Introduction
Gastric ulcers are characterized by necrosis,
induction of oxidative stress and secretion of inflammatory factors
(1). In the Western population, the
prevalence of gastric ulcers is 2.4% (2) and 6.07% in China (3). In addition, in patients with
gastrointestinal symptoms, the incidence rates of gastric ulcers
increases to 22.5% (4). According to
the epidemiological investigation, when individuals smoke, consume
alchol or use nonsteroidal anti-inflammatory drugs, the incidence
of gastric ulcer increases (5–7). Although gender differences have not been
reported for gastric ulcers, the incidence rate in women has
increased during the previous 10 years (8). The pathogenesis of gastric ulcers is
based on a multifactorial and complex interaction between
protective and aggressive factors, including mucosal integrity,
secretion of gastric acid, Helicobacter pylori, free oxygen
radicals and excess alcohol consumption (9–11).
Currently, the treatment is predominantly performed by inhibition
of gastric acid secretion, proton pump inhibitors and eradication
of H. pylori with antibiotics. However, such treatments are
not completely effective and produce certain adverse effects
(12). Disturbing the balance between
aggressive and protective factors that control cell apoptosis and
proliferation results in gastric ulceration, which then activates
the repairing system in the gastric mucosa. For these reasons, the
search for novel therapeutic agents is relevant, and medicinal
plants and natural products are included in these studies, since
many extracts and isolated compounds have shown promising results
in gastroprotective activities (13,14).
Fructus Arctii, the dried fruits of Arctium
lappa L., are well-known detoxifying agents in traditional
Chinese medicine (15). Arctigenin is
a lignin constituent of Fructus Arctii. Arctigenin displays
anti-H. pylori (16) and
anti-inflammatory activity (17–19),
inhibits T lymphocyte proliferation and the gene expression of IL-6
and interferon-γ, and exerts anti-tumor activity against
pancuronium-1 cells (20,21). However, there are few studies analyzing
anti-ulcer activity using arctigenin. Therefore, the present study
aimed to evaluate the potential effects of arctigenin on the
prevention (by the absolute ethanol model of ulcer induction) and
the treatment of experimental gastric ulcers (by the acetic acid
model of ulcer induction). In addition, malondialdehyde (MDA) and
superoxide dismutase (SOD) levels in serum and expression levels of
cytokines, such as tumor necrosis factor-α (TNF-α), interleukin-6
(IL-6), IL-10 and C-reactive protein (CRP) in the gastric tissues
were evaluated.
In the present study, the preventive effect of
arctigenin on gastric ulcers was investigated in a Sprague-Dawley
(SD) rat model. The results indicate that arctigenin effectively
decreases inflammatory factors in gastric ulcer rats and protects
them from gastric ulcer lesions.
Materials and methods
Preparation of arctigenin
The dried seeds of Arctium lappa L. were
bought from Cangshan (February 2012, Shandong, China).
Identification of the plants was confirmed by Dr Li Shouxin (senior
engineer; State Key Laboratory of Generic Manufacture Technology of
Chinese Traditional Medicine, Linyi, China). A voucher specimen
(no. 20110920) was deposited in the State Key Laboratory of Generic
Manufacture Technology of Chinese Traditional Medicine. The Fructus
Arctii was hydrolyzed by acid hydrolysis and alcohol extraction.
The crude product was separated by ethyl acetate extraction, and
the arctigenin with >75% purity was collected. A high purity of
arctigenin was obtained by ethanol crystallization. The finished
product was crystallized with anhydrous ethanol until the purity of
arctigenin was >99%.
Animals
One hundred male SD rats (200±20 g; age, 8–10 weeks)
were supplied by Lunan Pharmaceutical Group Co., Ltd. (Linyi,
China), acclimatized to a controlled temperature (23±2°C) and
maintained under a 12-h light/dark cycle. The animals were supplied
with pellet chow and water ad libitum. All experiments were
in accordance with the experimental protocols previously approved
by the Institution Animal Ethics Committee at the Pharmacological
Center of Lunan Pharmaceutical Group Co., Ltd., and performed in
accordance with the Declaration of Helsinki.
Ethanol-induced gastric ulcer
The model of ethanol-induced ulcers was performed as
described previously with minor modifications (22). Rats were randomly divided into five
groups (n=8 per group). Animals were administrated with vehicle
[20% PEG400 (Shanghai Chemical Co., Shanghai, China) in saline],
graded doses of arctigenin (0.05, 0.15 and 0.45 mg/kg; purity,
>99%, extracted in our laboratory) dissolved in saline
containing 20% PEG400 or cimetidine (36 mg/kg; Shandong Fangming
Pharmaceutical Group Co., Ltd., Heze, China) for 6 days. Animals
were deprived of food for 24 h before experiments. One-hour post
administration with 1 ml absolute ethanol, animals were
anesthetized with pentobarbital (50 mg/kg; Sigma-Aldrich, St.
Louis, MO, USA), the inferior vena cava was punctured and 2-ml
blood samples were collected in pro-coagulation tubes to obtain the
serum (by centrifugation at 1,024 × g for 10 min at 4°C). The serum
was stored at −80°C. The rats were anesthetized with 3%
pentobarbital (Sigma-Aldrich) the abdomen was opened, to expose the
abdominal aorta, and the rats were sacrificed by bloodletting of
the vena cardinalis. The stomachs were removed on ice, opened along
the greater curvature, washed with saline (0.9%), and the ulcer
index was evaluated according to the number and severity of lesions
formed. The scoring was performed according to the following scale
(23): 0, no visible ulcers; 1,
petechial hemorrhage or minute pin-point ulcers; 2, striate
hemorrhage and erosion <2 mm; 3, striate hemorrhage and erosion
≥2 and <3 mm; 4, striate hemorrhage and erosion ≥3 and <4 mm;
5, striate hemorrhage and erosion ≥4 and <5 mm.
The mean ulcer indices in each group were calculated
and expressed as the percentage of inhibition using the following
formula: Inhibition (%) = (control mean - treated mean/control
mean) × 100.
Acetic acid-induced gastric ulcer
The experiment was performed as described previously
(24) with minor modifications. Rats
had been fasting for 12 h before the experiment and had free access
to water. A longitudinal incision below the xiphoid process was
made in the anesthetized rats. The anterior wall of the stomach was
exposed, then 0.02 ml of 30% acetic acid was injected with a
microsyringe in the subserosal layer at the junction of the fundus
with the antrum, and later washed with saline. On the following
day, the daily treatments were initiated (once a day for 12 days)
in six groups: sham, vehicle, cimetidine (36 mg/kg), arctigenin
(0.05, 0.15 and 0.45 mg/kg) and the sham group (that underwent the
surgical procedure of ulcer induction without the application of
acetic acid). Following the final treatment, the rats were
anesthetized with 3% pentobarbital and sacrificed as described
above. The stomachs were removed. The minimum and maximum diameters
of the open ulcer were then measured, and the product was
considered to be the ulcer index. The 100-mg gastric tissue samples
obtained from the corpus region were stored at −80°C for the
subsequent measurement of TNF-α, IL-6, IL-10 and CRP using
ELISA.
Determination of MDA and SOD serum
levels
The blood samples were centrifuged at 1,024 × g for
10 min at 4°C to obtain the serum. Serum levels of MDA and SOD were
determined using a MDA Assay kit (Nanjing JianCheng Bioengineering
Institute, Nanjing, China) and Total SOD Assay kit (Nanjing
JianCheng Bioengineering Institute) according to the manufacturer's
instructions.
Measurement of TNF-α, IL-6, IL-10 and
CRP expression levels
Tissue samples were homogenized in 10 volumes of
0.9% saline and centrifuged at 1,024 × g at 4°C for 15 min. The
supernatant was collected and the levels of TNF-α (Tumor Necrosis
Factor-α Assay kit; Nanjing JianCheng Bioengineering Institute),
IL-6 (Interleukin-6 Assay kit; Nanjing JianCheng Bioengineering
Institute), IL-10 (Interleukin-10 Assay kit; Nanjing JianCheng
Bioengineering Institute) and CRP (C-Reactive Protein Assay kit;
Nanjing JianCheng Bioengineering Institute) were determined by
ELISA. All procedures were performed according to the
manufacturer's instructions.
Statistical analysis
The parameters were recorded for individuals within
all of the groups. Data are presented as the mean ± standard error
of the mean. Statistical analysis was performed with a one-way
analysis of variance (ANOVA) using SPSS 17.0 (SPSS, Inc., Chicago,
IL, USA) and P<0.05 was considered to indicate a statistically
significant difference. Continuous variables are expressed as means
± standard deviation and compared with two-tailed probability
values from an overall F test from a one-way ANOVA, and pairwise
comparisons with Fisher's test of least significant difference.
Results
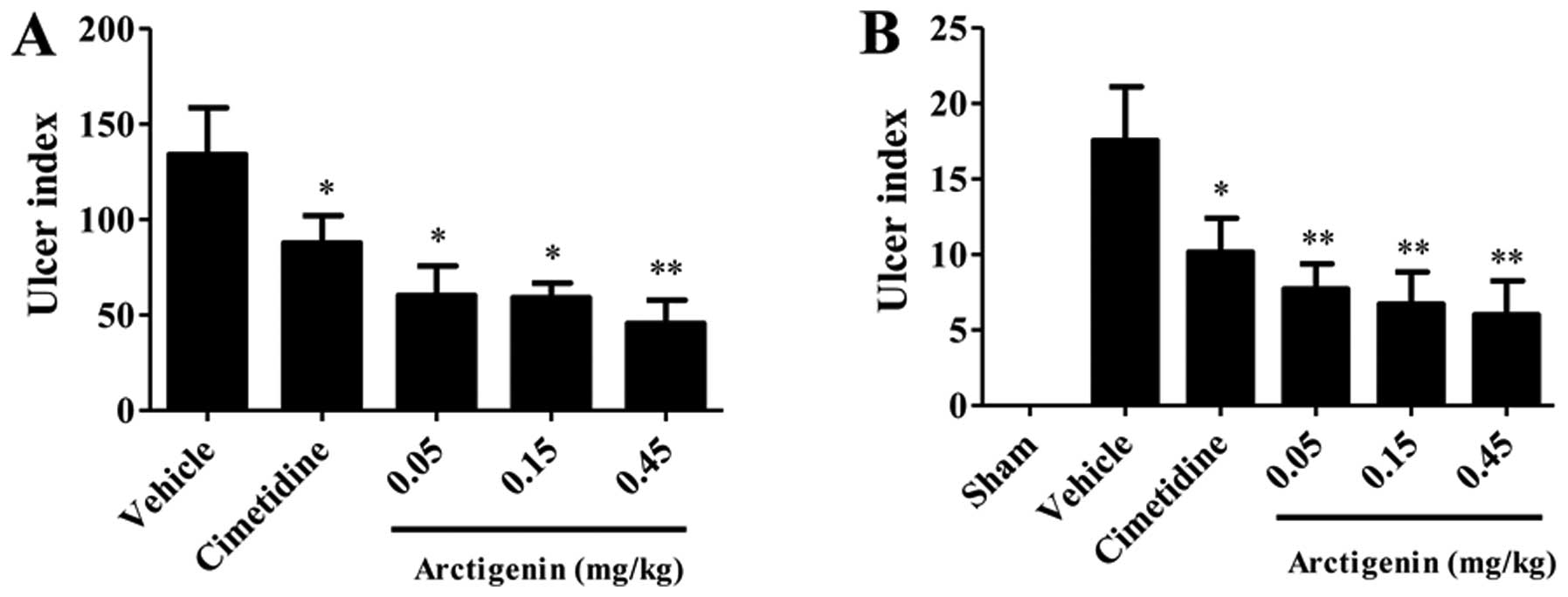
Ethanol-induced gastric ulcers
The gastroprotective effects of arctigenin on
acetic-induced gastric damage were observed in arctigenin-treated
rats (Fig. 1A). Ulcerated rats
pretreated with cimetidine or arctigenin demonstrated significantly
reduced (P<0.05) ulcer indices when compared with the vehicle
group. The cimetidine and arctigenin at doses of 0.05, 0.15, 0.45
mg/kg significantly inhibited the appearance of lesions by 31.60,
64.43, 53.91 and 53.04%, respectively. By determination of the
ulcer index, arctigenin resulted in an inverted curve, thus, the
optimum gastroprotective effect was obtained at a dose of 0.45
mg/kg; Fig. 1A).
Acetic acid-induced chronic ulcer
Serosal application of acetic acid to the
vehicle-treated rats resulted in extensive gastric lesions at 10
days of ulcer induction (17.56±3.56 mm2), where the
ulcer erosion index was found to be significantly high when
compared with the sham group rats without any lesions (P<0.001).
All doses of arctigenin (0.05, 0.15 and 0.45 mg/kg) reduced the
ulcer index significantly (P<0.01). However, 36 mg/kg cimetidine
reduced the ulcer index significantly (P<0.05). The percentages
inhibition was 65.83, 61.73, 56.09 and 42.14% for the groups
treated with 0.05, 0.15 and 0.45 mg/kg and cimetidine,
respectively. In the present study, arctigenin also presented an
inverted curve, so that the best gastroprotective effect was
obtained at a dose of 0.45 mg/kg; Fig.
1B).
Determination of the sera levels of
MDA and SOD
For the group that received vehicle only, the level
of MDA was 7.963±0.680 nmol/l. Pretreatment with arctigenin at
doses of 0.05, 0.15, 0.45 mg/kg and cimetidine significantly
decreased the levels of MDA (5.670±0.264, 4.962±0.311, 4.979±0.260
and 5.527±0.231 nmol/l, respectively) compared with the vehicle
group (P<0.01; Fig. 2A). The SOD
level in arctigenin-treated at 0.05 mg/kg (122.39±6.85 U/ml), 0.15
mg/kg (119.33±4.04 U/ml) and 0.45 mg/kg (145.50±6.83 U/ml)
significantly increased the SOD level compared with the vehicle
group (124.28±6.27 U/ml) (P<0.05; Fig.
2B).
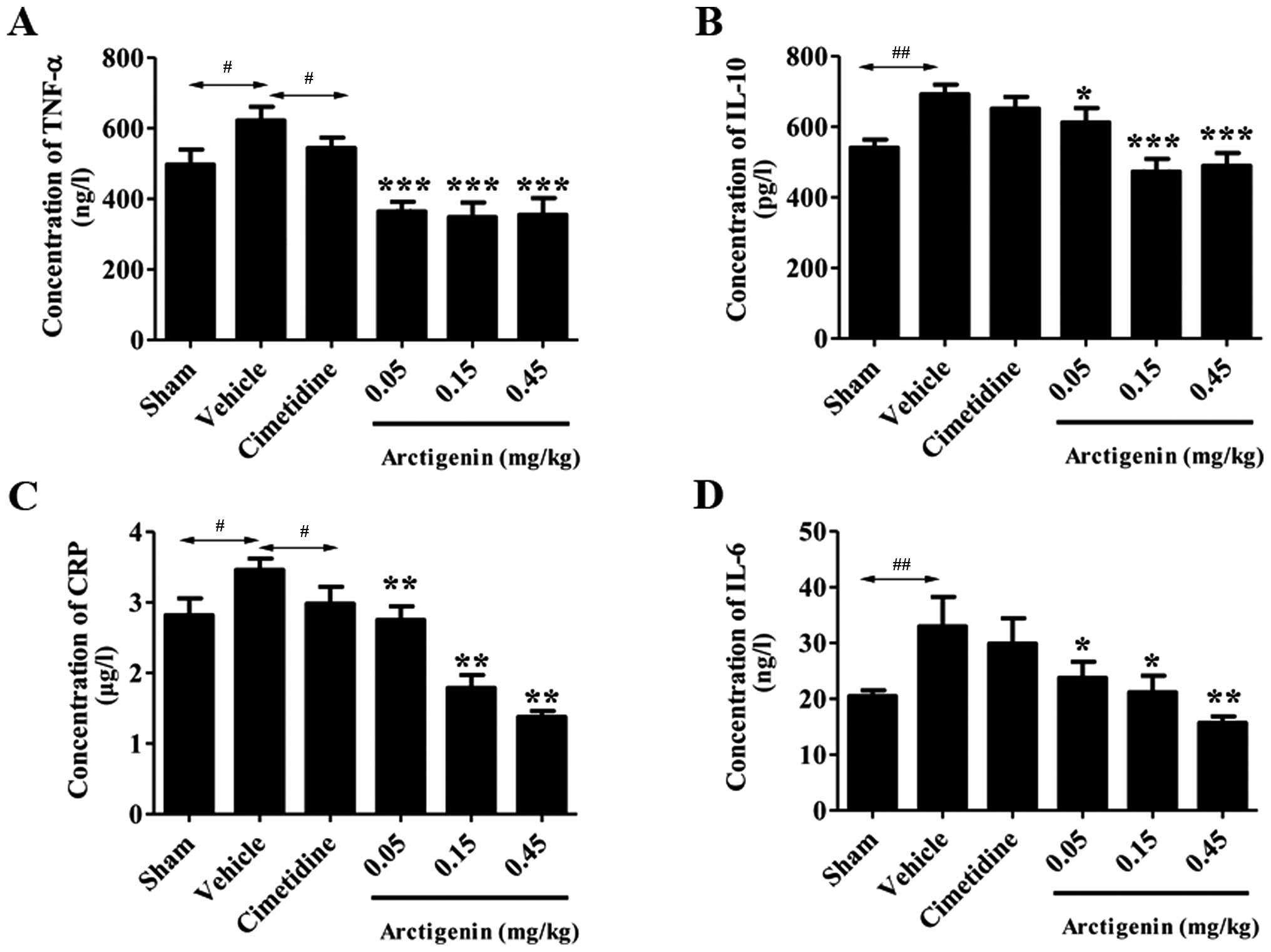
Comparison of the levels of cytokines
in rat stomach tissue samples
All doses of arctigenin treatment significantly
reduced the TNF-α levels (364.55±27.22, 348.43±41.45 and
355.13±60.35 ng/l; P<0.01) when compared with the vehicle group
(534.17±49.91 ng/l). However, treatment of cimetidine at the doses
of 36 mg/kg did not significantly decrease the TNF-α levels
(Fig. 3A).
The IL-10 levels in the vehicle group increased
significantly (692.21±27.36 pg/l; P<0.01) compared with the sham
group (605.75±57.20 pg/l; Fig. 3B).
The rats that received 0.05, 0.15 and 0.45 mg/kg arctigenin
demonstrated significantly reduced IL-10 levels (612.49±40.39,
473.02±36.30 and 489.46±36.26 pg/l, respectively; P<0.001) when
compared with the vehicle group. The other groups were not
significantly altered compared with the vehicle group.
Treatment with arctigenin at doses of 0.05, 0.15 and
0.45 mg/kg significantly decreased the levels of CRP [2.75±0.19
µg/l (P<0.05); 1.79±0.18 µg/l (P<0.01) and 1.38±0.08 µg/l
(P<0.01), respectively] when compared with the vehicle group.
However, rats that received cimetidine showed no significant
reduction in the CRP level when compared with the vehicle group
(2.98±0.24 µg/l; P>0.05) (Fig.
3C).
The gastric tissue IL-6 level in the vehicle group
(32.97±5.30 ng/l) demonstrated a significant increase when compared
with the sham group (20.48±1.05 ng/l; P<0.05). However,
cimetidine showed no significant reduction in the IL-6 level when
compared with the vehicle group. In addition, 0.05, 0.15 and 0.45
mg/kg arctigenin exhibited strong inhibition effects on IL-6
(23.77±2.88, 21.20±2.94 and 15.68±1.17 ng/l) compared with vehicle
group (Fig. 3D).
Discussion
To the best of our knowledge, the present study is
the first to report the gastroprotective of arctigenin from Fructus
Arctii, which inhibits the ulcer index induced by absolute ethanol
and acetic acid (Fig. 1), and provides
experimental evidence to support the traditional use of Fructus
Arctii in the treatment of stomach dysfunction.
Ethanol and acetic acid are the most commonly
utilized experimental models for the evaluation of anti-ulcer
activity in rats (24,25). The gastroprotective effect of
arctigenin in different experimental ulcer models is presented in
the current study, as various mechanisms are involved in the
etiology of gastric ulcers. Ethanol-induced gastric ulcers are a
reliable model of acute gastric mucosal ulceration; as shown in
Fig. 1A, arctigenin treatment
inhibited the gastric damage induced by ethanol at all doses with
similar efficacy as compared with the vehicle group.
In addition to the gastroprotective effect of
arctigenin, the healing effect on the gastric mucosa in the acetic
acid-induced ulcer model was investigated. This chronic ulcer
model, which highly resembles human chronic ulcers in terms of
pathological features and healing mechanisms, is utilized to
develop novel anti-ulcer medication, which may potentially prevent
ulcer relapse or enhance ulcer healing (26). Acetic acid is reported to produce
ulcers by gastric obstruction leading to increased quantities of
acidic gastric juice (27,28). In the current study, arctigenin caused
significant reductions in gastric lesions at all doses tested, when
compared with the vehicle group (Fig.
1B), indicating that arctigenin exerted curative effects. This
result suggested that arctigenin may have protective effects in the
treatment of chronic ulcers.
The effects of ethanol on the gastric mucosa may be
associated with the formation of reactive oxygen species (ROS),
which cause an imbalance between oxidant and antioxidant cellular
processes. It is known that lipid peroxidation is the result of ROS
interacting with the cell membrane, subsequently producing highly
reactive lipid-derived free radicals, such as MDA, to cause
oxidative gastric damage (29).
However, organisms possess enzymatic defenses (SOD) against the
lipid peroxidation. In the current study, arctigenin lowered the
elevated MDA level and increased the SOD level (Fig. 2). Thus, it was concluded that the
ability of arctigenin to reduce the MDA level and increase the SOD
level may contribute to its gastroprotective effect by inhibiting
oxidative gastric damage.
Inflammation is generally considered to be a highly
regulated defensive process characterized by the release of
cytokines from the blood to the affected tissue (30). The potent pro-inflammatory cytokines
(such as TNF, IL-1, interferon-γ) are involved in the occurrence
and development of inflammatory responses (31,32). The
acetic acid, a well-known ulcerogenic agent, stimulates
inflammation via the imbalance of pro- and anti-inflammatory
cytokines (33). In the current study,
acetic acid-induced ulcer models were used to investigate the
gastroprotective effect of arctigenin. Arctigenin effectively
regulated four pro-inflammatory cytokines and attenuated acetic
acid-induced ulcers. Thus, in the present study TNF-α, IL-6, IL-10
and CRP were evaluated in gastric homogenate (Fig. 3). TNF-α, which is increased in
non-steroidal anti-inflammatory drug-treated rats, appears to be a
key contributor on many forms of gastric mucosal damage (34,35). IL-10
is a pleiotropic cytokine with important immunoregulatory functions
whose actions influence activities of many cell-types in the immune
system. The levels of IL-10 are prominently increased in peptic
ulcer patients (36). Numerous
clinical studies reported that the levels of inflammatory factors
(IL-6, CRP and TNF-α) were consistent with the pathogenic condition
of gastric ulcer patients (37). It is
reported that an elevated CRP level is a positive predictive value
for peptic ulcers caused by active inflammation (38). These results corroborated the report of
Hyam et al (39), who observed
that arctigenin inhibited 2,4,6-trinitrobenzenesulfonic
acid-induced IL-6 and TNF-α expression. These findings reveal that
the anti-ulcerogenic effects of arctigenin may be mediated by
anti-inflammatory activities.
The results of the present study indicate that
arctigenin afforded remarkable ameliorative effects against gastric
mucosal lesions induced by ethanol and acetic acid, thereby
confirming anti-ulcer activity in SD rats. The gastroprotective
effect of arctigenin may be attributed to its activities against
oxidative and inflammatory damage. In conclusion, the results
obtained in the present study provide support for the use of
arctigenin as a gastroprotective medicine. Furthermore, the current
study provides more information on the possible underlying
mechanisms by which arctigenin exerts its anti-ulcer effects.
Acknowledgements
The present study was supported by the National
Science and Technology Support Program (grant no. 2012CB724001) and
the Shandong province Science and Technology Major Project (grant
no. 2015ZDJQ05004), gratefully received from The Generic
Manufacture Technology of Chinese Traditional Medicine and Lunan
Pharmaceutical Group Co., Ltd.
Glossary
Abbreviations
Abbreviations:
|
ARG
|
arctigenin
|
|
MDA
|
malondialdehyde
|
|
SOD
|
superoxide dismutase
|
|
TNF-α
|
tumor necrosis factor-α
|
|
IL-6
|
interleukin-6
|
|
IL-10
|
interleukin-10
|
|
CRP
|
C-reactive protein
|
References
|
1
|
de Souza Almeida ES, Filho VC, Niero R,
Clasen BK, Balogun SO and de Oliveira Martins DT: Pharmacological
mechanisms underlying the anti-ulcer activity of methanol extract
and canthin-6-one of Simaba ferruginea A. St-Hil. in animal models.
J Ethnopharmacol. 134:630–636. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Groenen MJ, Kuipers EJ, Hansen BE and
Ouwendijk RJ: Incidence of duodenal ulcers and gastric ulcers in a
Western population: Back to where it started. Can J Gastroenterol.
23:604–608. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dong WG, Cheng CS, Liu SP and Yu JP:
Epidemiology of peptic ulcer disease in Wuhan area of China from
1997 to 2002. World J Gastroenterol. 10:3377–3379. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Li Z, Zou D, Ma X, Chen J, Shi X, Gong Y,
Man X, Gao L, Zhao Y, Wang R, et al: Epidemiology of peptic ulcer
disease: Endoscopic results of the systematic investigation of
gastrointestinal disease in China. Am J Gastroenterol.
105:2570–2577. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Maity P, Biswas K, Roy S, Banerjee RK and
Bandyopadhyay U: Smoking and the pathogenesis of gastroduodenal
ulcer - recent mechanistic update. Mol Cell Biochem. 253:329–338.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
García Rodríguez LA and Hernández-Díaz S:
Risk of uncomplicated peptic ulcer among users of aspirin and
nonaspirin nonsteroidal antiinflammatory drugs. Am J Epidemiol.
159:23–31. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ko JK and Cho CH: Alcohol drinking and
cigarette smoking: A ‘partner’ for gastric ulceration. Zhonghua Yi
Xue Za Zhi (Taipei). 63:845–854. 2000.PubMed/NCBI
|
|
8
|
Wysocki A, Budzyński P, Kulawik J and
Drożdż W: Changes in the localization of perforated peptic ulcer
and its relation to gender and age of the patients throughout the
last 45 years. World J Surg. 35:811–816. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bhattacharya S, Banerjee D, Bauri AK,
Chattopadhyay S and Bandyopadhyay SK: Healing property of the Piper
betel phenol, allylpyrocatechol against indomethacin-induced
stomach ulceration and mechanism of action. World J Gastroenterol.
13:3705–3713. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Pakrashi A, Pandit S, Bandyopadhyay SK and
Pakrashi SC: Antioxidant effect of Phyllanthus emblica fruits on
healing of indomethacin induced gastric ulcer in rats. Indian J
Clin Biochem. 18:15–21. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zheng XG, Zhang JJ and Huang YC: Study on
the effect of weitongning on epidermal growth factor and nitric
oxide contents in tissue of stomach of rats with gastric ulcer.
Zhongguo Zhong Xi Yi Jie He Za Zhi. 24:549–551. 2004.(In Chinese).
PubMed/NCBI
|
|
12
|
Lin PC, Chang CH, Hsu PI, Tseng PL and
Huang YB: The efficacy and safety of proton pump inhibitors vs
histamine-2 receptor antagonists for stress ulcer bleeding
prophylaxis among critical care patients: A meta-analysis. Crit
Care Med. 38:1197–1205. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Vasconcelos PC, Andreo MA, Vilegas W,
Hiruma-Lima CA and Pellizzon CH: Effect of Mouriri pusa tannins and
flavonoids on prevention and treatment against experimental gastric
ulcer. J Ethnopharmacol. 131:146–153. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Karakoyun B, Yüksel M, Ercan F, Erzik C
and Yeğen BC: Alpha-lipoic acid improves acetic acid-induced
gastric ulcer healing in rats. Inflammation. 32:37–46. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Park SY, Hong SS, Han XH, Hwang JS, Lee D,
Ro JS and Hwang BY: Lignans from Arctium lappa and their inhibition
of LPS-induced nitric oxide production. Chem Pharm Bull (Tokyo).
55:150–152. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kamkaen N, Matsuki Y, Ichino C, Kiyohara H
and Yamada H: The isolation of the anti-helicobacter pylori
compoundsin seeds of Arctium lappa Linn. Thai Pharm Health Sci J.
1:12–18. 2006.
|
|
17
|
Kang HS, Lee JY and Kim CJ:
Anti-inflammatory activity of arctigenin from Forsythiae Fructus. J
Ethnopharmacol. 116:305–312. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kou X, Qi S, Dai W, Luo L and Yin Z:
Arctigenin inhibits lipopolysaccharide-induced iNOS expression in
RAW264.7 cells through suppressing JAK-STAT signal pathway. Int
Immunopharmacol. 11:1095–1102. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhao F, Wang L and Liu K: In vitro
anti-inflammatory effects of arctigenin, a lignan from Arctium
lappa L., through inhibition on iNOS pathway. J Ethnopharmacol.
122:457–462. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tsai WJ, Chang CT, Wang GJ, Lee TH, Chang
SF, Lu SC and Kuo YC: Arctigenin from Arctium lappa inhibits
interleukin-2 and interferon gene expression in primary human T
lymphocytes. Chin Med. 6:122011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Awale S, Lu J, Kalauni SK, Kurashima Y,
Tezuka Y, Kadota S and Esumi H: Identification of arctigenin as an
antitumor agent having the ability to eliminate the tolerance of
cancer cells to nutrient starvation. Cancer Res. 66:1751–1757.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Morimoto Y, Shimohara K, Oshima S and
Sukamoto T: Effects of the new anti-ulcer agent KB-5492 on
experimental gastric mucosal lesions and gastric mucosal defensive
factors, as compared to those of teprenone and cimetidine. Jpn J
Pharmacol. 57:495–505. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Guth PH, Aures D and Paulsen G: Topical
asprin plus HCl gastric lesions in the rats. Cytoprotective effect
of prostaglandin, cimetidine, and probanthine. Gastroenterology.
76:88–93. 1979.PubMed/NCBI
|
|
24
|
Okabe S and Amagase K: An overview of
acetic acid ulcer models - the history and state of the art of
peptic ulcer research. Biol Pharm Bull. 28:1321–1341. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Mutoh H, Hiraishi H, Ota S, Ivey KJ,
Terano A and Sugimoto T: Role of oxygen radicals in ethanol-induced
damage to cultured gastric mucosal cells. Am J Physiol.
258:G603–G609. 1990.PubMed/NCBI
|
|
26
|
Jung J, Bae KH and Jeong CS:
Anti-Helicobacter pylori and antiulcerogenic activities of the root
cortex of Paeonia suffruticosa. Biol Pharm Bull. 36:1535–1539.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhang FY, Yang FJ, Yang JL, Wang L and
Zhang Y: Renin inhibition improves ovariectomy-induced osteoporosis
of lumbar vertebra in mice. Biol Pharm Bull. 37:1994–1997. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Jainu M and Devi CS: Antiulcerogenic and
ulcer healing effects of Solanum nigrum (L.) on experimental ulcer
models: Possible mechanism for the inhibition of acid formation. J
Ethnopharmacol. 104:156–163. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kwiecień S, Brzozowski T and Konturek SJ:
Effects of reactive oxygen species action on gastric mucosa in
various models of mucosal injury. J Physiol Pharmacol. 53:39–50.
2002.PubMed/NCBI
|
|
30
|
Bradding P, Feather IH, Wilson S, Bardin
PG, Heusser CH, Holgate ST and Howarth PH: Immunolocalization of
cytokines in the nasal mucosa of normal and perennial rhinitic
subjects. The mast cell as a source of IL-4, IL-5, and IL-6 in
human allergic mucosal inflammation. J Immunol. 151:3853–3865.
1993.PubMed/NCBI
|
|
31
|
Su SC, Hua KF, Lee H, Chao LK, Tan SK, Lee
H, Yang SF and Hsu HY: LTA and LPS mediated activation of protein
kinases in the regulation of inflammatory cytokines expression in
macrophages. Clin Chim Acta. 374:106–115. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Wang HD, Lu DX and Qi RB: Therapeutic
strategies targeting the LPS signaling and cytokines.
Pathophysiology. 16:291–296. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Beserra AM, Calegari PI, Souza MC, Dos
Santos RA, Lima JC, Silva RM, Balogun SO and Martins DT:
Gastroprotective and ulcer-healing mechanisms of ellagic acid in
experimental rats. J Agric Food Chem. 59:6957–6965. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Martin GR and Wallace JL: Gastrointestinal
inflammation: A central component of mucosal defense and repair.
Exp Biol Med (Maywood). 231:130–137. 2006.PubMed/NCBI
|
|
35
|
Appleyard CB, McCafferty DM, Tigley AW,
Swain MG and Wallace JL: Tumor necrosis factor mediation of
NSAID-induced gastric damage: Role of leukocyte adherence. Am J
Physiol. 270:G42–G48. 1996.PubMed/NCBI
|
|
36
|
Li TT and Liu XH: Clinical value of
determination of changes of serum Gas, IL-2, IL-10 and IL-18 levels
after transfusion of Red blood cells in patients with peptic ulcer.
Journal of Radioimmunology. 24:515–517. 2011.
|
|
37
|
Zhang Y: Impact of esomeprazole on
gastrointestinal hormones and inflammatory state of patients with
gastric ulcer. Journal of Clinical Medicine in Practice. 17:68–70.
2013.
|
|
38
|
Boehme MW, Autschbach F, Ell C and Raeth
U: Prevalence of silent gastric ulcer, erosions or severe acute
gastritis in patients with type 2 diabetes mellitus - a
cross-sectional study. Hepatogastroenterology. 54:643–648.
2007.PubMed/NCBI
|
|
39
|
Hyam SR, Lee IA, Gu W, Kim KA, Jeong JJ,
Jang SE, Han MJ and Kim DH: Arctigenin ameliorates inflammation in
vitro and in vivo by inhibiting the PI3K/AKT pathway and polarizing
M1 macrophages to M2-like macrophages. Eur J Pharmacol. 708:21–29.
2013. View Article : Google Scholar : PubMed/NCBI
|