Introduction
Chronic kidney disease (CKD) is becoming a major
public health concern and is also highly prevalent in developing
countries (1,2). Recently, based on a report published in
the Lancet in 2012, China had a higher incidence and prevalence
rate of CKD, estimating the overall prevalence of CKD to be 10.8%
(3). The number of patients with CKD
in China is estimated to be ~119.5 million (4). The incidence of complications in the CKD
patients is increasing with the changes of lifestyle. Vascular
calcification (VC) is a frequent complication in patients with CKD
and directly or indirectly contributes to cardiovascular disease
and increased mortality rates (5,6). It is
reported that VC is an actively regulated progress. Apart from the
passive precipitation of calcium phosphate, the
transdifferentiation of vascular smooth muscle cells (VSMCs) into
osteoblast-like cells, as well as changes in the expression of
bone-associated and mineralization regulating proteins, and
apoptosis play critical roles in VC (7). However, the underlying pathophysiological
mechanisms are not well understood. It is proposed that along with
traditional cardiovascular risk factors, non-traditional risk
factors, such as those associated with uremic status and a
disturbed bone and mineral metabolism, are likely to control
whether or not VC occurs in patients with CKD (8).
Magnesium is involved in numerous important
enzymatic processes and also plays a role in skeletal and mineral
metabolism and vascular tone (9,10). Data from
observational clinical studies showed an inverse association
between serum magnesium concentrations and the presence of VC or
atherosclerosis (11,12). However, to date, only a limited number
of experimental studies performed in animals have confirmed these
findings, whereas the majority investigated the role of lowering
dietary magnesium on VC (13,14). Thus far, only 2 studies have reported
that magnesium has a favorable effect on bone matrix mineralization
in an in vitro model (15,16).
Therefore, the present study aimed to investigate whether
increasing magnesium concentrations influence calcification of rat
aortic vascular smooth muscle cells (RAVSMCs).
Materials and methods
Cell culture of RAVSMC
RAVSMCs were prepared as previously described with
minor modifications (17–19). Briefly, RAVSMCs were isolated from the
thoracic aorta of adult male Sprague-Dawley rats (80–100 g). After
the rats had been anaesthetized with chloral hydrate (400 mg/kg),
the thoracic aorta was obtained under aseptic conditions and cut
into small pieces following the removal of residual blood. Small
pieces of tissue (1–2 mm2) were placed in a culture dish
in Dulbecco's modified Eagle's medium (DMEM) supplemented with 15%
fetal bovine serum (FBS; HyClone Corp., Logan, UT, USA), 4.5 g
glucose, 100 U/ml penicillin and 100 µg/ml streptomycin in a 5%
CO2 incubator at 37°C. Cells that migrated from explants
were collected when confluent. The cells were maintained in DMEM
supplemented with 15% FBS, and the medium was replaced twice a
week. RAVSMCs were identified by the SMC typical hill and valley
appearance, and immunocytochemistry using a monoclonal antibody
against the α-smooth muscle actin protein 1A4 (Acta 2) (Santa Cruz
Biotechnology, Inc., Dallas, TX, USA) further confirmed the purity
of the primary cell culture (20). The
cells between passages 6 and 12 were used in all the
experiments.
Calcification assays
RAVSMC calcification was induced as previously
described (21). VSMCs were randomly
divided into a negative control group, high phosphorus and
magnesium intervention groups, a negative control group using low
glucose DMEM medium containing 10% FBS and a high phosphorus group
in which 10 mM β-glycerophosphate (BGP) was added to normal medium
to generate high phosphorus medium. Magnesium chloride was added to
the medium for the magnesium intervention groups on the basis of
high phosphorus; the final concentrations of magnesium ions
(Mg2+) were 11, 2 and 3 mM (magnesium intervention
groups 1, 2 and 3, respectively), and the stimulating time was 7
days. Control medium was prepared equally but without BGP. The
medium was replaced twice a week and Mg2+ was added from
the beginning and at each medium renewal of the experiment.
Supernatants were collected for further investigations.
For precise biochemical Ca2+
measurements, calcium content in the supernatant was extracted with
6 N hydrochloric acid overnight. The o-cresolphthalein
complexone method was conducted using a Calcium Assay kit (BioSino
Biotechnology, Beijing, China) and normalized to the protein
content of the same culture.
For alizarin red staining (AR), cells were washed
twice with phosphate-buffered saline (PBS) and fixed with ethanol
95%. Subsequently, the samples were exposed to 40 mM AR (pH 4.2).
Following two washing steps, images were captured of the wells to
show the presence of induced mineralization.
Assay of alkaline phosphatase (ALP)
activity
Cells were plated at a density of 2×105
cells/well into 24-well plates. The cells were cultured for 7 days
after intervention and rinsed 3 times with PBS. Subsequently, 500
µl of 0.1% Triton X-100 was added to each well and incubated for
12–24 h at 4°C. The protein assay was performed with the
bicinchoninic acid protein assay reagent (Sigma, St. Louis, MO,
USA). ALP activity was assayed by a method modified from that of
Lowry et al (22). In brief,
the assay mixtures contained 0.1 M 2-amino-2-methyl-1-propanol, 1
mM MgCl2, 8 mM p-nitrophenyl phosphate disodium
and the cell homogenates. After incubation for 4 min at 37°C, the
reaction was stopped with 0.1 N NaOH and the absorbance was read at
405 nm. Each value was expressed as p-nitrophenol produced in
nanomoles/min/microgram of protein.
RNA extraction and reverse
transcription-polymerase chain reaction (RT-PCR)
RT-PCR was performed to determine the expression
levels of the target gene, Cbfα1. Total RNA was extracted
from cultured cells using TRIzol reagent (Invitrogen Life
Technologies, Grand Island, NY, USA) according to the
manufacturer's instructions. cDNA was synthesized using the
advantage RT-for-PCR kit (Clontech, Palo Alto, CA, USA) with oligo
(dT) priming according to the manufacturer's instructions. The
GAPDH gene was used as the endogenous control. The primers
for Cbfα1 were: 5′-CCGCACGACAACCGCACCAT-3′ (sense) and
5′-CGCTCCGGCCCACAAATCTC-3′ (antisense). The primers for
GAPDH were 5′-CAAGGTCATCCATGACAACTTTG-3′ (sense),
5′-GTCCACCACCCTGTTGCTGTAG-3 (antisense). The generated PCR products
were 289-bp for Cbfα1 and 496-bp for GAPDH. The PCR
condition consisted of one incubation for 2 min at 95°C, followed
by 35 cycles of a 30-sec denaturation at 95°C, a 30-sec annealing
at 55°C and a 45-sec extension at 72°C, and a final extension at
72°C for 5 min. The PCR products were tested in 1% agarose gel in
electrophoresis, visualized with ethidium bromide staining and
quantified using an image analysis system (Gel work-2ID; Cell
Signaling Technology, Shanghai, China). The optical density value
of the mRNA expression was calculated.
Statistical analysis
Each experiment was repeated independently 3 times
and all the data are expressed as mean ± standard deviation. Means
were compared by the Student's t-test. Means between multiple
groups were performed using the analysis of variance (ANOVA).
Intergroup comparison was made using ANOVA and the
Student-Newman-Keuls test. All the statistical analyses were
performed using the SPSS 17.0 software (SPSS, Inc., Chicago, IL,
USA). For all the statistical tests, P<0.05 was considered to
indicate a statistically significant difference.
Results
Effects of BGP on calcium content of
cultured RAVSMCs
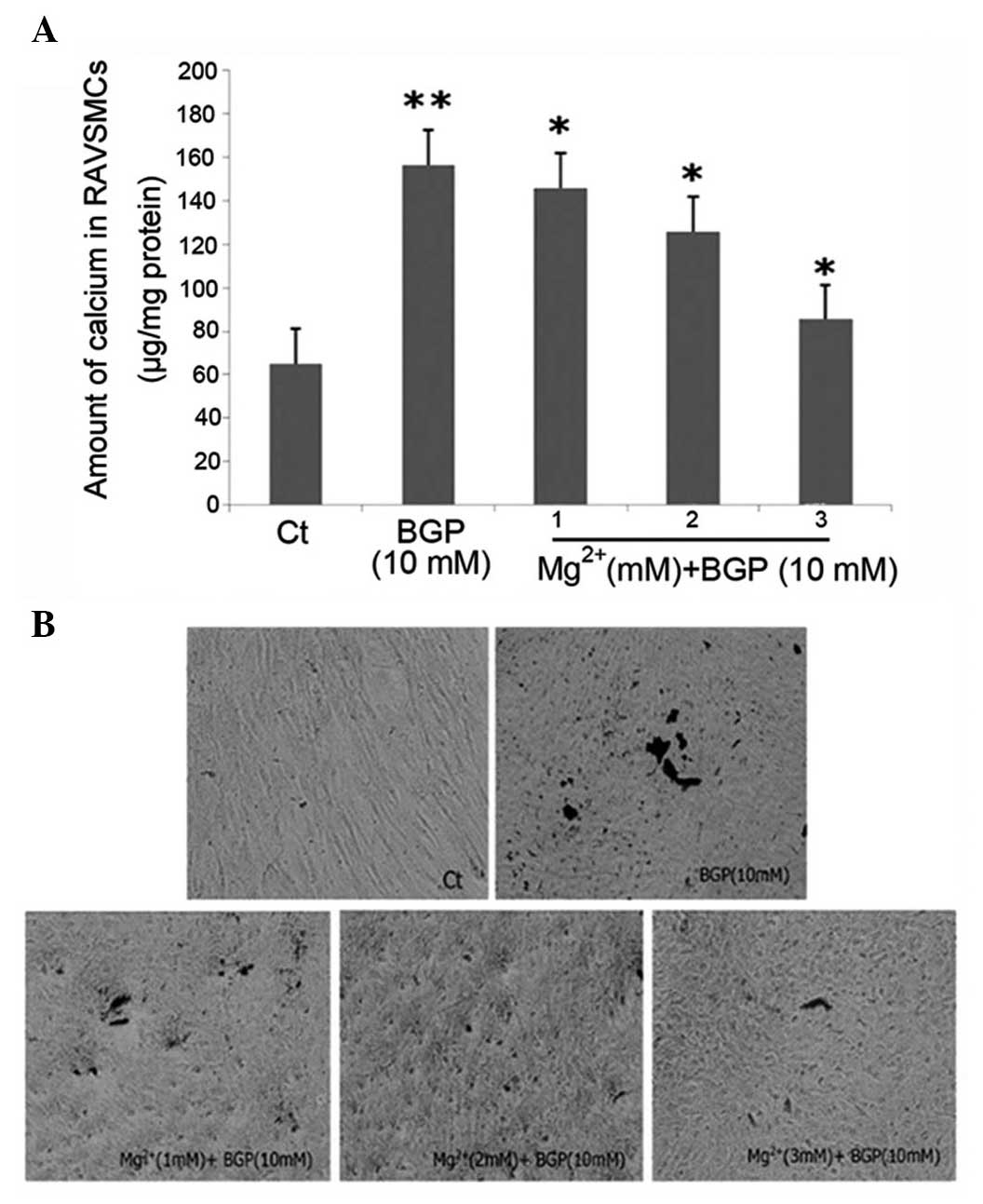
Biochemical Ca2+ measurements were
performed on day 7 after the intervention with various media
conditions. The calcium content of the BGP group was significantly
higher than those of the control group (Fig. 1A).
Mg2+ inhibits BGP-induced
calcification in RAVSMCs
To investigate the effects of different
Mg2+ concentrations on VC, the calcium content was
measured of the cells incubated with the indicated conditions. AR
staining was also performed on day 7 to further confirm the
occurrence of calcium/phosphate (Ca/P) deposition. In the presence
of 10 mM BGP disodium, Mg2+ at a total concentration of
1, 2 and 3 mM in the medium was effective to significantly inhibit
the calcium content on day 7. After 7 days of intervention,
Mg2+ decreased the calcium content significantly in a
dose-dependent manner (Fig. 1A). The
effect of Mg2+ was evident at 1 mM, and became clearer
as the concentration increased and reached the maximum at 3 mM. In
addition to the biochemical analysis, Ca/P deposits were also
identified by AR staining (Fig. 1B).
The size and amount of the granular calcified formations appear to
decrease with the addition of Mg2+ in a dose-dependent
manner.
Effects of Mg2+ on Cbfα1
expression and activity of ALP in RAVSMCs
To further validate the effects of Mg2+
on the differentiation of RAVSMCs, the gene expression associated
with osteoblast differentiation was examined on day 7 after
intervention of Mg2+ by RT-PCR. RT-PCR showed that the
mRNA expression of Cbfα1 was downregulated following
intervention with 1, 2 and 3 mM Mg2+ (P<0.05)
(Fig. 2). After 7 days of
intervention, the ALP activity of the BGP group was significantly
higher than those of the control group (P<0.05). Mg2+
decreased the activity of ALP significantly in a dose-dependent
manner (Fig. 3). The effect of
Mg2+ was evident at 1 mM, became clearer as the
concentration increased and reached the maximum at 3 mM. These data
demonstrated that Mg2+ plays an important role in
preventing BGP-induced calcification in RAVSMCs
Discussion
Results obtained from previous clinical studies have
indicated that lower magnesium levels are associated with increased
VC in uremic and non-uremic conditions, and higher serum magnesium
results in a decreased risk of peripheral VC in non-diabetic
haemodialysis patients (13,23–26).
Furthermore, magnesium supplementation improved the media thickness
in patients on hemodialysis (12).
Notably, the dietary magnesium level influenced the ectopic
mineralization in an animal model, which may have broader
implications (13,27). However, the detailed mechanisms by
which magnesium acts on VC were not clear and the relevant studies
were few and limited. The aim of the present study was to provide
in vitro evidence for the preventive effect of magnesium on
calcification in a cell culture model of RAVSMCs.
Magnesium is the second most abundant intracellular
divalent cation and functions as an allosteric modulator of several
enzymes, or bridges structurally distinct molecules (28). Previous clinical studies showed that a
low magnesium status has an important role in the pathogenesis of
cardiovascular disease (29),
hypertension (30) and thrombosis
(6) in subjects without kidney
disease. In the present experimental model, BGP-induced
calcification was strongly inhibited by increasing magnesium
concentrations in the media of RAVSMCs in a dose-dependent manner
and was stable over a period of ≤7 days. Increasing magnesium
concentrations decreased calcium deposition, providing evidence
that magnesium is able to impair hydroxyapatite crystal growth in
in vitro experiments, which is in agreement with the
previous studies. It has been suggested that the effect of
magnesium on VC may be mediated via this mechanism (31–33). The
present study also found that magnesium was not only able to
prevent RAVSMC calcification but also inhibit progression of
already established calcification. Even partly reverted
calcification was observed with longer incubation time, which
renewed the attraction in the therapeutic applications of magnesium
on VC. Although phosphate binders are administered to patients of
CKD in order to lower serum phosphorus concentrations, as one
aspect of VC development, VC progressed overtime. Therefore,
magnesium administration or magnesium-containing phosphate binder
supplementation in CKD patients may be beneficial as it may
partially revert or at least inhibit the progression of VC.
VC is an active, cell-mediated multistep process
that includes apoptosis, and the osteochondrogenic differentiation
of VSMCs is similar to bone formation, with the role of deposition
of calcium-phosphate in terms of matrix mineralization (7,8,34). The bone-related factors, particularly
the specific osteogenic transcription factor Cbfα1, were shown to
be upregulated in VSMCs undergoing BGP-induced transdifferentiation
into osteoblast-like cells. Factors such as ALP, which may
contribute to the mineralization process, were also upregulated by
elevated phosphate concentrations in in vitro models
(35). In the present study, high
phosphorus induced the enhanced expression of Ca2+
content, Cbfα1 and ALP, while these decreased when
administrated with higher magnesium levels, clearly showing that
the protective effect of magnesium on RAVSMCs calcification by not
only decreasing the deposition of calcium in the cells but also
affecting the osteogenic transdifferentiation. However, it appears
unlikely, that the inhibitory effect of magnesium on calcification
will also account in the bone, as it has been shown that the
physiological magnesium concentrations present in bone are not able
to inhibit crystal growth (32). The
present study suggests that magnesium inhibits the pathological
transdifferentiation process from VSMCs into osteoblast-like cells,
which does not occur in the physiological process of calcification
in the bone. However, detailed clinical investigations regarding
the effect of magnesium on bone metabolism, specifically in renal
failure patients, are rare and (24)
contradictory (36,37). Well designed in vitro and
clinical studies to further evaluate the influence of magnesium on
bone are required.
In conclusion, higher magnesium levels prevented
calcification and further progression of already established
calcification in RAVSMCs. Increased magnesium concentrations not
only reduced the deposition of calcium, but also inhibited
osteogenic transdifferentiation, which are consistent with
experimental animal studies and with clinical studies linking
elevated magnesium levels to beneficial effects on VC (11,26,38). However, the detailed mechanism by which
magnesium may influence this process is unclear. Thus, it appears
to be that magnesium influences the molecular processes associated
with VC, providing an important insight into the clinical
application of magnesium. More clinical research is required to
observe the serum magnesium levels in patients with renal failure
and to confirm a possible protective effect of magnesium against
VC. There is a large gap concerning controlled interventional
studies providing unchallengeable results to improve the
understanding of its role.
Acknowledgements
The present study was supported by the project of
the Hebei Natural Science Fund (grant no. H2012206157) and the
project of the Hebei Major Medical Science (grant no.
GL2011-51).
References
|
1
|
Nugent RA, Fathima SF, Feigl AB and Chyung
D: The burden of chronic kidney disease on developing nations: A
21st century challenge in global health. Nephron Clin Pract.
118:c269–c277. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Eknoyan G, Lameire N, Barsoum R, Eckardt
KU, Levin A, Levin N, Locatelli F, MacLeod A, Vanholder R, Walker
R, et al: The burden of kidney disease: Improving global outcomes.
Kidney Int. 66:1310–1314. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yano Y, Fujimoto S, Asahi K and Watanabe
T: Prevalence of chronic kidney disease in China. Lancet.
380:213–216. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Liu ZH: Nephrology in China. Nat Rev
Nephrol. 9:523–528. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Blacher J, Guerin AP, Pannier B, Marchais
SJ and London GM: Arterial calcifications, arterial stiffness and
cardiovascular risk in end-stage renal disease. Hypertension.
38:938–942. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Goodman WG, Goldin J, Kuizon BD, Yoon C,
Gales B, Sider D, Wang Y, Chung J, Emerick A, Greaser L, et al:
Coronary-artery calcification in young adults with end-stage renal
disease who are undergoing dialysis. N Engl J Med. 342:1478–1483.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cozzolino M, Missaglia E, Ortiz A, Bellasi
A, Adragao T, Apostolous T, Vescovo G and Gallieni M: Vascular
calcification in chronic kidney disease. Recenti Prog Med.
101:442–452. 2010.(In Italian). PubMed/NCBI
|
|
8
|
Moe SM and Chen NX: Pathophysiology of
vascular calcification in chronic kidney disease. Circ Res.
95:560–567. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Spiegel DM: Magnesium in chronic kidney
disease: Unanswered questions. Blood Purif. 31:172–176. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
M de Francisco AL and Rodriguez M:
Magnesium - its role in CKD. Nefrologia. 33:389–399.
2013.PubMed/NCBI
|
|
11
|
Ishimura E, Okuno S, Kitatani K, Tsuchida
T, Yamakawa T, Shioi A, Inaba M and Nishizawa Y: Significant
association between the presence of peripheral vascular
calcification and lower serum magnesium in hemodialysis patients.
Clin Nephrol. 68:222–227. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Turgut F, Kanbay M, Metin MR, Uz E, Akcay
A and Covic A: Magnesium supplementation helps to improve carotid
intima media thickness in patients on hemodialysis. Int Urol
Nephrol. 40:1075–1082. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
van den Broek FA and Beynen AC: The
influence of dietary phosphorus and magnesium concentrations on the
calcium content of heart and kidneys of DBA/2 and NMRI mice. Lab
Anim. 32:483–491. 1998. View Article : Google Scholar
|
|
14
|
Planells E, Llopis J, Perán F and Aranda
P: Changes in tissue calcium and phosphorus content and plasma
concentrations of parathyroid hormone and calcitonin after
long-term magnesium deficiency in rats. J Am Coll Nutr. 14:292–298.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Nakatani S, Mano H, Ryanghyok IM, Shimizu
J and Wada M: Excess magnesium inhibits excess calcium-induced
matrix-mineralization and production of matrix gla protein (MGP) by
ATDC5 cells. Biochem Biophys Res Commun. 348:1157–1162. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kircelli F, Peter ME, Sevinc Ok E, Celenk
FG, Yilmaz M, Steppan S, Asci G, Ok E and Passlick-Deetjen J:
Magnesium reduces calcification in bovine vascular smooth muscle
cells in a dose-dependent manner. Nephrol Dial Transplant.
27:514–521. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Jeong IK, Oh H, Park SJ, Kang JH, Kim S,
Lee MS, Kim MJ, Hwang YC, Ahn KJ, Chung HY, et al: Inhibition of
NF-κB prevents high glucose-induced proliferation and plasminogen
activator inhibitor-1 expression in vascular smooth muscle cells.
Exp Mol Med. 43:684–692. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhai K, Hubert F, Nicolas V, Ji G,
Fischmeister R and Leblais V: β-Adrenergic cAMP signals are
predominantly regulated by phosphodiesterase type 4 in cultured
adult rat aortic smooth muscle cells. PLoS One. 7:e478262012.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wang HY, Huang RP, Han P, Xue DB, Li HB,
Liu B, Shan P, Wang QS, Li KS and Li HL: The effects of artemisinin
on the proliferation and apoptosis of vascular smooth muscle cells
of rats. Cell Biochem Funct. 32:201–208. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Skalli O, Pelte MF, Peclet MC, Gabbiani G,
Gugliotta P, Bussolati G, Ravazzola M and Orci L: Alpha-smooth
muscle actin, a differentiation marker of smooth muscle cells, is
present in microfilamentous bundles of pericytes. J Histochem
Cytochem. 37:315–321. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chen NX, O'Neill KD, Duan D and Moe SM:
Phosphorus and uremic serum up-regulate osteopontin expression in
vascular smooth muscle cells. Kidney Int. 62:1724–1731. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lowry OH, Roberts NR, Wu ML, Hixon WS and
Crawford EJ: The quantitative histochemistry of brain. II. Enzyme
measurements. J Biol Chem. 207:19–37. 1954.PubMed/NCBI
|
|
23
|
Shioi A, Nishizawa Y, Jono S, Koyama H,
Hosoi M and Morii H: Beta-glycerophosphate accelerates
calcification in cultured bovine vascular smooth muscle cells.
Arterioscler Thromb Vasc Biol. 15:2003–2009. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Meema HE, Oreopoulos DG and Rapoport A:
Serum magnesium level and arterial calcification in end-stage renal
disease. Kidney Int. 32:388–394. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Tzanakis I, Pras A, Kounali D, Mamali V,
Kartsonakis V, Mayopoulou-Symvoulidou D and Kallivretakis N: Mitral
annular calcifications in haemodialysis patients: A possible
protective role of magnesium. Nephrol Dial Transplant.
12:2036–2037. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Tzanakis I, Virvidakis K, Tsomi A,
Mantakas E, Girousis N, Karefyllakis N, Papadaki A, Kallivretakis N
and Mountokalakis T: Intra- and extracellular magnesium levels and
atheromatosis in haemodialysis patients. Magnes Res. 17:102–108.
2004.PubMed/NCBI
|
|
27
|
LaRusso J, Li Q, Jiang Q and Uitto J:
Elevated dietary magnesium prevents connective tissue
mineralization in a mouse model of pseudoxanthoma elasticum
(Abcc6(–/–)). J Invest Dermatol. 129:1388–1394. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Wolf FI and Cittadini A: Magnesium in cell
proliferation and differentiation. Front Biosci. 4:D607–D617. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Liao F, Folsom AR and Brancati FL: Is low
magnesium concentration a risk factor for coronary heart disease?
The Atherosclerosis Risk in Communities (ARIC) Study. Am Heart J.
136:480–490. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Peacock JM, Folsom AR, Arnett DK, Eckfeldt
JH and Szklo M: Relationship of serum and dietary magnesium to
incident hypertension: The Atherosclerosis Risk in Communities
(ARIC) Study. Ann Epidemiol. 9:159–165. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ennever J and Vogel JJ: Magnesium
inhibition of apatite nucleation by proteolipid. J Dent Res.
60:838–841. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Blumenthal NC and Posner AS:
Hydroxyapatite: Mechanism of formation and properties. Calcif
Tissue Res. 13:235–243. 1973. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Boskey AL and Posner AS: Effect of
magnesium on lipid-induced calcification: An in vitro model for
bone mineralization. Calcif Tissue Int. 32:139–143. 1980.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Reynolds JL, Joannides AJ, Skepper JN,
McNair R, Schurgers LJ, Proudfoot D, Jahnen-Dechent W, Weissberg PL
and Shanahan CM: Human vascular smooth muscle cells undergo
vesicle-mediated calcification in response to changes in
extracellular calcium and phosphate concentrations: A potential
mechanism for accelerated vascular calcification in ESRD. J Am Soc
Nephrol. 15:2857–2867. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Steitz SA, Speer MY, Curinga G, Yang HY,
Haynes P, Aebersold R, Schinke T, Karsenty G and Giachelli CM:
Smooth muscle cell phenotypic transition associated with
calcification: Upregulation of Cbfa1 and downregulation of smooth
muscle lineage markers. Circ Res. 89:1147–1154. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Gonella M, Ballanti P, Della Rocca C,
Calabrese G, Pratesi G, Vagelli G, Mazzotta A and Bonucci E:
Improved bone morphology by normalizing serum magnesium in
chronically hemodialyzed patients. Miner Electrolyte Metab.
14:240–245. 1988.PubMed/NCBI
|
|
37
|
Morinière P, Vinatier I, Westeel PF,
Cohemsolal M, Belbrik S, Abdulmassih Z, Hocine C, Marie A, Leflon
P, Roche D, et al: Magnesium hydroxide as a complementary
aluminium-free phosphate binder to moderate doses of oral calcium
in uraemic patients on chronic haemodialysis: Lack of deleterious
effect on bone mineralisation. Nephrol Dial Transplant. 3:651–656.
1988.PubMed/NCBI
|
|
38
|
Adamopoulos C, Pitt B, Sui X, Love TE,
Zannad F and Ahmed A: Low serum magnesium and cardiovascular
mortality in chronic heart failure: A propensity-matched study. Int
J Cardiol. 136:270–277. 2009. View Article : Google Scholar : PubMed/NCBI
|