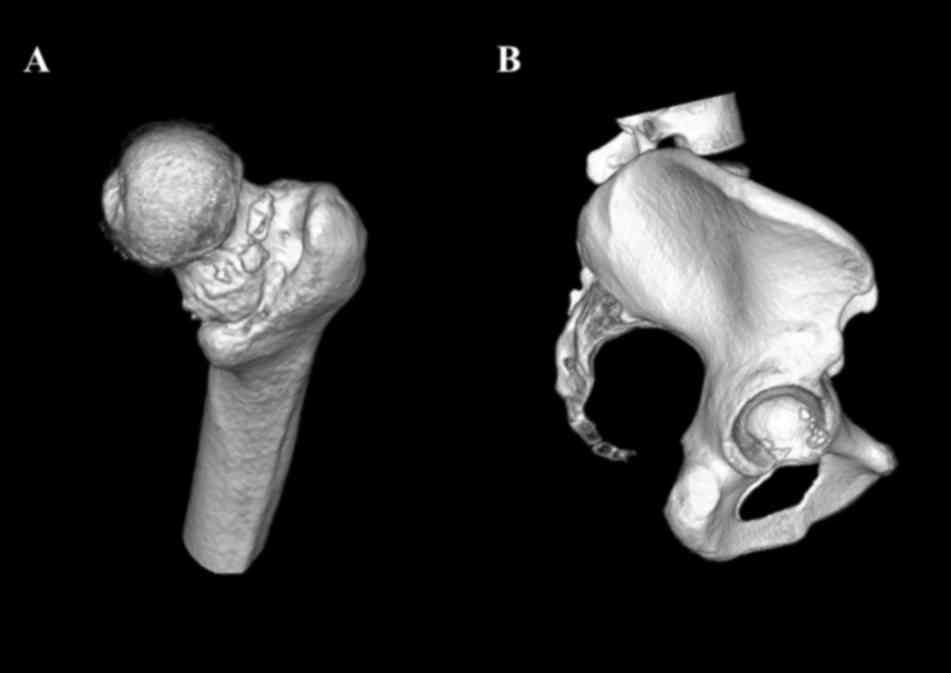
Radiographic examination revealed an osseous
protuberance near the posteroinferior portion of the femoral neck.
Oval-shaped ossifications were observed at the right hip joint
(Fig. 1). There was no sign of
fracture or pre-existing joint abnormality, such as osteoarthritis
or osteonecrosis. Computed tomography was performed for precise
evaluation of the numbers and locations of loose bodies. Loose
bodies were relatively uniform in size with smooth margins, and
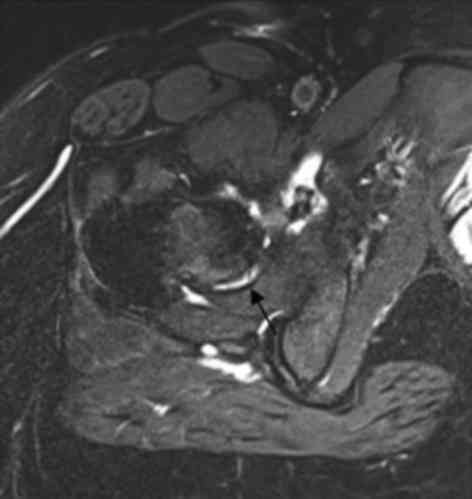
some exhibited internal marrow trabeculation (Fig. 2). T1-weighted axial magnetic
resonance imaging demonstrated an osseous protrusion at the
posteroinferior aspect of the femoral neck, extending to the lesser
trochanter. This osseous protuberance was connected to the bone
marrow of the metaphysis, with a thin surrounding high-signal
structure on fat-suppressed T2-weighted images (Fig. 3). These findings were indicative of
cartilage. Multiple small intra-articular loose bodies <5 mm in
short diameter exhibited a low signal on both T1- and T2-weighted
images.
An arthroscopic approach was selected to minimize
the potential for surgical morbidity. The patient was positioned
supine on the fracture table with the affected limb in traction.
First, the anterolateral portal was positioned over the superior
and anterior borders of the great trochanter. A 70°-angled
arthroscope was used for viewing the hip joint, and the anterior
and posterolateral portals were viewed under direct vision. Saline
was infused under a pressure of 60 mmHg to assist with capsular
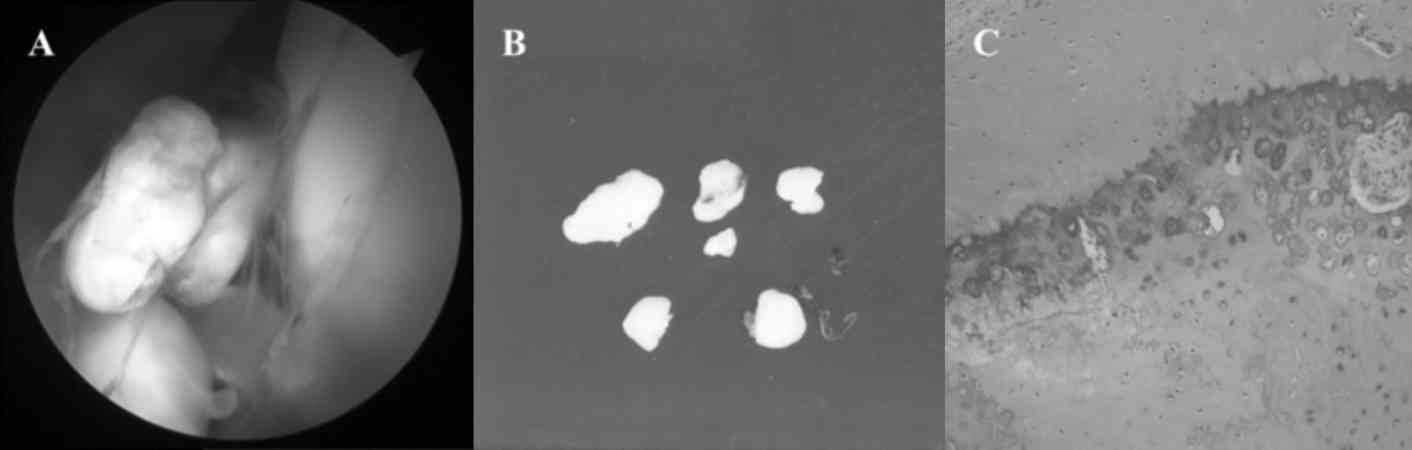
distension during surgery. Several ossified loose bodies and
synovitis of the capsule were observed (Fig. 4A). The osseous loose bodies of the
acetabular fossa and surrounding space were removed (Fig. 4B). No lesions suggested osteochondral
fracture or osteochondritis dissecans in the hip joint.
Histologically, the loose bodies were round cartilaginous nodules
with endochondral ossification. A central osteocartilaginous core
was enclosed within fibrotic synovial tissue (Fig. 3C). The patient was discharged after
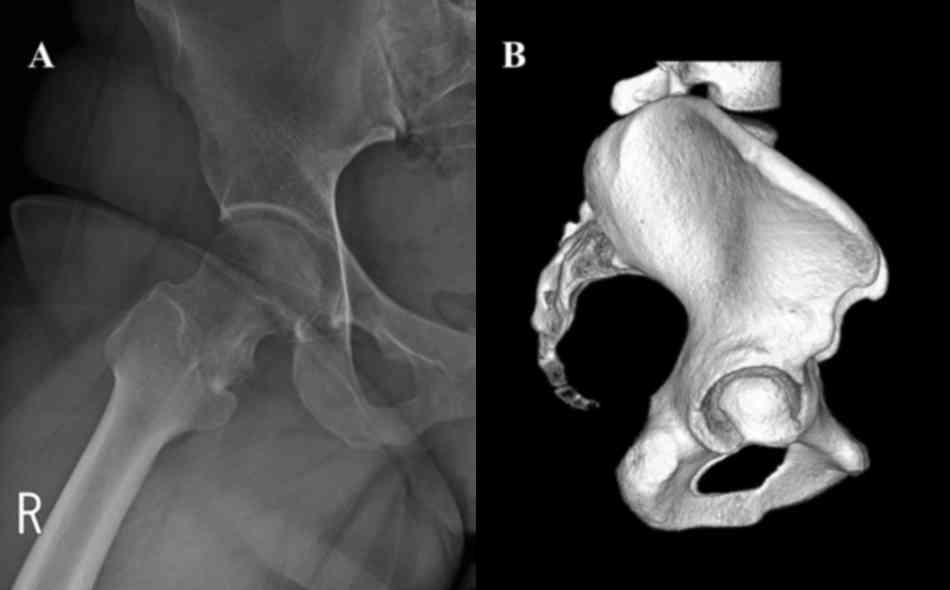
postoperative wound care and was followed up for 2 years; at the
last follow-up visit (August 2016) she remained in good condition,
with a full range of motion of the hip joint and without signs of
limping, SOC recurrence, or femoral head AVN (Fig. 5).
Discussion
Arthrotomy and arthroscopic surgery were considered
for the treatment of the patient in the present case. Accessing
posterior lesions of the femoral neck is difficult through the
anterior surgical hip dislocation procedure reported by Ganz et
al (6) The lesion is easily
approached through a posterior dislocation procedure; however, the
risk of soft tissue and vascular damage is high with this approach.
The most worrisome consideration for surgical hip dislocation is
the occurrence of postoperative femoral head AVN. As the median
circumflex artery was close to the femoral neck lesion in our
patient, she was considered to be at high risk for AVN of the
femoral head associated with damage to the median circumflex
artery.
To avoid femoral head AVN, arthroscopic removal of
loose bodies of the acetabular fossa and surrounding space was
performed. However, the limited working area in the hip joint
complicated visualization and instrument manipulation. The
anterior, anterolateral and posterolateral portals were used to
address the limited visualization and working space. Visualization
was improved by using a 70° arthroscope, sufficient traction, and
capsular distension of the hip joint.
Ilizaliturri et al (7) reported that the lateral synovial fold
is a constant, reliable landmark for arthroscopically identifying
the blood supply of the hip. Since the branches of the median
circumflex artery are posterior to this landmark, capsular or bony
resection must not be performed posterior to the lateral synovial
fold. Therefore, a partial synovectomy was also performed in a
limited area that did not exceed the lateral synovial fold. The
patient has been followed up for 2 years, and she continues to have
full range of motion of the hip joint, with no signs of limping,
SOC recurrence, or femoral head AVN. However, the future
possibility of osteochondromatosis recurrence and resection of the
femoral neck osseous mass must be considered.
Multiple osseous loose bodies in the hip joint are
usually caused by osteochondral fractures, osteochondritis
dissecans, or pre-existing joint abnormalities, such as
osteoarthritis, osteonecrosis, or rheumatoid arthritis. SOC may
also be a rare cause. In present case, no pre-existing joint
abnormalities, such as osteoarthritis, osteonecrosis, or rheumatoid
arthritis were found. In addition, no lesions that suggested
osteochondral fracture or osteochondritis dissecans were observed
in the hip joint. Primary SOC was ruled out based on the absence of
pathognomonic findings, such as numerous and relatively small
osteochondral loose bodies throughout the joint (8).
Milgram et al hypothesized that osteochondral
loose bodies may slowly grow with nourishment from the synovial
fluid, while loose bodies are free of synovial attachments
(9). Peh et al have described
patients with secondary SOC around the osteochondromas of the
femoral neck and pubic bone. They suggested that cartilaginous
debris from the osteochondroma can stimulate metaplastic changes in
the synovial lining, contributing to further development of
osteochondral nodules (4).
In the present case, the presence of osteochondroma
was considered to have played a significant role in the development
of SOC. Due to the specific anatomy, mechanical blockage may occur
through direct contact of the widened and enlarged femoral neck
against the acetabular rim. This mechanism damages the labrum and
adjacent articular cartilage. Although no definitive association
between trauma and the development of SOC has been confirmed,
limited evidence supports microtrauma as a precipitating factor in
certain cases (10). The
cartilaginous debris may have been nourished by synovial fluid to
provoke repetitive traumatic inflammatory reactions and irritation
caused by the loose body itself.
In conclusion, the appropriate treatment of an
intra-articular osteochondroma involving the posteroinferior aspect
of the femoral neck associated with secondary SOC may be difficult
due to a high risk of AVN following surgical excision. The present
case was successfully treated with arthroscopic removal of SOC, and
the patient's symptoms completely resolved without recurrence.
The patient signed an informed consent for the
publication of this case report and any accompanying images.
Ethical approval of this study was waived by the Ethics Committee
of Chonbuk National University Hospital, as this was a case report
and the number of patients was <3.
References
|
1
|
Siebenrock KA and Ganz R: Osteochondroma
of the femoral neck. Clin Orthop Relat Res. 211–218. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jung HT, Hwang DS, Jeon YS and Kim PS:
Arthroscopic resection of osteochondroma of hip joint associated
with internal snapping: A case report. Hip Pelvis. 27:43–48. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kanauchi T, Suganuma J, Kawasaki T,
Mochizuki R, Inoue Y, Uchikawa S, Kitamura K and Honda A: Fracture
of an osteochondroma of the femoral neck caused by impingement
against the ischium. Orthopedics. 35:e1438–e1441. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Peh WC, Shek TW, Davies AM, Wong JW and
Chien EP: Osteochondroma and secondary synovial
osteochondromatosis. Skeletal Radiol. 28:169–174. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ilica Turan A, Yasar E, Sanal Tuba H,
Duran C and Guvenc I: Sciatic nerve compression due to femoral neck
osteochondroma: MDCT and MR findings. Clin Rheumatol. 27:403–404.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ganz R, Gill TJ, Gautier E, Ganz K, Krügel
N and Berlemann U: Surgical dislocation of the adult hip a
technique with full access to the femoral head and acetabulum
without the risk of avascular necrosis. J Bone Joint Surg Br.
83:1119–1124. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ilizaliturri VM Jr, Orozco-Rodriguez L,
Acosta-Rodríguez E and Camacho-Galindo J: Arthroscopic treatment of
cam-type femoroacetabular impingement: Preliminary report at 2
years minimum follow-up. J Arthroplasty. 23:226–234. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Murphey MD, Vidal JA, Fanburg-Smith JC and
Gajewski DA: Imaging of synovial chondromatosis with
radiologic-pathologic correlation. Radiographics. 27:1465–1488.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Milgram JW: The development of loose
bodies in human joints. Clin Orthop Relat Res. 292–303.
1977.PubMed/NCBI
|
|
10
|
Wright JM, Matayoshi E and Goldstein AP:
Bursal osteochondromatosis overlying an osteochondroma of a rib. A
case report. J Bone Joint Surg Am. 79:1085–1088. 1997. View Article : Google Scholar : PubMed/NCBI
|