Introduction
Adhesive capsulitis, also known as frozen shoulder,
is a common pathological condition of the shoulder that affects
2-5% of the general population (1,2). The
etiology is still unknown but risk factors include female sex, age
>40 years, preceding trauma, human leukocyte antigen-B27
positivity and prolonged immobilization (3). Systemic diseases associated with
adhesive capsulitis are diabetes mellitus, stroke, thyroid
disorders and Parkinson's disease (4). Most patients with adhesive capsulitis
present with pain and development of functional restriction of both
active and passive glenohumeral joint motions, which causes
shoulder stiffness (5). These
symptoms typically begin gradually, worsen over time and then
resolve, usually within one to three years (5). The pathology of adhesive capsulitis
remains unclear but may include a chronic inflammatory response
with fibroblastic proliferation, which may be immunomodulated and
which induces capsule thickening and tightening around the shoulder
joint, thus restricting its movement (6).
Patients with adhesive capsulitis present with
insidious onset, dull and aching pain, which is often worse at
night and associated with movement and restricted passive and
active range of motion (ROM) of the shoulder in all directions,
particularly external rotation (7).
Physical examination shows diffuse tenderness over the glenohumeral
joint and limited passive and active shoulder ROM. There are three
phases of frozen shoulder: Phase I, the painful or pain-dominant
phase; Phase II, the adhesive or stiffness phase; and Phase III,
the resolution or thawing phase (1,8). The
management of adhesive capsulitis includes analgesic medications,
physical modalities, ROM exercises, manipulation under anesthesia
and surgical intervention (2,9).
Adhesive capsulitis is usually diagnosed based on
history and physical examination. There are few specific laboratory
tests that may be performed if concern for an underlying systemic
disease contributes to the condition or radiological markers for
adhesive capsulitis diagnosis. Plain radiograph, which mainly
displays the bony structure, cannot rule out other pathologies that
present with shoulder pain and limit ROM that mimic frozen
shoulder, such as biceps tendinopathy, rotator cuff tendinopathy or
tear, and subacromial and subdeltoid bursitis. These conditions can
mimic frozen shoulder, but may also occur concomitantly and cannot
be differentiated by physical examination. Thus, further
investigations, such as magnetic resonance imaging (MRI),
ultrasound or arthroscopy, should be considered for evaluating soft
tissue shoulder structure (4,10).
Numerous studies have reported on the concomitant
pathophysiology associated with primary frozen shoulder by MRI or
arthrography findings. The pathology has been attributed to
structures such as the subacromial bursa, joint capsule,
coraco-humeral ligament and synovial joint (10).
Musculoskeletal ultrasound (MSK US) is mostly used
for investigating soft tissue lesions, such as tendinopathy,
synovitis and bursitis. It has numerous advantages, such as shorter
examination times, lower cost and wider availability to patients
compared with non-MRI-compatible implants (11). Ultrasound is a noninvasive,
radiation-free diagnostic test and it does not have any
contraindications. Ultrasound imaging provides simultaneous
comparison between multiple regions and can be used to facilitate
interventional procedures (12). In
previous studies, ultrasound examinations of patients with adhesive
capsulitis have revealed increased thickness of the inferior
glenohumeral capsule, coracohumeral ligament (CHL), soft tissue in
rotator interval and axillary recess capsule (ARC) thickness
(13-15).
The diagnostic cutoff values for adhesive capsulitis showed that
the CHL thickness had a sensitivity of 77-74-95% and a specificity
of 88-99%, while the ARC thickness had a sensitivity of 68.9-93.8%
and a specificity of 90.2-98% (11,16,17).
Doppler signals and hypoechoic echotexture in the rotator interval
demonstrated high sensitivity (97%) and specificity (100%) for the
diagnosis of adhesive capsulitis (18). Ultrasound has also identified common
soft tissue pathologies in patients with shoulder pain, both with
and without limited range of motion, such as subacromial bursitis
and rotator cuff tendinopathy (15). A study exploring the prevalence of
subacromial-subdeltoid bursitis found that effusion in the
subacromial-subdeltoid bursa was frequently associated with
shoulder pain, often independently from the underlying pathology
(19). An evaluation of rotator
cuff pathology in stiff shoulder by MRI and ultrasound found that
the severity of the ROM limitation did not correspond to the
severity of the rotator cuff tear (20). Al Khayyat et al (17) found that using MSK US as a
first-line imaging modality was as reliable as MRI for diagnosing
adhesive capsulitis. This conclusion was based on the evaluation of
combined ultrasound parameters, including grey-scale changes,
thickening of shoulder ligaments, axillary pouch thickening,
alterations in the long head of the biceps tendon sheath, and
changes in the supraspinatus and infraspinatus. These findings
assist physicians in everyday clinical practice (17). Numerous studies have evaluated
shoulder structure in adhesive capsulitis and shoulder pain by
ultrasound. However, they only evaluated and reported on thickness
of ligament, capsule and soft tissue in the rotator interval. Only
a small number of studies have used MSK ultrasound to evaluate
rotator cuff disorders (19-21).
The aim of the present study was to use ultrasound to evaluate
pathologies that can occur concomitantly with adhesive
capsulitis.
Patients and methods
Study design and participants
This study was designed as a cross-sectional
descriptive study. We enrolled 96 patients with adhesive capsulitis
diagnoses from the rehabilitation or orthopedics clinic at
Srinagarind Hospital, Faculty of Medicine, Khon Kaen University
(Khon Kaen, Thailand). The inclusion criteria were a patient age of
>18 years, unilateral local shoulder pain for >3 months and
>50% limitation in active and passive glenohumeral joint ROM in
comparison to the uninvolved shoulder for greater than or equal to
two directions (21,22). Exclusion criteria were clinical
evidence of significant cervical spine disease, history of
significant trauma to the shoulder, prior surgery, dislocation or
fractures on the affected shoulder, inability to cooperate during
the examination and inability to sit in a chair for >30 min.
The sample was estimated size based on the standard
formula for prevalence studies,
where P is the expected prevalence of 0.493 based on
a previous study (19), Z is the
test statistic corresponding to a 95% confidence interval and d is
the required precision of 0.1. This gave a sample size estimate of
96 participants.
Data collection
All patients were assessed clinically and by
ultrasonographic examination of their affected shoulders. Prior
written informed consent was obtained from all patients.
Demographic data collected included age, gender, body weight and
height, underlying disease, duration of shoulder pain, site of
pain, handedness and occupation. Occupation was classified
according to work demands. Home and office work was considered
light work, while farming and technical work were considered heavy
work (23). Shoulder pain severity
was assessed using a numerical rating scale, with 0 indicating no
pain and 10 representing the most severe pain. Medical treatments,
including medications (analgesics or muscle relaxants) and types of
physical therapy (physical modalities and range-of-motion
exercises) were recorded. All participants were requested to
complete the Thai Shoulder Pain and Disability Index (SPADI)
questionnaire [Phongamwong and Choosakde (24)], which demonstrates excellent
validity and reliability. The internal consistency of the pain
subscale, disability subscale and total scale was outstanding, with
Cronbach's α coefficients of 0.92, 0.94 and 0.95, respectively,
closely matching the original English version by Roach et al
(25) (Cronbach's α=0.95). The Thai
SPADI (24) was chosen for the
present study due to its cultural relevance, language specificity
and greater applicability to the local population in Thailand. All
of this information was obtained by a physician who was not a
musculoskeletal ultrasonographic examiner.
Patients' affected shoulders were examined to
identify the area of maximal tenderness by palpating anterior,
posterior, medial and lateral shoulder sites. Both passive and
active ROM for the affected shoulders were tested. Limited
functional shoulder (ROM was defined as passive shoulder forward
flexion of 120 degrees or less, abduction of 130 degrees or less
and internal and external rotation of 60 degrees or less (26-28).
MSK US was performed on the affected shoulder by a
specialist in rehabilitation medicine who had >10 years'
experience in MSK US and was blinded to the clinical diagnoses. The
ultrasonography protocol followed standard practice with the GE
LOGIQ™ e Ultrasound System (GE Healthcare) and used a 9L-D linear
array transducer to collect images. Participants sat upright in a
chair during the ultrasonographic examination. Ultrasound
abnormalities and characteristics of the biceps tendon,
supraspinatus tendon, subdeltoid-subacromial bursa, subscapularis
tendon, infraspinatus tendon, acromioclavicular joint and
glenohumeral joint were documented according to the guidelines of
The European Society of Musculoskeletal Radiology (29). The definitions of ultrasonographic
pathology were based on international guidelines of The Outcomes
Measures in Rheumatology (OMERACT 7) (26).
Statistical analysis
For all statistical analyses, Stata software v.13
(StataCorp LP) was utilized. Continuous data were expressed as the
mean ± standard deviation (SD) if the data were normally
distributed and median with interquartile range if the data were
not normally distributed. Ordinal and categorical data were
presented as frequencies and percentages. Chi-squared tests were
conducted to determine the association between limited functional
shoulder ROM and abnormal ultrasonographic findings.
Results
Baseline characteristics
Of the 96 patients enrolled in the present study, 64
(66.6%) were female. The age of the patients (mean ± SD) was
59.0±11.8 years. Most patients were right-handed (81.0%) and most
did heavy work (52.0%) and had a normal body mass index (40.6%)
(Table I).
 | Table IBaseline characteristics. |
Table I
Baseline characteristics.
| Characteristic | Value |
|---|
| Sex | |
|
Male | 32 (33.3) |
|
Female | 64 (66.6) |
| Age, years | 59.0±11.8 |
| BMI,
kg/m2 | 23.3±3.4 |
|
Underweight | 4 (4.1) |
|
Normal | 39 (40.6) |
|
Overweight | 28 (29.1) |
|
Obese | 25 (26.0) |
| Handedness | |
|
Right | 77 (81.0) |
|
Left | 18 (18.9) |
| Underlying
diseases | 70 (72.9) |
|
DM | 19 (19.7) |
|
HT | 29 (30.2) |
|
DLP | 27 (28.1) |
|
Others | 39 (40.6) |
| Occupation | |
|
Light work
(home and office work) | 29 (30.2) |
|
Heavy work
(farming or technician) | 50 (52.0) |
|
None | 17 (17.7) |
Shoulder pain characteristics
Table II shows that
most shoulder pain occurred on the dominant side (57.2%). The
median duration of shoulder pain was 4 months. The mean numeric
pain severity rating was 6.8 (severe pain). A large majority,
(82.1%), of patients had experienced previous treatments, including
medications and/or physical therapy and/or exercise, before their
ultrasonographic examination. The most common area of maximal
tenderness was the anterior region. A sizeable number of patients
had SPADI scores in the severe range (36.4%) and very severe range
(33.3%).
 | Table IIShoulder characteristics. |
Table II
Shoulder characteristics.
| Characteristic | Value |
|---|
| Shoulder pain
site | |
|
Dominant | 55 (57.2) |
|
Non-dominant | 41 (42.7) |
| Duration of pain,
months | 4 (3-6) |
| Severity on the
NRS | 6.8±2.0 |
| Previous
treatment | |
|
None | 17 (17.7) |
|
Self-exercise | 9 (9.3) |
|
Medications
(analgesic or muscle relaxant) | 27 (28.1) |
|
Physical
therapy: Modality + ROME | 18 (18.7) |
|
Medication
and physical therapy | 25 (26.0) |
| Area of maximal
tenderness | |
|
None | 14 (14.5) |
|
Anterior | 65 (67.7) |
|
Posterior | 11 (11.4) |
|
Lateral | 6 (6.2) |
| Active/passive
ROM | |
|
Forward
flexion |
130.9±32.8/139.3±31.0 |
|
Abduction |
117.1±42.1/126.1±40.2 |
|
Internal
rotation |
34.2±21.6/40.3±23.0 |
|
External
rotation |
71.1±16.0/74.7±16.1 |
| SPADI score | 54.3±17.8 |
|
Mild
(0-20) | 2 (2.0) |
|
Moderate
(21-40) | 20 (20.8) |
|
Severe
(41-60) | 35 (36.4) |
|
Very severe
(61-80) | 32 (33.3) |
|
Extremely
severe (81-100) | 7 (7.2) |
Shoulder ultrasound findings
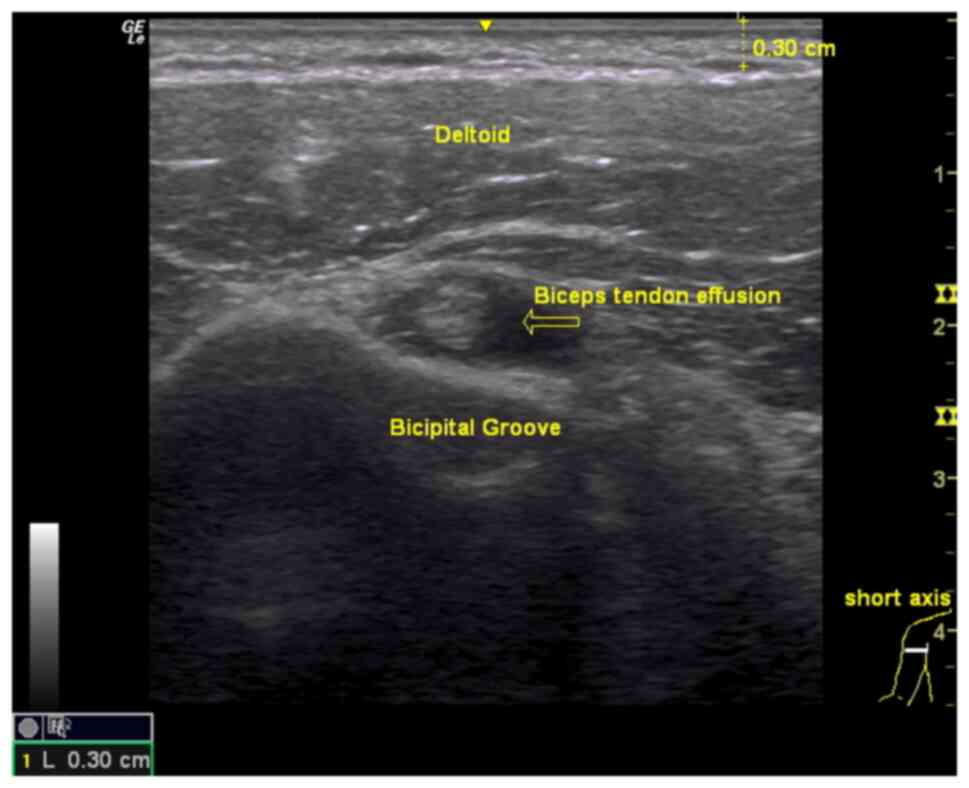
Abnormal shoulder ultrasound findings were found in
all 96 cases (100%). On ultrasonographic imaging, the top three
abnormalities were biceps tendon effusion (71.8%) (Fig. 1), positive dynamic supraspinatus
impingement (56.2%) and subdeltoid-subacromial bursitis (47.9%)
(Table III) The relationship
between limited functional shoulder ROM and common abnormal
ultrasonographic findings was analyzed. The results showed that a
limited passive ROM (PROM) in shoulder flexion of ≤120 degrees was
significantly associated with positive dynamic supraspinatus
impingement. Similarly, a limited PROM in shoulder abduction of
≤130 degrees was significantly associated with subdeltoid and
subacromial bursitis, as well as positive dynamic supraspinatus
impingement. In addition, a limited PROM in shoulder internal
rotation of ≤60 degrees was significantly associated with positive
dynamic supraspinatus impingement (Table IV).
 | Table IIIUltrasound findings. |
Table III
Ultrasound findings.
| Structural
feature | Value |
|---|
| Biceps tendon | |
|
Normal
echogenicity | 27 (28.1) |
|
Effusion | 69 (71.8) |
|
Calcification | 2 (2.0) |
| Subscapularis
tendon | |
|
Normal
echogenicity | 85 (88.5) |
|
Tendinosis | 6 (6.2) |
|
Partial
rupture | 1 (1.0) |
|
Calcification | 4 (4.1) |
| Acromioclavicular
joint | |
|
Normal
echogenicity | 88 (91.6) |
|
Effusion | 3 (3.1) |
|
Calcification | 4 (4.1) |
|
Increase
vascularity | 1 (1.0) |
| Supraspinatus
tendon | |
|
Normal
echogenicity | 48 (50.0) |
|
Tendinosis | 37 (38.5) |
|
Partial
rupture | 7 (7.2) |
|
Full
rupture | 1 (1.0) |
|
Calcification | 10 (10.4) |
|
Irregular
cortex | 1 (1.4) |
|
Subdeltoid-subacromial bursa | |
|
Normal
echogenicity | 50 (52.0) |
|
Bursitis | 46 (47.9) |
| Infraspinatus
tendon | |
|
Normal
echogenicity | 82 (85.4) |
|
Tendinosis | 2 (2.0) |
|
Partial
rupture | 2 (2.0) |
|
Calcification | 8 (8.3) |
|
Effusion | 2 (2.0) |
| Glenohumeral
joint | |
|
Normal
echogenicity | 79 (82.2) |
|
Effusion | 7 (7.2) |
|
Calcification | 11 (11.4) |
| Dynamic
supraspinatus impingement | |
|
Negative | 38 (39.5) |
|
Positive | 54 (56.2) |
|
Non-applicable | 4 (4.1) |
 | Table IVRelationship between limited
functional ROM and abnormal ultrasound. |
Table IV
Relationship between limited
functional ROM and abnormal ultrasound.
| ROM limit/abnormal
ultrasound finding | Yes | No | P-value |
|---|
| Flexion (PROM
≤120) | 36 (37.5) | | |
|
Biceps
tendon effusion | 25 (69.4) | 11 (30.6) | 0.68 |
|
Supraspinatus
tendon - tendinosis | 15 (41.7) | 21 (58.3) | 0.63 |
|
Subdeltoid-subacromial
bursa - bursitis | 15 (41.7) | 21 (58.3) | 0.34 |
|
Dynamic
supraspinatus impingement positive | 25 (57.6) | 8 (24.2) | 0.013 |
| Abduction (PROM
≤130) | 50 (52.0) | | |
|
Biceps
tendon effusion | 33 (66.0) | 17 (34.0) | 0.18 |
|
Supraspinatus
tendon-tendinosis | 18 (36.0) | 32 (64.0) | 0.59 |
|
Subdeltoid-subacromial
bursa - bursitis | 19 (38.0) | 31 (62.0) | 0.043 |
|
Dynamic
supraspinatus impingement positive | 34 (72.3) | 13 (27.7) | 0.007 |
| Internal rotation
(PROM ≤60) | 81 (84.3) | | |
|
Biceps
tendon effusion | 60 (74.0) | 21 (35.9) | 0.27 |
|
Supraspinatus
tendon-tendinosis | 30 (37.0) | 51 (63.0) | 0.48 |
|
Subdeltoid-subacromial
bursa - bursitis | 40 (49.4) | 41 (50.6) | 0.50 |
|
Dynamic
supraspinatus impingement positive | 51 (62.4) | 27 (34.6) | 0.002 |
| External rotation
(PROM ≤60) | 25 (26.0) | | |
|
Biceps
tendon effusion | 15 (60.0) | 10 (40.0) | 0.13 |
|
Supraspinatus
tendon - tendinosis | 10 (40.0) | 15 (60.0) | 0.86 |
|
Subdeltoid-subacromial
bursa - bursitis | 10 (40.0) | 15 (60.0) | 0.36 |
|
Dynamic
supraspinatus impingement positive | 17 (73.9) | 6 (26.1) | 0.09 |
Discussion
The present study was the first to evaluate both
rotator cuff and non-rotator cuff parameters, including
acromioclavicular joint, biceps tendon, subscapularis tendon,
supraspinatus tendon, subdeltoid-subacromial bursa, infraspinatus
tendon, glenohumeral joint and the dynamic supraspinatus
impingement test. As expected, abnormal ultrasound findings were
present in all of the cases, as most had severe shoulder pain. A
sizeable number of patients had SPADI scores in the severe range
and most did heavy work. The most common abnormal ultrasonographic
finding in the present cohort of patients with adhesive capsulitis
was biceps tendon effusion. This was consistent with the most
common physical examination finding of maximal tenderness in the
anterior shoulder region, also found in previous studies (30,31).
In cases of adhesive capsulitis, effusion can be easily detected in
the region of the long head of the biceps tendon, often appearing
as a target sign. However, glenohumeral joint effusion may be most
reliably detected and quantified in the posterior glenohumeral
joint recess, where it is typically found less frequently than in
the long head of the biceps tendon region (30,32).
According to the present results, effusion is detected more
frequently in the region of the long head of the biceps tendon
(71.8%) than in the glenohumeral joint (7.2%). Park et al
(30) suggested biceps tendon
effusion may be due to joint shrinkage in adhesive capsulitis
pushing the joint fluid to another space, such as the biceps long
head tendon sheath. However, biceps tendon effusion is not
associated with biceps pathology alone and may also be found in
rotator cuff disease (33) or
subacromial impingement (34).
Therefore, it is essential to correlate these findings with
physical examinations simultaneously.
The second most common abnormal ultrasonographic
finding in the present study was positive dynamic supraspinatus
impingement. There were 3 cases exhibiting severe limitations in
abduction ROM and 1 case diagnosed with a full-thickness tear of
the supraspinatus tendon. More than half of the patients in the
present study had a positive dynamic impingement test, consistent
with Tandon et al (14), who
found high sensitivity for dynamic supraspinatus impingement in
adhesive capsulitis. Kim et al (35) also found that subacromial gliding
limitation of the supraspinatus tendon is associated with decreased
shoulder joint capacity, an important feature of adhesive
capsulitis. However, positive dynamic supraspinatus impingement
findings are known to occur in numerous other pathologies, such as
rotator cuff tears, impingement syndromes, tendinitis and
subacromial bursitis (14).
Therefore, it is important to compare ultrasound results with
physical examinations to identify a possible diagnosis.
Stella et al (31) found subacromial-subdeltoid bursitis
in 11.3% of patients with adhesive capsulitis, whereas in the
present study, the extent of bursitis was 42.2%. However, their
study did not include patients' occupations. The difference between
the two studies may arise from the fact that the majority of
patients in the present study engaged in heavy work, potentially
resulting in repetitive severe trauma to the shoulder with a higher
prevalence of subdeltoid-subacromial bursitis.
The relationship between limited functional shoulder
ROM and abnormal ultrasonographic findings was also investigated in
the present study. It was hypothesized that limited shoulder
flexion may result from pathology in the biceps tendon, as the
biceps tendon plays a significant role in this motion (36). The present study showed that limited
shoulder flexion was associated with positive dynamic
supraspinatus, which differed from the initial hypothesis of the
present study. If patients present with limited shoulder flexion,
the pathology may involve not only the biceps tendon but also
positive dynamic supraspinatus impingement. Restricted shoulder
abduction could also result from supraspinatus tendon pathology and
nearby structures, as this tendon plays an important role in this
motion (37). This aligns with the
findings of the present study, which showed that limited shoulder
abduction was significantly associated with subdeltoid and
subacromial bursitis, as well as positive dynamic supraspinatus
impingement. It resembles the assessment of specific tests, such as
the Jobe test (38). It has also
been previously reported that posterior capsule shoulder
thickening, as well as muscle spasm of the posterior deltoid,
infraspinatus and teres minor can cause internal rotation
limitation (39). The
coraco-humeral ligament, which is usually the first structure to be
affected in adhesive capsulitis, restricts mainly external rotation
and additionally internal rotation of the shoulder joint (40). However, in the present study, it was
found that the most common ultrasonographic abnormality in limited
shoulder internal rotation was positive dynamic supraspinatus
impingement. The results of the present study thus differed from
the initial hypothesis. Therefore, it should be cautioned that
relying solely on physical examination may not accurately indicate
the true pathology. It may be recommended to combine physical
examination with simultaneous ultrasound for a more comprehensive
diagnosis of any shoulder abnormalities.
The study by Malavolta et al (41) from 2018 found that Asian ethnicity
is an independent risk factor for the development of adhesive
capsulitis. However, there is no published study showing any
inter-ethnic difference in the MSK US examination result in
patients with adhesive capsulitis. This provides an interesting
area for future research. In the present study, all patients had
abnormal ultrasound findings, and it was therefore not possible to
comparatively analyze factors associated with shoulder
ultrasonographic abnormalities. It may be recommended that
ultrasound should ideally be conducted in every case of adhesive
capsulitis and it is important to compare ultrasound results with
physical examinations to identify a possible diagnosis.
The present study had certain limitations that are
worth mentioning. First, the cross-sectional design limits the
determination of the temporal relationship of adhesive capsulitis
with the development of ultrasonographic abnormalities and it also
lacks a comparison group. Further studies are required with a
cohort of patients from multiple hospitals and potentially multiple
countries. Furthermore, most patients had undergone prior
treatments that could have influenced the ultrasound findings. In
addition, the associations between shoulder ultrasound
abnormalities and severity of their underlying disease or various
psychosocial factors such as anxiety, stress and poor sleep were
not determined in the present study. Consequently, future research
should address these variables to assess their potential impact on
shoulder pain or shoulder ultrasound abnormalities and should also
compare them to gold standard tests such as arthroscopy or MRI in
controlled trials with a larger sample size than that of the
present study. Furthermore, in the present study, MSK US was
performed by only one specialist, which is a limitation due to the
absence of confirmation from a second specialist. It may be
encouraged that physicians perform ultrasound in patients with
adhesive capsulitis and compare ultrasound results with physical
examinations to identify a possible diagnosis. However, it should
be noted that an abnormal ultrasonographic finding is not a
definite diagnosis for adhesive capsulitis in each patient, and the
final diagnosis should be based on the individual patient's
clinical and overall ultrasonographic findings.
In conclusion, in the present study, abnormal
shoulder ultrasonographic findings were found to be prevalent in
individuals with adhesive capsulitis. The most common abnormal
ultrasonographic imaging findings in adhesive capsulitis were
biceps tendon effusion, positive dynamic supraspinatus impingement
and subdeltoid-subacromial bursitis.
Acknowledgements
The authors would like to acknowledge Professor John
F Smith for editing the manuscript via the KKU Publication Clinic,
Srinagarind Hospital, Faculty of Medicine, Khon Kaen University,
Khon Kaen, Thailand.
Funding
Funding: This study was supported by the Faculty of Medicine
Research Fund, Khon Kaen University (grant no. IN66032).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
AM and PS confirm the authenticity of all the raw
data. AM, JS and PS designed the study. AM and JS interpreted the
data. AM and PS wrote the manuscript. AM and JS performed
statistical analysis. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was reviewed and approved by the Khon Kaen
University Ethics Committee for Human Research (approval no.
HE651371). All participants provided written informed consent to
participate in the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare they have no competing
interests.
References
|
1
|
Dias R, Cutts S and assoud S: Frozen
shoulder. BMJ. 331:1453–1456. 2005.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Safran O, El-Haj M, Leibowitz G, Beyth S,
Furman Z, Milgrom C and Kandel L: Should patients with frozen
shoulder be screened for diabetes mellitus? Orthop J Sports Med.
5(2325967117716450)2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Le HV, Lee SJ, Nazarian A and Rodriguez
EK: Adhesive capsulitis of the shoulder: Review of pathophysiology
and current clinical treatments. Shoulder Elbow. 9:75–84.
2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Mezian K, Coffey R and Chang KV: Frozen
Shoulder. In: StatPearls. StatPearls Publishing, Treasure Island,
FL, 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482162/.
|
|
5
|
Hannafin JA and Chiaia TA: Adhesive
capsulitis. A treatment approach. Clin Orthop Relat Res.
372:95–109. 2000.PubMed/NCBI
|
|
6
|
Hand GC, Athanasou NA, Matthews T and Carr
AJ: The pathology of frozen shoulder. J Bone Joint Surg Br.
89:928–932. 2007.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Walmsley S, Osmotherly PG and Rivett DA:
Movement and pain patterns in early stage primary/idiopathic
adhesive capsulitis: A factor analysis. J Physiother. 100:336–343.
2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Brun S: Idiopathic frozen shoulder. Aust J
Gen Pract. 48:757–761. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Redler LH and Dennis ER: Treatment of
adhesive capsulitis of the shoulder. J Am Acad Orthop Surg.
27(e544)2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ryan V, Brown H, Minns Lowe CJ and Lewis
JS: The pathophysiology associated with primary (idiopathic) frozen
shoulder: A systematic review. BMC Musculoskele Disord.
17(340)2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Fields BKK, Skalski MR, Patel DB, White
EA, Tomasian A, Gross JS and Matcuk GR Jr: Adhesive capsulitis:
Review of imaging findings, pathophysiology, clinical presentation,
and treatment options. Skeletal Radiol. 48:1171–1184.
2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Özçakar L, Kara M, Chang KV, Çarl AB,
Akkaya N, Tok F, Chen WS, Wang TG, Tekin L, Ulaşl AM, et al:
Nineteen reasons why physiatrists should do musculoskeletal
ultrasound: EURO-MUSCULUS/USPRM recommendations. Am J Phys Med
Rehabil. 94:e45–49. 2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Homsi C, Bordalo Rodrigues M, da Silva JJ
and Stump XM: Ultrasound in adhesive capsulitis of the shoulder: Is
assessment of the coracohumeral ligament a valuable diagnostic
tool? Skelet Radiol. 35:673–678. 2006.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Tandon A, Dewan S, Bhatt S, Jain AK and
Kumari R: Sonography in diagnosis of adhesive capsulitis of the
shoulder: A case-control study. J Ultrasound. 20:227–236.
2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Jiang L, He J, Chen CPC, Xie D, Mai Y, Yue
B and Dou Z: The ultrasonographic features of shoulder pain
patients in a tertiary hospital in South China. Biomed Res Int.
2020(e3024793)2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Do JG, Hwang JT, Yoon KJ and Lee YT:
Correlation of ultrasound findings with clinical stages and
impairment in adhesive capsulitis of the shoulder. Orthop J Sports
Med. 9(23259671211003675)2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Al Khayyat SG, Falsetti P, Conticini E,
Frediani B, Galletti S and Stella SM: Adhesive capsulitis and
ultrasound diagnosis, an inseparable pair: A novel review. J
Ultrasound. 26:369–384. 2023.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Lee JC, Sykes C, Saifuddin A and Connel D:
Adhesive capsulitis: Sonographic changes in the rotator cuff
interval with arthroscopic correlation. Skelet Radiol. 34:522–527.
2005.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Draghi F, Scudeller L, Draghi AG and
Bortolotto C: Prevalence of subacromial-subdeltoid bursitis in
shoulder pain: An ultrasonographic study. J Ultrasound. 18:151–158.
2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Ueda Y, Sugaya H, Takahashi N, Matsuki K,
Kawai N, Tokai M, Onishi K and Hoshika S: Rotator cuff lesions in
patients with stiff shoulders: A prospective analysis of 379
shoulders. J Bone Joint Surg Am. 97:1233–1237. 2015.PubMed/NCBI View Article : Google Scholar
|
|
21
|
El Naggar TEDM, Maaty AIE and Mohamed AE:
Effectiveness of radial extracorporeal shock-wave therapy versus
ultrasound-guided low-dose intra-articular steroid injection in
improving shoulder pain, function, and range of motion in diabetic
patients with shoulder adhesive capsulitis. J Shoulder Elbow Surg.
29:1300–1309. 2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Çelik D and Kaya Mutlu E: Does adding
mobilization to stretching improve outcomes for people with frozen
shoulder? A randomized controlled clinical trial. Clin Rehabil.
30:786–794. 2016.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Abate M, Schiavone C and Salini V:
Sonographic evaluation of the shoulder in asymptomatic elderly
subjects with diabetes. BMC Musculoskelet Disord.
11(278)2010.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Phongamwong C and Choosakde A: Reliability
and validity of the Thai version of the Shoulder Pain and
Disability Index (Thai SPADI). Health Qual Life Outcomes.
13(136)2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Roach KE, Budiman-Mak E, Songsiridej N and
Lertratanakul Y: Development of a shoulder pain and disability
index. Arthritis Care Res. 4:143–149. 1991.PubMed/NCBI
|
|
26
|
Wakefield RJ, Balint PV, Szkudlarek M,
Filippucci E, Backhaus M, D'Agostino MA, Sanchez EN, Iagnocco A,
Schmidt WA, Bruyn GA, et al: Musculoskeletal ultrasound including
definitions for ultrasonographic pathology. J Rheumatol.
32:2485–2487. 2005.PubMed/NCBI
|
|
27
|
Namdari S, Yagnik G, Ebaugh DD, Nagda S,
Ramsey ML, Williams GR Jr and Mehta S: Defining functional shoulder
range of motion for activities of daily living. J Shoulder Elbow
Surg. 21:1177–1183. 2012.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Doğan M, Koçak M, Onursal Kılınç Ö, Ayvat
F, Sütçü G, Ayvat E, Kılınç M, Ünver Ö and Aksu Yıldırım S:
Functional range of motion in the upper extremity and trunk joints:
Nine functional everyday tasks with inertial sensors. Gait Posture.
70:141–147. 2019.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Klauser AS, Tagliafico A, Allen GM, Boutry
N, Campbell R, Court-Payen M, Grainger A, Guerini H, McNally E,
O'Connor PJ, et al: Clinical indications for musculoskeletal
ultrasound: A Delphi-based consensus paper of the European Society
of musculoskeletal Radiology. Eur Radiol. 22:1140–1148.
2012.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Park I, Lee HJ, Kim SE, Bae SH, Lee KY,
Park KS and Kim YS: Evaluation of the effusion within biceps long
head tendon sheath using ultrasonography. Clin Orthop Surg.
7:351–358. 2015.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Stella SM, Gualtierotti R, Ciampi B,
Trentanni C, Sconfienza LM, Del Chiaro A, Pacini P, Miccoli M and
Galletti S: Ultrasound features of adhesive capsulitis. Rheumatol
Ther. 9:481–495. 2022.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Zubler V, Mamisch-Saupe N, Pfirrmann CW,
Jost B and Zanetti M: Detection and quantification of glenohumeral
joint effusion: Reliability of ultrasound. Eur Radiol.
21:1858–1864. 2011.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Hanusch BC, Makaram N, Utrillas-Compaired
A, Lawson-Smith MJ and Rangan A: Biceps sheath fluid on shoulder
ultrasound as a predictor of rotator cuff tear: Analysis of a
consecutive cohort. J Shoulder Elbow Surg. 25:1661–1667.
2016.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Chang KV, Wu WT and Özçakar L: Association
of bicipital peritendinous effusion with subacromial impingement: A
dynamic ultrasonographic study of 337 shoulders. Sci Rep.
6(38943)2016.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Kim I, Yi JH, Lee J, Bae JH, Lim JK, Yoon
JP and Jeon IH: Limited subacromial gliding of the supraspinatus
tendon during dynamic ultrasonography can predict a decrease in
capacity and MR arthrographic features of the shoulder joint. Eur
Radiol. 22:2365–2370. 2012.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Diplock B, Hing W and Marks D: The long
head of biceps at the shoulder: A scoping review. BMC Musculoskelet
Disord. 24(232)2023.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Jeno SH, Munjal A and Schindler GS:
Anatomy, Shoulder and Upper Limb, Arm Supraspinatus Muscle. In:
StatPearls. StatPearls Publishing, Treasure Island, FL, 2024.
|
|
38
|
Gillooly JJ, Chidambaram R and Mok D: The
lateral Jobe test: A more reliable method of diagnosing rotator
cuff tears. Int J Shoulder Surg. 4:41–43. 2010.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Saldiran TC and Yilmaz O: Which one is the
most limited movement in restricted shoulder joint. J Hum Mov.
20:72–78. 2019.
|
|
40
|
Cho CH, Kim DH, Kim DH, Choi BC, Kim SG,
Lee DG and Cho JH: Comparative efficacy of rotator interval versus
posterior capsule approach intraarticular corticosteroid injections
for primary frozen shoulder: A single-blind, Randomized trial. Pain
Physician. 25:313–321. 2022.PubMed/NCBI
|
|
41
|
Malavolta EA, Gracitelli MEC, Ribeiro
Pinto GM, Freire da Silveira AZ, Assunção JH and Ferreira Neto AA:
Asian ethnicity: A risk factor for adhesive capsulitis? Rev Bras
Ortop. 53:602–606. 2018.PubMed/NCBI View Article : Google Scholar
|