Introduction
Fibrous dysplasia (FD) is a benign developmental
anomaly of intramedullary fibro-osseous tumorlike lesion
characterized by substituting fibrous connective tissue for normal
bone and marrow (1–3). It accounts for approximately 5% of
benign bone tumors around the world (4) and the incidence in China is 10–30 cases
per million (5). The craniofacial,
axial, and/or appendicular skeleton can be involved separately or
simultaneously by fibrous dysplasia, ranging from isolated
asymptomatic monostotic lesions uncovered accidentally to grave
incapacitating polyostotic lesions leading to pain, fracture,
deformity or loss of vision and hearing (6–8).
The surgical treatment of fibrous dysplasia of bone
is a challenge to orthopedic surgeons due to its wide clinical
spectrum and variation such as massive involvement, deformity and
pathological fracture.
There are no clear guidelines established for
orthopedic management of fibrous dysplasia of bone. Multifarious
treatments are reported based on the initial assessment age,
location and type of the lesion including conventional surgical
procedures like curettage or en bloc resection with bone grafting
in monostotic lesions and specific interventions like osteotomy
with internal fixation aiming at the prevention or correction of
bony deformities in extended lesions (5,9–15). Therefore, we undertook a
retrospective study of 22 patients and share our findings about FD
in terms of surgical management and outcomes.
Materials and methods
A retrospective study was performed in 22 patients
(23 lesions) histologically diagnosed with fibrous dysplasia (FD)
who were surgically treated in our hospital between December 2011
and July 2015 (Including one patient with two lesions, whose tibia
lesion was treated in another institute). Of these 22 patients, the
sex ratio was 1:1 and the age at operation ranged from 15 to 48
years with an average of 28.4 years.
Surgical operations including curettage and bone
grafting with or without internal fixation and osteotomy were
planned upon symptoms, impending fracture or progressive deformity.
Internal fixations were all provide by DePuy-Synthes, Paoli, CA,
USA and included plate and screws (P&S), dynamic hip screw
(DHS), intramedullary nail (IMN), proximal femoral nail
anti-rotation (PFNA). And massive allografts and internal fixations
were applied in lesions with low bone stock left after curettage.
Limited weight-bearing were allowed for all postoperative patients
for about 3 months.
To analysize the outcome, the functional evaluation
system of the Musculoskeletal Tumor Society (MSTS) score was used
in numberical scores and percentage rates caculated for the
extremities invovled. A percentage rate of over 70% was considered
to be a satisfactory result (16).
The radiographic result was considered as satisfactory, if there
was no local recurrence, pathological fracture, progression of
deformity or nonunion of bone.
This study was conducted in accordance with the
Declaration of Helsinki and with approval from the Ethics Committee
of West China Hospital (Chengdu, China). Written informed consent
was obtained from all participants or their guardians.
Results
Fourteen patients had a monostotic disease (MFD), of
which four patients were asymptomatic, eight patients presented
with pain and the other two had pathological fracture. Seven
patients had polyostotic disease (PFD) with complication of pain
and two of which suffered from pathological fracture. Further
details on sex, primary complaint, medical course, location, and
treatment were listed on Table I.
And the detailed clinical outcome was shown in Table II.
 | Table I.Clinical data. |
Table I.
Clinical data.
| Case | Sex | Age at operation | Lesion type | Follow-up period
(months) | Primary
complaints | Lesions undergone
surgery | Site | Treatment |
|---|
| 1 | Male | 16 | M | 37.1 | Pain | Ilium | L | CUR+BCG |
| 2 | Female | 45 | M | 23.7 | Pain | Ilium | L | CUR+BCG |
| 3 | Male | 31 | M | 17.1 | Found by chance | Ilium | R | CUR+BCG |
| 4 | Male | 45 | M | 18.3 | Found by chance | Ilium | L | CUR+BCG |
| 5 | Male | 42 | M | 21.3 | Pain | Proximal femur | R | CUR+BCG+PFNA |
| 6 | Male | 50 | M | 16.5 | Pain | Proximal femur | R | CUR+BCG+DHS |
| 7 | Male | 25 | M | 16.4 | Found by chance | Proximal femur | L | CUR+BCG+DHS |
| 8 | Female | 21 | M | 17.0 | Pain | Proximal femur | L | CUR+BCG+DHS |
| 9 | Male | 38 | M | 16.8 | Found by chance | Proximal femur | L | CUR+BCG+DHS |
| 10 | Female | 42 | M | 17.0 | Pain | Proximal femur | R | CUR+BCG+DHS |
| 11 | Female | 19 | M | 22.0 | Pain | Proximal femur | L | CUR+BCG+DHS |
| 12 | Male | 18 | M | 21.5 | Pain | Proximal femur | L | OST+CUR+BCG+IMN |
| 13 | Male | 16 | M | 17.6 | Fracture | Middle humerus | L | CUR+BCG+P&S |
| 14 | Female | 27 | M | 18.5 | Fracture | Middle humerus | R | CUR+FG+P&S |
| 15 | Male | 20 | P | 23.4 | Pain and limp | Tibia | L | OST
+CUR+BCG+IMN |
| 16 | Female | 48 | P | 20.1 | Pain and limp | Proximal femur | R |
OST+CUR+BCG+IMN |
| 17 | Female | 16 | P | 36.9 | Pain and limp | Proximal femur | R |
OST+CUR+BCG+PFNA |
| 18 | Female | 15 | P | 27.1 | Pain | Tibia | L | IMN |
| 19aa | Male | 17 | P | 43.1 | Pain | Tibia | R | CUR+BCG+IMN |
| 19b | Male | 18 | P | 30.6 | Pain | Proximal femur | R | CUR+BCG+PFNA |
| 20 | Female | 40 | P | 51.8 | Pain | Total femur | L | CUR+BCG+IMN |
| 21 | Female | 16 | P | 15.9 | Fracture | Total femur | L | CUR+BCG+PFNA |
| 22a | Female | 17 | P | 58.6 | Pain | Proximal femur | L | CUR+BCG+PFNA |
| 22b | Female | 21 | P | 15.1 | Pain | Tibia | L | CUR+BCG+AG |
 | Table II.Details of treatment outcome. |
Table II.
Details of treatment outcome.
|
|
|
| MSTS |
|
|
|---|
|
|
|
|
|
|
|
|---|
| Case | Lesions | Treatment | Pre | Post | Radiographic
results | Complications and
management |
|---|
| 1a | Ilium | CUR+BCG | 24 | 29 | S | None |
| 2a | Ilium | CUR+BCG | 24 | 30 | S | None |
| 3a | Ilium | CUR+BCG | 27 | 29 | S | None |
| 4a | Ilium | CUR+BCG | 27 | 30 | S | None |
| 5 | Proximal femur | CUR+BCG+PFNA | 17 | 28 | S | None |
| 6 | Proximal femur | CUR+BCG+DHS | 19 | 28 | S | None |
| 7 | Proximal femur | CUR+BCG+DHS | 28 | 29 | S | None |
| 8 | Proximal femur | CUR+BCG+DHS | 19 | 28 | S | None |
| 9 | Proximal femur | CUR+BCG+DHS | 27 | 29 | S | None |
| 10 | Proximal femur | CUR+BCG+DHS | 22 | 28 | S | None |
| 11 | Proximal femur | CUR+BCG+DHS | 22 | 29 | S | None |
| 12 | Proximal femur |
OST+CUR+BCG+IMN | 15 | 27 | S | None |
| 13 | Middle humerus |
CUR+BCG+P&S | 11 | 27 | S | None |
| 14 | Middle humerus | CUR+FG+P&S | 10 | 28 | S | None |
| 15 | Tibia |
OST+CUR+BCG+IMN | 13 | 24 | S | None |
| 16 | Distal fibula |
OST+CUR+BCG+IMN | 24 | 26 | S | None |
| 17 | Proximal femur |
OST+CUR+BCG+PFNA | 13 | 25 | S | None |
| 18 | Tibia | IMN | 20 | 28 | S | None |
| 19ab | Tibia | CUR+BCG+IMN | – | 28 | S | None |
| 19b | Proximal femur | CUR+BCG+PFNA | 19 | 28 | S | None |
| 20 | Total femur | CUR+BCG+IMN | 17 | 25 | S | None |
| 21 | Total femur | CUR+BCG+PFNA | 4 | 11 | U | Spiral blade
cutting out; Revision with AG; Poor outcome |
| 22a | Proximal femur | CUR+BCG+PFNA | 21 | 28 | S | None |
| 22b | Tibia | CUR+BCG+AG | 23 | 27 | S | None |
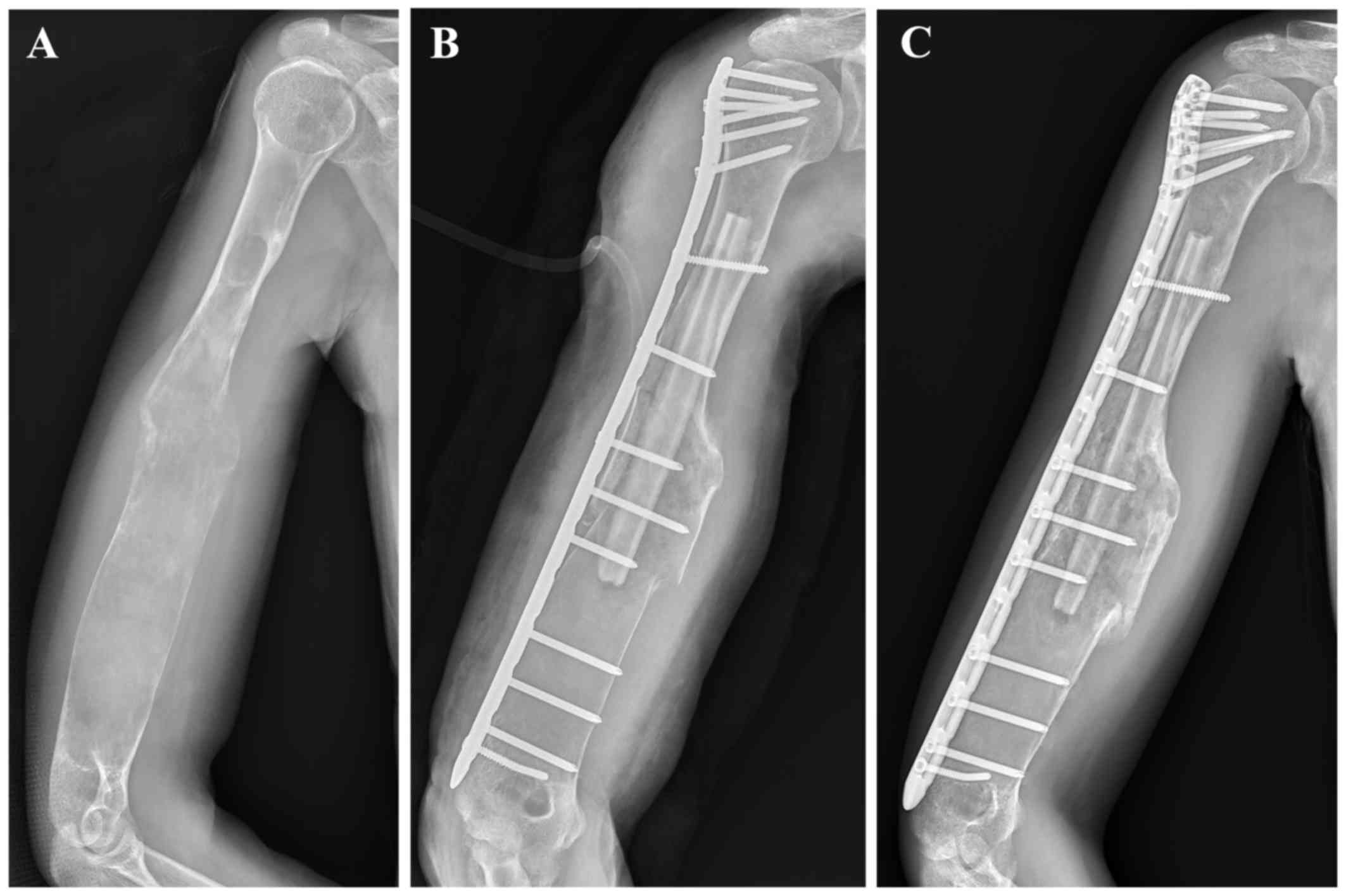
Monostotic group
Four patients (4/14) in the monostotic group were
asymptomatic, including two ilia and two proximal femurs. They were
treated with curettage and bone grafting with or without internal
fixations. Osteotomy, curettage, bone grafting and internal
fixation were applied in one patient with pain and shepherd crook
deformity in proximal femur. Two patients presented with
pathological fracture of the middle humerus and were treated with
curettage, bone grafting, internal fixation of plate and screws
(One typical case was showed in Fig.
1). Two patients with a symptomatic lesion in the
none-weight-bearing ilium were treated with simple curettage and
bone grafting, while the other five patients with a symptomatic
lesion in the weight-bearing femur undergone curettage, bone
grafting with dynamic hip screw (DHS) or proximal femoral nail
anti-rotation (PFNA). Bone union and satisfactory radiographic and
functional results were seen in all patients (mean age, 31.1 years)
in the monostotic group in the last follow-up (mean, 20.1
months).
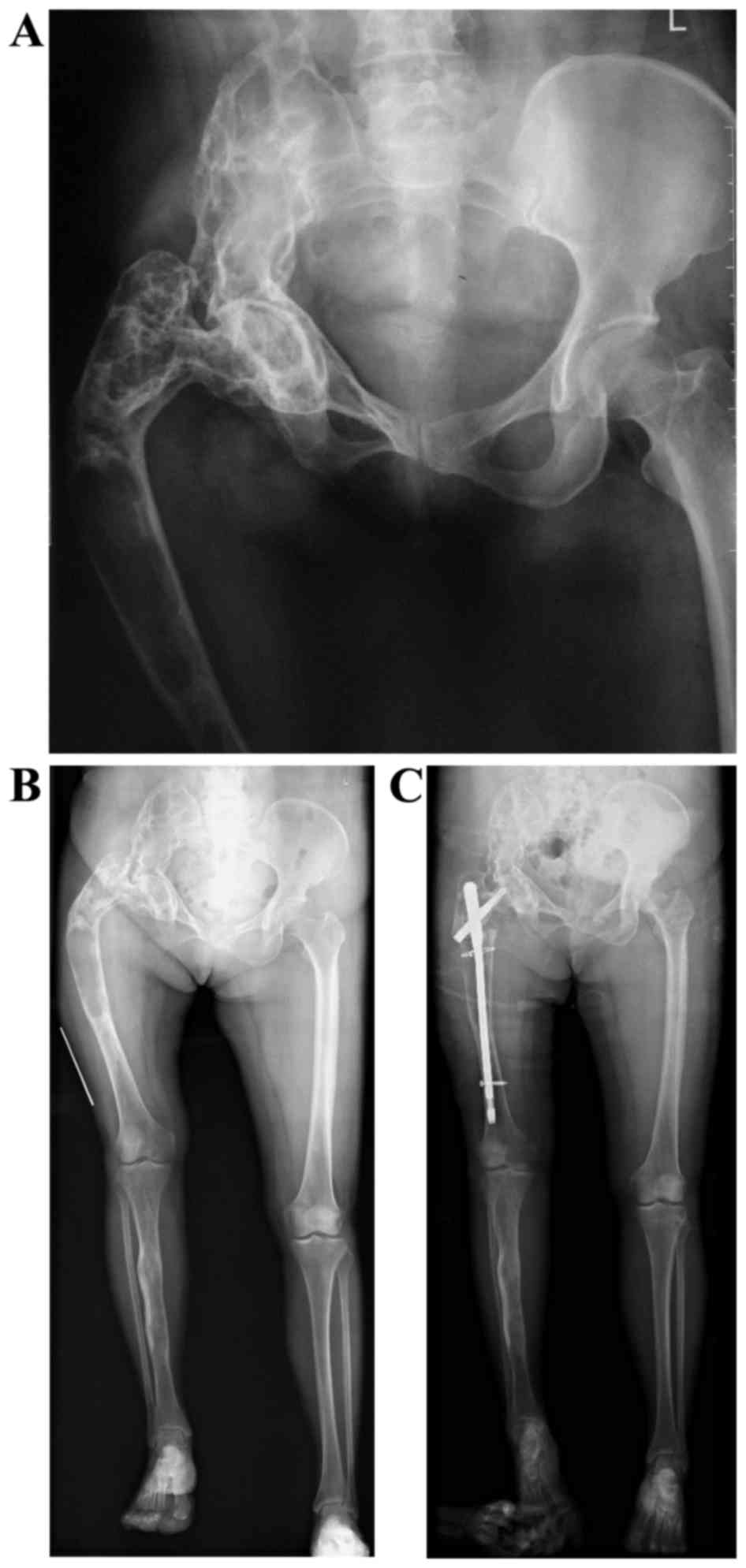
Polyostotic group
There were eight patients with a total of ten
lesions undergone surgery in the polyostotic group. Three patients
of two femurs and one tibia lesion had pain and severe deformities,
one of them had pathological fracture.
Curettage and bone grafting with allograft of fibula
or PFNA/IM nail was applied in six lesions with pain or
pathological fracture. Case 22 had two significant lesions of
proximal femur and tibia. Curettage, bone grafting and PFNA were
performed on the femur lesion to relieve symptoms and prevent
pathological fracture and deformity. As for tibia lesion, surgery
of curettage and allograft without internal fixations was performed
at four years after the first surgery due to progression and
aggravating pain. Satisfactory outcome acquired during the last
follow-up. In case 20, complication of spiral blade cutting out of
the femoral head occurred at 6-month after the surgery of
curettage, bone grafting and PFNA. And revision surgery of an
allograft fibula implanted to replace the spiral blade was
performed. But the radiographic and functional results were
unsatisfactory at 16-month follow-up.
Three patients with deformity of lower limbs were
treated with osteotomy, curettage, bone grafting and
PFNA/intramedullary nail (One typical case was showed in Fig. 2). The patient No. 17 with extreme
thin cortices of tibia were managed with intramedullary nail alone
to prevent pathological fracture and progression.
All patients in the polyostotic group were followed
up for averagely 34.6 (15.9–58.6) months. The average age at the
time of surgery was 23.6 (15–48) years. Except for Case 20, all
(7/8) patients had satisfactory functional and radiologic results.
There were no infection, recurrent fracture or progression of
deformity.
Discussion
Fibrous dysplasia is an abnormal development of bone
with multiple involvement and manifestations. There are no clear
guidelines established for surgical treatment of the dysplastic
lesions. In the present study, by retrospectively analyzing 22
patients with fibrous dysplasia and reviewing of the literatures
(11,17,18), we
deduce that patient age, biological activity, location and size of
the lesion are vital factors in surgical management options making
and surgical outcomes expected.
Patient age is significant since monostotic lesions
usually lose the potentiality to develop and become quiescent or
biological inactive after skeletal maturity. While, polyostic
lesions may continue to progress even in adulthood (4,12,19),
which indicates MFD may have a better prognosis than PFD. In our
study, the mean age in the MFD group at operation was 30.1 (16–45)
years as compared to 20.1 (15–40) years in the PFD group. All
patients with MFD showed satisfactory outcome after surgery while
one in seven patient from PFD group suffered hardware failure and
unsatisfactory outcome, which is similar to the study by Döhler
et al (20). He reported at
least three in four (the rest was lost during followup) monostotic
patients (mean age 40 years, range 22–61 years) had a satisfactory
outcome while two in seven polyostic patients (three in ten
lesions, mean age 6.9 years, range 2–14 years) had a poor results
postoperatively.
Harris et al (9) reported five in ten patients (ages:
Unspecified) with a femoral neck lesion had a poor result after
simple curettage and bone grafting (one with internal fixation).
But in our study four patients (ages: 16, 31, 45, 45 years) who had
ilium involvement and underwent simple curettage and autograft had
a satisfactory outcome and there were no recurrence noted upon the
last followup. Stephenson et al (11) reported nine in ten skeletally mature
patients (ages, ≥18 years) with upper extremity lesion had a
satisfactory outcome after curettage and bone grafting. We deduce
that younger patient age and femoral lesion (of high mechanical
forces) suggests relatively poorer prognosis treated with simple
curettage and bone grafting, which concurs with the study by
DiCaprio et al (7) that
symptoms in active lesions are unlikely to be relieved with simple
curettage and nonstructural bone grafting. For skeletally mature
adults with MFD, curettage and bone grafting may be indicated
(12). According to a recent
multivariate analysis, polyostotic form may be the only risk factor
of poor outcome (1). For young
patients with PFD, bone grafts usually fail to incorporate and then
are replaced by dysplastic lesions eventually, which suggests the
significance of restoring the mechanical axes and reinforcing the
bone with feasible internal fixations (21).
Underlying bone fragility in FD is common.
Non-weight-bearing management for fractures will exacerbate the
preexisting weakness of bone. Internal fixation allowing early
weight-bearing should be considered when fracture occurs,
especially in lower extremities. For lesions in the proximal femur,
especially subtrochanteric fractures, intramedullary nailing is a
reliable fixation choice (13,22,23). By
purchasing firmly into the femoral head, intramedullary nailing
could stabilize the femur and prevent refractures and loss of neck
shaft angle (24,25). Typical plate and screw devices are
not recommended (26). However, in
our study satisfactory outcome were noted in all nine patients
treated with DHS or plate and screws (six femurs and two humeri in
MFD group, one distal fibula in PFD group). We presume that plate
and screws should be used cautiously in selected lesions with
sufficient normal cortical bone or on low-weight-bearing sites like
fibula.
The bones especially the outer cortex are very thin,
weak and easily deformed in PFD. It would become much thornier to
manage, once fracture occurs upon deformity. In our study, Patient
No.20 treated with curettage, graft and PFNA had complication and
unsatisfactory outcome postoperatively which may related to minimal
residual bone stock of femoral head and neck. The early prevention
of bony deformities with corrective osteotomies and internal
fixation is underlined in the literatures (10,11,19) and
allograft, known as having the least and slowest replacement by the
host bones (7), may be the key to
prevent recurrence and disease progression.
Limitation of the current study: We would have
preferred to have a longer follow-up and more cases.
In conclusion, the management for monostotic
patients mostly depends on symptoms. Surgical management for MFD is
indicated in case of nonclassic presentation, potential mechanical
deficit leading to pain or fracture. MFD usually ends with
satisfactory outcome even with simple curettage and bone grafting
in selected patients. For patients with PFD, apart from the
measures above, osteotomy with PFNA or IM can correct bony
deformity, prevent recurrent fracture, and restore alignment, thus
improve functioning of limbs.
Acknowledgements
We thank Dr Yong Zhou and Dr Yi Luo (Department of
Orthopedics, West China Hospital, Sichuan University, Chengdu,
China) for the language assistance regarding this study
Funding
No funding was received.
Availability of data and material
The datasets used and analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
XF and HL analyzed and interpreted the patient data
regarding the fibrous dysplasia disease and wrote the article. YL
collected and analyzed the clinical data. HD and YX performed the
surgeries and designed the structures of the manuscript. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
This study was conducted in accordance with the
Declaration of Helsinki and with approval from the Ethics Committee
of West China Hospital (Chengdu, China). Written informed consent
was obtained from all participants or their guardians.
Consent for publication
Written informed consent was obtained from all
participants or their guardians.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Benhamou J, Gensburger D, Messiaen C and
Chapurlat R: Prognostic factors from an epidemiologic evaluation of
fibrous dysplasia of bone in a modern cohort: The FRANCEDYS study.
J Bone Miner Res. 31:2167–2172. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Riminucci M, Robey PG, Saggio I and Bianco
P: Skeletal progenitors and the GNAS gene: Fibrous dysplasia of
bone read through stem cells. J Mol Endocrinol. 45:355–364. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bianco P, Kuznetsov SA, Riminucci M,
Fisher LW, Spiegel AM and Robey PG: Reproduction of human fibrous
dysplasia of bone in immunocompromised mice by transplanted mosaics
of normal and Gsalpha-mutated skeletal progenitor cells. J Clin
Invest. 101:1737–1744. 1998. View
Article : Google Scholar : PubMed/NCBI
|
|
4
|
Campanacci M: Bone and soft tissue tumors:
Clinical features, imaging, pathology and treatment. Springer; New
York; 1999, View Article : Google Scholar
|
|
5
|
Zhang X, Shang X, Wang Y, He R and Shi G:
Intramedullary nailing for fibrous dysplasia of lower limbs. Oncol
Lett. 4:524–528. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Amit M, Collins MT, FitzGibbon EJ, Butman
JA, Fliss DM and Gil Z: Surgery versus watchful waiting in patients
with craniofacial fibrous dysplasia-a meta-analysis. PLoS One.
6:e251792011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
DiCaprio MR and Enneking WF: Fibrous
dysplasia. Pathophysiology, evaluation, and treatment. J Bone Joint
Surg Am. 87:1848–1864. 2005. View Article : Google Scholar
|
|
8
|
Satoh K, Mitsukawa N and Abe T: Is
prophylactic decompression of the optic canal necessary in surgical
correction of fronto-orbital fibrous dysplasia?: A review of 11
consecutive case. J Craniomaxillofac Surg. 42:1614–1616. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Harris WH, Dudley HR Jr and Barry RJ: The
natural history of fibrous dysplasia. An orthopaedic, pathological,
and roentgenographic study. J Bone Joint Surg Am. 44-A:207–233.
1962. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Guille JT, Kumar SJ and MacEwen GD:
Fibrous dysplasia of the proximal part of the femur. Long-term
results of curettage and bone-grafting and mechanical realignment.
J Bone Joint Surg Am. 80:648–658. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Stephenson RB, London MD, Hankin FM and
Kaufer H: Fibrous dysplasia. An analysis of options for treatment.
J Bone Joint Surg Am. 69:400–409. 1987.
|
|
12
|
Enneking WF and Gearen PF: Fibrous
dysplasia of the femoral neck. Treatment by cortical bone-grafting.
J Bone Joint Surg Am. 68:1415–1422. 1986. View Article : Google Scholar
|
|
13
|
Freeman BH, Bray EW III and Meyer LC:
Multiple osteotomies with Zickel nail fixation for polyostotic
fibrous dysplasia involving the proximal part of the femur. J Bone
Joint Surg Am. 69:691–698. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hagiwara Y, Iwata S, Yonemoto T and Ishii
T: Rotational valgus osteotomy for shepherd's crook deformity: A
case report. J Orthop Sci. 20:422–424. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Li L, Hou X, Li Q and Zhang L: En bloc
resection and bone graft: Does it alter the natural history of
monostotic expansile fibrous dysplasia in children? World J Surg
Oncol. 12:3492014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Enneking WF, Dunham W, Gebhardt MC,
Malawar M and Pritchard DJ: A system for the functional evaluation
of reconstructive procedures after surgical treatment of tumors of
the musculoskeletal system. Clin Orthop Relat Res. 286:241–246.
1993.
|
|
17
|
Fitzpatrick KA, Taljanovic MS, Speer DP,
Graham AR, Jacobson JA, Barnes GR and Hunter TB: Imaging findings
of fibrous dysplasia with histopathologic and intraoperative
correlation. AJR Am J Roentgenol. 182:1389–1398. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhibin Y, Quanyong L, Libo C, Jun Z,
Hankui L, Jifang Z and Ruisen Z: The role of radionuclide bone
scintigraphy in fibrous dysplasia of bone. Clin Nucl Med.
29:177–180. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Andrisano A, Soncini G, Calderoni PP and
Stilli S: Critical review of infantile fibrous dysplasia: Surgical
treatment. J Pediatr Orthop. 11:478–481. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Döhler JR and Hughes SP: Fibrous dysplasia
of bone and the Weil-Albright syndrome. A study of thirteen cases
with special reference to the orthopaedic treatment. Int Orthop.
10:53–62. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Leet AI, Boyce AM, Ibrahim KA, Wientroub
S, Kushner H and Collins MT: Bone-grafting in polyostotic fibrous
dysplasia. J Bone Joint Surg Am. 98:211–219. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ippolito E, Bray EW, Corsi A, de Maio F,
Exner UG, Robey PG, Grill F, Lala R, Massobrio M, Pinggera O, et
al: Natural history and treatment of fibrous dysplasia of bone: A
multicenter clinicopathologic study promoted by the European
Pediatric Orthopaedic Society. J Pediatr Orthop B. 12:155–177.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Stanton RP: Surgery for fibrous dysplasia.
J Bone Miner Res. 21(Suppl 2): P105–P109. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Jung ST, Chung JY, Seo HY, Bae BH and Lim
KY: Multiple osteotomies and intramedullary nailing with neck
cross-pinning for shepherd's crook deformity in polyostotic fibrous
dysplasia: 7 femurs with a minimum of 2 years follow-up. Acta
Orthop. 77:469–473. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Nishida Y, Tsukushi S, Hosono K, Nakashima
H, Yamada Y, Urakawa H and Ishiguro N: Surgical treatment for
fibrous dysplasia of femoral neck with mild but prolonged symptoms:
A case series. J Orthop Surg Res. 10:632015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
O'Sullivan M and Zacharin M:
Intramedullary rodding and bisphosphonate treatment of polyostotic
fibrous dysplasia associated with the McCune-Albright syndrome. J
Pediatr Orthop. 22:255–260. 2002. View Article : Google Scholar : PubMed/NCBI
|