Introduction
Stroke is one of the most common causes of adult
disability, and is considered to be the second leading cause of
mortality worldwide. The incidence of stroke has increased
markedly, particularly in developing countries, over the past four
decades (1). Ischemic stroke,
which accounts for 70–80% of stroke cases, is a major factor that
threatens human life and health (2). Cerebral ischemia, which is induced by
a transient or permanent reduction of blood supply, results in
disordered homeostasis, including insufficient oxygen and delivery
of glucose (3). Cerebral
ischemia-reperfusion (I/R) induces serious brain injuries, and is
associated with complex underlying mechanisms, including
peri-infarct depolarization, oxidative and nitrative stress,
excitotoxicity, inflammation and apoptosis, ultimately resulting in
cell death (4), mitochondrial
dysfunction, release of glutamate and proinflammatory mediators,
production of reactive oxygen species (ROS), and/or lipid
peroxidation (5). Due to the
complex pathological processes of cerebral ischemia, current
treatments have not exhibited the expected effects. Therefore,
natural products extracted from herbs have received increasing
interest with regards to the treatment of cerebral stroke (6).
Gastrodin (GAS; structure presented in Fig. 1) is a natural phenol compound
extracted from Gastrodia elata BI (7). GAS has been suggested for the
treatment of various ailments, including convulsive illness,
headache, vertigo, general paralysis, epilepsy and tetanus
(8). GAS is able to pass the
blood-brain barrier, and rapidly metabolizes to p-hydroxybenzyl
alcohol in the brain, liver and blood (9). It has previously been reported that
GAS ameliorates cerebral damage following transient focal cerebral
ischemia (10). The potential
underlying mechanisms have been identified in in vivo
models, by determination of ROS and hippocampal neuronal death
assessment, and in vitro models, by assessment of
excitotoxicity and neuroprotective effects (10,11).
Furthermore, it has been reported that GAS decreases the volume of
cerebral infarction and ameliorates cerebral injury in a rat model
of I/R, probably by improving the level of amino acids in the
striatum (12). In addition, GAS
significantly attenuates the levels of neurotoxic proinflammatory
mediators and proinflammatory cytokines by inhibiting the nuclear
factor-κB signaling pathway and phosphorylation of
mitogen-activated protein kinases (MAPKs) in
lipopolysaccharide-stimulated microglial cells (13). GAS also ameliorates Parkinson's
disease by downregulating connexin 43 (14), and improves anxiety-like behaviors
by decreasing the levels of interleukin (IL)-1β and inhibiting p38
MAPK phosphorylation in the hippocampus of a rat model of
post-traumatic stress disorder (15). These findings indicated that GAS
may exert beneficial effects on diseases of the central nervous
system. However, the effects and underlying mechanisms of GAS on
subacute phase cerebral I/R injury remain unknown.
The present study investigated the neuroprotective
effects of GAS on a rat model of subacute phase focal cerebral I/R
injury, and explored the possible underlying mechanisms with
regards to neuroinflammation and neuronal apoptotic pathways.
Materials and methods
Chemicals
GAS (purity >98% tested using high-performance
liquid chromatography) was purchased from Nanjing Zelang Medical
Technology Co., Ltd. (Nanjing, China). Nimodipine (Nim) was
obtained from Shandong Lukang Pharmaceutical Group Saite Co., Ltd.
(Tai'an, China). 2,3,5-Triphenyltetrazolium chloride (TTC) was
purchased from Sigma-Aldrich (St. Louis, MO, USA).
Animals
Male Sprague-Dawley rats (age, 9 weeks; weight,
250–280 g) were purchased from the Animal Center of the Third
Military Medical University [Chongqing, China; Certificate no. SCXK
(Jun) 2007-00005]. All animals were caged individually under a 12-h
light/dark cycle at 22–24°C with free access to food and water. All
procedures complied with the Current Guide for the Care and Use of
Laboratory Animals and the study was approved by the Zunyi Medical
University Animal Studies Committee (Zunyi, China). All rats were
randomly divided into 6 groups: Sham, I/R, I/R+15 mg/kg GAS, I/R+
30 mg/kg GAS, I/R+60 mg/kg GAS, and I/R+12 mg/kg Nim
(n=20/group).
Focal cerebral I/R surgery
The rats were pretreated with GAS for 7 days
followed by I/R surgery, and were then treated with GAS for another
7 days following I/R surgery. Nim was used as a positive control.
Following pretreatment with GAS or Nim for 7 days, the rats were
anesthetized with chloral hydrate (Sinopharm Chemical Reagent Co.,
Ltd., Shanghai, China) via intraperitoneal injection (350 mg/kg).
The right common carotid artery, internal carotid artery (ICA), and
external carotid artery (ECA) were then exposed through a midline
incision in the neck, and a monofilament nylon suture (external
diameter, 0.28 mm) with a silicone-coated tip was plugged into the
ICA, 16–18 mm from the bifurcation, through the ECA stump, and was
gently advanced to cause middle cerebral artery occlusion (MCAO). A
total of 2 h after MCAO, the suture was removed to restore blood
flow. The sham group underwent the same operation without MCAO.
Evaluation of neurological
deficits
Neurological deficits of the experimental animals
were graded on a scale of 0–4 on days 1, 3 and 7 post-cerebral I/R
injury (16). The criteria were
set as follows: 0, no neurological deficits; 1, failure to fully
extend right forepaw; 2, forelimb flexion plus decreased resistance
to lateral push; 3, falling to the right; 4, unable to walk
spontaneously and exhibited depressed levels of consciousness. Rats
in model and treated groups with a score between 2 and 3 were
selected for the present study.
Measurement of infarct volume
A total of 7 days after reperfusion the rats were
sacrificed following appropriate intraperitoneal anesthetization
with 350 mg/kg chloral hydrate (Sinopharm Chemical Reagent Co.,
Ltd.). Brains were removed, immediately frozen in liquid nitrogen,
and dissected into 2–3 mm slices. Subsequently, samples were placed
in 0.1% TTC solution for 10 min at 37°C in the dark. The red-purple
sections were assigned as noninfarcted areas, whereas white
sections were assigned as infarcted areas. The percentage of
infarction was calculated as follows: Percentage of infarction (%)
= (weight of white sections / weight of whole brain) × 100%.
Hematoxylin and eosin (HE)
staining
Rats were sacrificed (n=5/group) 7 days after
reperfusion, and brains were fixed by transcardial perfusion using
0.9% normal saline and 4% paraformaldehyde. Post-fixation, the
tissues were incubated in 4% paraformaldehyde for 24 h at 4°C.
Following dehydration in graded xylene and ethanol, the sections
were embedded in paraffin. Embedded brain tissue sections were
coronally sliced into 4 µm sections, and sections including the
hippocampus were analyzed. The sections were then stained with 0.5%
hematoxylin for 5 min, followed by 0.5% eosin for 1 min at room
temperature. The slices were observed under a light microscope
(Leica Microsystems Ltd., Wetzlar, Germany). The hippocampal CA1
region was selected to check for morphological alterations and to
assess cerebral injury.
Terminal deoxynucleotidyl transferase
dUTP nick end labeling (TUNEL) assay
A TUNEL assay was used to evaluate
apoptosis-associated DNA fragmentation using an In Situ Cell
Death Detection kit (Roche Molecular Biochemicals, Mannheim,
Germany). Following dehydration and rehydration in graded xylene
and ethanol, tissue sections were incubated with proteinase K (20
µg/ml) and Tris-HCl (pH 7.4–8.0; 10 mM) for 15 min at room
temperature. The sections were rinsed twice with phosphate-buffered
saline (PBS), and were incubated with TUNEL reaction mixture for 1
h at 37°C. Subsequently, the sections were rinsed with PBS (3×5 min
washes) and incubated with Converter-POD solution for 30 min at
37°C. After further rinsing with PBS (3×5 min washes), the sections
were incubated with diaminobenzidine substrate for 10 min. Images
of the ischemic penumbra, including the cortex and hippocampal CA1
region, were captured in each section under a light microscope. The
density of stained cells was observed under high magnification
(×400). Data were presented as cells per square millimeter.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Brain samples were collected from the ischemic
hemisphere of rats at day 7 post-reperfusion (n=5), following
treatment with various doses of GAS. The gene expression levels of
IL-1β, cyclooxygenase-2 (COX-2) and inducible nitric oxide synthase
(iNOS) were detected in the ischemic penumbra using RT-qPCR.
Briefly, the penumbra of ischemic tissue from the right cortex was
homogenized. Total RNA was extracted from the ischemic penumbra
using TRIzol® reagent (Invitrogen; Thermo Fisher
Scientific, Inc., Waltham, MA, USA) followed by chloroform-phenol
purification, and was quantified at 280 nm. RNA quality was
determined by measuring the ultraviolet absorption ratios at
280/260 nm. The RNA concentration of each sample was adjusted to 50
ng/µl. Purified total RNA was used to prepare cDNA using a RT kit
(Takara Biotechnology Co., Ltd., Dalian, China) with MMLV reverse
transcriptase and Oligo-(dT) primers. Subsequently, specific
regions of target genes were amplified using SYBR Premix Ex Taq
(Takara Biotechnology Co., Ltd.) and specific primers (Table I). The reaction volume of PCR was
15 µl containing 7.5 µl SYBR super mix, 0.5 µl of 10 µmol/µl
Primers 1/2, 3 µl of 5 ng/µl cDNA and 4 µl of 0.1% DEPC water. The
cycling conditions were 1 cycle of 95°C 10 min; 95°C for 10 sec,
60°C for 1 min for 40 cycles; 95°C for 1 min, 55°C for 1 min, and
55°C for 10 sec for 80 cycles. The quantification cycle values (Cq)
were used to determine gene expression levels (17). Gene expression levels of
glyceraldehyde 3-phosphate dehydrogenase were used as an internal
control. Each group was normalized to the sham group, which was set
at 100%.
 | Table I.Sequence of primers. |
Table I.
Sequence of primers.
| Gene | Forward primer
(5′-3′) | Reverse primer
(5′-3′) |
|---|
| iNOS |
AAGCACATTTGCCAATGGAGAC |
TGGAGCCCAGGCCAAATAC |
| COX-2 |
AACACGGACTTGCTCACTTTGTTG |
AATGGAGGCCTTTGCCACTG |
| IL-1β |
GCTGTGGCAGCTACCTATGTCTTG |
AGGTCGTCATCATCCCACGAG |
| GAPDH |
TAACCAGGCGTCCBATACG |
CAGTGCCAGCCTCGTCTCA |
Western blot analysis
A total of 7 days post-reperfusion, the rats were
anesthetized using choral hydrate. The brains were then removed and
coronally sectioned from −24.3 to +1.7 mm of the bregma, and the
right penumbra of ischemic cortex (as the right common carotid
artery had been occluded in rats) was separated, weighed and
homogenized in cytosolic extraction buffer. Protein was extracted
using RIPA lysis buffer (Beyotime Institute of Biotechnology,
Nanjing, China) lysis buffer containing 1% Nonidet P-40, 0.5%
sodium deoxycholate, 0.1% sodium dodecyl sulfate, 1 µg/ml aprotinin
and 100 µg/ml phenylmethylsulfonyl fluoride. Protein concentration
was determined using a Bio-Rad Protein Assay kit (cat. no. 5000002;
Bio-Rad Laboratories, Inc., Hercules, CA, USA). Total proteins were
diluted in 4X loading buffer and were incubated at 100°C for 5 min.
Samples (80 µg) were then loaded onto a loading gel and separated
on a Bis-Tris gel (12% gel for IL-1β and cleaved caspase-3; 10% gel
for COX-2; and 8% gel for iNOS). Separated proteins were
transferred onto a nitrocellulose membrane at 200 mA for 2 h.
Nonspecific sites were blocked for 1 h at room temperature in
fat-free milk solution [10% in 0.1% Tween-Tris-buffered saline
(TTBS)]. Membranes were then incubated overnight at 4°C with the
following rabbit polyclonal antibodies: Anti-IL-1β (cat. no.
ab9787; 1:1,000; Abcam, Cambridge, UK), anti-COX-2 (cat. no.
ab52237 1:1,000; Abcam), anti-iNOS (cat. no. ab3523; 1:1,000;
Abcam), anti-cleaved caspase-3 (cat. no. ab2302; 1:1,000; Abcam)
and anti-β-actin (cat. no. AF0003; 1:1,000; Beyotime Institute of
Biotechnology), in 5% bovine serum albumin TTBS solution. The
secondary antibodies (horseradish peroxidase-conjugated goat
anti-rabbit IgG (cat. no. A0208) and goat anti-mouse (cat. no.
A0216), (Beyotime Institute of Biotechnology) used were diluted to
1:1,000 and incubated for 1 h at room temperature. Subsequently,
the membranes were developed using the enhanced chemiluminescence
(ECL) reagent Beyo ECL plus (Beyotime Institute of Biotechnology).
Images of the blots were captured using a ChemiDoc XRS system
(Bio-Rad Laboratories, Inc.). The image was scanned and band
intensity was semi-quantified using Quantity One software v4.52
(Bio-Rad Laboratories, Inc.).
Statistical analysis
Data are presented as the mean ± standard error of
the mean. Statistical significance was determined using one-way
analysis of variance followed by Dunnett's multiple comparisons
post-hoc test using SPSS 13.0 software (SPSS, Inc., Chicago, IL,
USA). P<0.05 was considered to indicate a statistically
significant difference.
Results
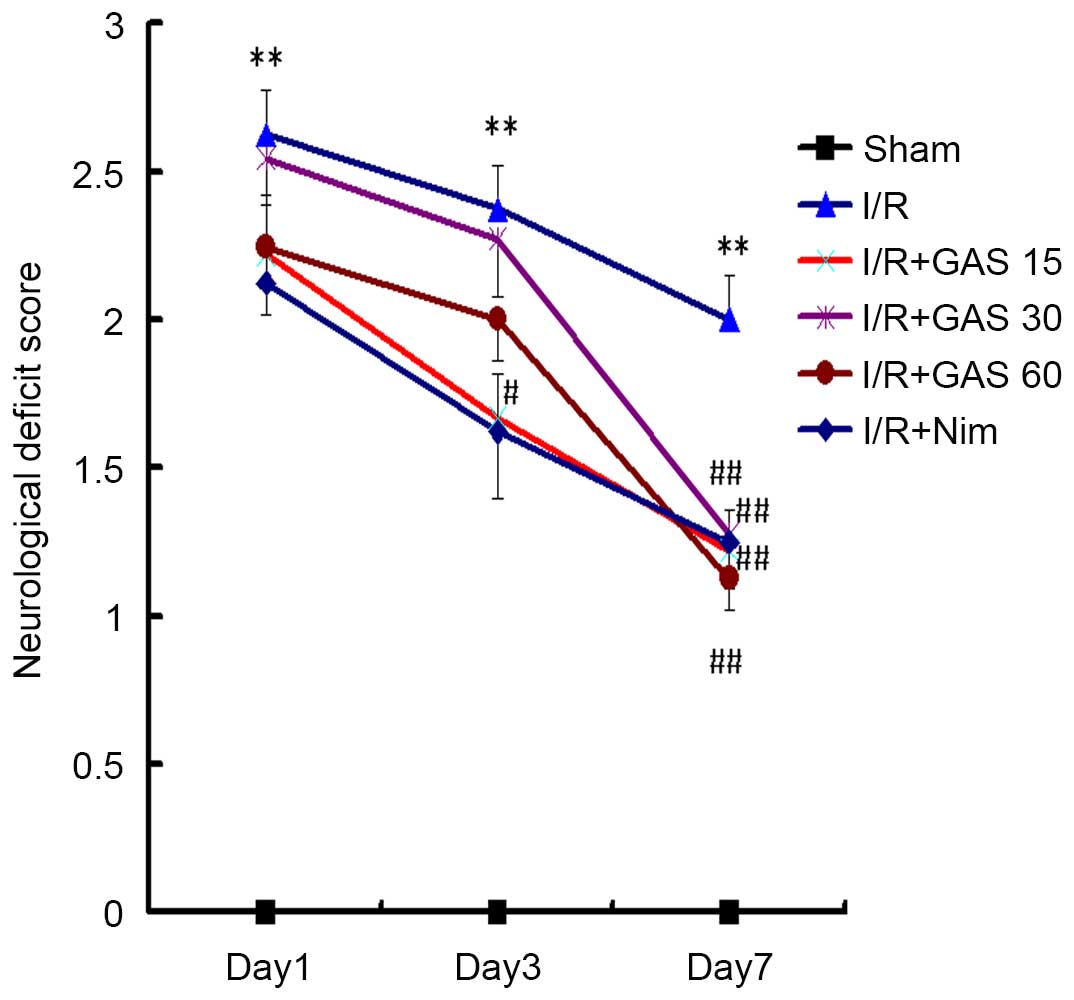
Effects of GAS on neurological
deficits in a rat model of cerebral I/R injury
To investigate the effects of GAS on neurological
deficits in a rat model of cerebral I/R injury, a behavioral test
was performed. Bederson's score was used as a criterion to evaluate
neurological deficits. All sham rats obtained a score of 0,
indicating no neurological deficits (Fig. 2). The rats that underwent the right
side cerebral I/R surgery exhibited paresis of the left paws. In
the model group, the neurological deficit scores were 2.63±0.48,
2.37±0.48 and 2±0.50 on days 1, 3 and 7, respectively. Compared
with the model group, the positive control group exhibited improved
neurological function, with significantly decreased scores on day 3
(1.63±0.74; P<0.05), and day 7 (1.25±0.46; P<0.01). In the
GAS treatment groups, the scores on day 7 at all three doses
exhibited significant differences compared with the I/R model
group.
Effects of GAS on brain infarct volume
in a rat model of subacute phase cerebral I/R injury
In addition to neurological deficit scores, the
protective effects of GAS were evaluated with regards to brain
infarct volume. No infarcted areas were observed in the sham group
(Fig. 3). Conversely, obvious
infarcted areas were observed in the model group. The positive
control group (Nim) exhibited a significantly smaller infarct
volume compared with the model group, and all three doses of GAS
exerted a similar effect to the positive control.
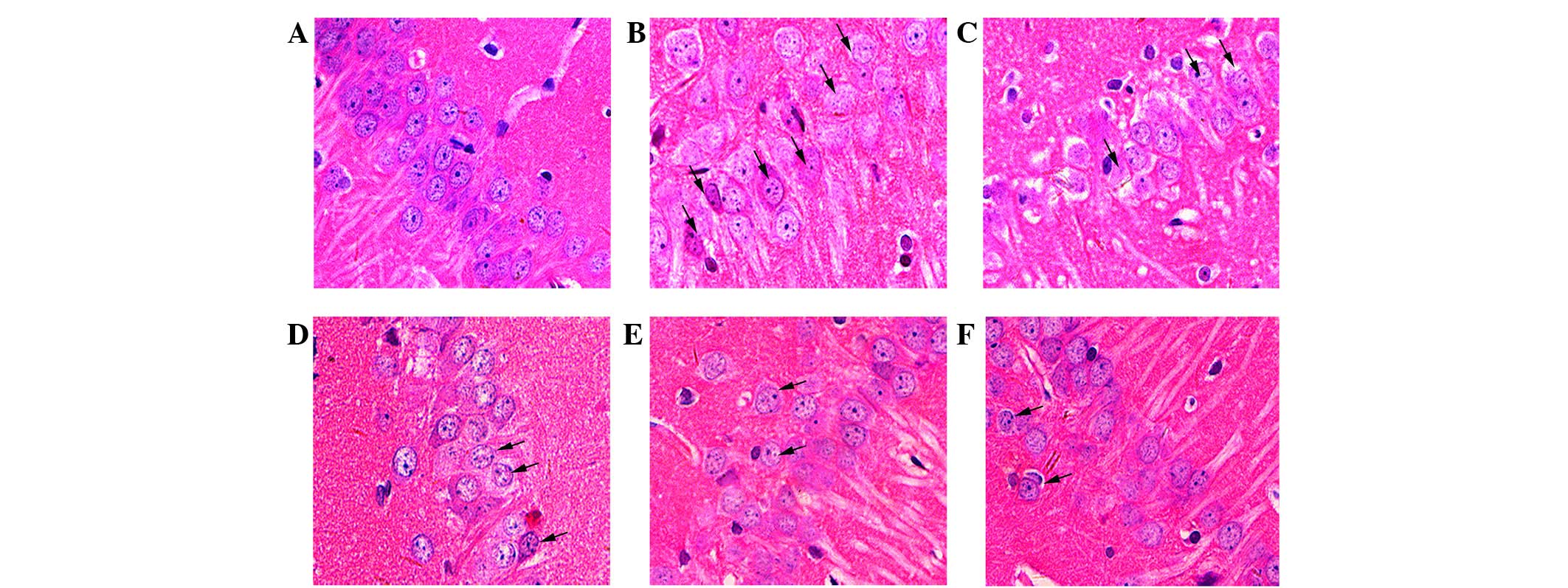
GAS attenuates pathological damage in
the hippocampus of the ischemic penumbra
The rat hippocampal CA1 region was observed
following HE staining (Fig. 4).
Compared with normal neurons in the sham group (Fig. 4A), severe cellular edema, condensed
nuclei and nuclear loss were observed in the model group (Fig. 4B). Damaged neurons in the model
group exhibited pyknosis and anachromasis of the nucleus, as well
as shrunken cell bodies in the hippocampal CA1 region. Nim slightly
decreased the damage (Fig. 4C),
whereas GAS markedly inhibited cellular edema and nuclear loss in
the hippocampal CA1 region (Fig.
4D-F).
GAS suppresses apoptosis in ischemic
hippocampal and cortical penumbra
A TUNEL assay was used to examine fragmented DNA in
the hippocampus and cortex in order to determine the potential
anti-apoptotic effects of GAS (Figs.
5 and 6). Microscopic
inspection of the hippocampal and cortical sections from sham rats
revealed morphologically normal neurons with almost no TUNEL
staining (Figs. 5A and 6A). A total of 1 week post-reperfusion,
the number of TUNEL-positive pyramidal neurons with various degrees
of DNA fragmentation was detected in the hippocampal CA1 region and
the cerebral cortex of ischemic penumbra (Figs. 5B and 6B). Treatment with Nim and GAS
significantly reduced the number of TUNEL-positive neurons
(P<0.01; Figs. 5 and 6).
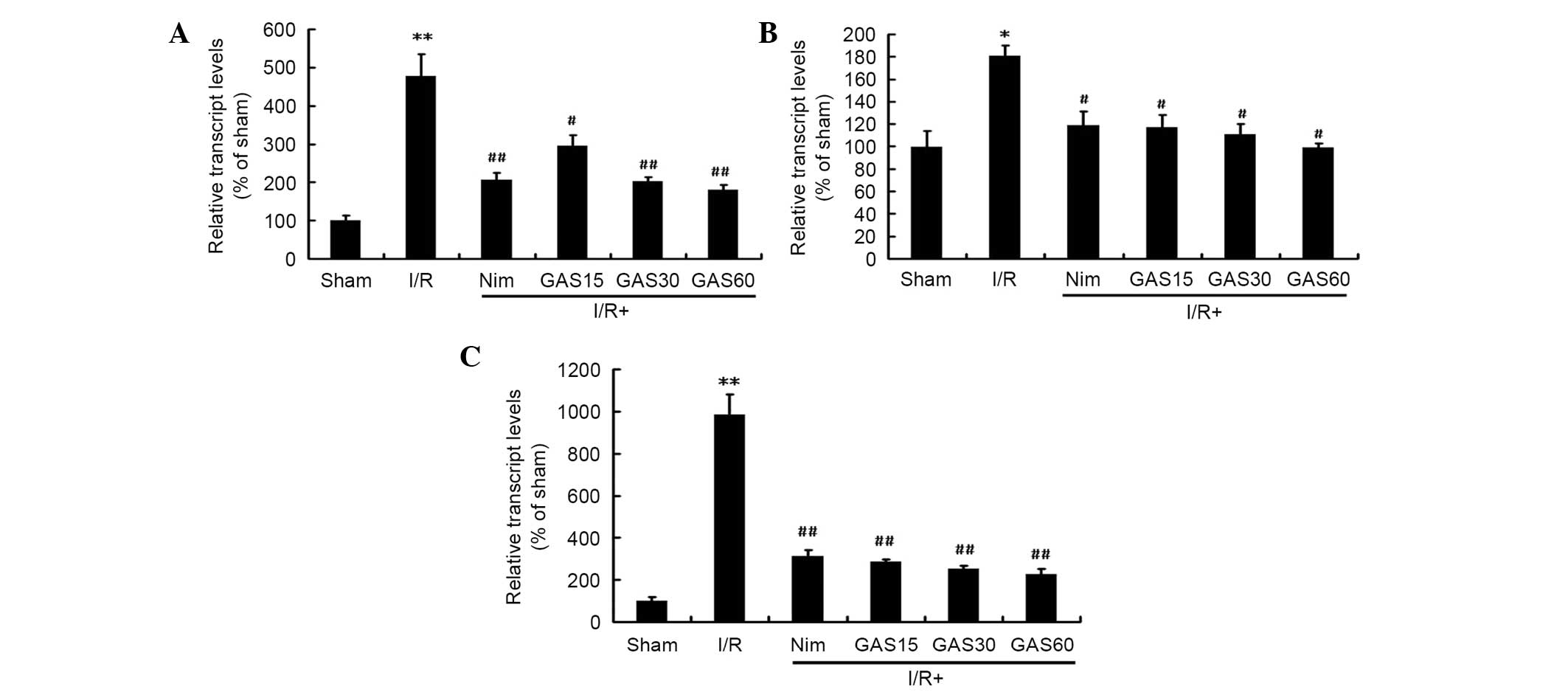
Effects of GAS on the mRNA expression
levels of IL-1β, COX-2 and iNOS in the ischemic penumbra
Due to the important roles of IL-1β, COX-2 and iNOS
on cerebral I/R-induced injury, the effects of GAS on the
regulation of these genes was investigated. RT-qPCR revealed that
all three genes were significantly increased in the model group
compared with in the sham group (Fig.
7). However, treatment with Nim or GAS significantly reduced
the gene expression levels of IL-1β, COX-2 and iNOS compared with
in the model group.
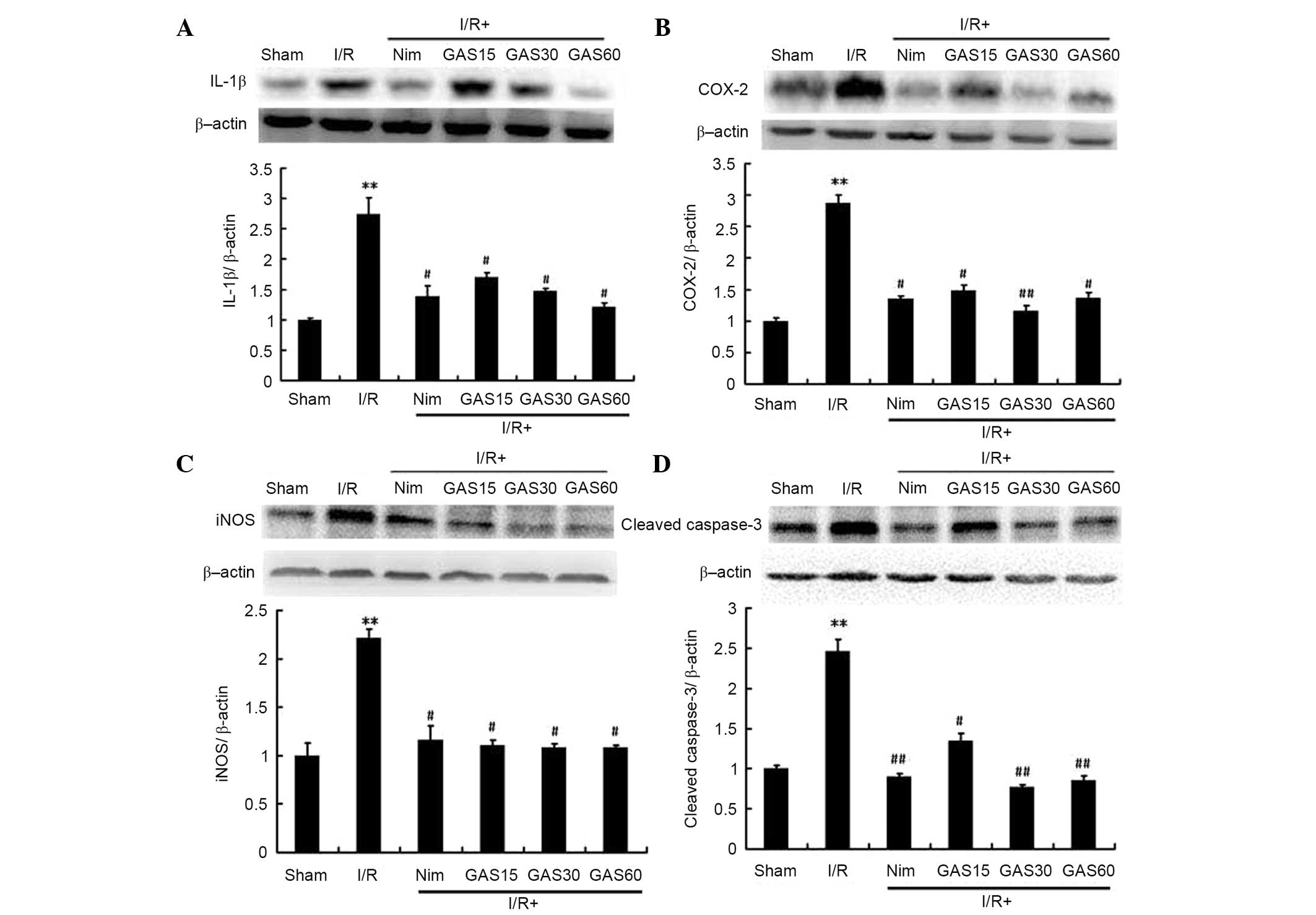
Effects of GAS on the protein
expression levels of IL-1β, COX-2, iNOS and cleaved caspase-3 in
the ischemic penumbra
In addition to the gene expression levels, the
protein expression levels of IL-1β, COX-2 and iNOS were determined
using western blotting. To confirm the possible role of apoptosis
in GAS-induced improvement, the levels of cleaved caspase-3 were
also detected. The protein expression levels of IL-1β, COX-2, iNOS
and cleaved caspase-3 were significantly higher in the model group
compared with in the sham group. As expected, GAS exhibited similar
effects to the positive compound Nim; both of which downregulated
the expression levels of the aforementioned proteins compared with
in the model group (P<0.05; Fig.
8).
Discussion
MCAO-induced focal cerebral I/R injury is the most
frequently used animal model of stroke (18,19).
The present study investigated the effects of GAS on I/R injury 7
days after reperfusion; I/R injury was induced by 2 h MCAO and Nim
was used as a positive control. Nim is a dihydropyridine calcium
channel blocker, which has been investigated for its therapeutic
application in various cerebrovascular trials, including ischemic
stroke and cerebral resuscitation (20). Nim has been reported to improve
cerebral metabolism in patients with severe head trauma (21), and it has also been shown to exert
beneficial effects in the reduction of infarct size in stroke
(22). Furthermore, post-ischemic
administration of Nim following focal cerebral I/R injury in rats
has been reported to alleviate excitotoxicity, neurobehavioral
alterations and bioenergetics (23). Similar to Nim, the present study
demonstrated that pretreatment with GAS for 7 days followed by I/R
surgery, and treatment with GAS for 7 days after I/R surgery
significantly attenuated I/R-induced disability and histological
damage, alleviated neuronal apoptosis, and reduced the mRNA and
protein expression levels of inflammatory and proapoptotic factors,
including IL-1β, COX-2, iNOS and cleaved caspase-3.
Although various mechanisms are associated with the
pathogenesis of stroke, increasing evidence has demonstrated that
inflammatory responses partly account for its pathogenic
progression (24). During the
subacute phase of ischemic brain injury, 1–7 days after the onset
of ischemia, inflammation exacerbates delayed infarct expansion and
has a key pathological role in ischemic injury (25). Tissue damage begins with an
inflammatory reaction following the interruption of cerebral blood
flow, and the administration of GAS exhibited potential
neuroprotective effects on MCAO-induced cerebral I/R injury in
rats. These effects are likely due to the inhibition of
inflammation-associated events. The behavioral test used in the
present study was designed to assess impairments consistent with
the known functional architecture of the rat brain, and
inflammatory mediators have previously been identified through
experimental investigations of brain edema (26). In the present study, edema lasted 7
days after MCAO in rats, which was accompanied by an increased
infarct size. In addition, behavioral abnormality, infarct size and
edema were significantly increased in the I/R group compared with
in the sham group. Conversely, in the I/R + GAS groups the
development of behavioral abnormality and infarct size was
significantly suppressed compared with in the I/R model group.
Inflammatory mediators, including IL-1, iNOS and
COX-2, are upregulated following cerebral I/R surgery (27,28).
Elevated expression levels of inflammatory mediators may enhance
neurological damage via the activation of various downstream
pathways (29). A previous study
demonstrated that inhibitors of iNOS attenuate infarct size
following focal cerebral ischemia (30). In addition, cerebral ischemia has
been reported to upregulate the inducible form of COX-2 in the
injured brain (31), and
attenuating microglial activation-induced expression of IL-1β may
provide a neuroprotective effect against transient cerebral
ischemic injury (32). GAS, which
is a compound isolated from the Chinese herb G. elata BI, was able
to significantly ameliorate cerebral I/R surgery-induced infarct
size in the present study. In addition, downregulation of the gene
and protein expression levels of IL-1β, COX-2 and iNOS were
detected in the penumbra of cerebral I/R rats, and may be
considered the potential underlying mechanism by which GAS protects
the brain from stroke-induced symptoms.
The present study also demonstrated that inhibition
of apoptosis was a mechanism by which GAS exerted neuroprotection
against cerebral I/R injury. Mitochondrial and death receptor
pathways are the two main apoptotic pathways. The caspase family
consists of cysteine proteases that induce apoptosis. Among the 12
known caspases in mammals, cleaved caspase-3 is a crucial biomarker
of neuronal apoptosis that also acts as an apoptotic executor
(33). In the present study, in
both the hippocampus and cerebral cortex of the cerebral I/R rats,
GAS significantly attenuated neuronal loss and the number of
TUNEL-positive cells. Therefore, inhibition of apoptosis is
potentially involved in the prevention of neuronal death. In the
present study, with regards to activated caspase-3, cerebral
ischemia increased its protein expression levels, which is
consistent with a previous study that reported elevated caspase-3
gene expression in transient cerebral ischemia (34). Conversely, treatment with GAS
significantly decreased the expression levels of cleaved caspase-3.
These results suggested that the protective effects of GAS may be
associated with the inhibition of apoptotic signaling pathways.
In conclusion, the present study demonstrated that
GAS was able to ameliorate subacute phase cerebral I/R injury, and
its protective effects may be induced by inhibiting IR-induced
upregulation of the inflammatory cytokine IL-1β, by inhibiting the
expression of the pro-oxidative enzymes COX-2 and iNOS in the
ischemic brain, and by inhibiting neuronal apoptosis via
suppression of apoptotic signaling pathways. These findings
suggested that GAS exerts a neuroprotective effect in the ischemic
brain, due to the inhibition of inflammation and apoptosis.
Therefore, GAS may be considered a potential therapeutic agent
against inflammation and apoptosis in subacute phase cerebral I/R
injury.
Acknowledgements
The present study was supported by the Brainstorm
Project on Social Development by Department of Science and
Technology of Guizhou Province (grant no. SY [2008] 3040); the
Program for Changjiang Scholars and Innovative Research Team in
University, China (grant no. IRT1197); the Program for New Century
Excellent Talents in University (grant no. NCET-11-0927); and the
Key Projects of Guizhou Science and Technology Department [grant
no. JZ(2014)2015].
References
|
1
|
Feigin VL, Lawes CM, Bennett DA,
Barker-Collo SL and Parag V: Worldwide stroke incidence and early
case fatality reported in 56 population-based studies: A systematic
review. Lancet Neurol. 8:355–369. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rosamond W, Flegal K, Furie K, Go A,
Greenlund K, Haase N, Hailpern SM, Ho M, Howard V, Kissela B, et
al: Heart disease and stroke statistics-2008 update: A report from
the American heart association statistics committee and stroke
statistics subcommittee. Circulation. 117:e25–e146. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Strosznajder RP, Czubowicz K, Jesko H and
Strosznajder JB: Poly (ADP-ribose) metabolism in brain and its role
in ischemia pathology. Mol Neurobiol. 41:187–196. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gonzalez CL, Gharbawie OA and Kolb B:
Chronic low-dose administration of nicotine facilitates recovery
and synaptic change after focal ischemia in rats.
Neuropharmacology. 50:777–787. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mehta SL, Manhas N and Raghubir R:
Molecular targets in cerebral ischemia for developing novel
therapeutics. Brain Res Rev. 54:34–66. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wu Pf, Zhang Z, Wang F and Chen JG:
Natural compounds from traditional medicinal herbs in the treatment
of cerebral ischemia/reperfusion injury. Acta Pharmacol Sin.
31:1523–1531. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhu H, Dai P, Zhang W, Chen E, Han W, Chen
C and Cui Y: Enzymic synthesis of gastrodin through microbial
transformation and purification of gastrodin biosynthesis enzyme.
Biol Pharm Bull. 33:1680–1684. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kumar H, Kim IS, More SV, Kim BW, Bahk YY
and Choi DK: Gastrodin protects apoptotic dopaminergic neurons in a
toxin-induced Parkinson's disease model. Evid-Based Compl Alt.
2013:5140952013. View Article : Google Scholar
|
|
9
|
Lin LC, Chen YF, Lee WC, Wu YT and Tsai
TH: Pharmacokinetics of gastrodin and its metabolite
p-hydroxybenzyl alcohol in rat blood, brain and bile by
microdialysis coupled to LC-MS/MS. J Pharm Biomed Anal. 48:909–917.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zeng X, Zhang S, Zhang L, Zhang K and
Zheng X: A study of the neuroprotective effect of the phenolic
glucoside gastrodin during cerebral ischemia in vivo and in vitro.
Planta Med. 72:1359–1365. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Xu X, Lu Y and Bie X: Protective effects
of gastrodin on hypoxia-induced toxicity in primary cultures of rat
cortical neurons. Planta Med. 73:650–654. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bie X, Chen Y, Han J, Dai H, Wan H and
Zhao T: Effects of gastrodin on amino acids after cerebral
ischemia-reperfusion injury in rat striatum. Asia Pac J Clin Nutr.
16:305–308. 2007.PubMed/NCBI
|
|
13
|
Dai JN, Zong Y, Zhong LM, Li YM, Zhang W,
Bian LG, Ai QL, Liu YD, Sun J and Lu D: Gastrodin inhibits
expression of inducible NO synthase, cyclooxygenase-2 and
proinflammatory cytokines in cultured LPS-stimulated microglia via
MAPK pathways. PloS One. 6:e218912011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wang Y, Wu Z, Liu X and Fu Q: Gastrodin
ameliorates Parkinson's disease by downregulating connexin 43. Mol
Med Rep. 8:585–590. 2013.PubMed/NCBI
|
|
15
|
Peng Z, Wang H, Zhang R, Chen Y, Xue F,
Nie H, Chen Y, Wu D, Wang Y, Wang H and Tan Q: Gastrodin
ameliorates anxiety-like behaviors and inhibits IL-1beta level and
p38 MAPK phosphorylation of hippocampus in the rat model of
posttraumatic stress disorder. Physiol Res. 62:537–545.
2013.PubMed/NCBI
|
|
16
|
Bederson JB, Pitts LH, Tsuji M, Nishimura
MC, Davis RL and Bartkowski H: Rat middle cerebral artery
occlusion: Evaluation of the model and development of a neurologic
examination. Stroke. 17:472–476. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) Method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hoffman GE, Merchenthaler I and Zup SL:
Neuroprotection by ovarian hormones in animal models of
neurological disease. Endocrine. 29:217–231. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Boyko M, Zlotnik A, Gruenbaum BF,
Gruenbaum SE, Ohayon S, Goldsmith T, Kotz R, Leibowitz A, Sheiner
E, Shapira Y and Teichberg VI: An experimental model of focal
ischemia using an internal carotid artery approach. J Neurosci
Methods. 193:246–253. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kakarieka A, Schakel E and Fritze J:
Clinical experiences with nimodipine in cerebral ischemia. J Neural
Trans Suppl. 43:13–21. 1994.
|
|
21
|
Aslan A, Gurelik M, Cemek M, Goksel HM and
Buyukokuroglu ME: Nimodipine can improve cerebral metabolism and
outcome in patients with severe head trauma. Pharmacol Res.
59:120–124. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Fogelholm R, Erilä T, Palomäki H, Murros K
and Kaste M: Effect of nimodipine on final infarct volume after
acute ischemic stroke. Cerebrovasc Dis. 10:189–193. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Babu CS and Ramanathan M: Post-ischemic
administration of nimodipine following focal cerebral
ischemic-reperfusion injury in rats alleviated excitotoxicity,
neurobehavioural alterations and partially the bioenergetics. Int J
Dev Neurosci. 29:93–105. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Muir KW, Tyrrell P, Sattar N and Warburton
E: Inflammation and ischaemic stroke. Curr Opin Neurol. 20:334–342.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ye YL, Shi WZ, Zhang WP, Wang ML, Zhou Y,
Fang SH, Liu LY, Zhang Q, Yu YP and Wei EQ: Cilostazol, a
phosphodiesterase 3 inhibitor, protects mice against acute and late
ischemic brain injuries. Eur J Pharmacol. 557:23–31. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Simard JM, Kent TA, Chen M, Tarasov KV and
Gerzanich V: Brain oedema in focal ischaemia: Molecular
pathophysiology and theoretical implications. Lancet Neurol.
6:258–268. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Jin R, Yang G and Li G: Inflammatory
mechanisms in ischemic stroke: Role of inflammatory cells. J Leukoc
Biol. 87:779–789. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Li F, Gong Q, Wang L and Shi J: Osthole
attenuates focal inflammatory reaction following permanent middle
cerebral artery occlusion in rats. Biol Pharm Bull. 35:1686–1690.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Maddahi A and Edvinsson L: Cerebral
ischemia induces microvascular pro-inflammatory cytokine expression
via the MEK/ERK pathway. J Neuroinflammation. 7:142010. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Jiang MH, Kaku T, Hada J and Hayashi Y:
7-Nitroindazole reduces nitric oxide concentration in rat
hippocampus after transient forebrain ischemia. Eur J Pharmacol.
380:117–121. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Iadecola C, Forster C, Nogawa S, Clark HB
and Ross ME: Cyclooxygenase-2 immunoreactivity in the human brain
following cerebral ischemia. Acta Neuropathol. 98:9–14. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Lujia Y, Xin L, Shiquan W, Yu C, Shuzhuo Z
and Hong Z: Ceftriaxone pretreatment protects rats against cerebral
ischemic injury by attenuating microglial activation-induced IL-1β
expression. Int J Neurosci. 124:657–665. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Hartmann A, Hunot S, Michel PP, Muriel MP,
Vyas S, Faucheux BA, Mouatt-Prigent A, Turmel H, Srinivasan A,
Ruberg M, et al: Caspase-3: A vulnerability factor and final
effector in apoptotic death of dopaminergic neurons in Parkinson's
disease. P Natl Acad Sci USA. 97:2875–2880. 2000. View Article : Google Scholar
|
|
34
|
Chen J, Nagayama T, Jin K, Stetler RA, Zhu
RL, Graham SH and Simon RP: Induction of caspase-3-like protease
may mediate delayed neuronal death in the hippocampus after
transient cerebral ischemia. J Neurosci. 18:4914–4928.
1998.PubMed/NCBI
|