Introduction
Schwannomas are mostly benign tumors. They are often
seen in the head, neck and extremities. Studies have shown that
only 0.7 to 2.6% of schwannomas are found in the retroperitoneum.
Those in pararenal space are even rarer. Although most schwannomas
are <5 cm in diameter, retroperitoneal schwannomas are able to
grow into a large size in such a non-restrictive space (1). They are mostly asymptomatic until they
grow too large to cause compression, which is usually ambiguous
pain. In the present study we introduce a case of a 35-year-old
female with a giant posterior pararenal schwannoma. To the best of
our knowledge, this is the first time to report a posterior
pararenal schwannoma in such a large size.
Materials and methods
The surgical specimen were fixed in 10% formalin at
room temperature overnight and embedded in paraffin. Later, the
specimen were cut into four-micrometer-thick sections. Before
staining, the sections were dewaxed in xylene, rehydrated through
decreasing concentrations of ethanol, and washed in PBS. After
that, the sections were stained with hematoxylin at 37°C for 15
min, rinsed under running water for 1 min and then left standing in
water for 5min. Similarly, Staining with 0.5% eosin was executed
for at 37°C for 3 min, followed by rinsing under running water.
After staining, sections were dehydrated through increasing
concentrations of ethanol and xylene. Rehydration was performed by
continuous immersion in xylene, graded concentrations of ethanol,
and tap water. Slides were kept in citrate buffer (pH 9.0) and two
cycles of heat retrieval were performed in oven at 99°C for ten and
five minutes.
Slides were washed in Tris buffer (pH 7.8). To
blocking endogenous peroxidase, all sections were incubated with
hydrogen peroxide for 10 min. Next, sections were washed thrice in
Tris buffer, followed by 30 min incubation with primary antibodies.
Primary antibodies used were S100 protein (cat. no. PIPA516257;
rabbit polyclonal antibody, dilution 1:300), CD34 (cat. no.
PIMA516924; mouse monoclonal antibody; QBend/10; dilution 1:100),
SMA (cat. no. PIMA511547; mouse monoclonal antibody; clone 1A4;
dilution 1:200), and Ki-67 (mouse monoclonal antibody; clone 4A1)
(all from Invitrogen, Waltham, MA, USA). Secondary antibody
including goat anti-mouse IgG (cat. no. PIA32723; dilution 1:500)
and goat anti-rabbit IgG (cat. no. A11034; dilution 1:500) (both
from Invitrogen) was added correspondingly after washing with Tris
buffer for 40 min. At last, chromogen diaminobenzidine (DAB) was
added for 10 min, followed by counterstaining with hematoxylin for
2 min, sequential immersions in xylene and alcohol and mounting
with distyrene plastisizer xylene (DPX). The results were observed
under light microscope.
Case report
A 35-year-old female was admitted to Peking
University Shenzhen Hospital (Shenzen, China) with an incidental
finding of a left retroperitoneal mass 1 month earlier. Except for
dull pain in left waist, no other symptoms showed up. On physical
examination, a large, firm, smooth, non-tender mass was palpable.
Ultrasound examination revealed a predominant solid mass measuring
109 × 89 × 86 mm between the left kidney and spleen, with multiple
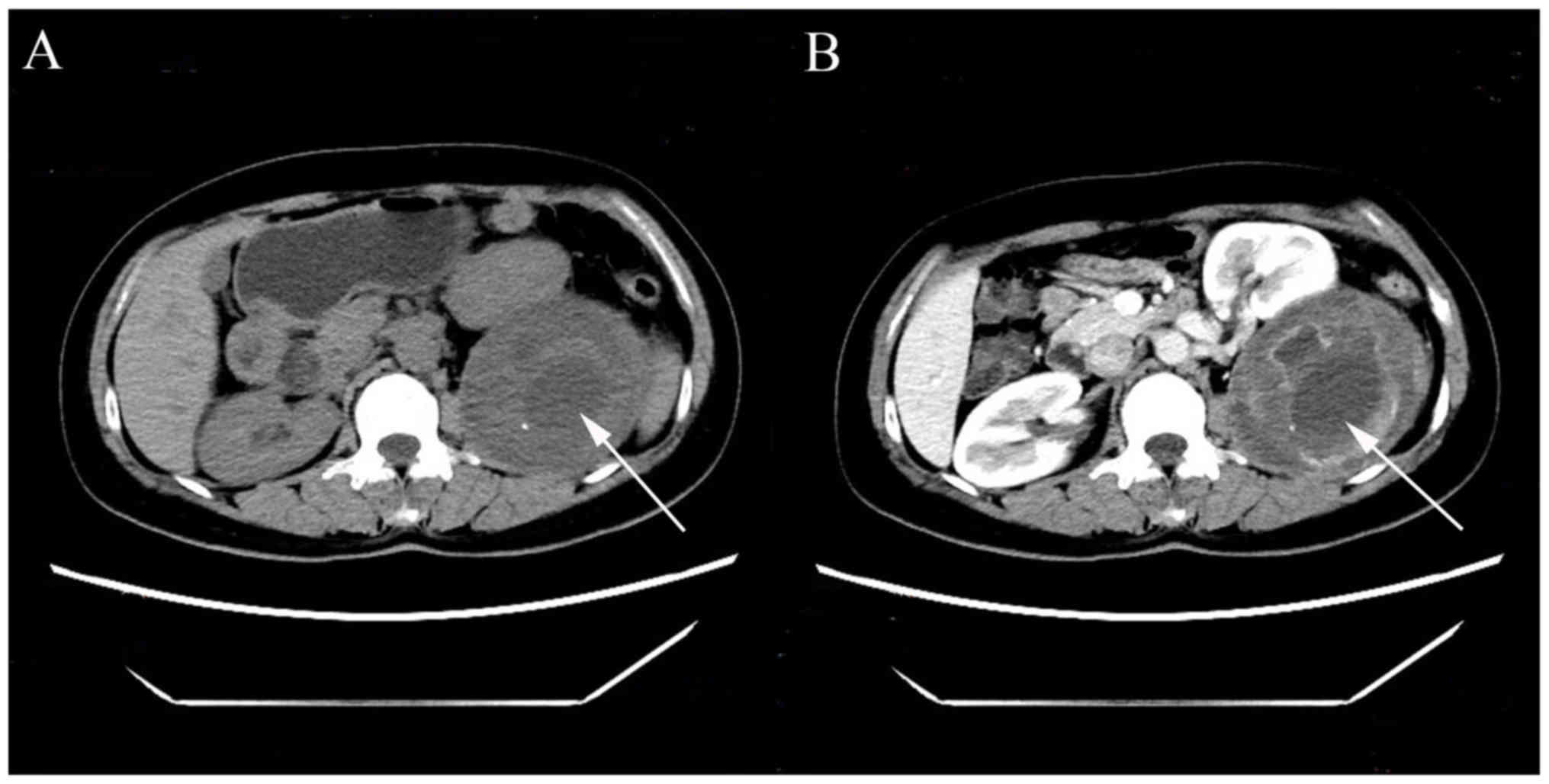
oval dark areas. Small amount of blood flow could be seen. CT scan
revealed a giant cystic solid mass with mixed density in the left
posterior pararenal space, adhering with pancreas, spleen, kidney
and psoas major muscle. The left kidney was pushed to inferior with
vascular circuity. The lesion was predominantly low density, 13–48
HU, well-demarcated, smooth with capsule, and measured 89 × 81 ×
104 mm with punctiform calcification inside it. On enhanced CT,
apparent heterogeneous contrast enhancement could be seen inside
the mass. The left kidney and adrenal gland had a normal morphology
and uniform density, showing no abnormality on enhanced CT. No
swollen lymph nodes were found (Fig.
1). According to the results above, adrenal neoplasms needed to
be distinguished, including pheochromocytoma, cortical adenoma, and
aldosteronoma. The blood pressure of the patient was in normal
range. Later hematologic examination showed that the secretion of
ACTH and cortisol (at OMN, 8 a.m. and 4 p. m.) had a normal
circadian rhythm and was within normal range. Catecholamine,
methoxy adrenalin, quantitative test of 24 h VMA (vanilmandelic
acid) were within normal limits. Angiotensin, renin, ALD
(aldosterone) in blood showed no abnormalities in both erect
position and clinostatism. Basically, adrenal neoplasms could be
ruled out. However, a preoperative diagnosis was still
challenging.
Later, the patient underwent surgery.
Intraoperatively, a cystic solid oval mass was found behind the
kidney in the left retroperitoneum, with obvious adhesion with
adjacent tissue. No obvious change in blood pressure of the patient
was seen when touching the mass. The mass has an intact capsule and
a complete resection was executed.
Gross examination showed a solid mass measuring 13 ×
8.5 × 6.5 cm, with cystic degeneration (4.0 cm in diameter). It was
wrapped with an intact smooth capsule (Fig. 2). On microscopy the mass was composed
of spindle cells, with regions of high and low cellularity (Antoni
A and B areas, respectively). Hemorrhagic and cystic degeneration
could be seen in central area (Fig.
3).
Immonohistochemical staining revealed positivity for
S100 and negative for CD34 and SMA. The Ki-67 proliferation index
was about 10%. Based on these, a diagnosis of schwannoma was
suggested. During the follow-up, there was no evidence of
recurrence.
Discussion
Schwannomas, arising from Schwann cells of
peripheral nerve sheaths, are mostly benign tumors. They are often
found in the head, neck and extremities in the 4th and 6th decades
of life (2) Studies have shown that
only 0.7–2.6% of schwannomas are found in the retroperitoneum.
Generally, schwannomas are less than 5cm in diameter. But
retroperitoneum is a non-restrictive space which allows the tumors
to reach a large size over a long time of growth (1). According to our search on Pubmed, we
found out about 30 cases on giant retroperitoneal schwannoma. Yet,
there have never reported a posterior pararenal schwannoma larger
than 10cm in diameter.
According to a literature published by G. Lannaci in
2016, twenty-one cases of primary renal schwannoma have been
reported in literature (3).
Schwannomas originating in the pararenal space are extremely rare.
To date, only a few cases have been reported. Miyagi T reported a
posterior pararenal schwannoma with a diameter of 3.0 × 2.5 cm in
1986 (4). In 2010, a patient
suffering from Neurofibromatosis Type 2 found a schwannoma
posterior and inferior to the left kidney, measuring 9.5 × 4 × 4 cm
(5). In 2013, Liu et al
mentioned eight patients with retroperitoneal schwannomas in the
anterior pararenal space (6). Here
in, we show a giant posterior pararenal schwannoma measuring 13 ×
8.5 × 6.5 cm, which we believe to be the biggest one that has been
reported in this location by far. This is the first time to report
a pararenal schwannoma with a size more than 10 cm in diameter.
Schwannomas are mostly well-demarcated round or oval
masses on CT and MRI. Cystic and hemorrhagic degeneration can be
seen in large retroperitoneal schwannomas, which appear as
inhomogeneous low-density masses and homogeneous to heterogeneous
contrast enhancement on enhanced CT. MRI images can reminder the
origin and the exact location of the mass. The intensity of the
masses can help with the inference of their properties. However,
these changes are non-specific. We are not able to make a final
diagnosis through these radiographic results.
Blood biochemical examination is conducive to
exclude adrenal neoplasms. The high concentration of certain
hormones in blood can reveal the existence of functional adenoma.
However, for non-functional adenoma, the hormones in blood could be
normal, which means that blood biochemical examination only plays a
limited role in diagnosis. Fine-needle aspiration biopsy is a way
to get the pathological diagnosis of retroperitoneal masses. Yet it
is suffered from controversy due to its low accuracy and potential
complications. Still, preoperative diagnosis is challenging and a
surgical removal is required for diagnosis.
For retroperitoneal masses larger than 4 cm,
especially those with clinical symptoms, surgical removal is
regarded as the most rational way, with the benefit of both
diagnosis and therapy. An incomplete excision may increase 5–10% of
local recurrence (7). Moreover the
possibility of malignancy is considerable. Therefore, a complete
excision is necessary.
To make a final diagnosis, we need to combine
pathology and immunohistochemistry. Histologically, there are two
growth patterns in schwannomas. The Antony A pattern is
characterized by a cell-rich structure with cell nuclei running
parallel to each other while the Antony B pattern has a loose
distribution of the cells with varying degrees of myxoid and
hyaline degeneration. Immunohistochemically, S100 is an important
marker for the diagnosis of schwannomas (8).
The prognosis of retroperitoneal schwannomas are
mostly good. The most common complication is recurrence, possibly
caused by incomplete excision. Malignant schwannomas has poor
prognosis and a high rate of recurrence though the malignant
transformation of retroperitoneal schwannomas appears to be
extremely rare (9).
In the present study, we introduced a giant
posterior pararenal schwannoma which was believed to be the largest
one reported in this location by far. There is a dilemma on the
preoperative diagnosis of pararenal schwannoma. It's important to
include schwannomas during the differentiation of pararenal masses,
especially for those with cystic and hemorrhagic degeneration since
the treatment and prognosis among them may differ a lot.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Natural Science Foundation of China (grant no. 81101922), Science
and Technology Development Fund Project of Shenzhen (grant nos.
JCYJ20160429090753103 and JCYJ20170307111334308), Clinical Research
Project of Shenzhen Health Commission (no. SZLY2018023), the fund
of ‘San-ming’ Project of Medicine in Shenzhen (grant no.
SZSM201612066), the Fund of Shenzhen Key Laboratory (grant no.
ZDSYS201504301045406) and the fund of Guangdong Key Medical
Subject.
Availability of data and materials
The datasets used during the current study are
available from the corresponding author on reasonable request.
Authors' contributions
XP and ZL performed data collection, interpretation
and drafted the manuscript. LiaZ and LiwZ contributed to the study
design and acquisition of data. XW, YY, SY and YC participated in
the study design, data collection, analysis of data and follow-up
of the patient. YL contributed to the study design, and the
analysis and interpretation of data.
Ethics approval and consent to
participate
Written informed consent to participate was obtained
from the patient.
Patient consent for publication
Consent for publication of any associated data and
accompanying images was obtained from the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Karaköse O, Pülat H, Oğuz S, Zihni İ,
Özçelik KÇ, Yalta TD and Eken H: A giant ancient schwannoma
mimicking an adnexal mass: Case report. Medicine (Baltimore).
95:e42402016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Baten E, Lerut J and Kempeneers I: Hybrid
open/closed resection procedure for ancient retroperitoneal
Schwannoma: Case report and review of the literature. Acta Chir
Belg. 116:289–292. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Iannaci G, Crispino M, Cifarelli P,
Montella M, Panarese I, Ronchi A, Russo R, Tremiterra G, Luise R
and Sapere P: Epithelioid angiosarcoma arising in schwannoma of the
kidney: Report of the first case and review of the literature.
World J Surg Oncol. 14:292016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Miyagi T, Shimamura M, Rin SY and
Matsubara F: Retroperitoneal schwannoma: A report of two cases and
review of the literature. Hinyokika Kiyo. 32:207–214.
1986.PubMed/NCBI
|
|
5
|
Patrinou A, Malindretos P, Koutroubas G,
Anagnostou N, Argiraki E and Syrganis C: A rare retroperitoneal
schwannoma in a patient with neurofibromatosis Type 2. NDT Plus.
3:288–290. 2010.PubMed/NCBI
|
|
6
|
Liu QY, Lin XF, Zhang WD, Li HG and Gao M:
Retroperitoneal schwannomas in the anterior pararenal space:
Dynamic enhanced multi-slice CT and MR findings. Abdom Imaging.
38:201–210. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lee NJ, Hruban RH and Fishman EK:
Abdominal schwannomas: Review of imaging findings and pathology.
Abdom Radiol (NY). 42:1864–1870. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Herden J, Drebber U, Ural Y, Zimmer S,
Wille S and Engelmann UH: Retroperitoneal schwannomas of renal and
pararenal origin: Presentation of two case reports. Rare Tumors.
7:56162015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Xu H, Sha N, Li HW, Bai M, Chen X, Hu HL
and Wu CL: A giant pelvic malignant schwannoma: A case report and
literature review. Int J Clin Exp Pathol. 8:15363–15368.
2015.PubMed/NCBI
|