Introduction
Renal cell carcinoma (RCC) accounts for ~3% of new
cancer cases and at the time of diagnosis 20–30% of all RCC
patients have a metastatic disease (1). The mortality of more than 100,000
patients is due to RCC every year, worldwide (2). Patients with sarcomatoid RCC, which
represents a histological variant found in 5–8% of all RCC, have a
poor prognosis, with a reported median survival of between nine and
19 months (3). Although several
studies with small numbers of patients (<20) have demonstrated
the efficacy of chemotherapy (4)
and molecular-targeted agents against sarcomatoid RCC (5), no consensus has been reached with
regard to the optimal approach for managing sarcomatoid RCC. The
current study presents a case of metastatic sarcomatoid RCC treated
with systemic chemotherapy followed by mammalian target of
rapamycin (mTOR) inhibitor maintenance therapy. Consent was
obtained from the family of the patient.
Case report
A 63-year-old male presented with lumbago, and
lumbar vertebral tumors were detected on magnetic resonance
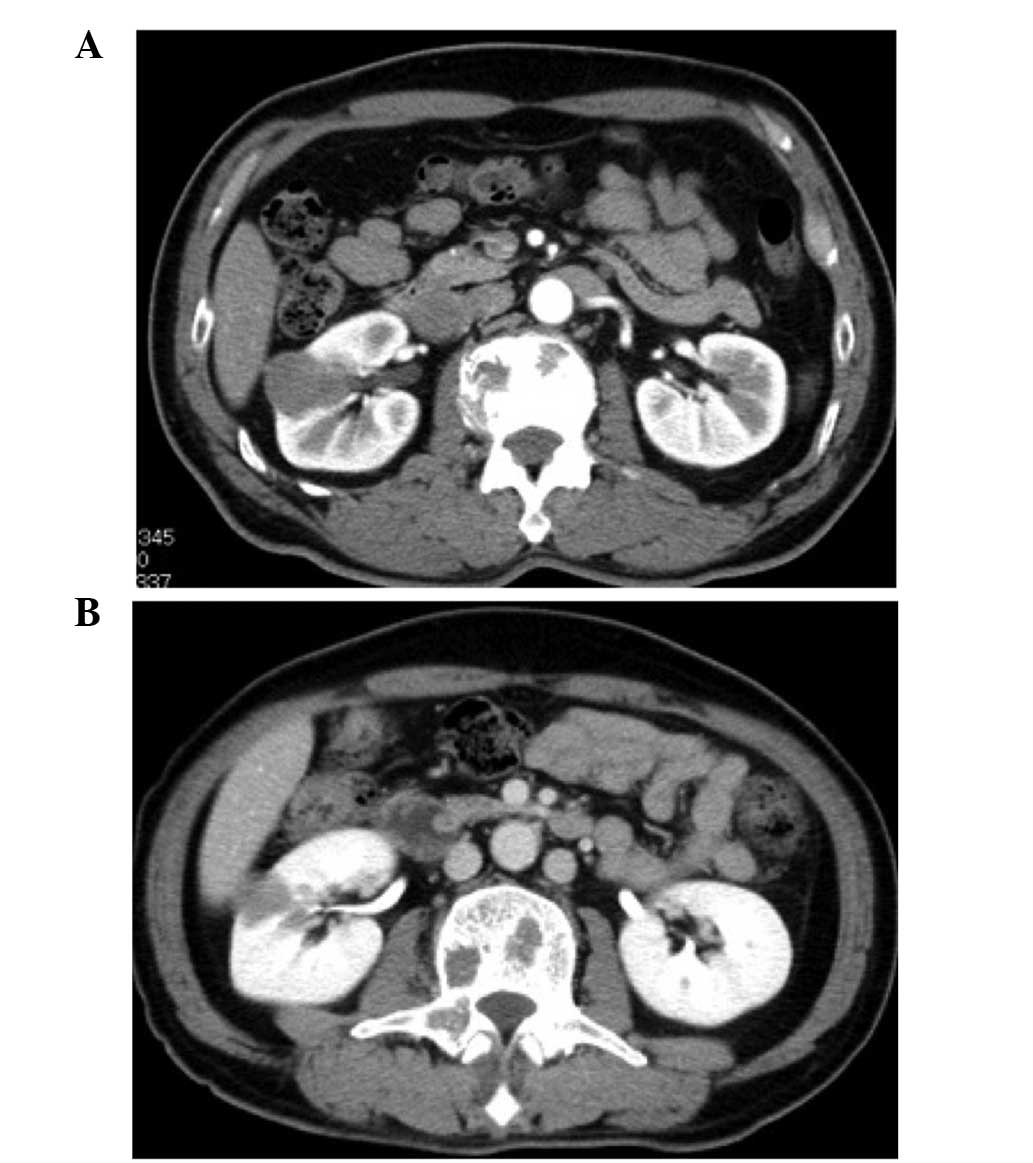
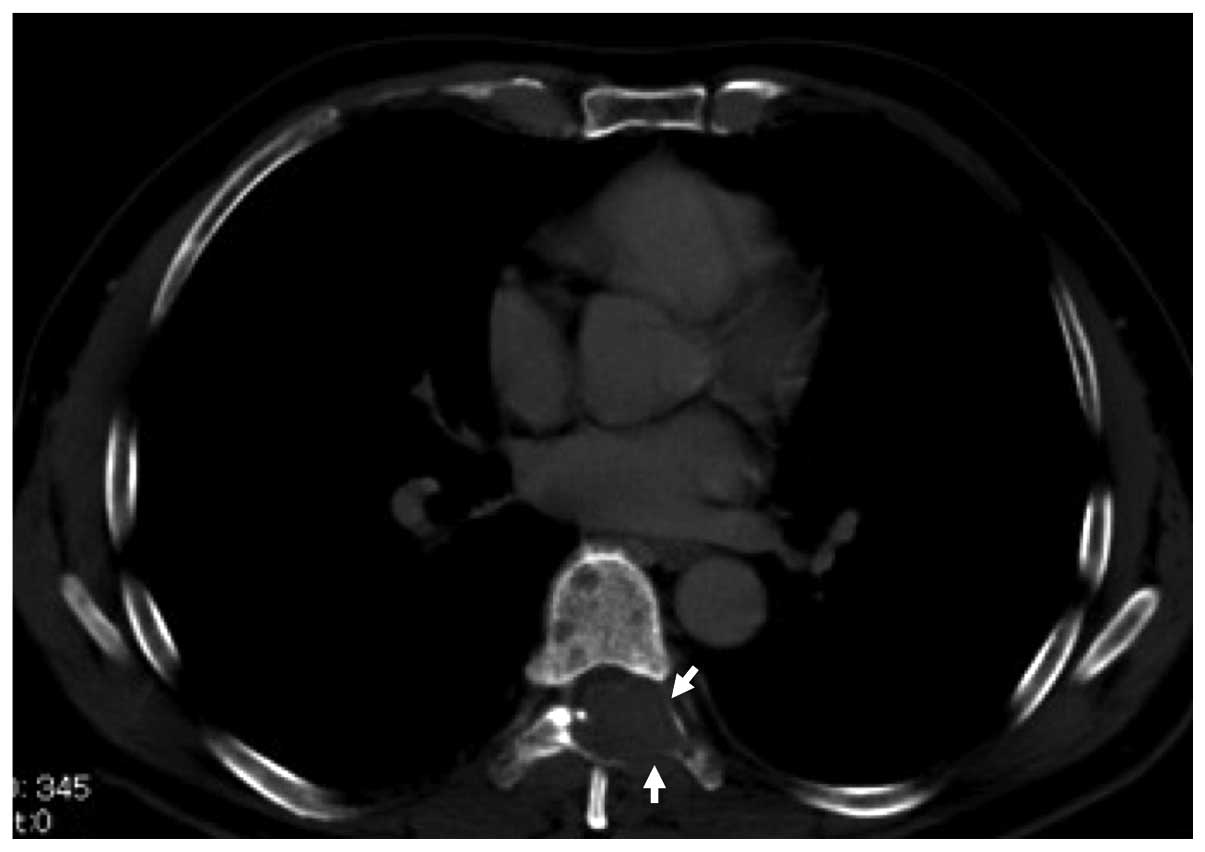
imaging. Subsequent computed tomography (CT) revealed a right renal
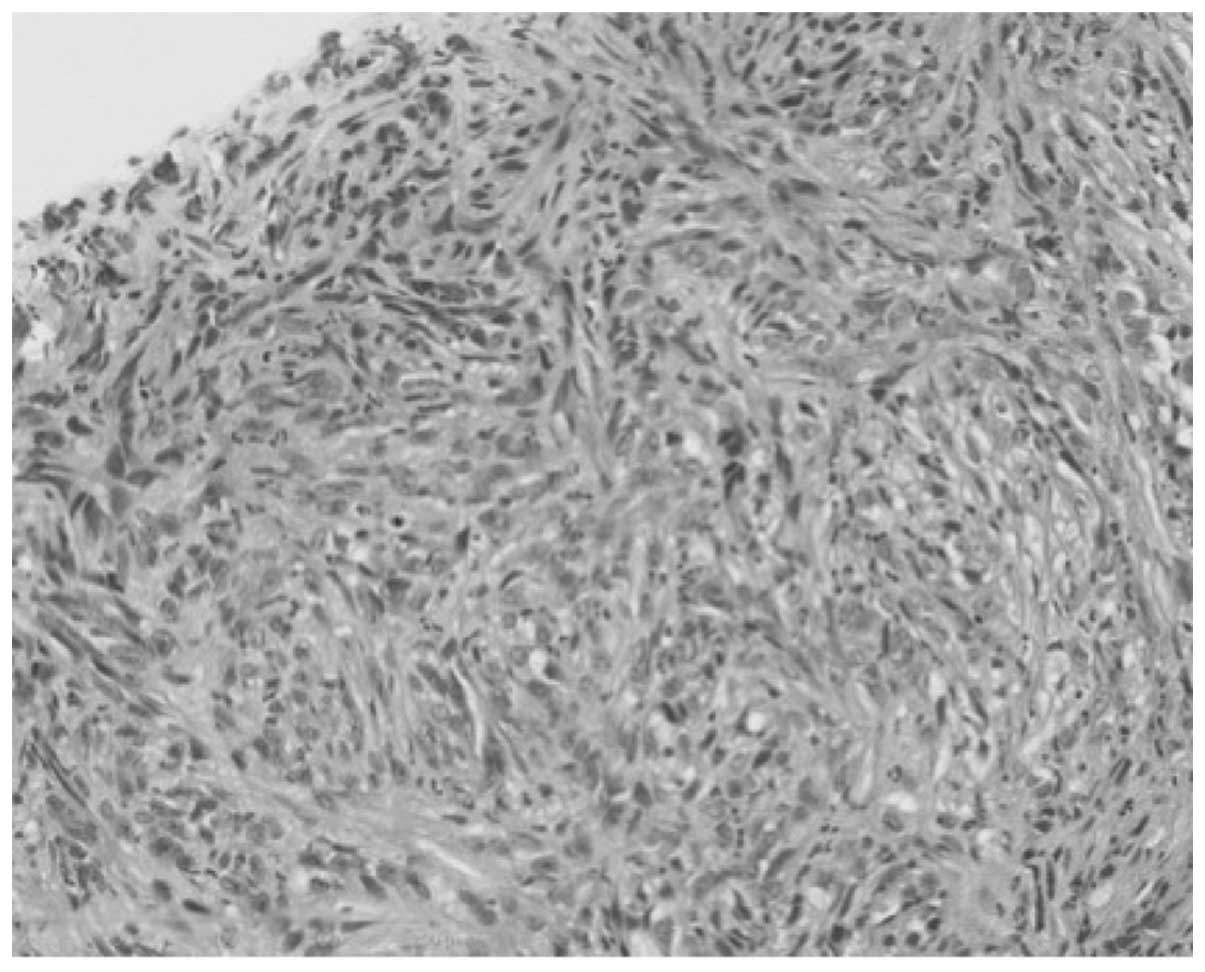
tumor and multiple bone metastases (Figs. 1A and 2). CT-guided biopsy of the right renal and
left sacroiliac tumors revealed pure sarcomatoid carcinoma without
any clear cell component, which was consistent with sarcomatoid RCC
and bone metastases (Fig. 3).
Radiation therapy (total dose of 30 Gy) was administered to the
thoracic vertebrae to relieve the pain due to bone metastases. Two
cycles of combination chemotherapy comprising of gemcitabine (1,500
mg/m2 on day one) and doxorubicin (50 mg/m2
on day one) (4) were administered,
resulting in a 20% reduction in the longest diameter of the right
renal tumor (Fig. 1B). However, due
to grade 3 neutropenia, chemotherapy was discontinued and
temsirolimus (25 mg once weekly) was administered, resulting in
stable disease for 19 months. During the 21-month treatment with
temsirolimus, the patient experienced no major adverse events with
the exception of grade 2 nausea. The patient succumbed to their
disease 30 months following the initiation of treatment.
Discussion
Sarcomatoid RCC, which accounts for 4% of all RCC,
has an aggressive nature and poor prognosis. Although novel
therapies include vascular endothelial growth factor, tyrosine
kinase inhibitors and mammalian target of rapamycin inhibitors, all
of which have shown significant activity against RCC with
metastases, no treatment has been established for sarcomatoid RCC
and few studies have analyzed this histological variant.
Furthermore, reports discussing the effects of vascular endothelial
growth factor-targeted agents are limited. Certain authors have
reported the efficacy of tyrosine kinase inhibitors for sarcomatoid
RCC only in patients with a limited amount of sarcomatoid
components (<20%) in the primary tumor (5). In addition, a recent study from the MD
Anderson Cancer Center illustrated that sunitinib shows no benefit
in RCC patients with >50% sarcomatoid components (6).
In 2004, Nanus et al (7) reported antitumor activity in several
patients with sarcomatoid RCC who had been treated with a
combination of gemcitabine and doxorubicin chemotherapy. A
favorable result led to an Eastern Cooperative Oncology Group phase
I trial to confirm the efficacy of this regimen (4). In this study, six of the 39 patients
(16%) achieved a complete or partial response and 10 patients (26%)
had stable disease; however, 14 patients (37%) developed grade 3 or
higher toxicities (4).
Experience with novel targeted agents in sarcomatoid
RCC is limited, whereas a phase III trial on temsirolimus versus
interferon showed survival benefit for patients with poor
prognostic features; likely to be sarcomatoid RCC (8). In addition, a case series by Areses
et al (9) indicated that
toxicity is not the main issue during temsirolimus use for
sarcomatoid RCC. Temsirolimus may be a valid therapeutic option
with tolerable toxicity for stabilizing tumor progression in
sarcomatoid RCC.
Recently, Staehler et al (10) reported that combination chemotherapy
using gemcitabine and doxorubicin with subsequent antiangiogenic
treatment using the multi-tyrosine kinase inhibitor, sorafenib,
resulted in additional progression-free survival in five of the
nine patients with sarcomatoid RCC. Furthermore, clinical trials on
combination therapy comprising of gemcitabine and
molecular-targeted agents are ongoing (11).
Immunohistochemistry has shown that sarcomatoid RCC
overexpresses hypoxia-inducible factor 1a (HIF-1a) and
phosphorylated eukaryotic initiation factor 4E-binding protein
(p-4E-BP1) (5). HIF-1a is directly
downstream of mTOR, whereas p-4E-BP1 is a direct target of mTOR
(12). These results may support
the clinical efficacy of mTOR inhibitor in sarcomatoid RCC, which
may compensate for the sequential use of chemotherapy and prolong
tumor control. Further investigation of the molecular biology of
the sarcomatoid variant may elucidate the specific features of
sarcomatoid RCC and provide appropriate treatment strategies.
Acknowledgements
The authors would like to thank Dr Horikawa of the
Akita Red Cross Hospital (Akita, Japan) for treatment
suggestions.
References
|
1
|
Sun M, Thuret R, Abdollah F, et al:
Age-adjusted incidence, mortality, and survival rates of
stage-specific renal cell carcinoma in North America: a trend
analysis. Eur Urol. 59:135–141. 2011.
|
|
2
|
Basso M, Cassano A and Barone C: A survey
of therapy for advanced renal cell carcinoma. Urol Oncol.
24:121–133. 2010.
|
|
3
|
de Peralta-Venturina M, Moch H, Amin M, et
al: Sarcomatoid differentiation in renal cell carcinoma: a study of
101 cases. Am J Surg Pathol. 25:275–284. 2001.
|
|
4
|
Haas NB, Lin X, Manola J, et al: A phase
II trial of doxorubicin and gemcitabine in renal cell carcinoma
with sarcomatoid features: ECOG 8802. Med Oncol. 29:761–767.
2012.
|
|
5
|
Molina AM, Tickoo SK, Ishill N, et al:
Sarcomatoid-variant renal cell carcinoma: treatment outcome and
survival in advanced disease. Am J Clin Oncol. 34:454–459.
2011.
|
|
6
|
Tannir NM, Plimack E, Ng C, et al: A phase
2 trial of sunitinib in patients with advanced non-clear cell renal
cell carcinoma. Eur Urol. 62:1013–1019. 2012.
|
|
7
|
Nanus DM, Garino A, Milowsky MI, et al:
Active chemotherapy for sarcomatoid and rapidly progressing renal
cell carcinoma. Cancer. 101:1545–1551. 2004.
|
|
8
|
Hudes G, Carducci M, Tomczak P, et al:
Temsirolimus, interferon alfa, or both for advanced renal-cell
carcinoma. N Engl J Med. 356:2271–2281. 2007.
|
|
9
|
Areses MC, Herranz UA, Ferrán BB, et al:
Temsirolimus in renal cell carcinoma with sarcomatoid
differentiation: a report of three cases. Med Oncol. 29:795–798.
2012.
|
|
10
|
Staehler M, Haseke N, Roosen A, et al:
Sorafenib after combination therapy with gemcitabine plus
doxorubicine in patients with sarcomatoid renal cell carcinoma: a
prospective evaluation. Eur J Med Res. 15:287–291. 2010.
|
|
11
|
Michaelson DF, McDermott MB, Atkins DC, et
al: Phase II trial of sunitinib and gemcitabine in patients with
sarcomatoid and/or poor-risk metastatic renal cell carcinoma. J
Clin Oncol. 28(suppl 15): e150762010.
|
|
12
|
Corradetti MN and Guan KL: Upstream of the
mammalian target of rapamycin: do all roads pass through mTOR?
Oncogene. 25:6347–6360. 2006.
|