Pancreatic adenocarcinoma is one of the worlds' most
aggressive malignancies with a five year survival rate of less than
5%, the worst prognosis among all cancers (1). The poor survival rate is mostly due to
the lack of a reliable early detection method, a tendency to
metastasise at an early stage and resistance to available
therapeutic options (2,3). In addition, there is often an absence of
symptoms in early disease and established disease can have clinical
similarities to benign conditions, making it difficult to diagnose
(4). The diagnosis of pancreatic
cancer relies on imaging and tissue biopsy, and the only curative
therapy is complete surgical resection. Non-invasive biomarkers,
such as those from serum, could provide a useful complement to
imaging and cytology diagnostic methods and have the potential to
aid clinical decisions as part of a routine blood test. Currently,
the only clinical biomarker used in the management of pancreatic
cancer is the serum marker CA19-9, which although used widely for
disease monitoring, does not provide adequate accuracy for early
detection and diagnosis. Given the usually late diagnosis of
pancreatic cancer, highly specific circulating biomarkers for
cancer detection and screening are urgently needed, and would be a
major breakthrough allowing treatment for more patients.
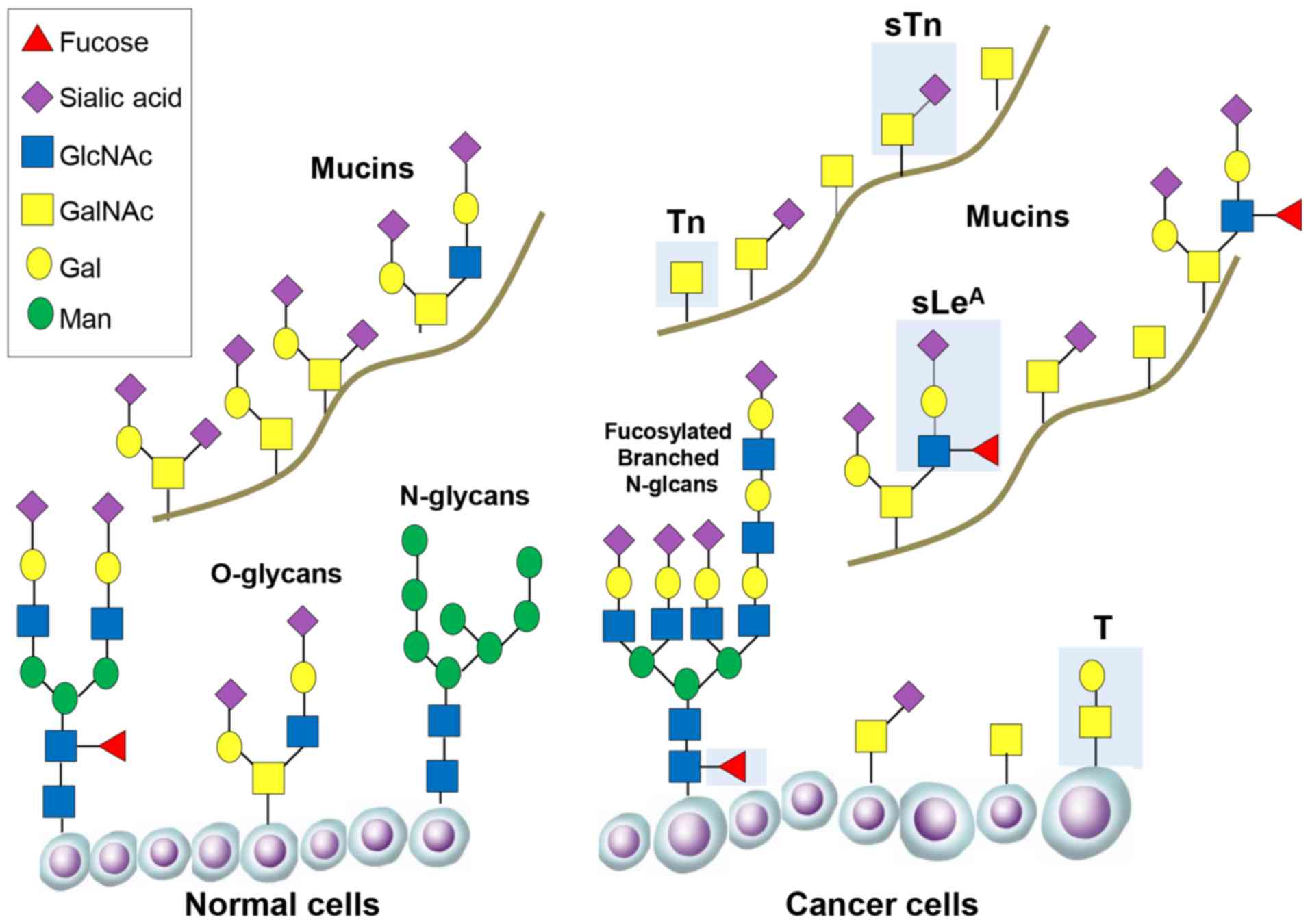
Glycosylation is an enzymatic process that links
glycan sugars to other glyans, lipids or proteins. Glycosylation
takes place in the Golgi apparatus and endoplasmic reticulum and
occurs as the consequence of the synchronised action of
glycosylation enzymes. The two most common mechanisms by which
glycans can be linked to lipids and proteins are O-linked and
N-linked glycosylation. In O-linked glycosylation glycans are added
sequentially to the hydroxyl oxygen of serine/threonine residues on
target proteins and extended to produce various core and terminal
structures that can be sialylated and/or fucosylated. In N-linked
glycosylation 14 sugar preassembled blocks are transferred
co-translationally to the amide group of an asparagine residue.
N-glycans contain a common pentasaccharide core region consisting
of three mannose and two N-acetylglucosamine (GlcNAc) subunits.
This can be further modified by the addition of terminal Gal
(galactose), GlcNAc, fucose and sialic acid moieties.
Glycans can control cell identity and cell
environment interactions. Changes in the glycosylation modification
of proteins that are expressed on the cell surface, or secreted by
cancer cells, are promising sources of potential biomarkers
(9,10). Glycoconjugates with altered
glycosylation are often shed into the circulation, allowing the
distinction between patients with and without cancer (11–13).
Recent research has uncovered new ways that glycosylation can
contribute to cancer biology, as well as new strategies to improve
treatment by exploiting glycans (14). This review discusses the changes in
glycosylation involved in pancreatic cancer, their role in disease
development and progression, and the huge potential to exploit
glycans to improve diagnosis and treatment.
In the normal pancreas glycosylated proteins have
important functions, including protection and lubrication of the
pancreatic ducts (15). In pancreatic
cancer glycosylation of proteins becomes deregulated, and the
aberrant expression of specific glycans is associated with disease
progression and poor prognosis. Changes to the glycome in
pancreatic cancer include increases in the sialyl Lewis antigens
(sLeA and sLex), an increase in truncated
O-glycans (Tn and sTn), increased branched and fucosylated
N-glycans, upregulation of specific proteoglycans and galectins,
and increased O-GlcNAcylation (some of these alterations are
summarised in Fig. 1 and Table I).
The most widely used serological assay used in the
management of pancreatic cancer detects a cancer associated
carbohydrate antigen, called CA 19-9, that contains a glycan known
as sialyl Lewis A (sLeA) (16–20).
sLeA is part of the Lewis family of blood group
antigens, named after the discoverer of a series of antigens found
on red blood cells. Studies have shown that sLeA is
found at low levels in normal tissue, higher levels in embryonic
tissue (21), and is overexpressed in
epithelial cancers (22). In the
normal pancreas sLeA is found on the epithelial surfaces
of the ducts, whereas in pancreatic cancer sLeA can be
heavily secreted into the lumen of proliferating ducts and pass
into the bloodstream (23).
Immature, truncated O-glycans are characteristic of
virtually all epithelial cancer cells (43). In pancreatic cancer, the expression of
the truncated cancer-associated O-glycans Tn and sialyl-Tn (sTn)
are linked to poor patient outcome (11), and associated with cancer cell growth
and metastasis (44,45). The normal pancreas does not express Tn
or sTn (46), but levels are high in
pancreatic cancer (30,45). Specifically, truncated O-glycans have
been detected on Nucleolin, EGFR and Her2 (45,47). COSMC
is a molecular chaperone that is essential for correct protein
O-glycosylation (48). Knockdown of
COSMC promotes aberrant O-glycosylation in pancreatic cancer, and
this is linked to anti-apoptotic and pro-metastatic cell behaviour,
reduced proliferation and increased migration (45). In addition to COSMC, the GALNT3 enzyme
is also linked to the aberrant production of tumor-associated
O-glycans in pancreatic cancer. GALNT3 is increased in
well/moderately differentiated pancreatic cancer, but lost in
poorly differentiated tissues (47,49).
Aberrant N-linked glycosylation is common in
pancreatic cancer. In particular, pancreatic cancer cells
frequently display increased levels of highly branched N-glycans,
and alterations to N-glvcan sialylation or fucosylation. Increased
levels of N-glycosylation has been found on integrins and ECM
adhesion proteins (50) and in
proteins involved in pathways important in pancreatic cancer such
as TGF-β, TNF, and NF-kappa-B signalling (51). N-glycosylation can also influence the
surface expression of receptor tyrosine kinases and enhance the
chemosensitivity of drug resistant pancreatic cancer cells
(52). N-glycans have shown promise
as biomarkers in pancreatic cancer. The sialyltransferase enzymes
ST6Gal1 and ST3Gal3 are overexpressed in pancreatic tissue and this
is linked to invasive potential (53–55). It is
also possible to detect changes to N-glycans in patient blood.
Increased fucosylation can be detected in serum from patients with
pancreatic cancer (56), and highly
branched N-glycans are increased in the blood of patients with
aggressive disease (57,58). Fucosylated epitopes occur on specific
proteins such as haptoglobin and ribonuclease 1 (RNASE1) and these
are currently being explored for use diagnostically (59,60).
The hexosamine biosynthetic pathway (HBP) produces
the amino sugar conjugate O-linked N-acetylglucosamine (O-GlcNAc).
Addition of O-GlcNAc to proteins (known as O-GlcNAcylation) can
alter key hallmarks of cancer including transcription, cell
signalling metabolism and epigenetics (61,62), and
may impact cell survival and resistance during chemotherapy
(63). O-GlcNAc is added to and
removed from proteins by the O-GlcNAc cycling enzymes OGT and OGA.
Both these enzymes are dramatically elevated in pancreatic cancer
relative to normal pancreas, as are the overall levels of protein
O-GlcNAcylation (64). In the normal
pancreas OGT allows cells to dynamically respond to glucose levels
by modulating O-linked protein glycosylation (65). When pancreatic cancer develops
increased O-GlcNAcylation may block cancer cell apoptosis and lead
to oncogenic activation of NF-κB signalling (66). Several proteins with defined roles in
pancreatic cancer have been shown to be modified by O-GlcNAc
including the heat shock protein HSP70 (67), the transcription factor Sp1 (68), the Wnt signalling proteins β-catenin
and LRP6 (69), and more recently the
transcription factor Sox2 that determines self-renewal in
pancreatic cancer and is responsible for tumour initiation
(70). Inhibiting O-GlcNAcylation can
reduce pancreatic tumour growth and progression suggesting HBP is
promising potential therapeutic target (66,71,72).
In addition to aberrant protein glycosylation,
cancer cells can also have alterations in proteoglycans (73). Proteoglycans are heavily glycosylated
glycoproteins with attached glycosaminoglycans (GAGs) such as
chondroitin sulphate and heparin sulphate that are located on the
cell surface or secreted. Numerous proteoglycans have been found to
be overexpressed in pancreatic cancer, including syndecan-1,
versican, decorin, lumican and biglycan (74–81). Of
particular interest, the heparin sulphate proteoglycan glypican-1
is overexpressed in pancreatic cancer cell models and patient
tumours (82) and has been shown to
contribute to pancreatic cancer progression using mouse models
(83,84). A recent study found that glypican-1 is
specifically expressed by circulating cancer exosomes, and may
serve as non-invasive diagnostic and screening tool to enable early
diagnosis of pancreatic cancer (85).
As well as changes in glycosylation patterns cancer
cells may also display altered expression of proteins that interact
with glycans. An important example of such proteins is the
galectins, which are a group of glycan binding proteins with an
established role in cancer biology (86). In pancreatic cancer, Galectin-1 (GAL1)
and Galectin-3 (GAL3) are overexpressed (87–90). This
is important for cancer progression since GAL1 can induce stroma
remodelling, tumour cell proliferation, invasion, angiogenesis,
inflammation, and metastasis (91,92), and
GAL3 can activate pancreatic cancer cells to produce inflammatory
cytokines (88). It is likely that
galectin specific targeting will have a broad therapeutic potential
in pancreatic cancer, either alone or in combination with other
therapies (88,93).
The survival rates for pancreatic cancer have
remained dismal for many years, and as such there is an urgent need
to improve diagnosis and treatment. A wide range of alterations to
glycans have been detected in pancreatic cancer, and these show
promise as both potential circulating biomarkers and as targets for
glycan specific therapies. The expression of specific glycans
within pancreatic tumours, their presence in patient serum, and
their possible ability to facilitate metastases, suggests glycans
could help guide precision medicine strategies. Recent profiling
has defined 4 molecular subtypes of pancreatic cancer (94), and it likely that diversity exists
between pancreatic cancers in the variety and type of glycans made
and secreted into the blood (24). To
fully exploit glycans clinically it will be vital to fully profile
the pancreatic cancer glycome and determine how this varies between
different tumour types.
Not applicable.
Not applicable.
Not applicable.
JM conceived the review, researched the literature
and wrote the manuscript.
Not applicable.
Not applicable.
The author declares that there are no competing
interests.
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2018. CA Cancer J Clin. 68:7–30. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Garrido-Laguna I and Hidalgo M: Pancreatic
cancer: From state-of-the-art treatments to promising novel
therapies. Nat Rev Clin Oncol. 12:319–334. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Maitra A and Hruban RH: Pancreatic cancer.
Annu Rev Pathol. 3:157–188. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Klöppel G and Adsay NV: Chronic
pancreatitis and the differential diagnosis versus pancreatic
cancer. Arch Pathol Lab Med. 133:382–387. 2009.PubMed/NCBI
|
|
5
|
Meezan E, Wu HC, Black PH and Robbins PW:
Comparative studies on the carbohydrate-containing membrane
components of normal and virus-transformed mouse fibroblasts. II.
Separation of glycoproteins and glycopeptides by sephadex
chromatography. Biochemistry. 8:2518–2524. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Munkley J and Elliott DJ: Hallmarks of
glycosylation in cancer. Oncotarget. 7:35478–35489. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Feizi T: Demonstration by monoclonal
antibodies that carbohydrate structures of glycoproteins and
glycolipids are onco-developmental antigens. Nature. 314:53–57.
1985. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pinho SS and Reis CA: Glycosylation in
cancer: Mechanisms and clinical implications. Nat Rev Cancer.
15:540–555. 2015. View
Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kailemia MJ, Park D and Lebrilla CB:
Glycans and glycoproteins as specific biomarkers for cancer. Anal
Bioanal Chem. 409:395–410. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Munkley J: Glycosylation is a global
target for androgen control in prostate cancer cells. Endocr Relat
Cancer. 24:R49–R64. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mereiter S, Balmaña M, Gomes J, Magalhães
A and Reis CA: Glycomic approaches for the discovery of targets in
gastrointestinal cancer. Front Oncol. 6:552016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Adamczyk B, Tharmalingam T and Rudd PM:
Glycans as cancer biomarkers. Biochim Biophys Acta. 1820:1347–1353.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Munkley J, Vodak D, Livermore KE, James K,
Wilson BT, Knight B, Mccullagh P, Mcgrath J, Crundwell M, Harries
LW, et al: Glycosylation is an androgen-regulated process essential
for prostate cancer cell viability. EBioMedicine. 8:103–116. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Munkley J, Mills IG and Elliott DJ: The
role of glycans in the development and progression of prostate
cancer. Nat Rev Urol. 13:324–333. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Moniaux N, Andrianifahanana M, Brand RE
and Batra SK: Multiple roles of mucins in pancreatic cancer, a
lethal and challenging malignancy. Br J Cancer. 91:1633–1638. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Magnani JL, Nilsson B, Brockhaus M, Zopf
D, Steplewski Z, Koprowski H and Ginsburg V: A monoclonal
antibody-defined antigen associated with gastrointestinal cancer is
a ganglioside containing sialylated lacto-N-fucopentaose II. J Biol
Chem. 257:14365–14369. 1982.PubMed/NCBI
|
|
17
|
Magnani JL, Brockhaus M, Smith DF,
Ginsburg V, Blaszczyk M, Mitchell KF, Steplewski Z and Koprowski H:
A monosialoganglioside is a monoclonal antibody-defined antigen of
colon carcinoma. Science. 212:55–56. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Herlyn M, Sears HF, Steplewski Z and
Koprowski H: Monoclonal antibody detection of a circulating
tumor-associated antigen. I. Presence of antigen in sera of
patients with colorectal, gastric, and pancreatic carcinoma. J Clin
Immunol. 2:135–140. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Magnani JL, Steplewski Z, Koprowski H and
Ginsburg V: Identification of the gastrointestinal and pancreatic
cancer-associated antigen detected by monoclonal antibody 19-9 in
the sera of patients as a mucin. Cancer Res. 43:5489–5492.
1983.PubMed/NCBI
|
|
20
|
Yue T, Partyka K, Maupin KA, Hurley M,
Andrews P, Kaul K, Moser AJ, Zeh H, Brand RE and Haab BB:
Identification of blood-protein carriers of the CA 19-9 antigen and
characterization of prevalence in pancreatic diseases. Proteomics.
11:3665–3674. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Lahdenne P, Pitkänen S, Rajantie J,
Kuusela P, Siimes MA, Lanning M and Heikinheimo M: Tumor markers CA
125 and CA 19-9 in cord blood and during infancy: Developmental
changes and use in pediatric germ cell tumors. Pediatr Res.
38:797–801. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Goonetilleke KS and Siriwardena AK:
Systematic review of carbohydrate antigen (CA 19-9) as a
biochemical marker in the diagnosis of pancreatic cancer. Eur J
Surg Oncol. 33:266–270. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kalthoff H, Kreiker C, Schmiegel WH,
Greten H and Thiele HG: Characterization of CA 19-9 bearing mucins
as physiological exocrine pancreatic secretion products. Cancer
Res. 46:3605–3607. 1986.PubMed/NCBI
|
|
24
|
Tang H, Hsueh P, Kletter D, Bern M and
Haab B: The detection and discovery of glycan motifs in biological
samples using lectins and antibodies: New methods and
opportunities. Adv Cancer Res. 126:167–202. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Shah UA and Saif MW: Tumor markers in
pancreatic cancer: 2013. JOP. 14:318–321. 2013.PubMed/NCBI
|
|
26
|
Barton JG, Bois JP, Sarr MG, Wood CM, Qin
R, Thomsen KM, Kendrick ML and Farnell MB: Predictive and
prognostic value of CA 19-9 in resected pancreatic adenocarcinoma.
J Gastrointest Surg. 13:2050–2058. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Galli C, Basso D and Plebani M: CA 19-9:
Handle with care. Clin Chem Lab Med. 51:1369–1383. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Yue T, Maupin KA, Fallon B, Li L, Partyka
K, Anderson MA, Brenner DE, Kaul K, Zeh H, Moser AJ, et al:
Enhanced discrimination of malignant from benign pancreatic disease
by measuring the CA 19-9 antigen on specific protein carriers. PLoS
One. 6:e291802011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Tempero MA, Uchida E, Takasaki H, Burnett
DA, Steplewski Z and Pour PM: Relationship of carbohydrate antigen
19-9 and Lewis antigens in pancreatic cancer. Cancer Res.
47:5501–5503. 1987.PubMed/NCBI
|
|
30
|
Remmers N, Anderson JM, Linde EM, DiMaio
DJ, Lazenby AJ, Wandall HH, Mandel U, Clausen H, Yu F and
Hollingsworth MA: Aberrant expression of mucin core proteins and
o-linked glycans associated with progression of pancreatic cancer.
Clin Cancer Res. 19:1981–1993. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Partyka K, Maupin KA, Brand RE and Haab
BB: Diverse monoclonal antibodies against the CA 19-9 antigen show
variation in binding specificity with consequences for clinical
interpretation. Proteomics. 12:2212–2220. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Tang H, Partyka K, Hsueh P, Sinha JY,
Kletter D, Zeh H, Huang Y, Brand RE and Haab BB: Glycans related to
the CA19-9 antigen are elevated in distinct subsets of pancreatic
cancers and improve diagnostic accuracy over CA19-9. Cell Mol
Gastroenterol Hepatol. 2:201–221.e215. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Xu HL, Zhao X, Zhang KM, Tang W and Kokudo
N: Inhibition of KL-6/MUC1 glycosylation limits aggressive
progression of pancreatic cancer. World J Gastroenterol.
20:12171–12181. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Pour PM, Tempero MM, Takasaki H, Uchida E,
Takiyama Y, Burnett DA and Steplewski Z: Expression of blood
group-related antigens ABH, Lewis A, Lewis B, Lewis X, Lewis Y and
CA 19-9 in pancreatic cancer cells in comparison with the patient's
blood group type. Cancer Res. 48:5422–5426. 1988.PubMed/NCBI
|
|
35
|
Singh S, Pal K, Yadav J, Tang H, Partyka
K, Kletter D, Hsueh P, Ensink E, Kc B, Hostetter G, et al:
Upregulation of glycans containing 3′ fucose in a subset of
pancreatic cancers uncovered using fusion-tagged lectins. J
Proteome Res. 14:2594–2605. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Tang H, Singh S, Partyka K, Kletter D,
Hsueh P, Yadav J, Ensink E, Bern M, Hostetter G, Hartman D, et al:
Glycan motif profiling reveals plasma sialyl-lewis × elevations in
pancreatic cancers that are negative for sialyl-lewis A. Mol Cell
Proteomics. 14:1323–1333. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Balmaña M, Sarrats A, Llop E, Barrabés S,
Saldova R, Ferri MJ, Figueras J, Fort E, de Llorens R, Rudd PM and
Peracaula R: Identification of potential pancreatic cancer serum
markers: Increased sialyl-Lewis X on ceruloplasmin. Clin Chim Acta.
442:56–62. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Natoni A, Macauley MS and O'Dwyer ME:
Targeting selectins and their ligands in cancer. Front Oncol.
6:932016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Takahashi S, Oda T, Hasebe T, Sasaki S,
Kinoshita T, Konishi M, Ueda T, Nakahashi C, Ochiai T and Ochiai A:
Overexpression of sialyl Lewis × antigen is associated with
formation of extratumoral venous invasion and predicts
postoperative development of massive hepatic metastasis in cases
with pancreatic ductal adenocarcinoma. Pathobiology. 69:127–135.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Rho JH, Mead JR, Wright WS, Brenner DE,
Stave JW, Gildersleeve JC and Lampe PD: Discovery of sialyl Lewis A
and Lewis X modified protein cancer biomarkers using high density
antibody arrays. J Proteomics. 96:291–299. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Metzgar RS, Gaillard MT, Levine SJ, Tuck
FL, Bossen EH and Borowitz MJ: Antigens of human pancreatic
adenocarcinoma cells defined by murine monoclonal antibodies.
Cancer Res. 42:601–608. 1982.PubMed/NCBI
|
|
42
|
Kawa S, Tokoo M, Oguchi H, Furuta S, Homma
T, Hasegawa Y, Ogata H and Sakata K: Epitope analysis of SPan-1 and
DUPAN-2 using synthesized glycoconjugates sialyllact-N-fucopentaose
II and sialyllact-N-tetraose. Pancreas. 9:692–697. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Munkley J: The role of Sialyl-Tn in
cancer. Int J Mol Sci. 17:2752016. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Radhakrishnan P, Dabelsteen S, Madsen FB,
Francavilla C, Kopp KL, Steentoft C, Vakhrushev SY, Olsen JV,
Hansen L, Bennett EP, et al: Immature truncated O-glycophenotype of
cancer directly induces oncogenic features. Proc Natl Acad Sci USA.
111:E4066–E4075. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Hofmann BT, Schlüter L, Lange P,
Mercanoglu B, Ewald F, Fölster A, Picksak AS, Harder S, El Gammal
AT, Grupp K, et al: COSMC knockdown mediated aberrant
O-glycosylation promotes oncogenic properties in pancreatic cancer.
Mol Cancer. 14:1092015. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Itzkowitz S, Kjeldsen T, Friera A,
Hakomori S, Yang US and Kim YS: Expression of Tn, sialosyl Tn, and
T antigens in human pancreas. Gastroenterology. 100:1691–1700.
1991. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Chugh S, Meza J, Sheinin YM, Ponnusamy MP
and Batra SK: Loss of N-acetylgalactosaminyltransferase 3 in poorly
differentiated pancreatic cancer: Augmented aggressiveness and
aberrant ErbB family glycosylation. Br J Cancer. 114:1376–1386.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Wang Y, Ju T, Ding X, Xia B, Wang W, Xia
L, He M and Cummings RD: Cosmc is an essential chaperone for
correct protein O-glycosylation. Proc Natl Acad Sci USA.
107:9228–9233. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Taniuchi K, Cerny RL, Tanouchi A, Kohno K,
Kotani N, Honke K, Saibara T and Hollingsworth MA: Overexpression
of GalNAc-transferase GalNAc-T3 promotes pancreatic cancer cell
growth. Oncogene. 30:4843–4854. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Pan S, Tamura Y, Chen R, May D, McIntosh
MW and Brentnall TA: Large-scale quantitative glycoproteomics
analysis of site-specific glycosylation occupancy. Mol Biosyst.
8:2850–2856. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Pan S, Chen R, Tamura Y, Crispin DA, Lai
LA, May DH, McIntosh MW, Goodlett DR and Brentnall TA: Quantitative
glycoproteomics analysis reveals changes in N-glycosylation level
associated with pancreatic ductal adenocarcinoma. J Proteome Res.
13:1293–1306. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Contessa JN, Bhojani MS, Freeze HH,
Rehemtulla A and Lawrence TS: Inhibition of N-linked glycosylation
disrupts receptor tyrosine kinase signaling in tumor cells. Cancer
Res. 68:3803–3809. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Pérez-Garay M, Arteta B, Llop E, Cobler L,
Pagès L, Ortiz R, Ferri MJ, de Bolós C, Figueras J, de Llorens R,
et al: α2,3-Sialyltransferase ST3Gal IV promotes migration and
metastasis in pancreatic adenocarcinoma cells and tends to be
highly expressed in pancreatic adenocarcinoma tissues. Int J
Biochem Cell Biol. 45:1748–1757. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Pérez-Garay M, Arteta B, Pagès L, de
Llorens R, de Bolòs C, Vidal-Vanaclocha F and Peracaula R:
alpha2,3-sialyltransferase ST3Gal III modulates pancreatic cancer
cell motility and adhesion in vitro and enhances its metastatic
potential in vivo. PLoS One. 5(pii): e125242010. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Hsieh CC, Shyr YM, Liao WY, Chen TH, Wang
SE, Lu PC, Lin PY, Chen YB, Mao WY, Han HY, et al: Elevation of
β-galactoside α2,6-sialyltransferase 1 in a fructoseresponsive
manner promotes pancreatic cancer metastasis. Oncotarget.
8:7691–7709. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Yue T, Goldstein IJ, Hollingsworth MA,
Kaul K, Brand RE and Haab BB: The prevalence and nature of glycan
alterations on specific proteins in pancreatic cancer patients
revealed using antibody-lectin sandwich arrays. Mol Cell
Proteomics. 8:1697–1707. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Park HM, Hwang MP, Kim YW, Kim KJ, Jin JM,
Kim YH, Yang YH, Lee KH and Kim YG: Mass spectrometry-based
N-linked glycomic profiling as a means for tracking pancreatic
cancer metastasis. Carbohydr Res. 413:5–11. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Zhao J, Qiu W, Simeone DM and Lubman DM:
N-linked glycosylation profiling of pancreatic cancer serum using
capillary liquid phase separation coupled with mass spectrometric
analysis. J Proteome Res. 6:1126–1138. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Kamada Y, Kinoshita N, Tsuchiya Y,
Kobayashi K, Fujii H, Terao N, Kamihagi K, Koyama N, Yamada S,
Daigo Y, et al: Reevaluation of a lectin antibody ELISA kit for
measuring fucosylated haptoglobin in various conditions. Clin Chim
Acta. 417:48–53. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Barrabés S, Pagès-Pons L, Radcliffe CM,
Tabarés G, Fort E, Royle L, Harvey DJ, Moenner M, Dwek RA, Rudd PM,
et al: Glycosylation of serum ribonuclease 1 indicates a major
endothelial origin and reveals an increase in core fucosylation in
pancreatic cancer. Glycobiology. 17:388–400. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Fardini Y, Dehennaut V, Lefebvre T and
Issad T: O-GlcNAcylation: A new cancer hallmark? Front Endocrinol
(Lausanne). 4(99)2013.PubMed/NCBI
|
|
62
|
Bond MR and Hanover JA: A little sugar
goes a long way: The cell biology of O-GlcNAc. J Cell Biol.
208:869–880. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Liu Y, Cao Y, Pan X, Shi M, Wu Q, Huang T,
Jiang H, Li W and Zhang J: O-GlcNAc elevation through activation of
the hexosamine biosynthetic pathway enhances cancer cell
chemoresistance. Cell Death Dis. 9:4852018. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Qian K, Wang S, Fu M, Zhou J, Singh JP, Li
MD, Yang Y, Zhang K, Wu J, Nie Y, et al: Transcriptional regulation
of O-GlcNAc homeostasis is disrupted in pancreatic cancer. J Biol
Chem. 293:13989–14000. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Konrad RJ and Kudlow JE: The role of
O-linked protein glycosylation in beta-cell dysfunction. Int J Mol
Med. 10:535–539. 2002.PubMed/NCBI
|
|
66
|
Ma Z, Vocadlo DJ and Vosseller K:
Hyper-O-GlcNAcylation is anti-apoptotic and maintains constitutive
NF-κB activity in pancreatic cancer cells. J Biol Chem.
288:15121–15130. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Zachara NE, O'Donnell N, Cheung WD, Mercer
JJ, Marth JD and Hart GW: Dynamic O-GlcNAc modification of
nucleocytoplasmic proteins in response to stress. A survival
response of mammalian cells. J Biol Chem. 279:30133–30142. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Banerjee S, Sangwan V, McGinn O, Chugh R,
Dudeja V, Vickers SM and Saluja AK: Triptolide-induced cell death
in pancreatic cancer is mediated by O-GlcNAc modification of
transcription factor Sp1. J Biol Chem. 288:33927–33938. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Garg B, Giri B, Majumder K, Dudeja V,
Banerjee S and Saluja A: Modulation of post-translational
modifications in β-catenin and LRP6 inhibits Wnt signaling pathway
in pancreatic cancer. Cancer Lett. 388:64–72. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Sharma NS, Gupta VK, Dauer P, Kesh K,
Hadad R, Giri B, Chandra A, Dudeja V, Slawson C, Banerjee S, et al:
O-GlcNAc modification of oncogenic transcription factor Sox2
promotes protein stability and regulates self-renewal in pancreatic
cancer. bioRxiv. doi: https://doi.org/10.1101/345223.
|
|
71
|
Dwek RA, Butters TD, Platt FM and Zitzmann
N: Targeting glycosylation as a therapeutic approach. Nat Rev Drug
Discov. 1:65–75. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
72
|
Vasconcelos-Dos-Santos A, Oliveira IA,
Lucena MC, Mantuano NR, Whelan SA, Dias WB and Todeschini AR:
Biosynthetic machinery involved in aberrant glycosylation:
Promising targets for developing of drugs against cancer. Front
Oncol. 5:1382015. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Iozzo RV and Sanderson RD: Proteoglycans
in cancer biology, tumour microenvironment and angiogenesis. J Cell
Mol Med. 15:1013–1031. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Pan S, Chen R, Stevens T, Bronner MP, May
D, Tamura Y, McIntosh MW and Brentnall TA: Proteomics portrait of
archival lesions of chronic pancreatitis. PLoS One. 6:e275742011.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Pan S, Chen R, Reimel BA, Crispin DA,
Mirzaei H, Cooke K, Coleman JF, Lane Z, Bronner MP, Goodlett DR, et
al: Quantitative proteomics investigation of pancreatic
intraepithelial neoplasia. Electrophoresis. 30:1132–1144. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Chen R, Yi EC, Donohoe S, Pan S, Eng J,
Cooke K, Crispin DA, Lane Z, Goodlett DR, Bronner MP, et al:
Pancreatic cancer proteome: The proteins that underlie invasion,
metastasis, and immunologic escape. Gastroenterology.
129:1187–1197. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Chen WB, Lenschow W, Tiede K, Fischer JW,
Kalthoff H and Ungefroren H: Smad4/DPC4-dependent regulation of
biglycan gene expression by transforming growth factor-beta in
pancreatic tumor cells. J Biol Chem. 277:36118–36128. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Koninger J, Giese T, di Mola FF, Wente MN,
Esposito I, Bachem MG, Giese NA, Büchler MW and Friess H:
Pancreatic tumor cells influence the composition of the
extracellular matrix. Biochem Biophys Res Commun. 322:943–949.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Koninger J, Giese NA, di Mola FF, Berberat
P, Giese T, Esposito I, Bachem MG, Büchler MW and Friess H:
Overexpressed decorin in pancreatic cancer: Potential tumor growth
inhibition and attenuation of chemotherapeutic action. Clin Cancer
Res. 10:4776–4783. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Weber CK, Sommer G, Michl P, Fensterer H,
Weimer M, Gansauge F, Leder G, Adler G and Gress TM: Biglycan is
overexpressed in pancreatic cancer and induces G1-arrest in
pancreatic cancer cell lines. Gastroenterology. 121:657–667. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Conejo JR, Kleeff J, Koliopanos A, Matsuda
K, Zhu ZW, Goecke H, Bicheng N, Zimmermann A, Korc M, Friess H and
Büchler MW: Syndecan-1 expression is up-regulated in pancreatic but
not in other gastrointestinal cancers. Int J Cancer. 88:12–20.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Kleeff J, Ishiwata T, Kumbasar A, Friess
H, Büchler MW, Lander AD and Korc M: The cell-surface heparan
sulfate proteoglycan glypican-1 regulates growth factor action in
pancreatic carcinoma cells and is overexpressed in human pancreatic
cancer. J Clin Invest. 102:1662–1673. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Whipple CA, Young AL and Korc M: A
KrasG12D-driven genetic mouse model of pancreatic cancer requires
glypican-1 for efficient proliferation and angiogenesis. Oncogene.
31:2535–2544. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Aikawa T, Whipple CA, Lopez ME, Gunn J,
Young A, Lander AD and Korc M: Glypican-1 modulates the angiogenic
and metastatic potential of human and mouse cancer cells. J Clin
Invest. 118:89–99. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Melo SA, Luecke LB, Kahlert C, Fernandez
AF, Gammon ST, Kaye J, LeBleu VS, Mittendorf EA, Weitz J, Rahbari
N, et al: Glypican-1 identifies cancer exosomes and detects early
pancreatic cancer. Nature. 523:177–182. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Ebrahim AH, Alalawi Z, Mirandola L,
Rakhshanda R, Dahlbeck S, Nguyen D, Jenkins M, Grizzi F, Cobos E,
Figueroa JA, et al: Galectins in cancer: Carcinogenesis, diagnosis
and therapy. Ann Transl Med. 2:882014.PubMed/NCBI
|
|
87
|
Qian D, Lu Z, Xu Q, Wu P, Tian L, Zhao L,
Cai B, Yin J, Wu Y, Staveley-O'Carroll KF, et al: Galectin-1-driven
upregulation of SDF-1 in pancreatic stellate cells promotes
pancreatic cancer metastasis. Cancer Lett. 397:43–51. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Zhao W, Ajani JA, Sushovan G, Ochi N,
Hwang R, Hafley M, Johnson RL, Bresalier RS, Logsdon CD, Zhang Z
and Song S: Galectin-3 mediates tumor cell-stroma interactions by
activating pancreatic stellate cells to produce cytokines via
integrin signaling. Gastroenterology. 154:1524–1537.e6. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Chen R, Pan S, Ottenhof NA, de Wilde RF,
Wolfgang CL, Lane Z, Post J, Bronner MP, Willmann JK, Maitra A and
Brentnall TA: Stromal galectin-1 expression is associated with
long-term survival in resectable pancreatic ductal adenocarcinoma.
Cancer Biol Ther. 13:899–907. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Chen R, Dawson DW, Pan S, Ottenhof NA, de
Wilde RF, Wolfgang CL, May DH, Crispin DA, Lai LA, Lay AR, et al:
Proteins associated with pancreatic cancer survival in patients
with resectable pancreatic ductal adenocarcinoma. Lab Invest.
95:43–55. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Martinez-Bosch N, Fernández-Barrena MG,
Moreno M, Ortiz-Zapater E, Munné-Collado J, Iglesias M, André S,
Gabius HJ, Hwang RF, Poirier F, et al: Galectin-1 drives pancreatic
carcinogenesis through stroma remodeling and Hedgehog signaling
activation. Cancer Res. 74:3512–3524. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Orozco CA, Martinez-Bosch N, Guerrero PE,
Vinaixa J, Dalotto-Moreno T, Iglesias M, Moreno M, Djurec M,
Poirier F, Gabius HJ, et al: Targeting galectin-1 inhibits
pancreatic cancer progression by modulating tumor-stroma crosstalk.
Proc Natl Acad Sci USA. 115:E3769–E3778. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Seguin L, Camargo MF, Wettersten HI, Kato
S, Desgrosellier JS, von Schalscha T, Elliott KC, Cosset E,
Lesperance J, Weis SM and Cheresh DA: Galectin-3, a druggable
vulnerability for KRAS-addicted cancers. Cancer Discov.
7:1464–1479. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Bailey P, Chang DK, Nones K, Johns AL,
Patch AM, Gingras MC, Miller DK, Christ AN, Bruxner TJ, Quinn MC,
et al: Genomic analyses identify molecular subtypes of pancreatic
cancer. Nature. 531:47–52. 2016. View Article : Google Scholar : PubMed/NCBI
|