Introduction
Hemangioblastomas are tumors of the central nervous
system that most frequently arise from the vascular system; they
are classed as is WHO grade I tumors (1). In adults, 7–10% of tumors arise in the
posterior fossa (2) and the
cerebellum is the most common site of occurrence (3,4). As a
number of features may be observed on magnetic resonance imaging
(MRI), (1,3–6)
according to previous reports, cerebellar hemangioblastoma can be
predominantly divided into two categories on the basis of MRI
findings. The most common radiological presentation of cerebellar
hemangioblastoma is a large sac or cyst and small tumor nodules. We
hypothesize that this type may be further divided into two
subtypes: One which exhibits no enhancement at the wall of the
large cyst, but with evenly enhanced tumor nodules; and another
with an enhanced large cyst and tumor nodules. The less common type
of cerebellar hemangioblastoma is a solid mass, and also comprises
two subtypes: One type contains multiple solid tumors and exhibits
homogeneous enhancement on MRI; the other subtype is a solid tumor
with single or multiple cysts, where the solid portion is enhanced
and the cystic region is non-enhanced (7). In addition to the two main tumor
types, the rarest variant of this tumor exhibits an enhanced cyst
wall, based on the cystic nodules, and is accompanied by enhanced
uneven walls (6). The first type (a
large sac or cyst with small tumor nodules) has surrounding edema.
The other two types (one type is a solid mass, one type exhibits
enhanced cyst wall) exhibit an obvious mass and do not have
surrounding edema. However, in spite of these characteristic
features on imaging, in the preoperative and differential
diagnoses, solid cerebellar hemangioblastoma and nodular cerebellar
hemangioblastoma with enhanced wall are often misdiagnosed as
high-grade gliomas (6).
For cerebellar hemangioblastoma with an enhanced
cystic wall, surgical resection is the most effective treatment.
The tumor is unlikely to recur following complete resection,
therefore chemotherapy or radiotherapy is not usually required.
Cerebellar hemangioblastoma exhibits a good prognosis following
complete resection, with a five-year survival rate of >50%
(2). The current study presents two
cases of cerebellar hemangioblastoma, which both exhibited enhanced
wall thickness. Written informed consent was obtained from both
patients.
Case reports
Case one
A 66-year-old male, presented to the Department of
Neurosurgery, Tiantan Hospital, Capital Medical University
(Beijing, China) with the primary complaint of an intermittent
headache for four months, with two months of ataxia. Physical
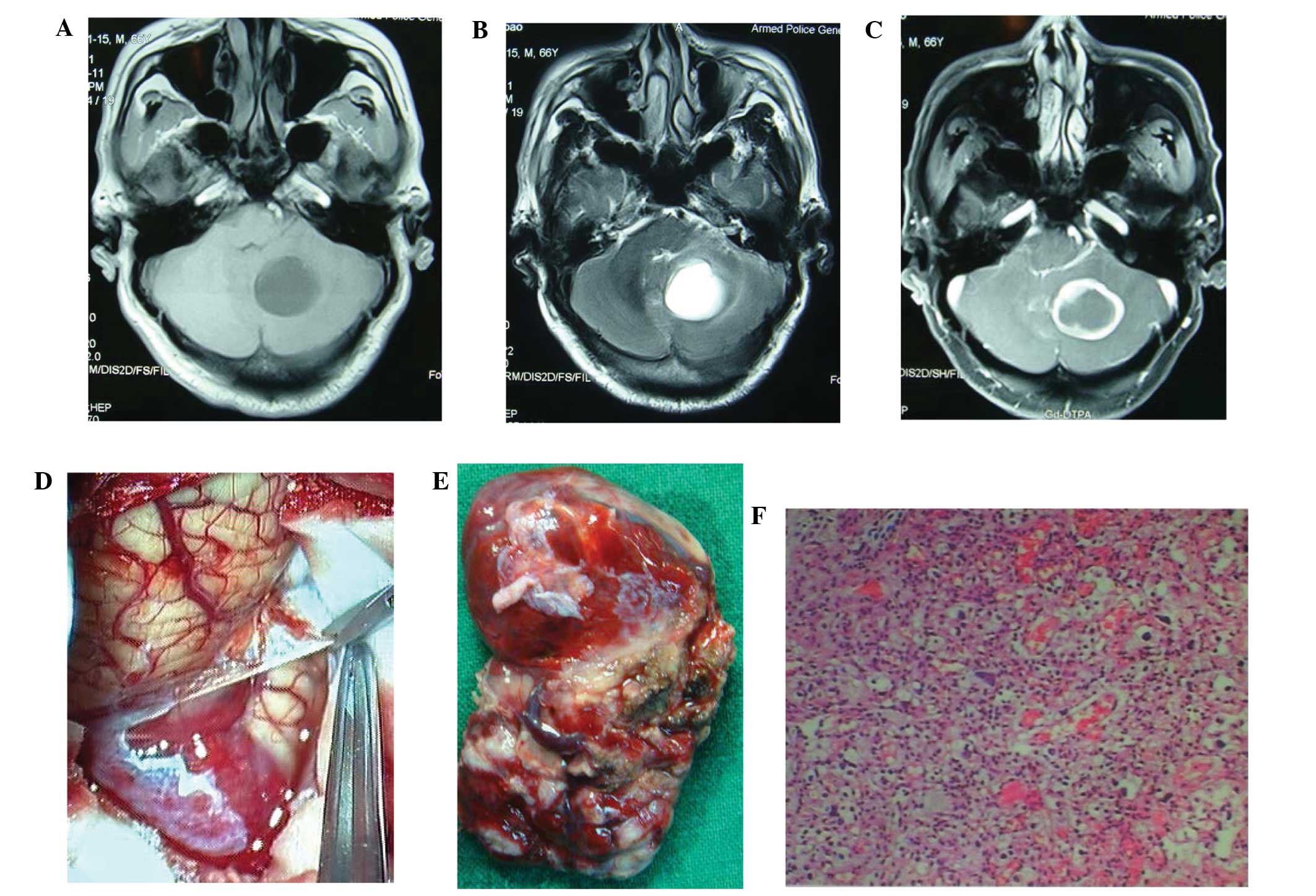
examination showed abnormal ataxia in the right extremities. MRI
revealed a cystic mass in the right cerebellar hemisphere. The mass
was hypointense on T1-weighted images, hyperintense on T2-weighted
images, and showed an enhanced solid portion on the wall of the
mass following the injection of
gadolinium-diethylenetriaminepentaacetate (Fig. 1A, B, C). The patient was treated
using the suboccipital approach under general anesthesia; two thick
draining veins were identified at the surface of the tumor with
multiple, thick feeding arteries surrounding the tumor, all of
which were closely adhered to the surrounding tissues. The tumor
boundary was clear, and the upper region, located in the brain
parenchyma, was cystic (Fig. 1D).
The cyst fluid was light yellow and transparent, with a volume of
~5 ml. After cutting the wall membrane, the cluster of red vasular
masses with abundant blood supply was evident. The tumor boundary
was separated by occluding the blood supply and blocking the
draining veins. The complete resected mass was ~2×3×3 cm size
(Fig. 1E). Hematoxylin and eosin
(HE) staining confirmed the diagnosis of hemangioblastoma (Fig. 1F). Postoperatively, the headache
completely regressed and the ataxia subsided. Follow-up was
conducted annually and three years after surgery the patient was
asymptomatic. At the time of writing the patient was well, with no
evidence of recurrence.
Case two
A 60-year-old male was admitted to the Department of
Neurosurgery, Tiantan Hospital, Capital Medical University, with
gait ataxia, headaches, nausea and vomiting for one month. Physical
examination showed abnormal ataxia in the left extremities with
gait ataxia. Subsequently, MRI revealed irregular long T1/T2
signals in the left cerebellar hemisphere and vermis, and enhanced
irregular nodular lesions without obvious edema (Fig. 2A, B, C). Surgery was performed to
remove the lesions, during which, a red, medium-texture, nodular
tumor with a rich blood supply was identified. The cyst fluid was
pale yellow with a volume of ~8 ml. For the complete resection of
the tumor, it was fully separated from the surrounding tissue. On
removal, the tumor measured 1.5×1×1 cm in size. As with the
previous case, HE staining confirmed the diagnosis of
hemangioblastoma (Fig. 2D). Two
years after surgery the patient was asymptomatic, with no evidence
of recurrence.
Discussion
Cerebellar hemangioblastoma is the most common form
of hemangioblastoma (3,4). Based on MRI findings, there are
several known types of this tumor. The most common type consists of
small nodular tumors on the side of a large cyst and the two rarer
types comprise a solid mass, or a lesion with an enhanced cyst wall
due to cystic nodules, which exhibits enhanced uneven walls on
imaging (2).
Surgical resection is the most effective treatment
for cerebellar hemangioblastomas with an enhanced cystic wall
(8). However, for this type of
lesion, the tumor must not be punctured, biopsied or blocked via
resection due to the rich blood supply. The enhanced tumor wall
indicates that it contains partial tumor cells, therefore to avoid
recurrence of the tumor, the wall and the solid part of the tumor
require total resection (9). This
type of tumor has a benign characteristic, and is generally located
in the brain parenchyma (9).
However, tumors may perforate the surface of the brain and
metastasize to the surrounding regions (10). Following complete resection, it is
unlikely that the tumor will recur, and therefore chemotherapy or
radiotherapy is not frequently required (9). Even in cases where residual tumors are
identified, only a small number of these tumors become
malignant.
According to our experience regarding surgical
procedures, in order to achieve separation of the lesion from the
surrounding tissue in the present cases, initially the feeding
artery was occluded until the surface tension decreased, and
subsequently the draining veins were blocked (11). The tumors were then resected
completely. Multiple feeding arteries are often present, as well as
more than one abnormally thick draining vein, with large diameters
and thick walls (9), which were
identified in the two patients of the present cases. Occasionally,
a localized flow and rich blood supply within the tumor is observed
and the color of intravenous blood is bright red (9), which occurred in the present cases.
However, caution must be taken not to block the draining veins
mistakenly based on the color of the blood, as this may result in
heavy bleeding due to the venous return obstruction.
In the present cases the tumors were resected
successfully. No subsequent treatment was required following
surgery, and a full recovery was achieved. After three years of
follow-up, the patients were asymptomatic and at the time of
writing, no recurrences had been identified. Continued follow-up of
the two patients has been planned. The limitations of the current
study included the small number of cases presented and the short
follow-up periods.
References
|
1
|
Lee JY, Cho BM, Oh SM, et al: Delayed
diagnosis of cerebellar hemangioblastoma after intracerebellar
hemorrhage. Surg Neurol. 67:419–421. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Aldape KD, Plate KH, Vortmeyer AO, et al:
Haemangioblastoma. WHO Classification of Tumours of the Nervous
System. Louis DN, Ohgaki H, Wiestler OD and Cavenee WK: IARC Press;
Lyon: 2007
|
|
3
|
Simone CB II, Russell RR, Ondos J, et al:
Infratentorial craniospinal irradiation for von Hippel-Lindau: a
retrospective study supporting a new treatment for patients with
CNS hemangioblastomas. Neuro Oncol. 13:1030–1036. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Horvathy DB, Hauck EF, Ogilvy CS, et al:
Complete preoperative embolization of hemangioblastoma vessels with
Onyx 18. J Clin Neurosci. 18:401–403. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gelabert González M: Posterior fossa
hemangioblastomas. Neurologia. 22:853–859. 2007.
|
|
6
|
Zhou LF and Du GH: Diagnosis and surgical
treatment of posterior fossa solid hemangilblastomas. Chin Med J.
113:129–132. 2000.
|
|
7
|
Wan JQ, Cui H and Wang Y: Surgical
management of large solid hemangioblastomas of the posterior fossa.
J Clin Neurosci. 18:39–42. 2011. View Article : Google Scholar
|
|
8
|
Neumann HP, Eggert HR, Weigel K, et al:
Hemangioblastomas of the central nervous system. A 10-year study
with special reference to von Hippel-Lindau syndrome. J Neurosurg.
70:24–30. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jito J and Nozaki K: Treatment strategies
for cerebellar hemangioblastomas: simple or further studies? World
Neurosurg. 82:619–620. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Liao CC and Huang YH: Clinical features
and surgical outcomes of sporadic cerebellar hemangioblastomas.
Clin Neurol Neurosurg. 125:160–165. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yan PX, Wang ZC, Yu CJ and Guan SS: The
diagnosis and microsurgical treatment of solid cerebellar
hemangioreticuloma. Zhonghua Wai Ke Za Zhi. 42:777–780. 2004.(In
Chinese). PubMed/NCBI
|