Introduction
Surgery is one of the standard therapies for
numerous thyroid diseases. A total of 80,000 thyroidectomies per
year are performed in the United States alone (1). The thyroid is the highly vascularized
gland and hemostasis is one of the key limiting factors in
morbidity and mortality in thyroid surgery. Similar to bleeding,
other possible sources of postoperative morbidity include dysphonia
and dysphagia due to recurrent and/or superior laryngeal nerve
injury, hypocalcaemia due to parathyroid ischemia or unintended
deprivation, postsurgical hemorrhage, wound infection and
postoperative pain. However, the risk of perioperative mortality or
major disability is extremely low (2–5).
New vessel-sealing systems, including electrothermal
bipolar-activated devices [such as LigaSure® (LS)] or
ultrasonic systems [such as UltraCision® or Harmonic
Focus® devices (HS)] have been applied to thyroid
surgery in recent years. The aim was to reduce blood loss, surgical
time and length of skin incision. The LS obliterate the lumen by
creating a seal using a combination of pressure and electrothermal
energy to change the vessel wall structure (6). The HS simultaneously cut and seal vessels
by denaturing and coagulating collagen fibers, using mechanical
energy such as ultrasound (7).
Numerous randomized controlled trials (RCTs) have been testing
these two types of devices since 2000. Several reviews exist that
evaluate the possible superiority of each individual device in
thyroid surgery (8–14). Each exhibited its own limitations;
particularly when regarding comparisons made and completeness of
evidence. Furthermore, a meta-analysis comparing these two
techniques is limited, which made an updated systematic review of
the literature desirable.
The aim of the present meta-analysis was to perform
a comparison between HS and LS to assess surgical time,
postoperative complications and other parameters in thyroid
surgery.
Materials and methods
Meta-analyses principles
The meta-analysis was conducted by adhering to the
principles of ‘Preferred Reporting Items for Systematic Reviews and
Meta-Analyses’ statement (15,16).
Search strategy
Three individual investigators (AU, TH and ZM)
searched the electronic databases according to the standards of the
Cochrane collaboration. The following databases were searched:
MEDLINE, Cochrane Library, EMBASE and ISI Web of Science. No
language or time-period limitations were applied. The search was
carried out in March 2015. An update on December 2015 yielded no
new studies. All the relevant studies were scanned, and all
additional studies of potential interest were also retrieved.
Experienced thyroid surgeons were consulted to ensure that all
relevant studies were included.
Eligibility criteria
RCTs that compared the following two hemostasis
techniques in open partial and/or total thyroidectomy were included
for analysis: Ultrasonic systems (UltraCision®, Harmonic
Ace®, FOCUSTM; Ehticon Endosurgery Inc., Cincinnati, OH,
USA; Harmonic Focus®; Ethicon, Somerville, NJ, USA; or
related systems; HS) and electrothermal bipolar-activated vessel
sealing systems (Ligasure Vessel Sealing System®,
LigaSure® Precise, LigaSure Atlas LS1020, LigaSure™
LF1212; Valleylab Inc., Covidien, Boulder, CO, USA; or unspecified
LigaSure instruments; LS). RCTs assessing methods for minimally
invasive or video-assisted surgery were excluded. Eligibility was
assessed for each study by two investigators (AU and TH). Any
disagreement was resolved by a third investigator following
discussion.
Data extraction
A standardized electronic extraction sheet was used
to extract the data. The primary outcome parameter was total
surgical time. Secondary outcome parameters were as follows:
Surgical bleeding, postoperative bleeding, length of hospital stay,
thyroid weight and serum calcium level. In one study the serum
calcium level was reported in mg/dl, which was converted to
mmol/l.
From each eligible RCT, the following baseline
characteristics were compiled in the database: Study name,
publication year, journal reference, country, study design
(randomization, allocation concealment and blinding), sample size,
baseline data such as age, gender and interventions (intervention
groups and surgical experience).
Quality assessment
The risk of bias and quality in each eligible study
was assessed by Cochrane's risk of bias tool, including the
following 7 areas: Random sequence generation, allocation
concealment, blinding of participants and personnel, blinding of
outcome assessment, incomplete outcome data, selective reporting
and other biases (17,18). Investigators independently assessed the
risk of bias in each eligible trial, and a final consensus was
reached. A risk of bias graph was drawn, and risk of bias summary
was compiled.
Statistical analysis
Statistical analysis was performed and forest plots
were generated using the Review Manager software (version 5.3; The
Nordic Cochrane Centre, Copenhagen, Denmark). Total surgical time,
amount of intraoperative blood loss, postoperative blood loss,
duration of postoperative hospital stay, thyroid weight, serum
calcium level and the effective size of each trial were assessed by
the mean difference (MD) between treatment groups, and pooled as
the weighted mean difference (WMD) with 95% confidence interval
(CI) using the inverse variance method. Statistical heterogeneity
was tested by using χ2 and I2 tests. When
heterogeneity was high (I2 >50%), the random effect
model was used; otherwise, the fixed effect model was applied.
P<0.05 was considered to indicate a statistically significant
difference. The methods by Hozo et al (19) were used to convert median and range
estimates into mean and standard deviation.
Results
Studies included in the
meta-analyses
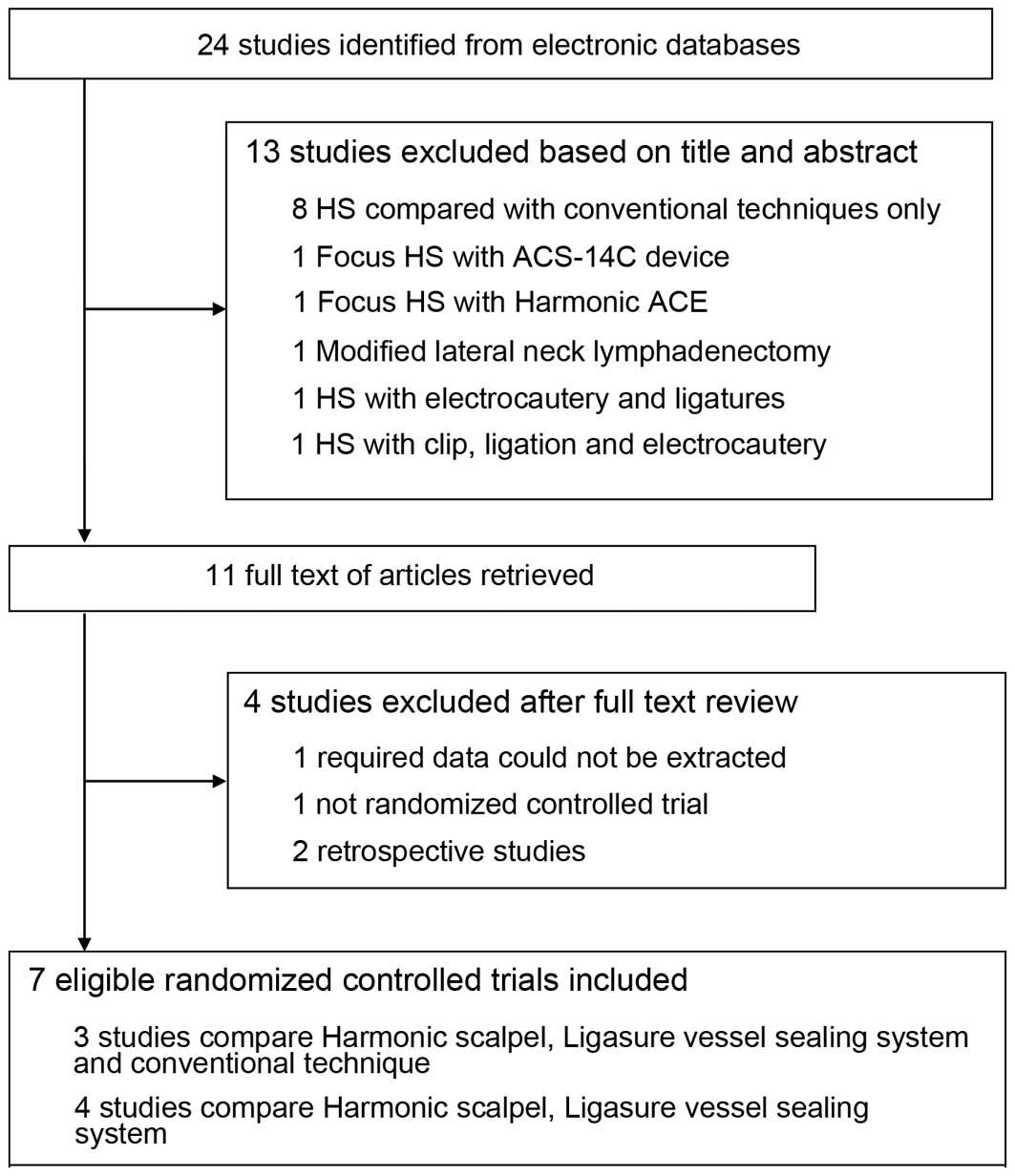
The electronic literature searches identified 24
potential studies, of which 13 were excluded on the basis of
abstract or title. Eleven full-text studies were retrieved.
Following further careful scrutiny, 4 were excluded as they did not
match the criteria. Seven were considered eligible according to the
inclusion criteria (20–26). The detailed search procedure is
presented in Fig. 1. Baseline
characteristics of the included trials and patients are presented
in Tables I and II. There were a total of 981 patients, with
492 in the HS group and 489 in the LS group.
 | Table I.Characteristics of the eligible
randomized controlled trials. |
Table I.
Characteristics of the eligible
randomized controlled trials.
| First author,
year | Country | Recruitment
time | Interventions | Control | Surgical
experience | Primary
endpoint | Power analysis and
sample size | Refs. |
|---|
| Bove, 2010 | Italy | 2010 | HF and LS | TT | Expert
surgeons | Surgical time | No | (26) |
| Dionigi, 2012 | Italy | 2011–2012 | HF | LS | Senior
surgeons | Surgical time | Yes | (25) |
| Dionigi, 2013 | Italy | 2012 | HF | LSP | Surgeons familiar
with the two devices | iPTH and serum
calcium level | Yes | (24) |
| Kwak, 2014 | South Korea | 2013–2014 | HAS | LSP | Single endocrine
surgeon | Surgical time | Yes | (23) |
| Pons, 2009 | France | 2009 | HS and LS | CH | Not mentioned | Surgical time | Yes | (22) |
| Rahbari, 2011 | USA | 2010–2011 | HF | LSP | Not mentioned | Surgical time | Yes | (21) |
| Sartori, 2008 | Italy | 2008 | HS and LS | CT | Surgical team
dedicated to endocrine surgery | Surgical time | No | (20) |
 | Table II.Baseline characteristics of the
included patients. |
Table II.
Baseline characteristics of the
included patients.
| First author,
year | Groups | Cases, n | Men, n | Women, n | Mean age ± SD,
years | Mean surgical time
± SD, min | Refs. |
|---|
| Bove, 2010 | HF | 25 | 6 | 19 |
50.5±12.1 |
62.7±14.1 | (26) |
|
| LS | 25 | 7 | 18 |
51.1±12.1 |
68.9±7.4 |
|
| Dionigi, 2012 | HF | 92 | 17 | 75 | 40.8
(20–79)a |
76±10 | (25) |
|
| LS | 90 | 20 | 70 | 41
(20–83)a |
73±9 |
|
| Dionigi, 2013 | FS | 96 | 16 | 80 |
43±11.33 |
73±11.33 | (24) |
|
| LP | 103 | 24 | 79 |
45±10.50 |
85±13.33 |
|
| Kwak, 2014 | HAS | 164 |
20b |
80b | 48.77±10.74 |
71.93±18.26 | (23) |
|
| LSP | 156 |
15.6b |
84.4b | 49.42±10.90 |
75.15±20.13 |
|
| Pons, 2009 | HS | 20 | NA | NA | NA |
114±9 | (22) |
|
| LS | 20 | NA | NA | NA |
122±10 |
|
| Rahbari, 2011 | HF | 45 | 9 | 36 | 46.1c |
184.2±66.2 | (21) |
|
| LSP | 45 | 9 | 36 | 48.7c |
187.6±52.6 |
|
| Sartori, 2008 | HS | 50 | NA | NA | 56±14 |
94±24 | (20) |
|
| LS | 50 | NA | NA | 56±14 |
129±32 |
|
The quality of the included studies was good in
terms of sample size, allocation concealment, blinding and other
sources of bias (Fig. 2). All the
studies applied randomization and provided adequate data for
analysis. Surgical experience was described in 5 of the 7 studies.
Two studies did not provide any information regarding surgical
experience, indicating bias could be possible from this point.
Surgical time
Surgical time was a major outcome of the
meta-analysis (Fig. 3). Even though
one of the RCTs used surgical time as the time from anesthesia to
anesthesia (21), following
discussion, the investigators decided that it would not affect the
final comparisons. All 7 RCTs (20–26) were
included in the analysis, which demonstrated that surgical time
between HS and LS surgery was significantly different (WMD, −8.79
min; 95% CI, −15.91 to −1.67; P=0.02), as HS was significantly
shorter than LS, and the random effect model was used.
Surgical blood loss
No significant differences were observed for
intraoperative blood loss between HS and LS. The pooled estimate
was −6.07 ml in intraoperative blood loss (95% CI, −21.75 to 9.61;
P=0.45) using the random effect model (Fig. 4). In addition, no differences were
observed in the postoperative blood loss between HS and LS. The
pooled estimate was 1.01 ml for postoperative blood loss (95% CI,
−4.53 to 6.55; P=0.72) using the fixed effect model (Fig. 5).
Hospital stay
No significant differences were observed in the
length of hospitalization between HS and LS (WMD, 0.00 days; 95%
CI, −0.04 to 0.04; P=0.84), and the fixed effect model was applied
(Fig. 6).
Thyroid weight
Fig. 7 demonstrated
that thyroid weight was not significantly different in the two
groups (WMD, 1.78 g; 95% CI, −0.89 to 4.45; P=0.19), and the fixed
effect model was applied.
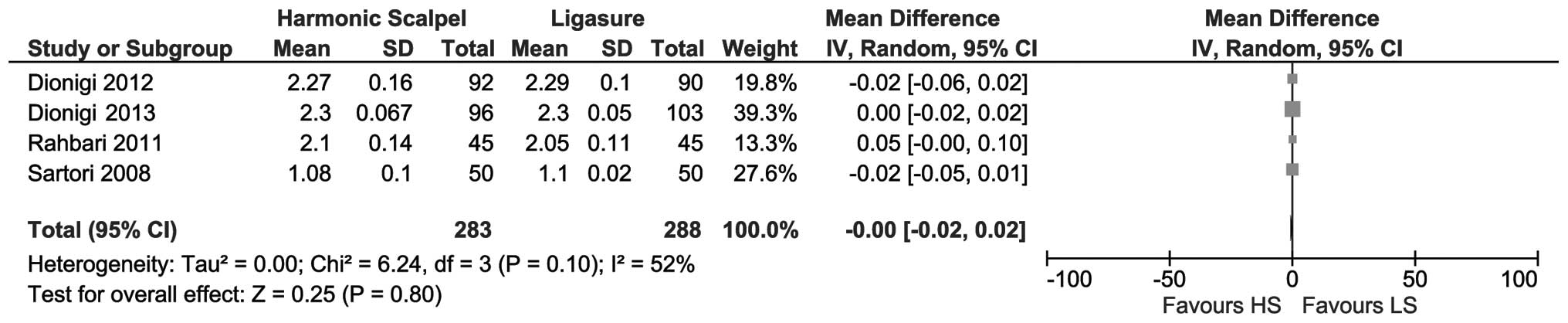
Serum calcium level
As shown in Fig. 8, no
significant difference was observed between the serum calcium level
in the two groups (WMD, 0.00 mmol/l; 95% CI, −0.02 to 0.02;
P=0.80), and the random effect model was applied.
Discussion
The development of devices, such as HS and LS
instruments, has led to shorter surgical time (22). One explanation for the decrease in the
surgical time could be due to reduction in the time required for
the hemostasis of the blood vessels of the thyroid gland. Other
points such as the experience and expertise of surgeons using these
devices could be the reason for the decrease in surgical time. The
HS combines hemostasis and cutting in a single instrument, thus
avoiding the loss of time when associated with the manipulation of
several instruments (22). By
contrast, the LS instrument can only be used for hemostasis, and
sectioning was performed with other instruments such as scissors
(23). McNally et al (27) reported that the surgical time was
significantly decreased in the HS group compared with the LS
instrument group. This was a retrospective analysis of a
prospectively maintained database, so it was excluded in the
present analysis. In this study, no significant differences in
estimated blood loss, gland weight and hypocalcemia were
observed.
HS has been proven to be a safe and useful device in
open and video-assisted cervical surgery (28–34).
Compared with the standard electric scalpel, HS leads to a shorter
surgical time, less lateral thermal spread, and no smoke and no
electric energy passage through the body of the patient (35,36). By
contrast, the LS system is a method of bipolar hemostasis that
denatures the collagen and elastin of the vascular wall and the
connecting tissue around the vessels. The tissues are then merged.
This technology can coagulate vessels that have a diameter ≤7 mm
(37,38). LS is a more time-consuming
multiple-sealing approach at the same vessel but HS divides the
tissue at the same time of coagulation. HS and LS devices have been
developed over the years. In particular, HS has specialized from
its previous generations (CS 14) to Focus, while the LS Precise now
has a blade, which has led to considerable improvement in surgical
time (39). The present study is a
meta-analysis comparing the use of the HS and LS technique in
thyroid surgery including all available evidences until December
2015. This meta-analysis demonstrated that using the HS systems
could significantly reduce surgical time.
Contin et al (39) published a systematic review and
meta-analysis comparing HS, LS and a convention technique other in
2013. The study compared HS and LS with the conventional technique,
and HS and LS separately. The study concluded that HS and LS were
significantly different compared to conventional hemostasis in
terms of surgical time. It also concluded that HS was faster in
comparison to LS. At present, it is >2 years since this
meta-analysis was published. The present study identified new
evidence from the RCTs by Bove et al (26) in 2013 and Kwak et al (23) in 2014. Therefore, the present study is
a more updated meta-analysis comparing HS and LS, including all the
currently available RCTs.
It is important to mention the heterogeneity among
studies while interpreting the meta-analysis results, as certain
differences in methodologies may influence the results. The present
meta-analysis included 7 studies, all RCTs. Differences in the
experience of surgeons and surgical procedures may have affected
the surgical outcomes of the thyroid surgery. Firstly, there were
certain differences in the surgical procedures performed in the
studies. In the RCT by Bove et al (26), superior thyroid artery was ligated
classically when it was >3 mm. However, in the RCT by Dionigi
et al (25), the branches of
the superior thyroid vessels were individually divided proximal to
the thyroid gland (peripheral ligation) to avoid injuring the
external branch of the superior laryngeal nerve and the superior
parathyroid gland. The branches of the inferior thyroid artery were
divided proximal to the thyroid gland capsule to avoid injuring the
recurrent laryngeal nerve and the inferior parathyroid glands. In
the cases of the inadvertent removal of a parathyroid gland, the
technique of parathyroid auto-transplantation was used.
Intraoperative neuro-monitoring of the laryngeal nerves was
routinely performed in all the subjects. Secondly, the experience
of the surgeon was also an important element affecting the outcome.
In the RCT by Bove et al (26),
it was reported that harmonic scissors had numerous advantages as
it was easier to handle and dissect well while maintaining the
advantages of coagulating while cutting. These characteristics were
possibly responsible for the reduction in the duration of surgery
observed. HS could significantly reduce the surgical time at
institutions that performed numerous procedures routinely. It was
suggested that HS could demonstrate its superiority much better in
the hands of experienced surgeons.
The use of HS leading to shorter surgical time has
already been established from previous analyses and numerous RCTs
(20,22,26,27,39), and the
clinical relevance of surgical time as a primary outcome can be
questioned from a patient-centered point of view. As individual
patients will not be concerned with whether their surgery finishes
8 min earlier or later, it is suggested that upcoming studies
should focus on more patient-oriented outcomes such as patient
reported voice quality, nerve and parathyroid vasculature
preservations rather than surgical time. Procedures during thyroid
surgery such as neuro-monitoring may help in the documentation of
nerve preservation, which will reflect the thermal spreading
property of devices to the adjacent tissues. Reduction of surgical
time is a significant advantage for surgical practice as it results
in a smaller hospital stay and hospital-related wound infection
rate. However, the saving of surgical time has to be set in
association with the convenience to a patient, such as higher costs
of the device. Since personnel and material costs differ between
countries and institutions, every single institution has to
reassess the possible benefit of using these devices.
There were certain other limitations in the present
study. First, there was a limited number of studies, as well as
sample size, which was also a major restriction of the current
research. Second, these studies were performed mainly in a single
institution. Third, all the devices in the HS and LS category were
compared, however, a number of newer devices in the two groups are
more efficient compared to their previous versions. As a wide range
of trial participants were included by covering male and female
patients with typical age ranges, partial and total
thyroidectomies, the external validity of these findings are
anticipated to be high.
In conclusion, the present study provided a
quantitative comparison of HS with LS in thyroid surgery. The
results showed a significant reduction of surgical time of HS
compared with LS. The postoperative morbidity was not affected. The
results of the present study may be useful for high-volume centers
performing numerous thyroidectomies every day.
Acknowledgements
The present study was supported by the National Key
Clinical Specialty Project (awarded to the Department of Nuclear
Medicine, Radiology and General Surgery). The study was also
supported by the Tianjin Medical University General Hospital New
Century Excellent Talent Program; Young and Middle-aged Innovative
Talent Training Program from Tianjin Education Committee; and the
Talent Fostering Program (the 131 Project) from Tianjin Education
Committee, Tianjin Human Resources and Social Security Bureau
(awarded to Dr Zhaowei Meng).
References
|
1
|
Bhattacharyya N and Fried MP: Assessment
of the morbidity and complications of total thyroidectomy. Arch
Otolaryngol Head Neck Surg. 128:389–392. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chiang FY, Lee KW, Huang YF, Wang LF and
Kuo WR: Risk of vocal palsy after thyroidecitomy with
identification of the recurrent laryngeal nerve. Kaohsiung J Med
Sci. 20:431–436. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lo CY, Kwok KF and Yuen PW: A prospective
evaluation of recurrent laryngeal nerve paralysis during
thyroidectomy. Arch Surg. 135:204–207. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Dedivitis RA, Pfuetzenreiter EG Jr, Castro
MA and Denardin OV: Analysis of safety of short-stay thyroid
surgery. Acta Otorhinolaryngol Ital. 29:326–330. 2009.PubMed/NCBI
|
|
5
|
Shindo M and Stern A: Total thyroidectomy
with and without selective central compartment dissection: A
comparison of complication rates. Arch Otolaryngol Head Neck Surg.
136:584–587. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Slakey DP: Laparoscopic liver resection
using a bipolar vessel-sealing device: LigaSure. HPB Oxf.
10:253–255. 2008. View Article : Google Scholar
|
|
7
|
Meurisse M, Defechereux T, Maweja S,
Degauque C, Vandelaer M and Hamoir E: Evaluation of the Ultracision
ultrasonic dissector in thyroid surgery. Prospective randomized
study. Ann Chir. 125:468–472. 2000.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Macario A, Dexter F, Sypal J, Cosgriff N
and Heniford BT: Operative time and other outcomes of the
electrothermal bipolar vessel sealing system (LigaSure) versus
other methods for surgical hemostasis: A meta-analysis. Surg Innov.
15:284–291. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yao HS, Wang Q, Wang WJ and Ruan CP:
Prospective clinical trials of thyroidectomy with LigaSure vs
conventional vessel ligation: A systematic review and
meta-analysis. Arch Surg. 144:1167–1174. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cirocchi R, D'Ajello F, Trastulli S,
Santoro A, Di Rocco G, Vendettuoli D, Rondelli F, Giannotti D,
Sanguinetti A, Minelli L, et al: Meta-analysis of thyroidectomy
with ultrasonic dissector versus conventional clamp and tie. World
J Surg Oncol. 8:1122010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ecker T, Carvalho AL, Choe JH, Walosek G
and Preuss KJ: Hemostasis in thyroid surgery: Harmonic scalpel
versus other techniques - a meta-analysis. Otolaryngol Head Neck
Surg. 143:17–25. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Melck AL and Wiseman SM: Harmonic scalpel
compared to conventional hemostasis in thyroid surgery: A
meta-analysis of randomized clinical trials. Int J Surg Oncol.
2010:3960792010.PubMed/NCBI
|
|
13
|
Zhang ZJ, Zhang P, Tian JH, Li J, Li L,
Tian J and Yang KH: Ultrasonic coagulator for thyroidectomy: A
systematic review of randomized controlled trials. Surg Innov.
17:41–47. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Garas G, Okabayashi K, Ashrafian H, Shetty
K, Palazzo F, Tolley N, Darzi A, Athanasiou T and Zacharakis E:
Which hemostatic device in thyroid surgery? A network meta-analysis
of surgical technologies. Thyroid. 23:1138–1150. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Moher D, Shamseer L, Clarke M, Ghersi D,
Liberati A, Petticrew M, Shekelle P and Stewart LA: PRISMA-P Group:
Preferred reporting items for systematic review and meta-analysis
protocols (PRISMA-P) 2015 statement. Syst Rev. 4:12015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Moher D, Liberati A, Tetzlaff J and Altman
DG: PRISMA Group: Preferred reporting items for systematic reviews
and meta-analyses: The PRISMA statement. Int J Surg. 8:336–341.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Higgins JP, Altman DG, Gøtzsche PC, Jüni
P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L and Sterne JA:
Cochrane Bias Methods Group; Cochrane Statistical Methods Group:
The Cochrane Collaboration's tool for assessing risk of bias in
randomised trials. BMJ. 343:d59282011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hopp L: Risk of bias reporting in Cochrane
systematic reviews. Int J Nurs Pract. 21:683–686. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hozo SP, Djulbegovic B and Hozo I:
Estimating the mean and variance from the median, range, and the
size of a sample. BMC Med Res Methodol. 5:132005. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sartori PV, De Fina S, Colombo G, Pugliese
F, Romano F, Cesana G and Uggeri F: Ligasure versus Ultracision in
thyroid surgery: A prospective randomized study. Langenbecks Arch
Surg. 393:655–658. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Rahbari R, Mathur A, Kitano M, Guerrero M,
Shen WT, Duh QY, Clark OH and Kebebew E: Prospective randomized
trial of ligasure versus harmonic hemostasis technique in
thyroidectomy. Ann Surg Oncol. 18:1023–1027. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Pons Y, Gauthier J, Ukkola-Pons E, Clément
P, Roguet E, Poncet JL and Conessa C: Comparison of LigaSure vessel
sealing system, harmonic scalpel, and conventional hemostasis in
total thyroidectomy. Otolaryngol Head Neck Surg. 141:496–501. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kwak HY, Chae BJ, Park YG, Kim SH, Chang
EY, Kim EJ, Song BJ, Jung SS and Bae JS: Comparison of surgical
outcomes between papillary thyroid cancer patients treated with the
Harmonic ACE scalpel and LigaSure Precise instrument during
conventional thyroidectomy: A single-blind prospective randomized
controlled trial. J Surg Res. 187:484–489. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Dionigi G, Van Slycke S, Rausei S, Boni L
and Dionigi R: Parathyroid function after open thyroidectomy: A
prospective randomized study for ligasure precise versus harmonic
FOCUS. Head Neck. 35:562–567. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Dionigi G, Boni L, Rausei S, Frattini F,
Ferrari CC, Mangano A, Leotta A and Franchin M: The safety of
energy-based devices in open thyroidectomy: A prospective,
randomised study comparing the LigaSure™ (LF1212) and the
Harmonic® FOCUS. Langenbecks Arch Surg. 397:817–823.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Bove A, Bongarzoni G, Palone G, Di Renzo
R, Di Nicola M, Corradetti L and Corbellini L: Comparative study of
an electrothermal bipolar vessel sealing system
(LigaSure®), a harmonic curved shears (Harmonic Focus™),
and traditional technique in total thyroidectomy. Am Surg.
76:E94–E96. 2010.PubMed/NCBI
|
|
27
|
McNally MM, Agle SC, Williams RF and
Pofahl WE: A comparison of two methods of hemostasis in
thyroidectomy. Am Surg. 75:1073–1076. 2009.PubMed/NCBI
|
|
28
|
Manouras A, Lagoudianakis EE, Antonakis
PT, Filippakis GM, Markogiannakis H and Kekis PB: Electrothermal
bipolar vessel sealing system is a safe and time-saving alternative
to classic suture ligation in total thyroidectomy. Head Neck.
27:959–962. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kiriakopoulos A, Dimitrios T and Dimitrios
L: Use of a diathermy system in thyroid surgery. Arch Surg.
139:997–1000. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Miccoli P: Minimally invasive surgery for
thyroid and parathyroid diseases. Surg Endosc. 16:3–6. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Miccoli P, Materazzi G, Fregoli L,
Panicucci E, Kunz-Martinez W and Berti P: Modified lateral neck
lymphadenectomy: Prospective randomized study comparing harmonic
scalpel with clamp-and-tie technique. Otolaryngol Head Neck Surg.
140:61–64. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Siperstein AE, Berber E and Morkoyun E:
The use of the harmonic scalpel vs conventional knot tying for
vessel ligation in thyroid surgery. Arch Surg. 137:137–142. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Voutilainen PE and Haglund CH:
Ultrasonically activated shears in thyroidectomies: A randomized
trial. Ann Surg. 231:322–328. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Dralle H, Sekulla C, Haerting J,
Timmermann W, Neumann HJ, Kruse E, Grond S, Mühlig HP, Richter C,
Voss J, et al: Risk factors of paralysis and functional outcome
after recurrent laryngeal nerve monitoring in thyroid surgery.
Surgery. 136:1310–1322. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Boddy SA, Ramsay JW, Carter SS, Webster
PJ, Levison DA and Whitfield HN: Tissue effects of an ultrasonic
scalpel for clinical surgical use. Urol Res. 15:49–52. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Gossot D: Ultrasonic dissectors in
endoscopic surgery. Ann Chir. 52:635–642. 1998.(In French).
PubMed/NCBI
|
|
37
|
Youssef T, Mahdy T, Farid M and Latif AA:
Thyroid surgery: Use of the LigaSure Vessel Sealing System versus
conventional knot tying. Int J Surg. 6:323–327. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Lachanas VA, Prokopakis EP, Mpenakis AA,
Karatzanis AD and Velegrakis GA: The use of Ligasure Vessel Sealing
System in thyroid surgery. Otolaryngol Head Neck Surg. 132:487–489.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Contin P, Gooßen K, Grummich K, Jensen K,
Schmitz-Winnenthal H, Büchler MW and Diener MK: ENERgized vessel
sealing systems versus CONventional hemostasis techniques in
thyroid surgery - the ENERCON systematic review and network
meta-analysis. Langenbecks Arch Surg. 398:1039–1056. 2013.
View Article : Google Scholar : PubMed/NCBI
|