Introduction
Extrauterine manifestations of leiomyomas are rare.
Within the gastrointestinal tract, leiomyomas predominately occur
in the esophagus (1). Gastric
leiomyomas are benign submucosal tumors composed of smooth muscle
cells, and account for 2.5% of all gastric neoplasms (2,3).
Leiomyomas are most frequently encountered in patients aged 50–70
years and bear no gender predilection (4). These tumors are slow-growing and
usually asymptomatic; however, they may become clinically evident
when the overlying gastric mucosa ulcerates with ensuing
hemorrhage. Herein, we describe the case of a 68-year-old female
patient presenting with hematemesis and found to have a gastric
submucosal lesion on esophagogastroduodenoscopy (EGD), which was
diagnosed as a gastric leiomyoma following histopathological
examination.
Case report
A 68-year-old female patient with a medical history
of chronic gastritis, hypertension, hyperlipidemia, atrial
fibrillation (not on anticoagulation), a cerebral vascular event
with residual left-sided weakness, seizure disorder, iron
deficiency anemia, and anemia of chronic disease, presented with a
complaint of hematemesis. On physical examination, the abdomen was
soft, non-tender and non-distended. The heart rate was 85
beats/min, the blood pressure was 123/80 mmHg, the respiratory rate
was 20 breaths/min, with an oxygen saturation of 95% on room air
and a temperature of 97.6°F. The laboratory findings were as
follows: Sodium 143 mmol/l, potassium 3.6 mmol/l, albumin 2.7 g/dl,
alkaline phosphatase 47 U/l, aspartate aminotransferase 13 U/l,
alanine aminotransferase 10 U/l, hemoglobin 5.1 g/dl, hematocrit
17%, white blood cell count 16.1 K/cmm, and platelet count 262
K/cmm.
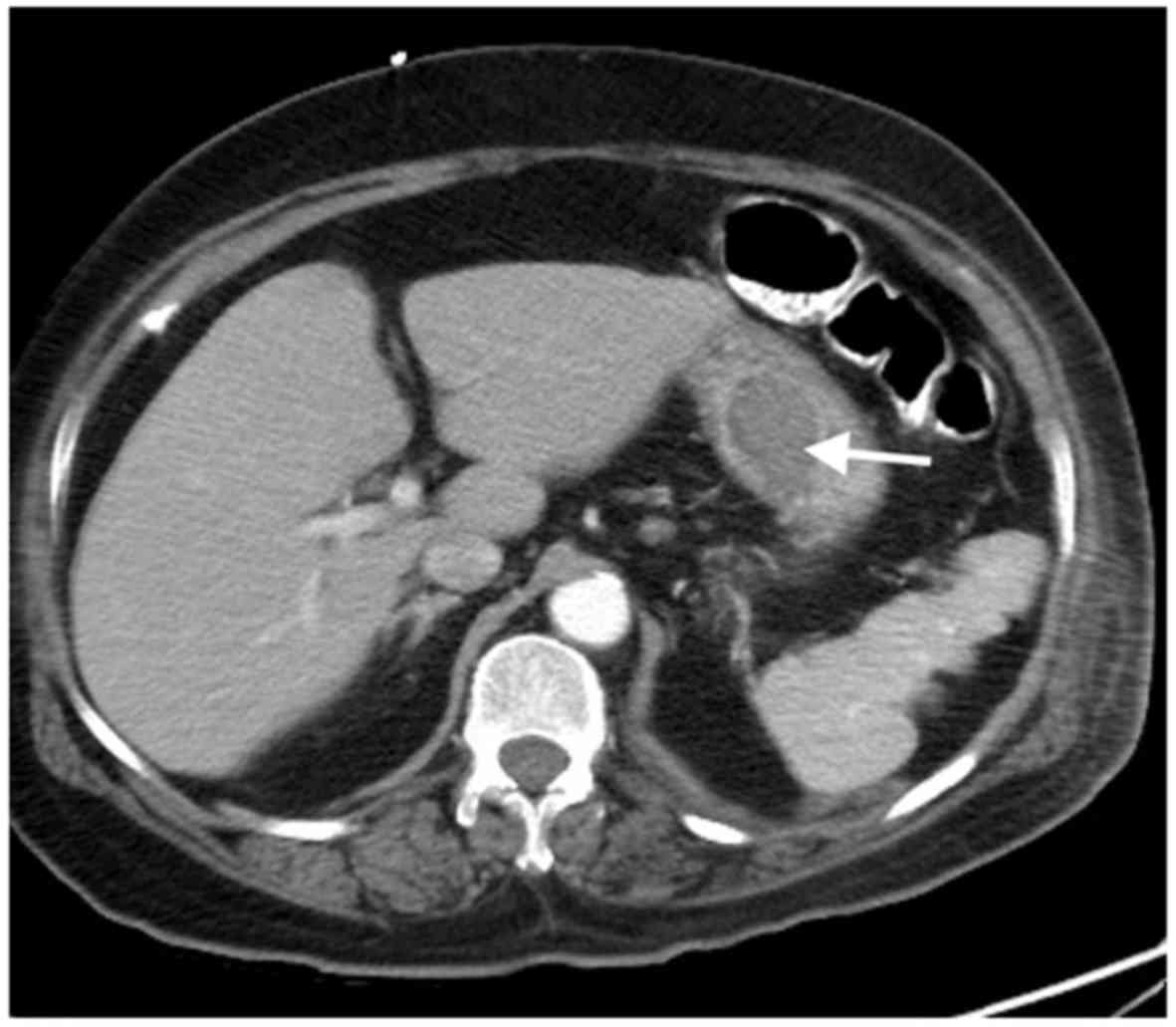
An abdominal computed tomography (CT) scan revealed
a mass lesion seen protruding from the gastric lesser curvature
into the lumen, measuring ~4.1×2.6 cm (Fig. 1). There was no evidence of extension
of the mass outside the walls of the stomach. During
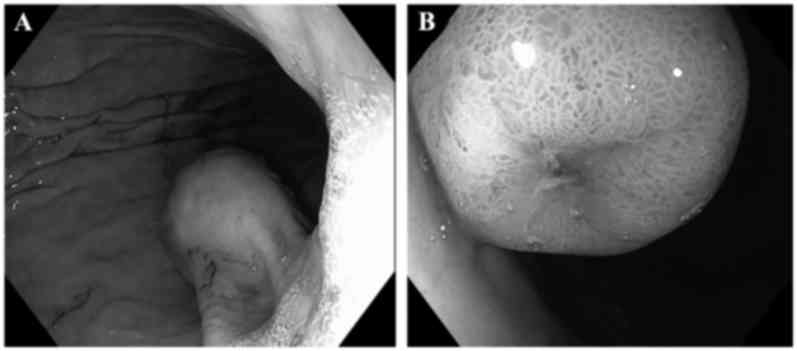
esophagogastroduodenoscopy (EGD), a 4-cm submucosal lesion was
identified along the lesser curvature of the stomach near the
cardia (Fig. 2). Two umbilicated
areas of ulceration were seen over the lesion, with no active
bleeding. The lesion was biopsied without excision. To
histologically process the biopsied specimen, a section ≤3-mm thick
was used. The section was fixed using 10% neutral buffered
formalin. Next, the section slide was left in a 65°C oven to melt
the paraffin. Finally, staining protocol for hematoxylin and eosin
staining were performed at room temperature for 45 min. Following
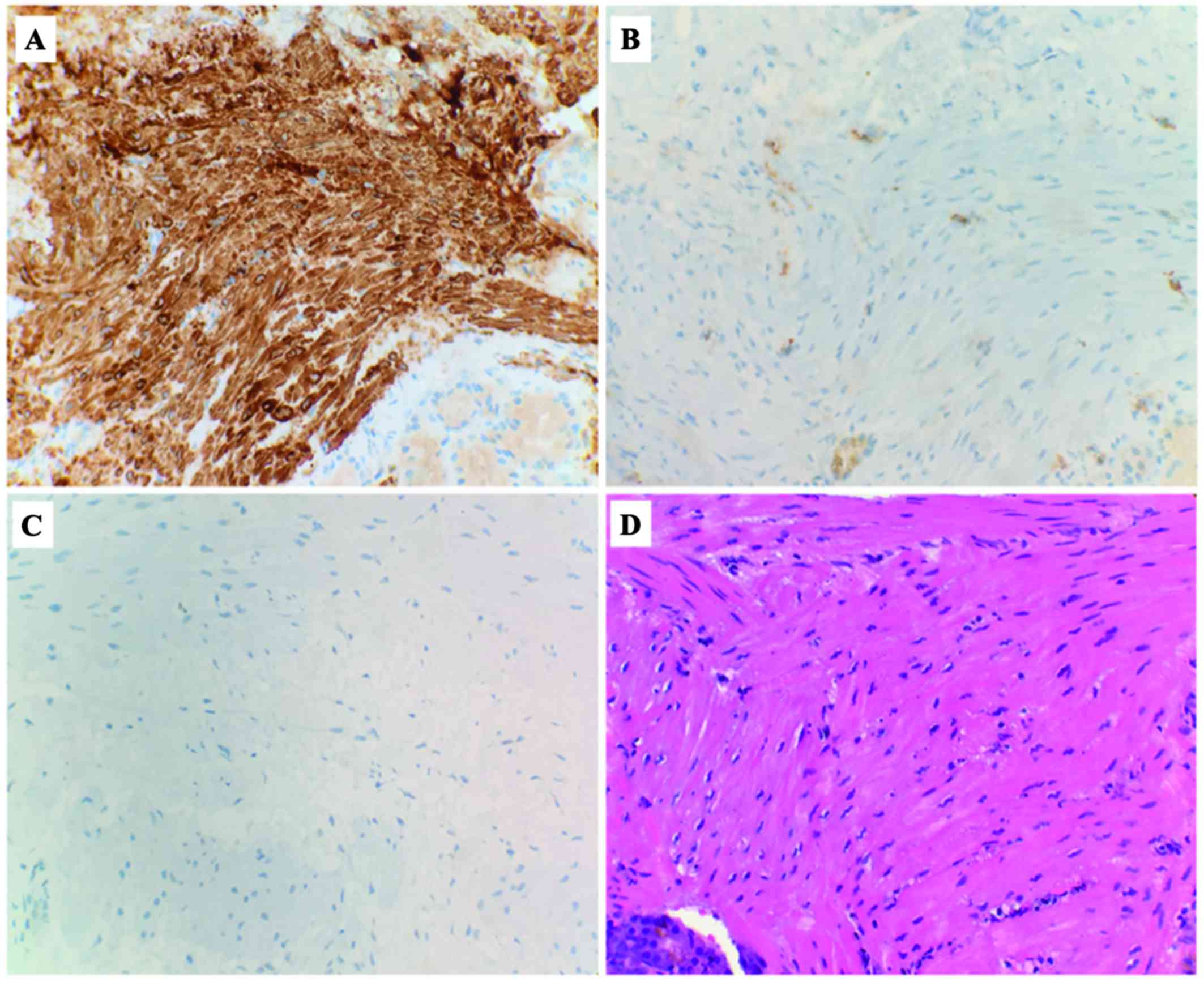
histopathological processing, light microscopy revealed that the
lesion was composed of bundles of elongated cells with oblong
nuclei, and a submucosa with smooth muscle cell proliferation. On
immunohistochemical examination, the cells of the lesion were
positive for smooth muscle myosin heavy chain and negative for
CD117 (c-kit) and S-100; the proliferation index (Ki-67) was
<10% (Fig. 3). These findings
were consistent with the diagnosis of gastric leiomyoma. Following
the procedure, the same day, the patient made a good recovery.
Consent was obtained from the patient regarding the publication of
the case details and associated images.
Discussion
Leiomyomas of the gastric cardia appear as
homogeneous, low-attenuation masses with an endoluminal growth
pattern, often ranging from 1.3 to 4.7 cm in diameter (5,6). These
tumors may also be found in the corpus and antrum of the stomach.
When the tumors grow to >2 cm, they are more likely to present
with central ulceration (6). The
differential diagnosis of leiomyomas includes gastrointestinal
stromal tumors (GISTs) and schwannomas. Histologically, they appear
as round, solitary lesions arising from the muscularis mucosae,
muscularis propriae, and possibly from smooth muscle of the vessel
wall in the bowel (3). Their benign
nature is evidenced by the microscopic appearance of abundant
hyperplastic smooth muscle cells with minimal mitotic activity and
low c-kit expression (7). However,
the pathogenesis of gastric leiomyomas remains largely unclear.
In the past, leiomyomas and GISTs were referred to
interchangeably. However, it is clinically important to distinguish
these two entities, as leiomyomas are benign, while GISTs may
display malignant potential (8).
True leiomyomas are strongly and diffusely positive for desmin and
smooth muscle actin (7).
Additionally, true leiomyomas and schwannomas stain negative for
CD117 and CD34, while GISTs are positive for these markers
(9,10). Leiomyomas tend to occur in younger
patients compared with GISTs (7).
Leiomyosarcomas are far less common and can be differentiated from
leiomyomas by their very high mitotic rate (11).
The clinical presentation of leiomyomas depends on
their size and location. The majority of gastric leiomyomas are
slow-growing and asymptomatic; therefore, they are usually found
incidentally on EGD, surgical exploration, or at autopsy (12). When symptomatic, leiomyomas manifest
with upper gastrointestinal bleeding, atypical epigastric pain or
non-specific dyspepsia, generally due to mucosal ulceration
(13). The predisposing factors
associated with gastric leiomyoma bleeding include treatment with
anticoagulants, non-steroidal anti-inflammatory drugs and
corticosteroids (14–16). Endoscopically, leiomyomas appear as
smooth, well-defined tumors, with stretched and effaced mucosal
folds overlying the lesions, also referred to as the Schindler's
sign (17).
According to the American Gastrointestinal
Association (AGA), patients with submucosal tumors <3 cm may be
followed up by periodic EGD or endoscopic ultrasound examinations,
while lesions >3 cm, in which the malignant potential cannot be
determined by less invasive means, require surgical or endoscopic
excision for diagnosis (18,19). If the tumor is not removed, it may
invade surrounding tissue. In conclusion, gastric leiomyoma is a
rare, benign submucosal tumor originating from smooth muscle cells,
most commonly found in the gastric cardia. It bears no predilection
for gender and is most frequently found in patients aged 50–70
years. It is important to differentiate leiomyoma from
leiomyosarcoma, which is a malignant tumor, and from GISTs, which
possess malignant potential. Furthermore, according to AGA practice
guidelines, surgical or endoscopic resection is recommended for
tumors sized >3 cm. The patients with surgically resected tumors
have a favorable clinical outcome.
Acknowledgements
Not applicable.
Funding
No funding was received.
Authors' contributions
DR, QTT and SN conceived and designed the study. DR
and QTT drafted the manuscript. EO, SN, DE and MR critically
revised the manuscript for intellectual content. All authors
approved the manuscript for submission.
Availability of data and materials
Not applicable.
Ethics approval
This manuscript was acknowledged and approved by The
Brooklyn Hospital Center Institutional Review Board on June 22,
2017 (no. 1082889-1).
Consent for publication
The patient provided written informed consent for
the publication of the case details and associated images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wang ZQ, Wang S, Ye YJ, Kang YL, Sun KK
and Zheng HF: Gastrointestinal mesenchymal tumors: A clinical
pathologic and immunohistochemical study of 210 cases. Zhonghua Wei
Chang Wai Ke Za Zhi. 10:11–16. 2007.(In Chinese). PubMed/NCBI
|
|
2
|
Morgan BK, Compton C, Talbert M, Gallagher
WJ and Wood WC: Benign smooth muscle tumors of the gastrointestinal
tract. A 24 year experience. Ann Surg. 211:63–66. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Agaimy A and Wünsch PH: True smooth muscle
neoplasms of the gastrointestinal tract: Morphological spectrum and
classification in a series of 85 cases from a single institute.
Langenbecks Arch Surg. 392:75–81. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gupta AK, Berry M and Mitra DK: Ossified
gastric leiomyoma in a child: A case report. Pediatr Radiol.
25:48–49. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hur BY, Kim SH, Choi JY, Rha SE, Lee MW,
Kim SY, Han JK and Choi BI: Gastroduodenal glomus tumors:
Differentiation from other subepithelial lesions based on dynamic
contrast-enhanced CT findings. AJR Am J Roentgenol. 197:1351–1359.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lee MJ, Lim JS, Kwon JE, Kim H, Hyung WJ,
Park MS, Kim MJ and Kim KW: Gastric true leiomyoma: Computed
tomographic findings and pathological correlation. J Comput Assist
Tomogr. 31:204–208. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Miettinen M, Sobin LH and Sarlomo-Rikala
M: Immunohistochemical spectrum of GISTs at different sites and
their differential diagnosis with a reference to CD117 (KIT). Mod
Pathol. 13:1134–1142. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kang HC, Menias CO, Gaballah AH, Shroff S,
Taggart MW, Garg N and Elsayes KM: Beyond the GIST: Mesenchymal
tumors of the stomach. Radiographics. 33:1673–1690. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Greenson JK: Gastrointestinal stromal
tumors and other mesenchymal lesions of the gut. Mod Pathol.
16:366–375. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ramai D, Lai J, Changela K, Reddy M and
Shahzad G: Transverse colon schwannoma treated by endoscopic
mucosal resection: A case report. Mol Clin Oncol. 7:830–832. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Miettinen M: Smooth muscle tumors of soft
tissue and non-uterine viscera: Biology and prognosis. Mod Pathol.
27 Suppl 1:S17–S29. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Payne WG, Murphy CG and Grossbard LJ:
Combined laparoscopic and endoscopic approach to resection of
gastric leiomyoma. J Laparoendosc Surg. 5:119–122. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Matsuda M, Watanabe Y, Tonosu N, Nabeya Y,
Arima H, Matsuzaki H, Ohira G, Sato H, Mizushima T and Uehara T:
Hemoperitoneum secondary to exophytic leiomyoma: report of a case.
Surg Today. 30:448–450. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Stalnikowicz R, Eliakim R, Ligumsky M and
Rachmilewitz D: Drug-induced bleeding of gastric leiomyoma. Am J
Gastroenterol. 82:419–420. 1987.PubMed/NCBI
|
|
15
|
Saxton NL: Hemorrhage from a gastric
leiomyoma during anticoagulant therapy. Report of a case. J Iowa
State Med Soc. 51:717–721. 1961.PubMed/NCBI
|
|
16
|
Din NA: Aspirin-induced haemorrhage in
gastric leiomyoma. J R Coll Surg Edinb. 18:246–248. 1973.PubMed/NCBI
|
|
17
|
Apostolopoulos P, Zalonis A, Karamoutzos
A, Mavrogiannis P, Vlachou E, Tsibouris P and Alexandrakis G:
Endoscopic submucosal dissection for the diagnosis and treatment of
a gastric submucosal tumor: Initial experience in Greece. Ann
Gastroenterol. 25:358–360. 2012.PubMed/NCBI
|
|
18
|
Schindler R, Blomquist OA, et al:
Leiomyosarcoma of the stomach; its roentgenologic and gastroscopic
diagnosis and its possible relationship to pernicious anemia. Surg
Gynecol Obstet. 82:239–252. 1946.PubMed/NCBI
|
|
19
|
Hwang JH, Rulyak SD and Kimmey MB:
American Gastroenterological Association Institute: American
gastroenterological association institute technical review on the
management of gastric subepithelial masses. Gastroenterology.
130:2217–2228. 2006. View Article : Google Scholar : PubMed/NCBI
|