|
1
|
Barbero MG: ¿Como ha afectado la COVID- 19
al sistema sanitario y la formación de los médicos y que hemos
aprendido? Educación Médica. 22:S1–S2. 2021.
|
|
2
|
Pan American Health Organization:
Epidemiological update: SARS-CoV-2 and other respiratory viruses in
the Americas Region-8 January 2024., 2024.
|
|
3
|
Delgado-Enciso I, Paz-Garcia J,
Barajas-Saucedo CE, Mokay-Ramírez KA, Meza-Robles C, Lopez-Flores
R, Delgado-Machuca M, Murillo-Zamora E, Toscano-Velazquez JA,
Delgado-Enciso J, et al: Safety and efficacy of a COVID-19
treatment with nebulized and/or intravenous neutral electrolyzed
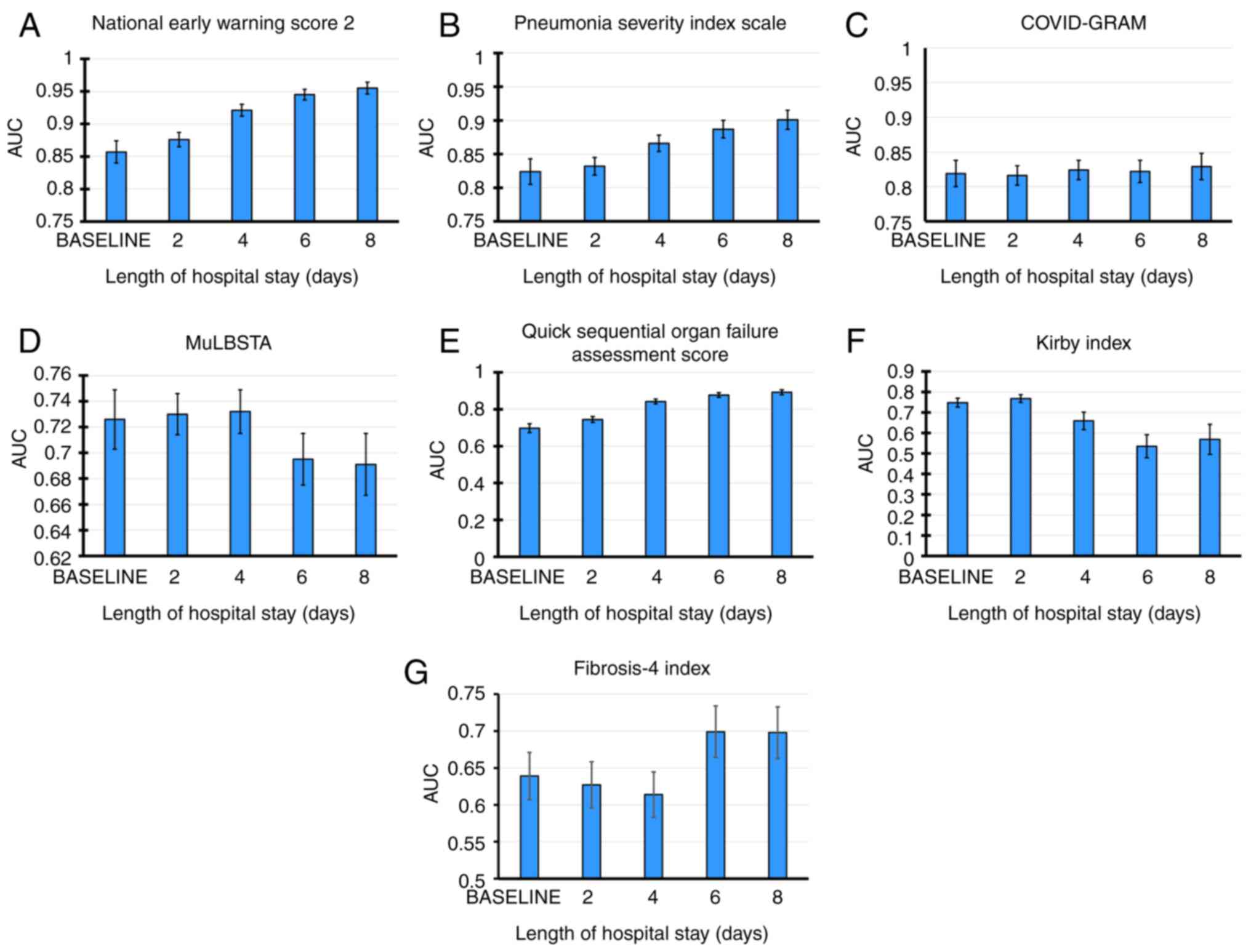
saline combined with usual medical care vs. usual medical care
alone: A randomized, open-label, controlled trial. Exp Ther Med.
22(915)2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Mascellino MT, Di Timoteo F, De Angelis M
and Oliva A: Overview of the main anti-SARS-CoV-2 vaccines:
Mechanism of action, efficacy and safety. Infect Drug Resist.
14:3459–3476. 2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Havers FP, Pham H, Taylor CA, Whitaker M,
Patel K, Anglin O, Kambhampati AK, Milucky J, Zell E, Moline HL, et
al: COVID-19-associated hospitalizations among vaccinated and
unvaccinated adults 18 years or older in 13 US States, January 2021
to April 2022. JAMA Intern Med. 182:1071–1081. 2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Chang D, Chang X, He Y and Tan KJK: The
determinants of COVID-19 morbidity and mortality across countries.
Sci Rep. 12(5888)2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Abate SM, Checkol YA and Mantefardo B:
Global prevalence and determinants of mortality among patients with
COVID-19: A systematic review and meta-analysis. Ann Med Surg
(Lond). 64(102204)2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Gray WK, Navaratnam AV, Day J, Wendon J
and Briggs TWR: COVID-19 hospital activity and in-hospital
mortality during the first and second waves of the pandemic in
England: An observational study. Thorax. 77:1113–1120.
2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
de Jesus Ascencio-Montiel I, Ovalle-Luna
OD, Rascón-Pacheco RA, Borja-Aburto VH and Chowell G: Comparative
epidemiology of five waves of COVID-19 in Mexico, March 2020-August
2022. BMC Infect Dis. 22(813)2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Mendoza-Hernandez MA, Guzman-Esquivel J,
Ramos-Rojas MA, Santillan-Luna VV, Sanchez-Ramirez CA,
Hernandez-Fuentes GA, Diaz-Martinez J, Melnikov V, Rojas-Larios F,
Martinez-Fierro ML, et al: Differences in the evolution of
clinical, biochemical, and hematological indicators in hospitalized
patients with COVID-19 according to their vaccination scheme: A
cohort study in one of the world's highest hospital mortality
populations. Vaccines (Basel). 12(72)2024.PubMed/NCBI View Article : Google Scholar
|
|
11
|
COVID-19 Tablero
México-CONACYT-CentroGeo-GeoInt-DataLab.
|
|
12
|
Myrstad M, Ihle-Hansen H, Tveita AA,
Andersen EL, Nygård S, Tveit A and Berge T: National early warning
score 2 (NEWS2) on admission predicts severe disease and
in-hospital mortality from Covid-19-a prospective cohort study.
Scand J Trauma Resusc Emerg Med. 28(66)2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
De Socio GV, Gidari A, Sicari F, Palumbo M
and Francisci D: National early warning score 2 (NEWS2) better
predicts critical Coronavirus Disease 2019 (COVID-19) illness than
COVID-GRAM, a multi-centre study. Infection. 49:1033–1038.
2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Heldt S, Neuböck M, Kainzbauer N, Shao G,
Tschoellitsch T, Duenser M, Kaiser B, Winkler M, Para C, Meier J,
et al: qSOFA score poorly predicts critical progression in COVID-19
patients. Wien Med Wochenschr. 172:211–219. 2022.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Alanís-Naranjo JM, Anguiano-Álvarez VM,
Hammeken-Larrondo EF and Olguín-Contreras G: Desempeño de PSI/PORT
y SOFA para predicción de ventilación mecánica invasiva en neumonía
por SARS-CoV-2. Med Crít. 36:155–160. 2022.
|
|
16
|
Moreno-Pérez Ó, Andrés M, León-Ramirez JM,
Sánchez-Payá J, Boix V, Gil J and Merino E: The COVID-GRAM tool for
patients hospitalized with COVID-19 in Europe. JAMA Intern Med.
181(1000)2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
George R, Mehta AA, Paul T, Sathyapalan
DT, Haridas N, Kunoor A and Ravindran GC: Validation of MuLBSTA
score to derive modified MuLB score as mortality risk prediction in
COVID-19 infection. PLoS Glob Public Health.
2(e0000511)2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Sandoval-Gutiérrez JL: A 40 años de la
descripción del índice de Kirby (PaO2/FiO2). Med Intensiva.
39(521)2015.PubMed/NCBI View Article : Google Scholar : (In Spanish).
|
|
19
|
García-Pereña L, Sesma VR, Divieso ML,
Carrascosa AL, Fuentes SV and Parra-Ruiz J: Beneficio del empleo
precoz de la oxigenoterapia nasal de alto flujo (ONAF) en pacientes
con neumonía por SARS-CoV-2. Med Clin (Barc). 158:540–542.
2022.PubMed/NCBI View Article : Google Scholar : (In English,
Spanish).
|
|
20
|
Liu CY, Chou SF, Chiang PY, Sun JT, Tsai
KC, Jaw FS, Chang CT, Fan CM, Wu YH, Lee PY, et al: The FIB-4
scores in the emergency department to predict the outcomes of
COVID-19 patients in Taiwan. Heliyon. 10(e25649)2024.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Schreiner AD, Moran WP, Zhang J,
Livingston S, Marsden J, Mauldin PD, Koch D and Gebregziabher M:
The association of fibrosis-4 index scores with severe liver
outcomes in primary care. J Gen Intern Med. 37:3266–3274.
2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Fan G, Tu C, Zhou F, Liu Z, Wang Y, Song
B, Gu X, Wang Y, Wei Y, Li H, et al: Comparison of severity scores
for COVID-19 patients with pneumonia: A retrospective study. Eur
Respir J. 56(2002113)2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Sheerin T, Dwivedi P, Hussain A and
Sivayoham N: Performance of the CURB65, NEWS2, qSOFA, SOFA, REDS,
ISARIC 4C, PRIEST and the novel COVID-19 severity scores, used to
risk-stratify emergency department patients with COVID-19, on
mortality-an observational cohort study. COVID. 3:555–566.
2023.
|
|
24
|
Ahnert P, Creutz P, Horn K,
Schwarzenberger F, Kiehntopf M, Hossain H, Bauer M, Brunkhorst FM,
Reinhart K, Völker U, et al: Sequential organ failure assessment
score is an excellent operationalization of disease severity of
adult patients with hospitalized community acquired
pneumonia-results from the prospective observational PROGRESS
study. Crit Care. 23(110)2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Becerra-Muñoz VM, Núñez-Gil IJ, Eid CM,
Aguado MG, Romero R, Huang J, Mulet A, Ugo F, Rametta F, Liebetrau
C, et al: Clinical profile and predictors of in-hospital mortality
among older patients hospitalised for COVID-19. Age Ageing.
50:326–334. 2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Kamarudin AN, Cox T and Kolamunnage-Dona
R: Time-dependent ROC curve analysis in medical research: Current
methods and applications. BMC Med Res Methodol.
17(53)2017.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Goulden R, Hoyle MC, Monis J, Railton D,
Riley V, Martin P, Martina R and Nsutebu E: qSOFA, SIRS and NEWS
for predicting inhospital mortality and ICU admission in emergency
admissions treated as sepsis. Emerg Med J. 35:345–349.
2018.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Shahsavarinia K, Moharramzadeh P, Arvanagi
RJ and Mahmoodpoor A: qSOFA score for prediction of sepsis outcome
in emergency department. Pak J Med Sci. 36:668–672. 2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Xinxin Z: MuLBSTA score for viral
pneumonia mortality. MDCalc, 2020.
|
|
30
|
World Health Organization (WHO): Clinical
Management of COVID-19: Evolving Guidelines. WHO, Geneva, 2021.
|
|
31
|
United Mexican States - Ministry of
Health: Regulations of the General Health Law concerning Health
Research. Official Gazette of the Federation: 1-31, 1987.
|
|
32
|
Miranda-Novales MG and Villasís-Keever MÁ:
El protocolo de investigación VIII. La ética de la investigación en
seres humanos. Rev Alerg Mex. 66:115–122. 2019.PubMed/NCBI View Article : Google Scholar : (In Spanish).
|
|
33
|
Charlson ME, Carrozzino D, Guidi J and
Patierno C: Charlson Comorbidity index: A critical review of
clinimetric properties. Psychother Psychosom. 91:8–35.
2022.PubMed/NCBI View Article : Google Scholar
|
|
34
|
National Center for Health Statistics:
National Center for Health Statistics (NCHS) C for DC and P (CDC):
Glossary. National Health Interview Survey, 2017.
|
|
35
|
Delgado-Enciso I, Gonzalez-Hernandez NA,
Baltazar-Rodriguez LM, Millan-Guerrero RO, Newton-Sanchez O,
Bayardo-Noriega A, Aleman-Mireles A, Enriquez-Maldonado IG,
Anaya-Carrillo MJ, Rojas-Martinez A and Ortiz-Lopez R: Association
of matrix metalloproteinase-2 gene promoter polymorphism with
myocardial infarction susceptibility in a Mexican population. J
Genet. 88:249–252. 2009.PubMed/NCBI View Article : Google Scholar
|
|
36
|
James PA, Oparil S, Carter BL, Cushman WC,
Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML,
MacKenzie TD, Ogedegbe O, et al: 2014 evidence-based guideline for
the management of high blood pressure in adults. JAMA. 311:507–520.
2014.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Jonathan B, Cilloniz C and Torres A:
Community-acquired pneumonia (non COVID-19). BMJ Best Practice,
2023.
|
|
38
|
ARDS Definition Task Force. Ranieri VM,
Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E,
Camporota L and Slutsky AS: Acute respiratory distress syndrome:
The Berlin definition. JAMA. 307:2526–2533. 2012.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Bucci T, Galardo G, Gandini O, Vicario T,
Paganelli C, Cerretti S, Bucci C, Pugliese F and Pastori D:
Research On Medical patients Admitted to the Emergency Department
(ROMA-ED) study group. Fibrosis-4 (FIB-4) index and mortality in
COVID-19 patients admitted to the emergency department. Intern
Emerg Med. 17:1777–1784. 2022.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Kuma A, Mafune K, Uchino B, Ochiai Y,
Miyamoto T and Kato A: Potential link between high FIB-4 score and
chronic kidney disease in metabolically healthy men. Sci Rep.
12(16638)2022.PubMed/NCBI View Article : Google Scholar
|
|
41
|
DeLaney M and Khoury C: Community-acquired
pneumonia in the emergency department. Emerg Med Pract. 23:1–24.
2021.PubMed/NCBI
|
|
42
|
Wang D, Willis DR and Yih Y: The pneumonia
severity index: Assessment and comparison to popular machine
learning classifiers. Int J Med Inform. 163(104778)2022.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Fine MJ, Auble TE, Yealy DM, Hanusa BH,
Weissfeld LA, Singer DE, Coley CM, Marrie TJ and Kapoor WN: A
prediction rule to identify low-risk patients with
community-acquired pneumonia. N Engl J Med. 336:243–250.
1997.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Morales-Aguirre AM, Márquez-González H,
Salazar-Rosales H, Álvarez-Valencia JL, Muñoz-Ramírez CM and
Zárate-Castañón P: Cociente PaO2/FiO2 o índice de Kirby:
Determinación y uso en población pediátrica. Residente. 10:88–92.
2015.
|
|
45
|
QxMD Software Inc: COVID-GRAM critical
Illness risk score-MDCalc. Medscape, 2020.
|
|
46
|
Liang W, Liang H, Ou L, Chen B, Chen A, Li
C, Li Y, Guan W, Sang L, Lu J, et al: Development and validation of
a clinical risk score to predict the occurrence of critical illness
in hospitalized patients with COVID-19. JAMA Intern Med.
180:1081–1089. 2020.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Gary BS: National early warning score
(NEWS) 2. MDCalc, 2020.
|
|
48
|
Teasdale G, Murray G, Parker L and Jennett
B: Adding up the glasgow coma score. In: Proceedings of the 6th
European Congress of Neurosurgery. Springer Vienna, Vienna,
pp13-16, 1979.
|
|
49
|
Smith GB, Redfern OC, Pimentel MA, Gerry
S, Collins GS, Malycha J, Prytherch D, Schmidt PE and Watkinson PJ:
The national early warning score 2 (NEWS2). Clin Med (Lond).
19(260)2019.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Royal College of Physicians: Royal College
of physicians. National early warning score (NEWS) 2: Standardising
the assessment of acute-illness severity in the NHS. Updated report
of a working party. London: RCP. London, 2017.
|
|
51
|
Ferreira M, Blin T, Collercandy N,
Szychowiak P, Dequin PF, Jouan Y and Guillon A: Critically ill
SARS-CoV-2-infected patients are not stratified as sepsis by the
qSOFA. Ann Intensive Care. 10(43)2020.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Seymour CW, Liu VX, Iwashyna TJ,
Brunkhorst FM, Rea TD, Scherag A, Rubenfeld G, Kahn JM,
Shankar-Hari M, Singer M, et al: Assessment of clinical criteria
for sepsis: For the third international consensus definitions for
sepsis and septic shock (Sepsis-3). JAMA. 315:762–774.
2016.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Guo L, Wei D, Zhang X, Wu Y, Li Q, Zhou M
and Qu J: Clinical features predicting mortality risk in patients
with viral Pneumonia: The MuLBSTA score. Front Microbiol.
10(2752)2019.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Polo TCF and Miot HA: Aplicações da curva
ROC em estudos clínicos e experimentais. J Vasc Bras.
19(e20200186)2020.
|
|
55
|
Safari S, Baratloo A, Elfil M and Negida
A: Evidence based emergency medicine; part 5 receiver operating
curve and area under the curve. Emerg (Tehran). 4:111–113.
2016.PubMed/NCBI
|
|
56
|
Unal I: Defining an optimal cut-point
value in ROC analysis: An alternative approach. Comput Math Methods
Med. 2017:1–14. 2017.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Evans HJ, Gibson NA, Bennett J, Chan SY,
Gavlak J, Harman K, Ismail-Koch H, Kingshott RN, Langley R, Morley
A, et al: British thoracic society guideline for diagnosing and
monitoring paediatric sleep-disordered breathing. Thorax.
78:s1–s27. 2023.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Artero A, Madrazo M, Fernández-Garcés M,
Miguez AM, García AG, Vieitez AC, Guijarro EC, Aizpuru EM, Gómez
MG, Manrique MA, et al: Severity scores in COVID-19 pneumonia: A
multicenter, retrospective, cohort study. J Gen Intern Med.
36:1338–1345. 2021.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Asai N, Watanabe H, Shiota A, Kato H,
Sakanashi D, Hagihara M, Koizumi Y, Yamagishi Y, Suematsu H and
Mikamo H: Efficacy and accuracy of qSOFA and SOFA scores as
prognostic tools for community-acquired and healthcare-associated
pneumonia. Int J Infect Dis. 84:89–96. 2019.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Toori KU, Qureshi MA, Chaudhry A and
Safdar MF: Neutrophil to lymphocyte ratio (NLR) in COVID-19: A
cheap prognostic marker in a resource constraint setting. Pak J Med
Sci. 37:1435–1439. 2021.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Ulloque-Badaracco JR, Salas-Tello W,
Al-kassab-Córdova A, Alarcón-Braga EA, Benites-Zapata VA, Maguiña
JL and Hernandez AV: Prognostic value of neutrophil-to-lymphocyte
ratio in COVID-19 patients: A systematic review and meta-analysis.
Int J Clin Pract. 75(e14596)2021.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Pasin L, Navalesi P, Zangrillo A, Kuzovlev
A, Likhvantsev V, Hajjar LA, Fresilli S, Lacerda MVG and Landoni G:
Corticosteroids for patients with coronavirus disease 2019
(COVID-19) with different disease severity: A meta-analysis of
randomized clinical trials. J Cardiothorac Vasc Anesth. 35:578–584.
2021.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Preetam M and Anurag A: MuLBSTA score in
COVID-19 pneumonia and prediction of 14.day mortality risk: A study
in an Indian cohort. J Family Med Prim Care. 10:223–227.
2021.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Micó-Gandia J, Pina-Belmonte A,
Aguilera-Ayllón A, Carmona-Martín M, Piles-Roger L, Martínez-Reig M
and Artero-Mora M: CO-121-MULBSTA, PSI y CURB65, predicción de
pronóstico en pacientes con COVID-19. Rev Clin Esp. 1(221)2021.(In
Spanish).
|
|
65
|
Schumacher AE, Kyu HH, Aali A, Abbafati C,
Abbas J, Abbasgholizadeh R, Abbasi MA, Abbasian M, Abd ElHafeez S,
Abdelmasseh M, et al: Global age-sex-specific mortality, life
expectancy, and population estimates in 204 countries and
territories and 811 subnational locations, 1950-2021, and the
impact of the COVID-19 pandemic: A comprehensive demographic
analysis for the global burden of disease study 2021. Lancet.
8:S0140–S6736. 2024.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Ruggeri P and Esquinas A: Fibrosis-4
(FIB-4) index and mortality in COVID-19 patients admitted to the
emergency department: a new interesting predictive index for
patients with COVID-19 disease? Intern Emerg Med. 17:2451–2452.
2022.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Estella A: Usefulness of CURB-65 and
pneumonia severity index for influenza A H1N1v pneumonia. Monaldi
Arch Chest Dis. 77:118–121. 2015.
|
|
68
|
Armiñanzas C, de Las Revillas FA, Cuadra
MG, Arnaiz A, Sampedro MF, González-Rico C, Ferrer D, Mora V,
Suberviola B, Latorre M, et al: Usefulness of the COVID-GRAM and
CURB-65 scores for predicting severity in patients with COVID-19.
Int J Infect Dis. 108:282–288. 2021.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Ahn JH and Choi EY: Expanded A-DROP score:
A new scoring system for the prediction of mortality in
hospitalized patients with community-acquired pneumonia. Sci Rep.
8(14588)2018.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Power L, Mullally D, Gibney ER, Clarke M,
Visser M, Volkert D, Bardon L, de van der Schueren MAE and Corish
CA: MaNuEL Consortium. A review of the validity of malnutrition
screening tools used in older adults in community and healthcare
settings-A MaNuEL study. Clin Nutr ESPEN. 24:1–13. 2018.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Ranganathan P and Aggarwal R: Common
pitfalls in statistical analysis: Understanding the properties of
diagnostic tests-Part 1. Perspect Clin Res. 9:40–43.
2018.PubMed/NCBI View Article : Google Scholar
|