Introduction
Among the hepatic vascular tumors, cavernous
hemangioma and infantile hemangioendothelioma are benign, while
epithelioid hemangioendothelioma and angiosarcoma are malignant.
Cavernous hemangioma occurs at all ages, but most frequently in
adults, while infantile hemangioendothelioma occurs between birth
and 21 years of age (1).
α-fetoprotein (AFP) is a fetal-specific glycoprotein produced by
the fetal liver. Usually, the AFP serum concentration falls rapidly
subsequent to birth, while normal adult levels are usually achieved
by the age of eight to 12 months. The normal range of AFP for
adults and children is variously reported as <50, <10 and
<5 μg/l (2,3). Clinically, AFP is one of the
indicators that aids in the diagnosis of hepatocellular carcinoma
(HCC), particularly for the patients with chronic liver diseases
(3–5). There are numerous studies that have
reported a higher level of AFP serum exhibiting an increased
association with a poor prognosis for patients with HCC (4,6). There
are numerous other diseases, excluding HCC, that are also
associated with an increased serum AFP level, including fulminant
hepatitis, hepatic cirrhosis, gastric cancer and endodermal sinus
tumors of the testes, ovaries and extragonadal sites (7–13). As
one of the benign neoplasms, the AFP level of hepatic cavernous
hemangioma patients is not usually outside the normal range. The
present study reports the case of hepatic cavernous hemangioma with
a highly elevated AFP level in a 47-year-old male. Written informed
consent was obtained from the patient.
Case report
Patient history
A 47-year-old male was admitted to the Department of
Hepatobiliary Surgery (The First Affiliated Hospital of Sun Yat-Sen
University, Guangzhou, Guangdong, China) on 14th February 2013 with
a six-month history of fatigue and a four-month history of elevated
alanine and aspartate aminopherase levels according to colorimetric
assay. The patient possessed a 20-year history of chronic hepatitis
B with no medical control. In January 2013, the patient was
admitted to Dongguan Kanghua Hospital (Dongguan, Guangdong, China)
with a five-month history of fatigue.
Examination
During his hospitalization at Dongguan Kanghua
Hospital, abdominal computed tomography (CT) scans revealed a tumor
located in the right liver, with good enhancement in the arterial
and portal venous phases, and multiple cysts in the liver. Magnetic
resonance imaging (MRI) revealed a tumor with good enhancement. A
diagnosis of hemangioma was considered, but hepatocellular
carcinoma could not be excluded. On 4th February, abdominal
sonography in the outpatient clinic of The First Affiliated
Hospital of Sun Yat-Sen University revealed a solid nodule located
in segment eight of the liver, multiple cysts in segments 2, 4 and
5 of the liver, calcification in segment six of the liver and
multiple gallbladder polyps. The serum level of AFP was 371.51 μg/l
(normal range, 0–20 μg/l). During physical examination, no ascites
were detected and the abdomen was tender on palpation. The results
of the laboratory tests performed during hospitalization are shown
in Table I. Serum levels of tumor
markers, including AFP, carcinoembryonic antigen (CEA) and
carbohydrate antigen (CA)-199 were out of the normal range
(Table II).
 | Table IResult of laboratory tests. |
Table I
Result of laboratory tests.
| Laboratory test | On admission | Post-operative week
four | Reference range |
|---|
| Alanine
aminotransferase (U/l) | 300↑ | 35 | 1–40 |
| Aspartate
aminotransferase (U/l) | 390↑ | 91↑ | 1–37 |
| Fasting plasma
glucose (mmol/l) | 4.6 | 4.9 | 2.9–6.0 |
| Urea (mmol/l) | 4.4 | 12.1 | 2.9–8.6 |
| Serum creatinine
(μmol/l) | 73 | 102 | 53–115 |
| Lactate dehydrogenase
(U/ml) | 256↑ | 120↓ | 114–240 |
|
Gamma-glutamyltransferase (U/l) | 323↑ | 101↓ | 2–50 |
| Alkaline phosphatase
(U/l) | 98 | 71 | 0–110 |
| Total protein
(g/l) | 76.4 | 42.3 | 64.0–87.0 |
| Albumin (g/l) | 37.5 | 32.4 | 35.0–50.0 |
| Globulin (g/l) | 38.9 | 9.9↓ | 20.0–32.0 |
| Direct bilirubin
(μmol/l) | 19.7↑ | 29.3↑ | 0.5–7.0 |
| Indirect bilirubin
(μmol/l) | 25↑ | 25.2↑ | 3.0–15.0 |
| Sodium (mmol/l) | 139 | 129 | 135–145 |
| Potassium
(mmol/l) | 4.16 | 4.3 | 3.5–5.3 |
| Hemoglobin (g/l) | 169↑ | 140 | 120–160 |
| Hematocrit
(proportion of 1.0) | 0.494↑ | 0.28 | 0.110–0.280 |
| White blood cells
(×109/l) | 5.19 | 9.19 | 4.00–10.00 |
| Platelets
(×109/l) | 141 | 288 | 100–300 |
| Mean corpuscular
volume (fl) | 96.5↑ | 95.9↑ | 82–95 |
| Markers of viral
hepatitis |
| Hepatitis B surface
antigen | + | | |
| Antibody to
hepatitis B surface antigen | − | | |
| Antibody to
hepatitis C virus | − | | |
| Hepatitis B
e-antigen | + | | |
| Antibody to
hepatitis B e-antigen | + | | |
 | Table IISerum level of tumor markers. |
Table II
Serum level of tumor markers.
| Tumor marker | On admission | Two days after
operation | One week after
operation | Two weeks after
operation | Reference range |
|---|
| AFP (ug/l) | 371.51↑ | 180 | 111 | 24.45 | 0.00–20.00 |
| CEA (ug/l) | 5.59↑ | | | | 0.00–5.00 |
| CA199 (U/ml) | 39.74↑ | | | | 0.00–35.00 |
| CA125 (U/ml) | 14.20 | | | | 0.00–35.00 |
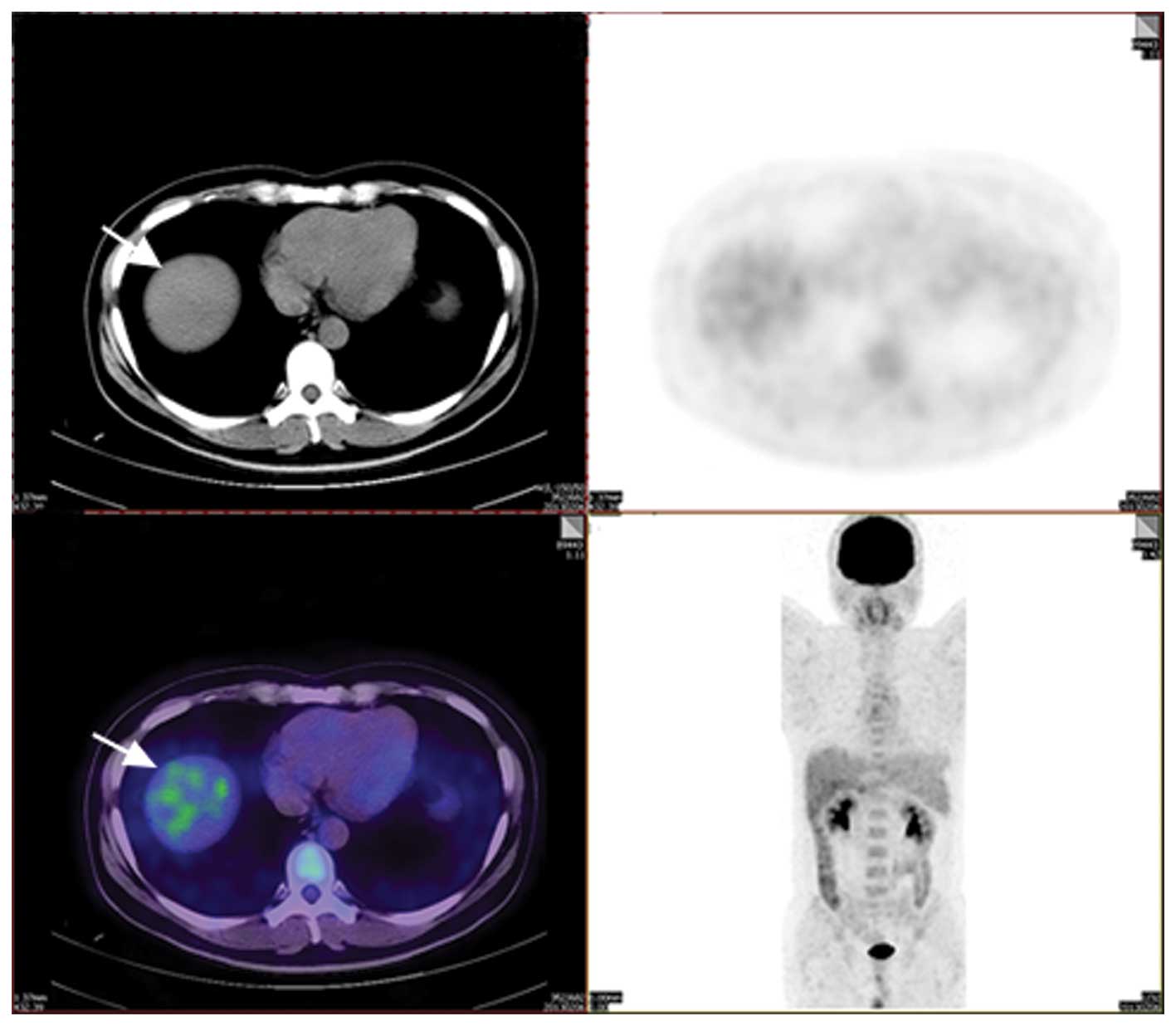
CT scans revealed a 1.3-cm well-defined tumor
located in segment eight of the liver (Fig. 1), with good enhancement in the
arterial and portal venous phases, multiple hypodense cysts in the
liver and calcified lymph nodes prior to segment five in the
abdominal cavity. The positron emission tomography (PET) study
revealed a tumor of low intensity (Fig.
2), multiple hypodense cysts and multiple gallbladder polyps.
Due to the age of the patient, the presence of a hepatic hypodense
lesion resembling a tumor and the high tumor marker levels, the
differential diagnosis comprised hepatocellular carcinoma, focal
nodular hyperplasia and hemangioma. To exclude hepatocellular
carcinoma, a typical hepatectomy was recommended to remove segment
eight of the liver and gall bladder.
Treatment
Exploratory laparotomy was performed on 18th
February 2013, and a dark red-colored soft tumor (1.7×1.5 cm in
diameter) in segment eight of the liver was revealed.
Intra-operative ultrasound examination was performed, which
identified no other lesions in the remaining sections of the liver.
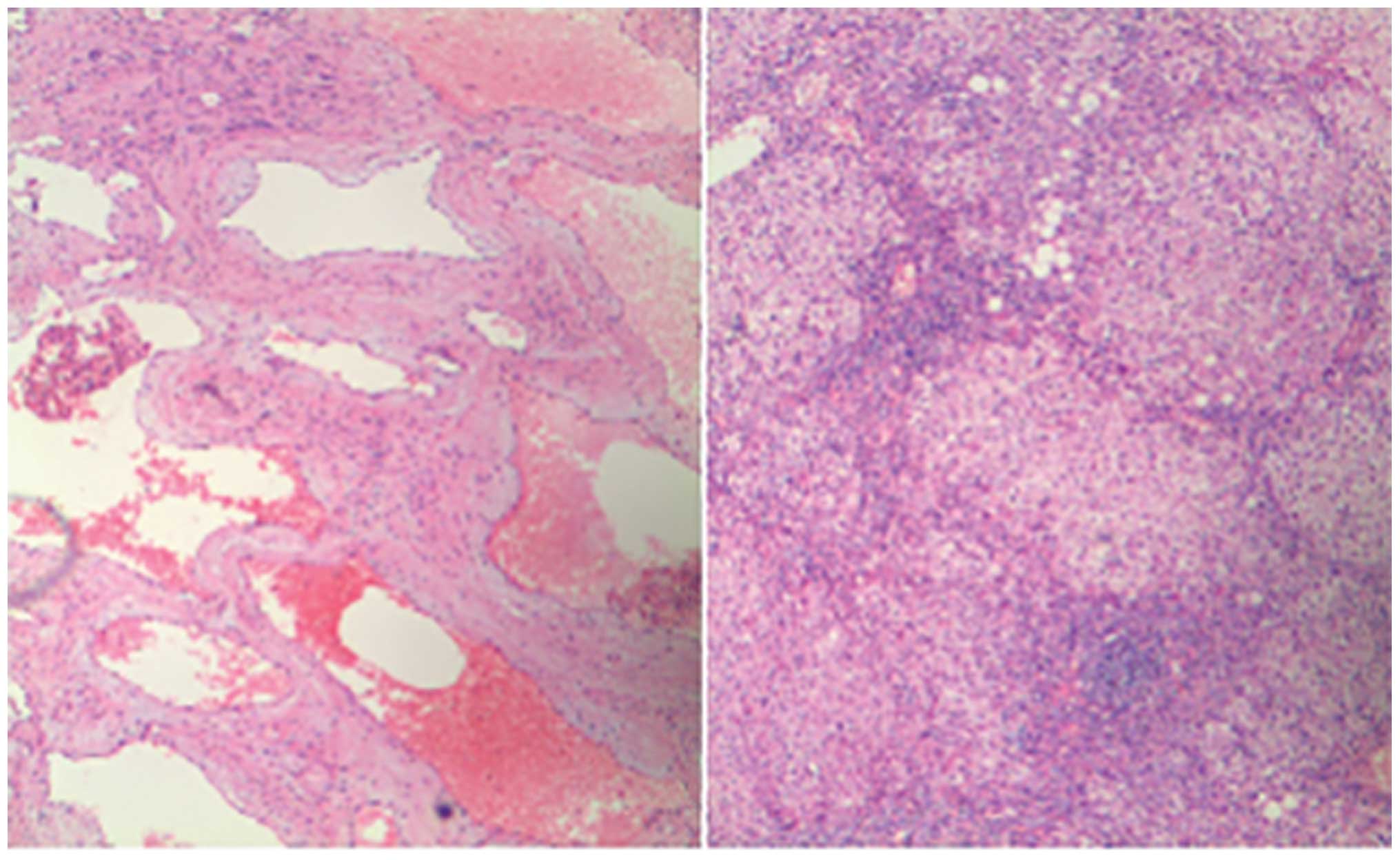
Intra-operative pathology and post-operative histopathology
examinations revealed that the tumor was a cavernous hemangioma of
the liver (Fig. 3). The serum AFP
level had decreased to 111 μg/l by post-operative day seven and to
24.45 μg/l by post-operative week two.
Discussion
Cavernous hemangioma is the most common hepatic
vascular tumor in adults (1).
However, the carcinoma biomarkers of hemangioma are usually within
the normal range (2,14,15).
The abdominal ultrasound examination and CT scan performed on the
present patient revealed a localized hepatic nodule with the
characteristics of hepatic hemangioma, while the highly elevated
AFP and CEA levels suggested HCC. However, the intra-operative
pathology and post-operative histopathology examinations revealed a
liver cavernous hemangioma. The literature was searched and only
three cases were found, one in English and the other two in Chinese
(14,15). All the patients in the previously
reported cases were Chinese, consisting of one male and two
females. All three cases were diagnosed following a routine health
examination and were negative for the hepatitis B surface antigen.
Their pre-operative AFP levels were 1890, 784 and 224 μg/l,
respectively, and returned to normal levels (0–20 μg/l) within four
weeks of the surgical removal of the tumor. The tumors were not
located in the same segments, but the three reported cases were all
>6.0 cm in diameter. The majority of cases occurred as a single
mass and were clinically asymptomatic. CT scans revealed all
reported cases to possess well-defined nodular lesions, with a good
enhancement in the arterial and venous phases following contrast
injection. All cases were diagnosed as hepatocellular carcinoma,
focal nodular hyperplasia or cavernous hemangioma prior to
pathological examination.
These studies suggest that the production of AFP
originates from hepatic hemangioma, implying that certain hepatic
cavernous hemangioma may possess the ability to synthesize and
secrete AFP. For the present patient, the serum AFP level decreased
rapidly following hepatectomy. With a 20-year history of chronic
hepatitis and an elevated level of tumor markers, the current case
prompts consideration of cancer stem cells, which exhibit distinct
proliferative and differentiative capacity (16). Although this patient possessed a
20-year history of chronic hepatitis B, which could be a possible
reason for elevated serum AFP, the existence of cancer stem cells
should not be excluded. According to certain studies into cancer
stem cells, it is likely that AFP, CEA and CA199 were produced by
cancer stem cells in the hemangioma during development (17–19).
The history of chronic hepatitis could concurrently promote the
appearance of hepatic cancer stem cells (20–22).
Once a liver lesion with elevated AFP level is
found, it is important to differentiate whether the liver lesion is
HCC or not. The treatment choice should be based on the nature and
extent of disease, so that surgery depends on the surgical risk and
the benefit.
In conclusion, clinicians should be aware that there
are certain tumors besides HCC and endodermal sinus tumors, such as
hepatic cavernous hemangioma, that may produce AFP in adults.
Acknowledgements
Financial support was provided for the present study
by the Program Sci-tech Research Development of Guangdong Province
(no. 2012B061700090), the Science and Technology Program of
Guangzhou (no. 201300000187) and the Science and Technology Program
of Huizhou Daya Bay (national) economic and technological
development zone (no. 2013A01016).
References
|
1
|
Ishak KG, Anthony PP, Niederau C and
Nakanuma Y: Mesenchymal tumours of the liver. World Health
Organization Classification of Tumors. Pathology and Genetics of
Tumours of the Digestive System. Hamilton SR and Aaltonen LA: IARC
Press; Lyon, France: pp. 191–198. 2000
|
|
2
|
Ball D, Rose E and Alpert E:
Alpha-fetoprotein levels in normal adults. Am J Med Sci.
303:157–159. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Abu El Makarem M: An overview of
biomarkers for the diagnosis of hepatocellular carcinoma. Hepat
Mon. 12:e61222012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yan D, He Q, Chen Y, Wang L and Zhang X:
Detection of α-fetoprotein and glypican-3 mRNAs in the peripheral
blood of hepatocellular carcinoma patients by using multiple
FQ-RT-PCR. J Clin Lab Anal. 25:113–117. 2011. View Article : Google Scholar
|
|
5
|
Liu C, Xiao GQ, Yan LN, et al: Value of
alpha-fetoprotein in association with clinicopathological features
of hepatocellular carcinoma. World J Gastroenterol. 19:1811–1819.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Biondi A, Malaguarnera G, Vacante M, et
al: Elevated serum levels of Chromogranin A in hepatocellular
carcinoma. BMC Surg. 12(Suppl 1): S72012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Miller RR, Champagne K and Murray RC:
Primary pulmonary germ cell tumor with blastomatous
differentiation. Chest. 106:1595–1596. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shimada H, Noie T, Ohashi M, Oba K and
Takahashi Y: Clinical significance of serum tumor markers for
gastric cancer: a systematic review of literature by the Task Force
of the Japanese Gastric Cancer Association. Gastric Cancer.
17:26–33. 2014. View Article : Google Scholar
|
|
9
|
Abdel-Rahman M, Saad Y, El-Raziky M, et
al: Hepatitis C genotype 4 with normal transaminases: Correlation
with fibrosis and response to treatment, a cohort Egyptian study of
4277 patients. Clin Res Hepatol Gastroenterol. 37:479–484. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wang L, Zhong Y, Sun L, et al: Clinical
and pathological features of hepatoid carcinoma of the ovary. World
J Surg Oncol. 11:292013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Tong HL, Dong ZN, Wen XY, et al: Impact of
chronic kidney disease on serum tumor markers concentrations. Chin
Med J (Engl). 126:274–279. 2013.
|
|
12
|
Valentino F, Torchio M, Morbini P and
Danova M: Synchronous presentation of hepatoid
alpha-fetoprotein-producing lung cancer and colorectal
adenocarcinoma. Tumori. 98:130e–134e. 2012.PubMed/NCBI
|
|
13
|
Paradies G, Zullino F, Orofino A and
Leggio S: Unusual presentation of sacrococcygeal teratomas and
associated malformations in children. Clinical experience and
review of the literature. Ann Ital Chir. 84:333–346. 2013.
|
|
14
|
Han SL, Wu XL, Jia ZR and Wang PF: Adult
hepatic cavernous haemangioma with highly elevated
alpha-fetoprotein. Hong Kong Med J. 16:400–402. 2010.PubMed/NCBI
|
|
15
|
Wang ZG, Ding FQ, Zhang AL and Liu GZ:
Hepatic hemangioma associated with AFP elevation: two case reports.
Qilu Zhongliu Zazhi. 4:1531997.(In Chinese).
|
|
16
|
Visvader JE and Lindeman GJ: Cancer stem
cells in solid tumours: accumulating evidence and unresolved
questions. Nat Rev Cancer. 8:755–768. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Stovold R, Blackhall F, Meredith S, et al:
Biomarkers for small cell lung cancer: neuroendocrine, epithelial
and circulating tumour cells. Lung Cancer. 76:263–268. 2012.
View Article : Google Scholar
|
|
18
|
Liu J, Zheng M, Tang YL, Liang XH and Yang
Q: MicroRNAs, an active and versatile group in cancers. Int J Oral
Sci. 3:165–175. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sasaki N, Ishii T, Kamimura R, et al:
Alpha-fetoprotein-producing pancreatic cancer cells possess cancer
stem cell characteristics. Cancer Lett. 308:152–161. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wang C, Yang W, Yan HX, et al: Hepatitis B
virus X (HBx) induces tumorigenicity of hepatic progenitor cells in
3,5-diethoxycarbonyl-1,4-dihydrocollidine-treated HBx transgenic
mice. Hepatology. 55:108–120. 2012. View Article : Google Scholar
|
|
21
|
Arzumanyan A, Friedman T, Ng IO, et al:
Does the hepatitis B antigen HBx promote the appearance of liver
cancer stem cells? Cancer Res. 71:3701–3708. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sun YL, Yin SY, Xie HY, et al: Stem-like
cells in hepatitis B virus-associated cirrhotic livers and adjacent
tissue to hepatocellular carcinomas possess the capacity of
tumorigenicity. J Gastroenterol Hepatol. 23:1280–1286. 2008.
View Article : Google Scholar : PubMed/NCBI
|