Introduction
The endometrial tissue is generally confined to the
inner lining of the uterus and sheds during menstruation, however,
in adenomyosis, the endometrial tissue infiltrates the muscle layer
of the uterus. The condition is characterized by the presence of
endometrial tissue invasion into the myometrium, causing an
enlarged uterus and symptoms of dysmenorrhea, and heavy or
prolonged menstrual bleeding (1,2);
however, some women with adenomyosis may not experience any
noticeable symptoms. The exact cause of adenomyosis is unknown,
however hormonal imbalances, tissue injury and repair mechanisms,
and inflammation are hypothesized to play a role (3,4).
According to previous studies, mutated epithelial cells localized
in the entopic endometrial glands appear to play important roles in
the pathophysiology of adenomyosis (3,4). A
total of 21 longitudinal studies evaluating 25,600 women reported
the overall prevalence of isolated adenomyosis as 10% (5) and the incidence was reportedly highest
for women aged 41-45 years of age (6).
Treatment options for adenomyosis may include pain
management with medications, hormonal therapies, and, in severe
cases, surgical interventions such as hysterectomy or conservative
surgery (1,2,7). The
levonorgestrel-releasing intrauterine system (LNG-IUS) has
demonstrated some effectiveness (1,2,7) with
several studies revealing that LNG-IUS can effectively reduce
menstrual bleeding, pelvic pain and other symptoms associated with
adenomyosis (1,2,7).
Furthermore, it is considered a non-surgical treatment option,
making it particularly beneficial for women who wish to preserve
their fertility (8-11).
However, it is important to note that LNG-IUS may not be suitable
for all women with adenomyosis, especially in patients with an
oversized uterine cavity (uterine cavity depth, >10 cm)
(9). Levonorgestrel-releasing
intrauterine device (LNG-IUD) expulsion is the main factor
affecting long-term efficacy (12).
However, at present there are no current procedures to resolve this
issue. Therefore, the present study aimed to use a new method
(hysteroscopic LNG-IUD fixation surgery) to prevent LNG-IUD
expulsion and to improve the efficacy.
In the present study, by comparing hysteroscopic
LNG-IUD fixation intervention surgery and conventional implantation
of the LNG-IUD in patients with adenomyosis, efficacy outcomes
including the time of LNG-IUD expulsion, postoperative vaginal
bleeding time, uterine volume, dysmenorrhea, hemoglobin (HGB), and
menstrual volume were observed.
Materials and methods
Sample size calculation
Through preliminary experiments, it was revealed
that the LNG-IUD expulsion rate of the conventional method reached
50% in the treatment of patients with adenomyosis, while the
LNG-IUD expulsion rate after hysteroscopic LNG-IUD fixation was 0%.
By accepting a type 1 error i) of 0.05 and a type 2 error ii) of
0.1, the number of patients required for each group was 16. A
drop-out rate of 10% was estimated and therefore, it was calculated
that a total of 35 subjects were required.
General information
The patients with adenomyosis who underwent
hysteroscopic LNG-IUD fixation surgery were classified as the
experimental group and the patients who received conventional
implantation of the levonorgestrel-releasing intrauterine system
were classified as control group. A total of 35 patients with
adenomyosis were recruited to the Department of Gynecology of the
Affiliated Jinhua Hospital of Wenzhou Medical University (Jinhua,
China) from June 2020 to June 2022 with 17 cases in the control
group and 18 cases in the experimental group. During the
intervention period, a total of 4 cases dropped out, of which 2
cases were in the control group and 2 cases in the experimental
group, leaving 15 cases in the control group and 16 cases in the
experimental group. The present study was approved by The Medical
Ethics Committee of Affiliated Jinhua Hospital of Wenzhou Medical
University (Jinhua, China) (approval no. IBR-2020033-R), and all
patients signed informed consent.
The inclusion criteria were as follows: i) Patients
with symptoms of menorrhagia and dysmenorrhea met the criteria of
transvaginal ultrasonography [a globular shaped-uterus with
multiple areas of shadowing (increased and decreased echogenicity),
difficulty distinguishing the outer myometrium from the junctional
zone, as well as cystic changes within the junctional zone and
myometrium] (2,7); ii) patients were willing to take part
in the present study and signed informed consent; iii) patients
were female and aged 30-50 years; and iv) patients suffered from
adenomyosis and had refused hysterectomy surgery. The exclusion
criteria were as follows: i) Patients with contraindications for
progesterone therapy and hysteroscopy, including severe coagulation
disorders, severe heart, liver or kidney diseases, or mental
disorders; ii) patients who had suffered from female genital
tuberculosis, endometrial polyps, submucous myoma and endometrial
carcinoma; and iii) patients with postmenopausal status.
Treatment methods
The control group received conventional implantation
of the LNG-IUS whereby the LNG-IUS was inserted into the uterine
cavity of patients during menstruation on cycle days 5-7 by a
senior gynecologist. The patients took the bladder lithotomy
position and the operator used iodophor solution to sterilize the
vulva and vagina, and then routinely spread the disinfection towel.
The cervix was exposed using a vaginal speculum, and the cervix was
disinfected again with iodophor solution. The diluted lidocaine was
injected into the cervix at 4 and 7 o'clock directions after
grasping and stabilizing the cervix. The operator used a probe to
probe the uterine cavity after determining the position of the
uterus and then used a dilatation stick to dilate the cervix to the
number six dilation stick. Using a specialized inserter, the
operator guided the LNG-IUS through the cervix and into the uterus.
The LNG-IUD is a small T-shaped device made of flexible plain
plastic. The appropriate length of tail wire was left, with the
excess removed. Prior to withdrawal of the vaginal speculum, the
cervix was checked for active bleeding. After insertion of the
LNG-IUD, the healthcare provider performed an ultrasound exam to
confirm that the LNG-IUD was properly positioned within the
uterus.
The experimental group received hysteroscopic
LNG-IUD fixation surgery during the last days of the menstrual
cycle. To make the LNG-IUD fixing device the operator used one end
of the 3/0 Prolene line to fix the LNG-IUD longitudinal arm and
left the other end of the 3/0 Prolene, with a length of 1 cm, with
a knotted head. The body position, anesthesia method (Local
anesthesia with diluted lidocaine) and the early placement process
of the LNG-IUD fixation device in the experimental group were the
same as those in the control group. A 5.0 mm outer diameter of
hysteroscopy (Richard Wolf GmbH) was used to fix the knotted head
to the myometrium of the fundus utilizing a hysteroscopic puncture
needle under local anesthesia. The intrauterine pressure was
controlled within 100 mm Hg and the distension medium was normal
saline. Transabdominal ultrasonography was used throughout the
operation.
Participants were surveyed for follow-up at 3, 6 and
12 months after surgery either through telephone interviews or
in-person visits to the clinic. The follow-up process was carried
out until June 2023.
Evaluation indicators
The LNG-IUS expulsion was confirmed by vaginal
ultrasound examination. The time that the LNG-IUD was in place was
calculated from the first day post-surgery to the time of LNG-IUD
expulsion confirmed by vaginal ultrasound examination. The uterine
volume was calculated by color Doppler ultrasound examination using
the formula for an ovoid: Volume=D1 (cm) x D2 (cm) x D3 (cm) x0.52
ml. The depth of the uterine cavity was measured by a uterine
cavity probe during the operation. The menstrual volume was
evaluated using the menstrual blood loss score (MBLS) (13). MBLS was calculated using the
following formula: Days with heavy menstruation/total days with
heavy menstruation x the quantity of menstruation pads used=MBLS.
The quantity of menstruation pads used was evaluated according to
the following scoring system: Mini pad equivalent to 1, normal pad
equivalent to 1.5, super pad equivalent to 2 and night pad or super
plus pad equivalent to 3. The degree of dysmenorrhea was evaluated
using the visual analogue scale (VAS) (14).
A history of gonadotropin-releasing hormone agonist
(GnRH-a) treatment in the previous 6 months, a history of vaginal
delivery and cervical laceration was recorded, and the incidence of
perioperative complications such as air embolism, intravascular
absorption syndrome of surgical hysteroscopy, infection and uterine
perforation were observed.
Statistical analysis
Continuous variables of clinical characteristics
were expressed as the mean ± SD or the median
(Q1,Q3), and were evaluated using the
independent sample t-test or Kruskal-Wallis test. Dichotomous
variables between the groups were evaluated using the Fisher's
exact test. Kaplan-Meier estimates were used to generate survival
curves comparing patients who underwent hysteroscopic LNG-IUD
fixation with the control group, and it was followed by the
log-rank test. Univariable and multivariable associations [hazard
ratio (HR) and associated 95% confidence interval (CI)] with IUD
in-place variables were assessed using Cox regression analyses.
P<0.05 was considered to indicate a statistically significant
difference. Statistical analyses were performed using the
statistical software SPSS 25 (IBM Corp.). Data processing and
analysis were also performed using R version 4.3.0, along with
Storm Statistical Platform (www.medsta.cn/software).
Results
General data
A total 31 patients with adenomyosis completed the
research with 15 cases in the control group and 16 cases in the
experimental group. Basic characteristics including age, uterine
volume before treatment, uterine cavity depth, dysmenorrhea pain of
VAS and MBLS before treatment were compared between the two groups.
As demonstrated in Table I, no
significant differences were observed between the two groups. The
outcome was observed for 15.8±7.8 months post-surgery.
 | Table IComparison of the clinical
characteristics of patients before treatment. The experimental
(underwent hysteroscopic LNG-IUD fixation) and control groups
(underwent conventional implantation of LNG-IUD). |
Table I
Comparison of the clinical
characteristics of patients before treatment. The experimental
(underwent hysteroscopic LNG-IUD fixation) and control groups
(underwent conventional implantation of LNG-IUD).
| Variables | Total (n=31) | Control (n=15) | Experimental
(n=16) | Statistical test | P-value |
|---|
| Uterine volume (ml),
Mean ± SD | 300.98±125.92 | 287.79±128.41 | 313.35±126.42 | t=-0.56 | 0.581 |
| Age (years), M
(Q1, Q3) | 44.00 (41.00,
46.00) | 44.00 (40.50,
45.50) | 44.50 (41.75,
47.00) | Z=-1.15 | 0.248 |
| Uterine cavity (cm),
M (Q1, Q3) | 9.00 (9.00,
10.00) | 9.00 (8.25,
10.00) | 9.50 (9.00,
10.00) | Z=-1.72 | 0.086 |
| VAS, M
(Q1, Q3) | 5.00 (3.50,
6.00) | 6.00 (4.00,
6.00) | 4.00 (2.75,
5.25) | Z=-1.86 | 0.063 |
| MBLS, M
(Q1, Q3) | 12.00 (8.79,
18.00) | 10.00 (6.43,
14.50) | 15.00 (11.43,
18.75) | Z=-1.86 | 0.063 |
| History treatment of
GnRh-a in the past 6 months, n (%) | | | | Fisher's exact
test | 0.066 |
|
No | 12 (38.71) | 3 (20.00) | 9 (56.25) | | |
|
Yes | 19 (61.29) | 12 (80.00) | 7 (43.75) | | |
| History of vaginal
delivery, n (%) | | | | Fisher's exact
test | 1.000 |
|
No | 11 (35.48) | 5 (33.33) | 6 (37.50) | | |
|
Yes | 20 (64.52) | 10 (66.67) | 10 (62.50) | | |
| History of cervical
laceration, n (%) | | | | Fisher's exact
test | 0.113 |
|
No | 22 (70.97) | 13 (86.67) | 9 (56.25) | | |
|
Yes | 9 (29.03) | 2 (13.33) | 7 (43.75) | | |
| Menorrhagia, n
(%) | | | | Fisher's exact
test | 0.484 |
|
No | 1 (3.23) | 1 (6.67) | 0 (0.00) | | |
|
Yes | 30 (96.77) | 14 (93.33) | 16 (100.00) | | |
| Dysmenorrhea, n
(%) | | | | Fisher's exact
test | 0.600 |
|
No | 4 (12.90) | 1 (6.67) | 3 (18.75) | | |
|
Yes | 27 (87.10) | 14 (93.33) | 13 (81.25) | | |
Comparison of the therapeutic outcomes
post-treatment
The comparison of LNG-IUD expulsion rates between
the two groups after intervention measures is revealed in Table II. The LNG-IUD expulsion rate in
the experimental group (6.25%) was lower than that in the control
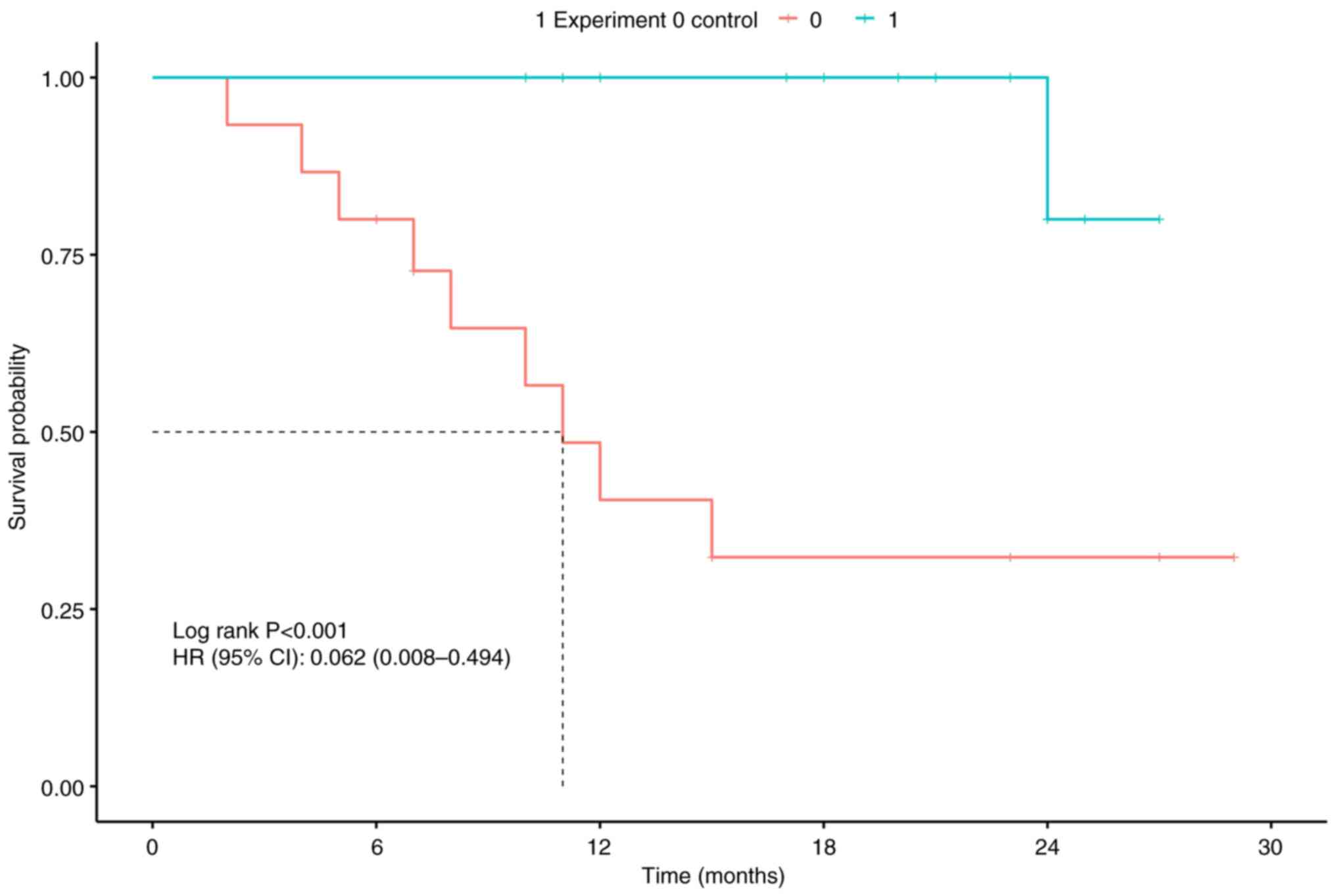
group (60%; P<0.05). The Kaplan-Meier survival curve for the
LNG-IUD is revealed in Fig. 1: The
median in-place time of IUD in the experimental group was
significantly higher than that in the control group. The LNG-IUD
in-place time was significantly longer in the experimental group
than in the control group at 20.50 (15.75, 24.00) and 10.00 (6.50,
15.00) months, respectively (P<0.05). The uterine volume of the
two groups after three months of intervention measures was not
significantly reduced and there were no statistical differences
between the two groups (P>0.05). The MBLS of both groups was
decreased after intervention measures, and the MBLS of the
experimental group after treatment demonstrated a greater reduction
than the control group, and the groups were significantly different
(P<0.05). The VAS of the two groups were both decreased after
intervention measures, however the VAS of the experimental group
after treatment was reduced more sharply, with significant
differences between the two groups (P<0.05). The time of
postoperative vaginal bleeding in the experimental group was
significantly shorter than the control group at 12.50 (9.25, 16.25)
and 120.00 (75.00,120.00) days, respectively (P<0.05). The
increased HGB after treatment in the experimental group (45.0±22.64
g/l) was higher than the control group (29.13±24.12 g/l), but there
was no statistical difference between the two groups (P=0.069).
 | Table IIComparison of the therapeutic outcomes
after treatment of the experimental and control groups. The
experimental (underwent hysteroscopic LNG-IUD fixation) and control
groups (underwent conventional implantation of LNG-IUD). |
Table II
Comparison of the therapeutic outcomes
after treatment of the experimental and control groups. The
experimental (underwent hysteroscopic LNG-IUD fixation) and control
groups (underwent conventional implantation of LNG-IUD).
| Variables | Total (n=31) | Control (n=15) | Experimental
(n=16) | Statistical test | P-value |
|---|
| Uterine volume after
three months of treatment, Mean ± SD | 279.97±117.88 | 283.50±106.27 | 276.66±131.26 | t=0.16 | 0.875 |
| Time of postoperative
vaginal bleeding (day), M (Q1, Q3) | 20.00 (10.00,
120.00) | 120.00 (75.00,
120.00) | 12.50 (9.25,
16.25) | Z=-2.65 | 0.008 |
| LNG-IUD in place
time (months), M (Q1, Q3) | 15.00 (10.00,
23.00) | 10.00 (6.50,
15.00) | 20.50 (15.75,
24.00) | Z=-2.59 | 0.009 |
| VAS after
treatment, M (Q1, Q3) | 1.00 (1.00,
2.50) | 3.00 (1.50,
3.50) | 1.00 (0.00,
1.00) | Z=-3.30 | <0.001 |
| MBLS after
treatment, M (Q1, Q3) | 1.20 (1.00,
4.17) | 3.33(2.00,
6.90) | 1.00 (1.00,
1.05) | Z=-3.56 | <0.001 |
| LNG-IUD expulsion,
n (%) | | | | - | 0.002 |
|
No | 21 (67.74) | 6 (40.00) | 15 (93.75) | | |
|
Yes | 10 (32.26) | 9 (60.00) | 1 (6.25) | | |
| HGB before
treatment, Mean ± SD | 88.55±21.69 | 91.27±24.46 | 86.0±19.19 | t=0.67 | 0.509 |
| HGB after
treatment, Mean ± SD | 125.87±18.94 | 120.4±21.39 | 131.0±15.24 | t=-1.60 | 0.121 |
| Increased HGB, Mean
± SD | 37.32±24.35 | 29.13±24.12 | 45.0±22.64 | t=-1.89 | 0.069 |
There were no complications reported, such as air
embolism, intravascular absorption syndrome of surgical
hysteroscopy, infection and uterine perforation, in the
experimental or control groups.
Cox regression analysis
Compared with the conventional implantation of
LNG-IUD, hysteroscopic LNG-IUD fixation surgery is the most
important protective factor for LNG-IUD expulsion both in single-
and multiple-factor Cox regression analyses, as demonstrated in
Tables III and IV. Multiple-factor Cox regression
analyses revealed that the LNG-IUD expulsion rate in patients with
adenomyosis was associated with hysteroscopic LNG-IUD fixation
surgery (HR, 1954.09), uterine cavity depth (HR, 16.63), MBLS (HR,
1.14), a history of GnRh-a treatment in the previous 6 months (HR,
2.10), a history of vaginal delivery (HR, 1.79) and a history of
cervical laceration (HR, 3.69; Table
IV). The conventional implantation of the LNG-IUS, uterine
cavity depth, menorrhagia before treatment, no GnRh-a treatment in
the previous 6 months, history of vaginal delivery and cervical
laceration are promoting factors of LNG-IUD expulsion.
 | Table IIISingle-factor Cox regression
analysis. |
Table III
Single-factor Cox regression
analysis.
| Variables | β | S.E | Z | P-value | HR (95% CI) |
|---|
| Age, years | -0.00 | 0.08 | -0.00 | 1.000 | 1.00
(0.86-1.17) |
| Uterine cavity
(cm) | 0.32 | 0.37 | 0.87 | 0.383 | 1.38
(0.67-2.84) |
| Uterine volume
before treatment (ml) | -0.00 | 0.00 | -0.18 | 0.855 | 1.00
(0.99-1.00) |
| VAS before
treatment | 0.20 | 0.14 | 1.44 | 0.150 | 1.22
(0.93-1.61) |
| MBLS before
treatment | -0.08 | 0.05 | -1.42 | 0.156 | 0.93
(0.83-1.03) |
| Group experience 1
control 0 | | | | | |
|
1 | | | | | Ref |
|
0 | 2.78 | 1.06 | 2.63 | 0.009 | 16.11
(2.02-128.15) |
| GnRh a | | | | | |
|
Yes | | | | | Ref |
|
No | -1.26 | 0.79 | -1.58 | 0.114 | 0.29
(0.06-1.35) |
| Vaginal
delivery | | | | | |
|
No | | | | | Ref |
|
Yes | 0.18 | 0.71 | 0.25 | 0.804 | 1.19
(0.30-4.77) |
| Cervical
laceration | | | | | |
|
No | | | | | Ref |
|
Yes | -0.18 | 0.70 | -0.26 | 0.795 | 0.83
(0.21-3.29) |
 | Table IVMultiple-factor Cox regression
analysis. |
Table IV
Multiple-factor Cox regression
analysis.
| Variables | β | S.E | Z | P-value | HR (95% CI) |
|---|
| Uterine cavity
(cm) | 2.81 | 1.68 | 1.67 | 0.095 | 16.63
(0.61-451.34) |
| Uterine volume
before treatment (ml) | -0.01 | 0.01 | -0.95 | 0.341 | 0.99
(0.98-1.01) |
| VAS before
treatment | -0.74 | 0.43 | -1.73 | 0.084 | 0.48
(0.20-1.11) |
| MBLS before
treatment | 0.13 | 0.11 | 1.23 | 0.219 | 1.14
(0.93-1.40) |
| Group experimental
1 control 0 | | | | | |
|
1 | | | | | Ref |
|
0 | 7.58 | 3.00 | 2.52 | 0.012 | 1,954.09
(5.41-705,537.98) |
| GnRh a | | | | | |
|
Yes | | | | | Ref |
|
No | 0.74 | 1.39 | 0.53 | 0.593 | 2.10
(0.14-31.75) |
| Vaginal
delivery | | | | | |
|
No | | | | | Ref |
|
Yes | 0.58 | 1.26 | 0.46 | 0.643 | 1.79
(0.15-20.99) |
| Cervical
laceration | | | | | |
|
No | | | | | Ref |
|
Yes | 1.31 | 1.23 | 1.07 | 0.287 | 3.69
(0.33-40.71) |
Discussion
Adenomyosis is a prevalent condition in the field of
gynecology, marked by the infiltration of endometrial tissue within
the muscular layer of the uterus (2). Prolonged and continuous bleeding can
result in anemia and may also lead to mental health issues due to
persistent pain during menstruation (2). Given that the condition adversely
affects the quality of life through menstrual discomfort,
reproductive health and fertility (2), it is imperative to establish long term
and effective therapies for adenomyosis. The efficacy and safety of
intrauterine placement of LNG-IUS for the treatment of adenomyosis
have been validated, most scholars consider that LNG-IUS is the
first-line treatment of adenomyosis (1,2). The
majority of patients with adenomyosis present with an enlarged
uterine volume and thickened myometrium, increasing the risk of
LNG-IUS descension and expulsion, thereby limiting its clinical
application and therapeutic efficacy (7,8). Park
et al (15) reported a
relatively high rate of LNG-IUS expulsion in patients with
adenomyosis, with rates reaching up to 37.5%. The incidence of
expulsion decreased to 21.8% following pretreatment with GnRH-a
(10). In the present study, the
expulsion rate of LNG-IUD in patients who underwent the
conventional method was as high as 60%. This may be related to the
excessive uterine volume of the patients recruited in the present
study.
A number of studies have reported on the effect of
hysteroscopic LNG-IUS fixation at present. Currently, Gynefix is an
available device specifically engineered to minimize the risk of
IUD expulsion, because Gynefix can be fixed in the myometrium
through a non-absorbable suture knot. However, it is not as
clinically effective as LNG-IUS, because it does not contain
levonorgestrel. The present study revealed the promising effects of
hysteroscopic LNG-IUD fixation surgery in prolonging the
in-position time of LNG-IUD with satisfactory results obtained. As
aforementioned, only 1 in 16 patients expelled the LNG-IUS after
follow-up. LNG-IUD in the uterine cavity was fixed through 3/0
prolene suture to decrease the rate of LNG-IUD expulsion, the
suture material used was 3/0 Prolene suture (Johnson &
Johnson). It was hypothesized that the patient with LNG-IUS
expulsion may be related to the smaller fixed knot. The incidence
of the expulsion of the LNG-IUS was comparable to that reported by
Zhang et al (12), one in 12
patients expelled the LNG-IUS, who performed polydioxanone suture
fixation of the LNG-IUS in the uterine cavity using the
hysteroscopic cold knife surgery system. However, Peng et al
(16), using a novel LNG-IUS
insertion technique, reported an LNG-IUS expulsion rate in only
10.2% of patients. Hysteroscopic LNG-IUD fixation surgery provides
a new option for patients with enlarged uterine volume, heavy
menstrual flow and a history of repeated LNG-IUD shedding.
Certain limitations of the present study must be
considered. Firstly, the results of the present study were
constrained due to the study design being a controlled clinical
trial rather than a randomized controlled trial, and therefore,
bias could not be minimized. Second, the findings of the present
study were limited by the small sample sizes in each group.
Moreover, the clinical data was sourced from a single hospital
rather than multiple centers. The results of multi-center inclusion
of more patients are more convincing. A longer follow-up time is
required to verify the long-term effectiveness of the new method.
At present, ~50 hysteroscopic LNG-IUD fixation surgeries have been
completed by the authors, and further advancements in research will
be achieved through longer follow-up times and larger sample
sizes.
Hysteroscopic LNG-IUD fixation surgery is an
efficient technique that has achieved effective LNG-IUD fixation in
the uterine cavity, with the advantages of being easy to operate,
having a short learning curve, requiring no special equipment or
instruments, causing minimal surgical trauma, having a short
operation time, allowing for quick recovery and easy removal.
Therefore, this procedure is suitable to be performed in hospitals
at all levels.
In conclusion, for patients with adenomyosis
experiencing dysmenorrhea or menorrhagia, hysteroscopic LNG-IUD
fixation surgery could offer a minimally invasive and efficient
alternative for the treatment of adenomyosis, and reduces the risk
of LNG-IUS expulsion after a mean follow-up of >1 year.
Hysteroscopic LNG-IUD fixation surgery is a favorable factor in
reducing LNG-IUD expulsion and relieving the symptoms of
dysmenorrhea or menorrhagia and is therefore a technology worth
investigating further.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by The Science and
Technology Bureau Foundation of Jinhua (grant no. 2021-4-300).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
PX, BY and JL performed the study conception and
design and provided administrative support. SL and EH provided the
study materials and recruited the patients. LM and EH collected and
assembled the data. PX and BY performed the data analysis and
interpretation. All authors wrote the manuscript. BY, JL and PX
performed all the surgical operations. All authors read and
approved the final manuscript. PX and BY confirm the authenticity
of all the raw data.
Ethics approval and consent to
participate
The present study was approved (approval no.
IBR-2020033-R) by The Medical Ethics Committee of Affiliated Jinhua
Hospital of Wenzhou Medical University (Jinhua, China). All
patients signed informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Dason ES, Chan C and Sobel M: Diagnosis
and treatment of adenomyosis. CMAJ. 193(E242)2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kho KA, Chen JS and Halvorson LM:
Diagnosis, evaluation, and treatment of adenomyosis. JAMA.
326:177–178. 2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Bulun SE, Yildiz S, Adli M, Chakravarti D,
Parker JB, Milad M, Yang L, Chaudhari A, Tsai S, Wei JJ and Yin P:
Endometriosis and adenomyosis: Shared pathophysiology. Fertil
Steril. 119:746–750. 2023.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Bulun SE, Yildiz S, Adli M and Wei JJ:
Adenomyosis pathogenesis: Insights from next-generation sequencing.
Hum Reprod Update. 27:1086–1097. 2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Mishra I, Melo P, Easter C, Sephton V,
Dhillon-Smith R and Coomarasamy A: Prevalence of adenomyosis in
women with subfertility: Systematic review and meta-analysis.
Ultrasound Obstet Gynecol. 62:23–41. 2023.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Yu O, Schulze-Rath R, Grafton J, Hansen K,
Scholes D and Reed SD: Adenomyosis incidence, prevalence and
treatment: United States population-based study 2006-2015. Am J
Obstet Gynecol. 223:94.e1–94.e10. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Schrager S, Yogendran L, Marquez CM and
Sadowski EA: Adenomyosis: Diagnosis and management. Am Fam
Physician. 105:33–38. 2022.PubMed/NCBI
|
|
8
|
Moawad G, Kheil MH, Ayoubi JM, Klebanoff
JS, Rahman S and Sharara FI: Adenomyosis and infertility. J Assist
Reprod Genet. 39:1027–1031. 2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Zhu L, Yang X, Cao B, Tang S and Tong J:
The suture fixation of levonorgestrel-releasing intrauterine device
using the hysteroscopic cold-knife surgery system: An original
method in treatment of adenomyosis. Fertil Steril. 116:1191–1193.
2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Li L, Leng J, Jia S and Lang J: Treatment
of symptomatic adenomyosis with the levonorgestrel-releasing
intrauterine system. Int J Gynaecol Obstet. 146:357–363.
2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Costanzi F, De Marco MP, Colombrino C,
Ciancia M, Torcia F, Ruscito I, Bellati F, Frega A, Cozza G and
Caserta D: The treatment with levonorgestrel releasing intrauterine
system (LNG-IUS) in patients affected by menometrorrhagia,
dysmenorrhea and adenomimyois: Clinical and ultrasonographic
reports. Eur Rev Med Pharmacol Sci. 25:3432–3439. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Zhang H, Cao B, Tong J, Guo J, Zheng J,
Zhu L, Niu Z and Chen L: An innovative surgical approach: Suture
fixation of the levonorgestrel-releasing intrauterine system in the
treatment of adenomyosis. BMC Womens Health. 22(451)2022.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Toxqui L, Pérez-Granados AM, Blanco-Rojo
R, Wright I and Vaquero MP: A simple and feasible questionnaire to
estimate menstrual blood loss: Relationship with hematological and
gynecological parameters in young women. BMC Womens Health.
14(71)2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Hawker GA, Mian S, Kendzerska T and French
M: Measures of adult pain: Visual analog scale for pain (VAS pain),
numeric rating scale for pain (NRS pain), McGill pain questionnaire
(MPQ), short-form mcgill pain questionnaire (SF-MPQ), chronic pain
grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS),
and measure of intermittent and constant osteoarthritis pain
(ICOAP). Arthritis Care Res (Hoboken). 63 (Suppl 11):S240–S252.
2011.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Park DS, Kim ML, Song T, Yun BS, Kim MK,
Jun HS and Seong SJ: Clinical experiences of the
levonorgestrel-releasing intrauterine system in patients with large
symptomatic adenomyosis. Taiwan J Obstet Gynecol. 54:412–415.
2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Peng FS, Wu MY, Yang JH, Chen SU, Ho HN
and Yang YS: Insertion of the Mirena intrauterine system for
treatment of adenomyosis-associated menorrhagia: A novel method.
Taiwan J Obstet Gynecol. 49:160–164. 2010.PubMed/NCBI View Article : Google Scholar
|