Introduction
The incidence of nasopharyngeal carcinoma (NPC) has
become decreased during the past decade (1). The characteristics of cervical lymphatic
metastasis in NPC remain to be elucidated (2). NPC has a high propensity of cervical
node metastasis, as lymphatic drainage of the nasopharynx is
predominantly to cervix (2). Patients
with NPC may be asymptomatic even with lymphatic metastasis, and
symptoms of NPC mimic that of thyroid carcinoma. Ultrasound in
isolation is therefore not reliable for selection of thyroid
nodules (3).
Thyroid metastasis from NPC is rare and may be
correctly diagnosed by fine needle aspiration biopsy (4). Differentiated diagnosis is crucial
because therapy regimens are completely different, and simultaneous
modulated radiotherapy plus chemotherapy is feasible and effective
for patients with advanced NPC (5).
Suspicion of multiple primary tumors is essential for patients with
head and neck neoplasms.
Case report
A 52-year-old female was admitted to a local
hospital with a painless mass in the anterior neck for 1 year
without significant clinical manifestations such as pain, increase
in temperature or bleeding. Furthermore, the thyroid function tests
were normal. Neck palpation, ultrasonography and cervical computer
tomography (CT) showed thyroid nodule and bilateral enlarged
cervical lymph nodes, with the largest one approximately 2.0 cm in
diameter (Fig. 1), with a strong
suspicion of thyroid carcinoma. A total thyroidectomy and radical
neck dissection were performed empirically on the basis of the
non-invasive tests. However, the patient suffered from persistent
headache and fever for a week, and was transferred to the Xuzhou
Central Hospital Affiliated to Southeast University (Jiangsu,
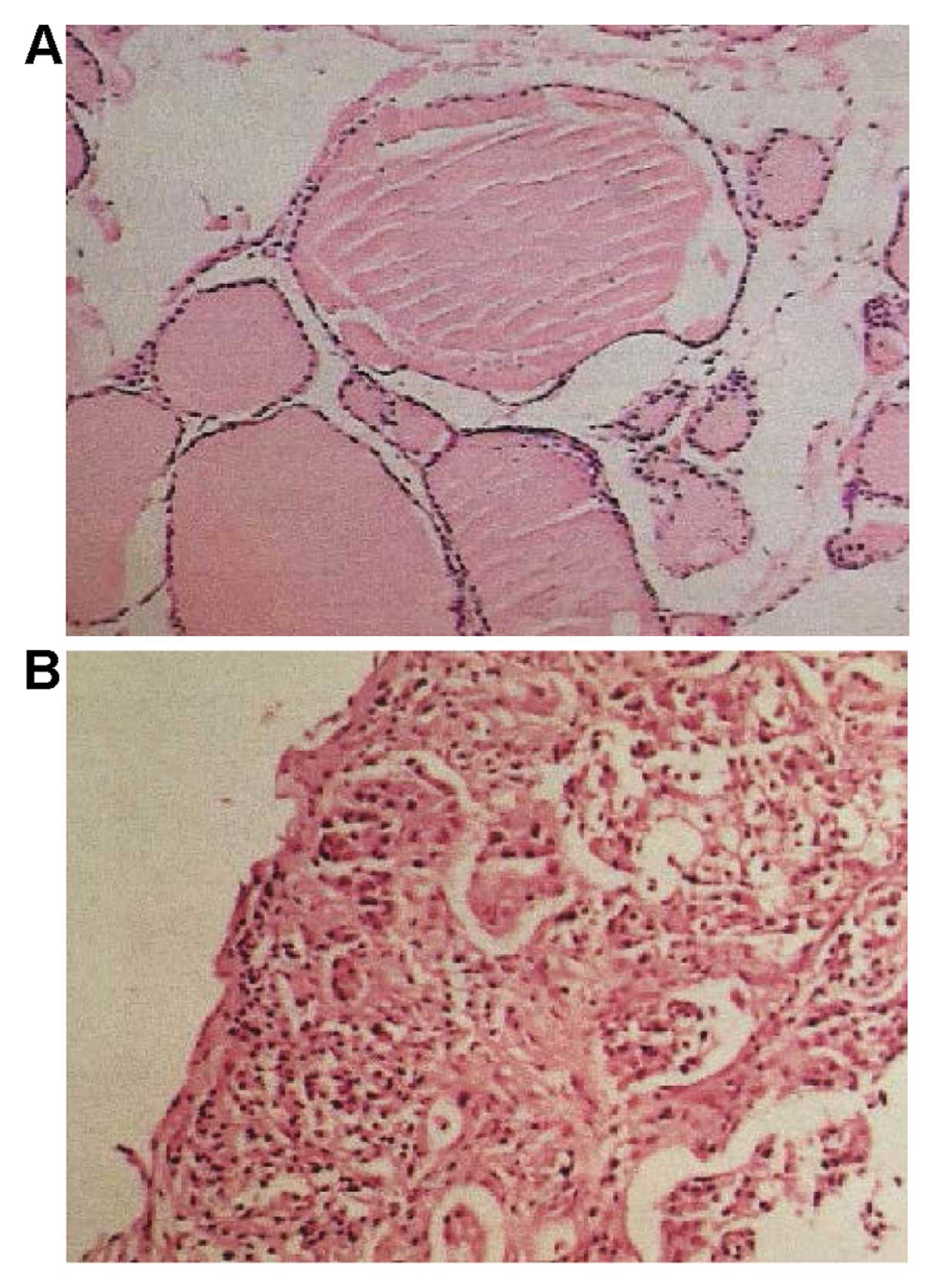
China). Following further diagnostic measures, thyroid adenoma and
NPC were confirmed by postoperative histopathology (Fig. 2), which was indicated by cranial CT
and nasal endoscopic biopsy (Fig. 3).
Subsequently, the patient received palliative radiotherapy and
L-thyroxine substitution therapy with relatively poor quality of
life.
The present study was approved by the Institutional
Review Board of the Xuzhou Central Hospital. Informed consent was
obtained from the patient.
Discussion
Lymph node metastasis of NPC follows an orderly
pattern, and the most commonly involved regions include
retropharyngeal and level II lymph nodes (2). The involvement of cervical and
retropharyngeal lymph nodes constitutes a potentially prognostic
factor for N1 patients with NPC (2010 UICC/AJCC staging system)
(6). Cases of multiple primary
malignancies in the same host are often examined, a lymph node
biopsy is required for diagnosis of NPC. It has been reported that
the most frequent primary malignancies with thyroid metastasis are
renal carcinoma, lung cancer and head and neck neoplasms (7,8). Therefore
recurrence or progression of non-thyroid malignancy must be
considered regardless of time elapsed since the initial diagnosis
(7).
In addition to non-invasive procedures such as whole
body CT or positron emission tomography, CT ultrasound-guided
fine-needle aspiration biopsy of thyroid nodules and lymph nodes,
respectively, may be utilized for a concrete differential diagnosis
of primary or metastatic neoplasms (9). Prior to treating the patient with any
surgical therapy a definite preoperative diagnosis is compulsory.
These practices are useful in the avoidance of unnecessary
extensive thyroidectomy (as in this particular patient) which would
deteriorate the quality of life for patients with NPC. Thus, each
case of patient with thyroid nodules and enlarged cervical lymph
nodes must be carefully evaluated using histopathology or even
immunohistochemistry, and metastatic tumor should be considered in
differential diagnosis to avoid misdiagnosis and mistreatment.
In conclusion, metastatic NPC in cervical lymph
nodes must be considered and biopsy should be performed separately
in the differential diagnosis of thyroid tumors to avoid
misdiagnosis and mistreatment.
Acknowledgements
We appreciate the kind assistance from the staff of
the Department of Pathology of Xuzhou Central Hospital. This study
was supported by the Speciality Fund for Jiangsu Key Laboratory of
Molecular and Translational Cancer Research (no. BM2013007).
References
|
1
|
Chua ML, Wee JT, Hui EP and Chan AT:
Nasopharyngeal carcinoma. Lancet. 387:1012–1024. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ho FC, Tham IW, Earnest A, Lee KM and Lu
JJ: Patterns of regional lymph node metastasis of nasopharyngeal
carcinoma: A meta-analysis of clinical evidence. BMC Cancer.
12:982012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Remonti LR, Kramer CK, Leitão CB, Pinto LC
and Gross JL: Thyroid ultrasound features and risk of carcinoma: A
systematic review and meta-analysis of observational studies.
Thyroid. 25:538–550. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chiumento C, Fiorentino A, Castaldo G and
Fusco V: A case of thyroid metastasis of nasopharyngeal cancer.
Tumori. 97:24e–6e. 2011.PubMed/NCBI
|
|
5
|
Fan TY, Xing J, Lu J, Liu TH, Xu M, Zhang
YJ, Shao Q, Li JB and Yu JM: Phase I/II study of induction
chemotherapy plus concurrent chemotherapy and SMART-IMRT-based
radiotherapy in locoregionally-advanced nasopharyngeal cancer.
Oncol Lett. 5:889–895. 2013.PubMed/NCBI
|
|
6
|
Shi Q, Shen C, Kong L, Wang X, Ding J, Gao
Y, Xu T and Hu C: Involvement of both cervical lymph nodes and
retropharyngeal lymph nodes has prognostic value for N1 patients
with nasopharyngeal carcinoma. Radiat Oncol. 9:72014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chung AY, Tran TB, Brumund KT, Weisman RA
and Bouvet M: Metastases to the thyroid: A review of the literature
from the last decade. Thyroid. 22:258–268. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hegerova L, Griebeler ML, Reynolds JP,
Henry MR and Gharib H: Metastasis to the thyroid gland: report of a
large series from the Mayo Clinic. Am J Clin Oncol. 38:338–342.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yoon JH, Kwak JY, Kim EK, Moon HJ, Kim MJ,
Kim JY, Koo HR and Kim MH: How to approach thyroid nodules with
indeterminate cytology. Ann Surg Oncol. 17:2147–2155. 2010.
View Article : Google Scholar : PubMed/NCBI
|