1. Introduction
Artificial intelligence (AI) has become increasingly
significant in the realm of innovation in the healthcare industry
in the last few years (1). AI, in
its broadest sense, is a branch of computer science that aims to
replace human intelligence using computer systems (2). This replication is achieved through
sophisticated pattern recognition, often at speeds and scales that
surpass human abilities. Proponents ardently argue that AI will
fundamentally transform healthcare for individuals and communities
(3). Alongside AI, subsets such as
machine learning (ML) and deep learning (DL) have seen significant
advancements in recent years, leading to groundbreaking
developments. Currently, AI is predominantly employed to enhance
the pace and quality of healthcare. Some of the present
applications of AI in this particular field include AI-assisted
algorithms to analyze and interpret medical imaging data, including
X-rays, MRIs and CT scans, to aid healthcare professionals in rapid
and accurate diagnoses (4). The
digitization of health-related data, coupled with rapid
technological advancements, is driving the advancement of AI
applications in healthcare (5).
There is a substantial number of reviews that discussed the impact
of AI on healthcare (4,5). One of them is a review by Rajpurkar
et al (5) on AI in
personalized medicine, which shows how AI is revolutionizing
healthcare by tailoring therapies to individuals' genetic,
environmental and lifestyle data. AI may improve the diagnosis of
health conditions, treatment choices and health outcomes, notably
in genomics and precision medicine (PM); the review also highlights
how AI may save healthcare costs, boost efficiency and improve
patient care, but it also raises data privacy and clinical
validation issues (5).
The implementation of AI in healthcare systems
represents a complex integration of multimodal systems that
necessitates fundamental advancements in areas such as privacy,
large-scale machine learning, optimization and model performance
(6). To successfully incorporate AI
into healthcare, two key concepts must be addressed: Data with
security and analytics with insights. Regarding data and security,
complete transparency and trust are essential for effective
integration. Similarly, the role of data analytics and insight is
crucial. AI has the capability to synthesize inputs from diverse
unstructured and structured sources to aid in making more informed
decisions, finding better solutions and fostering reasoned
discussions in multimodal applications - for instance, enabling
clinicians to make more accurate diagnoses and nurses to develop
sensible care and follow-up plans (7). Over the past decade, rapid
advancements in AI have unlocked the possibility of using
aggregated healthcare data to construct sophisticated models. These
models may automate diagnosis processes and enable a more precise
approach to healthcare by tailoring treatments and allocating
resources with utmost efficiency in a timely, effective and dynamic
manner (7,8). The development of such advanced AI
models that deliver high-quality healthcare applications requires
skilled professionals equipped with cutting-edge technology.
An enormous amount of untapped data that could
significantly impact our health exists outside the medical system.
For instance, factors such as lifestyle, diet, environment, medical
history and population health have significantly influenced health
outcomes and collectively account for ~60% of the determinants of
health. By contrast, genetics are responsible for only ~30% and the
actual health care received contributes only 10% (9). Throughout an individual's lifetime,
huge amounts of personal and health data are being generated. If
utilized appropriately, these data can unlock unique insights
leading to a longer and healthier life. Taking cancer as an
example, it involves complex interactions among cancer cells,
normal cells, surrounding tissue, the immune system and the
underlying molecular changes.
In the near future, it will likely be possible to
create dynamic visualizations of tumor development by employing
computer modeling and data integration techniques to amalgamate
these layers of information for more accurate diagnoses and
improved prognoses (10,11). With optimism, it can be predicted
that the advent of sophisticated AI technology and computational
systems will bring a more comprehensive understanding of tumor
biology within our grasp. The healthcare ecosystem is beginning to
recognize the critical role that AI-powered tools will play in
next-generation healthcare technologies. AI can enhance almost
every aspect of healthcare applications and delivery (12). For instance, the cost reductions
that AI may bring to the healthcare system are a significant
motivator of AI application adoption. In 2026, it is predicted that
AI applications would save the United States alone $150 billion in
yearly healthcare expenses (5). A
significant portion of these cost savings comes from shifting from
a reactive to a proactive strategy, with an emphasis on health
prevention of illnesses rather than treatment (13). In the present review, the aim is to
provide a comprehensive analysis of the current knowledge of AI
applications in healthcare, with a particular focus on novel and
emerging trends. Unlike previous reviews that often focus on a
specific application, this article uniquely integrates insights
from multiple domains, including diagnostic AI, patient care
optimization and personalized medicine. Furthermore, the evolving
regulatory and ethical considerations are highlighted, enabling
readers to grasp the multifaceted impacts of AI on the future of
healthcare.
2. AI
It is widely agreed that the term ‘AI’ indicates the
execution by computer of activities that are typically associated
with intelligent humans (4). ML
algorithms are at the heart of AI. Algorithms are converted to
code, which contains instructions for fast analysis and translation
of input into conclusions, information or other outputs. AI is
fueled by massive amounts of data and the ability to analyze that
data in a short period of time. An AI system is a machine-based
system that, given a set of human-defined goals, can make a
prediction, suggestion or choice that may have an impact on real or
virtual surroundings. Automated intelligence systems are intended
to function with various degrees of autonomy. When it comes to data
definition and analysis, ML is a subset of AI methods that is based
on the application of statistical and mathematical modeling
techniques (3). These newly
acquired patterns are then used to execute or steer specific
activities, as well as to create predictions.
ML may be divided into three types of learning based
on how it learns from data: Supervised learning, unsupervised
learning and reinforced learning (14). A model is trained using labeled data
(where the outcome variable is known) and the model infers a
function from the data that can be used to predict various outputs
based on different inputs. In contrast to supervised learning,
unsupervised learning includes the detection of hidden patterns in
data by a computer rather than the labeling of data. Reinforcement
learning is a method of teaching a machine to learn through trial
and error in order to achieve a goal, for which the machine is
either ‘rewarded’ or ‘punished’ based on whether its conclusions
help or hinder goal achievement (5).
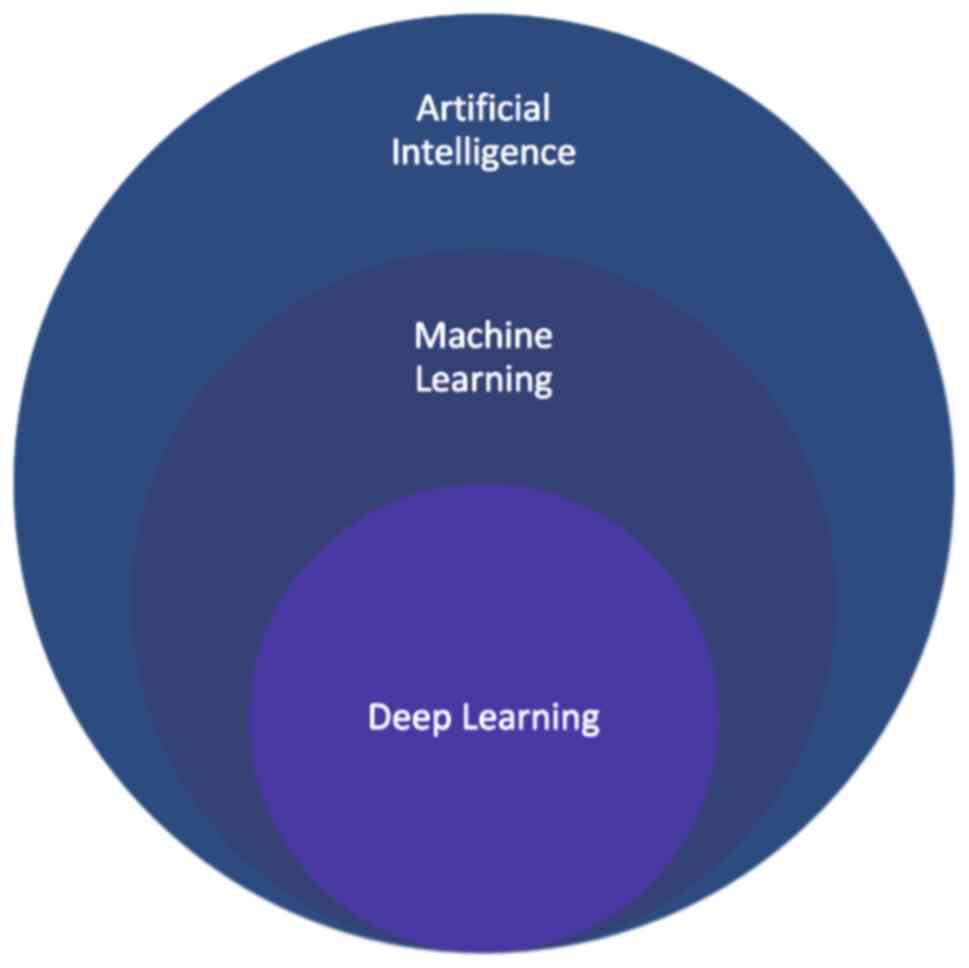
DL, also known as ‘deep structured learning’, is a
subset of machine learning that utilizes multi-layered neural
networks to extract features from data in a hierarchical fashion
manner (Fig. 1). DL can be
conducted under supervised, unsupervised or semi-supervised
settings. It is commonly associated with the need for large volumes
of data to effectively train models. Many machine learning
techniques are rooted in data-driven methodologies that depend on
vast quantities of high-quality data, often referred to as ‘big
data’ (BD) to yield accurate results. Consequently, complex
information is rapidly accumulated, resulting in the need for
terabytes or even petabytes of storage capacity (15).
3. Medical applications of AI
AI is rapidly becoming an important component of
contemporary healthcare, due to recent advancements in computer
science and informatics, among other factors. AI algorithms and
applications powered by AI are being utilized to assist medical
practitioners in clinical settings and ongoing research (Table I). Currently, clinical decision
support and image analysis are the most commonly encountered
applications of AI in medical contexts (3). Treatment, medication and other patient
requirements are all addressed through clinical decision support
systems, which provide clinicians with fast access to up-to-date
information and research that is relevant to the patient's
situation (3,16).
 | Table IApplications of artificial
intelligence that have the greatest potential in the healthcare
industry. |
Table I
Applications of artificial
intelligence that have the greatest potential in the healthcare
industry.
| Application | Description | AI techniques
used | Benefits |
|---|
| Medical imaging and
diagnostics | AI algorithms can
analyze medical images to detect diseases (e.g., cancer,
fractures) | DL (CNNs) and
computer vision | Improved accuracy and
faster diagnosis |
| Drug discovery and
development | Accelerates
identification of potential drug candidates and purposing existing
drugs | ML and predictive
analytics | Reduced time and cost
in drug development |
| Personalized
medicine | Tailoring treatment
plans based on individual genetics and health data | DM, genomic analysis
and ML | More effective
treatments and better outcomes |
| Predictive
analytics | Predicts patient
outcomes and disease risks based on data patterns | ML and statistical
modeling | Proactive care and
risk reduction |
| Patient monitoring
and care | Real-time monitoring
of patient vital signs with alert systems | IoT devices and ML
algorithms | Early issue detection
and improved safety |
| Robotic surgery | AI-assisted robots
enhance precision in surgical procedures | Robotics, computer
vision and ML | Minimally invasive
surgery and better outcomes |
| Disease outbreak
prediction | Uses data analysis to
predict and track disease outbreaks | Big data analytics
and epidemiological modeling | Early intervention
and public health planning |
| EHR management | Organizes and
analyzes EHR data for clinical insights | NLP, DM | Improved data
accessibility and decision-making |
| Telemedicine and
remote care | Delivers medical care
remotely via AI platforms | Video Analytics, ML
and NLP | Increased access and
patient convenience |
| Clinical decision
support | Aids clinicians with
evidence- based recommendations | Expert systems, ML
and NLP | Improved patient
outcomes and care quality |
| Health chatbots | Offers patients
information and symptom checking | NLP, ML and
conversational AI | 24/7 engagement and
reduced healthcare workload |
AI opens up an array of possibilities for the
development of intelligent medical products, innovative services
and new business models. There are numerous different types of AI
technologies in medicine, spanning from virtual to physical. The
ability of AI technologies to identify complex patterns and hidden
structures has allowed image-based detection and diagnostic systems
in healthcare to perform similarly or at times even better than a
clinician in certain instances, according to recent research
(17). Furthermore, clinical
decision-support systems that are powered by AI have the potential
to minimize human diagnostic errors, enhance decision-making
support, increase reproducibility and assist physicians in making
better use of data and documentation (18).
In medical imaging, for instance, AI technologies
are being used to detect abnormalities that may otherwise be
overlooked by a human radiologist in CT scans, X-rays, MRIs and
other imaging systems (19).
Several studies have already shown that AI can diagnose diseases as
well as or better than humans.
Recent advances in AI have shown significant promise
in medical diagnosis, particularly in the early detection of
diseases. In a study conducted by Esteva et al (20) a DL-algorithm was developed and
trained to identify skin cancer using images of skin lesions. The
model achieved an accuracy comparable to that of certified
dermatologists, with the ability to distinguish between malignant
and benign skin lesions (20).
Another study by Abràmoff et al (21) conducted a pivotal study to evaluate
the effectiveness of an autonomous AI system in detecting diabetic
retinopathy (DR) from retinal images. DR is a leading cause of
vision loss in adults, and early detection is crucial for
preventing progression. Traditional screening methods require
specialized ophthalmologists, which can be limited in
accessibility, especially in primary care settings (21). In another study they created an AI
model that achieved a sensitivity of over 90%, indicating a high
true positive rate in detecting early DR. Specificity was also
high, reducing the number of false positives and unnecessary
referrals. Their AI model demonstrated high sensitivity and
specificity, outperforming traditional diagnostic methods (21).
AI has exceeded radiologists in detecting tumors and
has aided researchers in building cohorts for clinical studies
(22). For instance, in a study
conducted by Akselrod-Ballin et al (23), a breast cancer prediction algorithm
trained on 38,444 mammography images from 9,611 women and
integrated with related health data, was able to predict biopsy
malignancy with an accuracy comparable to expert radiologists. This
algorithm could distinguish between benign and malignant screening
findings and had the potential to significantly reduce the number
of missed breast cancer diagnose. Radiologists, oncologists and
pathologists are poised to benefit from this synergy of AI, ML and
DL, which has been trained on a dataset of integrated imaging and
matched clinical records. It will assist them in improving
diagnoses and could help in the early detection of diseases when
intervention and treatment are most effective.
To investigate whether AI can reduce interval cancer
in mammography screening, Lång et al (24) conducted a significant study on the
use of artificial intelligence (AI) in mammography, which was
published in The Lancet Digital Health in 2020 and further
discussed in The Lancet Oncology in 2021. Their research focused on
evaluating the effectiveness of AI in breast cancer screening
programs by performing a study to analyze initial screening
mammograms of 429 sequential cases of women diagnosed with interval
cancer with a deep learning-based AI system. They found that the AI
system was able to spot 19% of interval cancers at the preceding
mammograms that showed negligible signs of malignancy. Of note,
these malignancies were accurately located and ranked as ‘high
risk’ by AI, thus avoiding additional screening.
Chaurasia et al (25) presented a breast cancer detection
system based on three data mining techniques (RepTree, RBF Network
and Simple Logistic). These algorithms were used to forecast the
survival rate of breast cancer data collection. The three
categorization methods were evaluated in order to determine which
was the most accurate in predicting the cancer survival rate in
another patient group.
Litjens et al (26) investigated the ability of DL to
enhance histopathologic slide analysis objectivity. To evaluate the
effectiveness of deep neural networks (DLN) in accurately detecting
prostate cancer from digitized H&E-stained histopathology
slides. Using DLN, the authors digitized histopathology in prostate
cancer detection in biopsy specimens with good accuracy.
Weng et al (27) developed a prediction method for
cardiovascular disease (CVD) utilizing ML on data collected from
>350,000 individuals exhibiting symptoms of CVD and the dataset
of 5,209 patients with CVD from the Framingham research, in which
the Framingham risk score was experimentally tested and compared.
They suggested a system that can predict the CVD risk with
outstanding accuracy. The implementation of ML techniques has been
shown to yield notable enhancements in the precision of CVD risk
assessment. This results in a greater number of patients being
identified as potential candidates for preventive treatment, while
concurrently reducing the incidence of unnecessary treatment.
In the field of digital pathology, with integration
of digital slides into the pathology workflow, advanced algorithms
and computer-aided diagnostic techniques extend the frontiers of
the pathologist's view beyond a microscopic slide and enable true
utilization and integration of knowledge beyond human limits and
boundaries. AI has already enabled pathologists to identify unique
imaging markers associated with disease processes with the goal of
improving early detection, determining prognosis and selecting
treatments most likely to be effective. This allows pathologists to
serve more patients while maintaining diagnostic and prognostic
accuracy. Automated image analysis tools offer a higher level of
precision and reliability in quantification compared to traditional
light microscopy techniques. For instance, the utilization of
computer-aided diagnosis is prevalent in the evaluation of estrogen
and progesterone receptor and HER2/neu in breast cancer, Ki67
assessment in carcinoid tumors and various other clinical and
research stains (28).
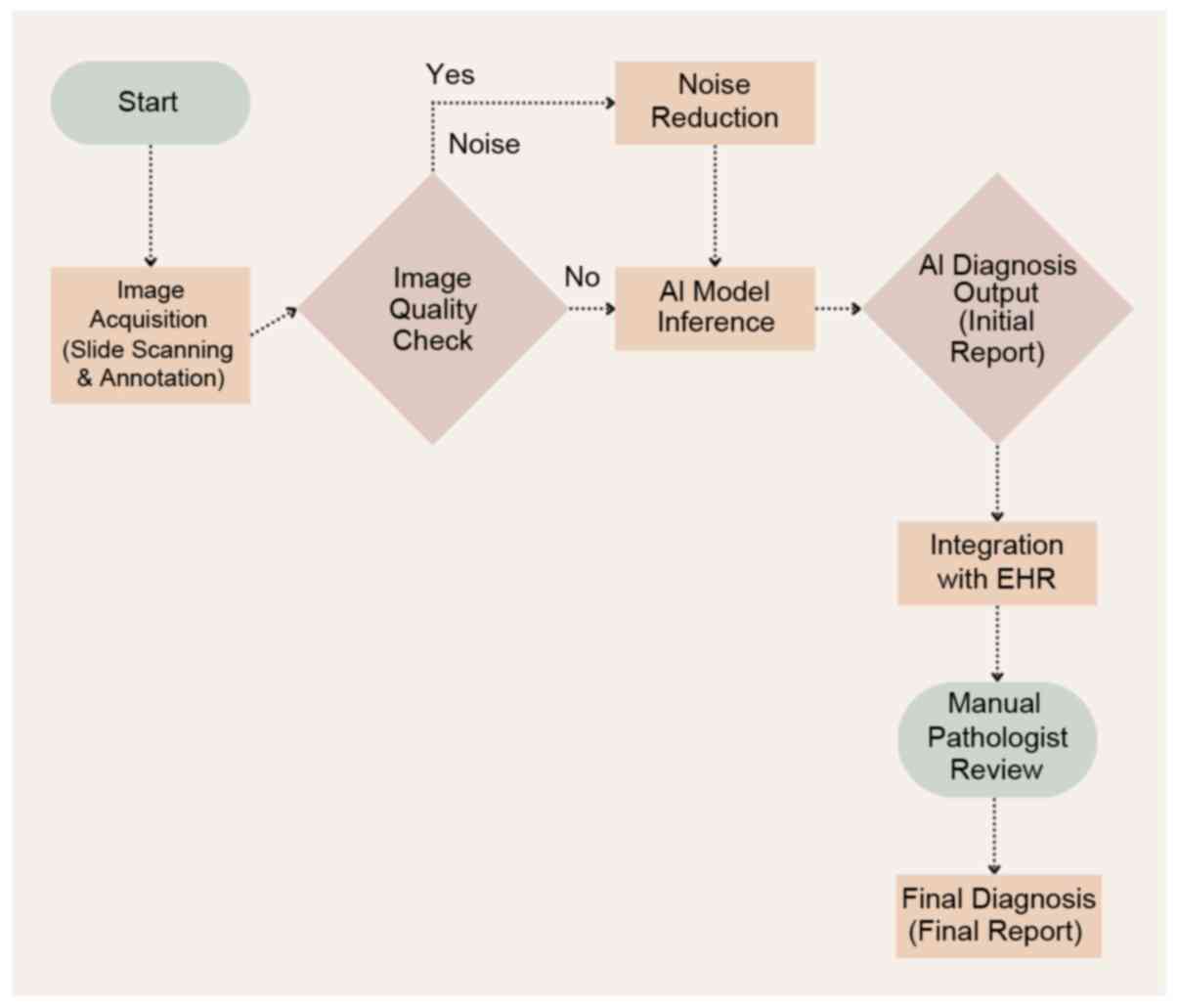
For digital slide analysis, Senaras et al
(29) presented a new DL
architecture, named DeepFocus™, which allows the automated
detection of unclear areas in digital slides for rapid re-scan in
order to enhance image quality for pathologists and image analysis
algorithms. Janowczyk et al (30) introduced an open-source program
called HistoQC to evaluate color histograms, brightness and
contrast of each slide and to detect cohort-level outliers. These
techniques have an important role in the quality control of
whole-slide scans to standardize the quality of images in
computational pathology (Fig.
2).
Niazi et al (31) employed DL techniques to detect tumor
regions in pancreatic neuroendocrine tumors. Their methodology
utilized transfer learning, a technique in which the
characteristics of a pre-existing DL-algorithm that has been
trained on a different classification task are adjusted and
retrained to classify regions of tumors and stroma. Tumor cells
exhibiting both Ki67 positivity and negativity were employed. Using
AI, pathologists can now be relieved from the heavy manual
annotations for each slide scan thanks to improvements in various
smart image-recognition algorithms. Campanella et al used ML
methods based on CNN and recurrent neural networks to evaluate
programmed cell death ligand-1 expression in immunohistochemistry
slides of late-stage non-small cell lung cancer specimens from
needle biopsies (32).
There are large volume of study and review on AI in
healthcare highlighted the dominance of imaging-based specialties
such as radiology, gastroenterology, and ophthalmology in AI
research. A substantial portion of studies use deep learning (DL),
with 75.2% of them focusing on image data. Large Language Models
(LLMs) are gaining traction, particularly in general healthcare and
surgery, suggesting a shift toward their broader application. The
review suggests that future developments may involve multimodal
models, enhancing both clinical and administrative aspects of
healthcare through AI advancements. The above-mentioned studies are
summarized in (Table II).
 | Table IISummary of studies on AI applications
in healthcare. |
Table II
Summary of studies on AI applications
in healthcare.
| Author(s), year | Title of study | Findings | (Refs.) |
|---|
| Esteva et al,
2017 | Dermatologist-level
classification of skin cancer with deep neural networks | Developed a deep
learning algorithm that identifies skin cancer from images of skin
lesions with accuracy comparable to certified dermatologists,
effectively distinguishing between malignant and benign
lesions. | (20) |
| Abràmoff et
al, 2018 | Pivotal trial of an
autonomous AI-based diagnostic system for detection of diabetic
retinopathy in primary care | Evaluated an
autonomous AI system for detecting diabetic retinopathy from
retinal images. The AI model achieved >90% sensitivity and high
specificity, outperforming traditional diagnostic methods and
reducing false positives and unnecessary referrals. | (21) |
| Akselrod- Ballin
et al, 2019 | Predicting breast
cancer by applying deep learning to linked health records and
mammograms | Created a breast
cancer prediction algorithm trained on 38,444 mammography images
and integrated health data from 9,611 women. The algorithm
predicted biopsy malignancy with accuracy comparable to expert
radiologists, potentially reducing missed breast cancer
diagnoses. | (23) |
| Lång et al,
2020 | Can artificial
intelligence reduce the interval cancer rate in mammography
screening? | Analyzed initial
screening mammograms of 429 women diagnosed with interval cancer
using an AI system. Found that AI could detect 19% of interval
cancers in prior mammograms, accurately locating and ranking them
as ‘high risk’, which could reduce missed diagnoses in screening
programs. | (24) |
| Chaurasia et
al, 2018 | Data mining technique
approach to predict breast cancer using machine learning | Presented a breast
cancer detection system using three data mining techniques
(RepTree, RBF Network and Simple Logistic) to forecast survival
rates. Evaluated these methods to determine the most accurate in
predicting cancer survival rates in different patient groups. | (25) |
| Litjens et al,
2016 | Deep learning as a
tool for increased accuracy and efficiency of histopathological
diagnosis | Investigated the use
of deep learning to enhance objectivity in histopathological slide
analysis. Using deep neural networks, they achieved good accuracy
in detecting prostate cancer from digitized H&E-stained
histopathology slides, improving diagnostic precision. | (26) |
| Weng et al,
2017 | Can
machine-learning improve cardiovascular risk prediction using
routine clinical data? | Developed a machine
learning-based method for cardiovascular disease risk prediction
using data from >350,000 individuals. Their system showed
outstanding accuracy compared to traditional methods, identifying
more candidates for preventive treatment while reducing unnecessary
interventions. | (27) |
| Senaras et
al, 2018 | DeepFocus:
Detection of out-of-focus regions in whole slide digital images
using deep learning | Introduced
DeepFocus™, a deep learning architecture for automated detection of
unclear areas in digital slides. This allows rapid re-scanning to
enhance image quality for pathologists and image analysis
algorithms, improving the overall efficiency of digital pathology
workflows. | (29) |
| Janowczyk et
al, 2019 | HistoQC: An
open-source quality control tool for digital pathology slides | Developed HistoQC,
an open-source program that evaluates color histograms, brightness
and contrast of each slide to detect cohort-level outliers. This
tool plays a crucial role in the quality control of whole- slide
scans, standardizing image quality in computational pathology. | (30) |
| Niazi et al,
2019 | Leveraging transfer
learning in deep neural networks for tumor classification using
non-small cell lung cancer | Employed deep
learning techniques with transfer learning to detect tumor regions
in pancreatic neuroendocrine tumors. Adjusted a pre-existing deep
learning algorithm to classify regions of tumors and stroma, using
tumor cells exhibiting both Ki67 positivity and negativity,
enhancing diagnostic accuracy. | (31) |
| Campanella et
al, 2019 | Clinical-grade
computational pathology using weakly supervised deep learning on
whole slide images | Used machine
learning methods based on convolutional neural networks and
recurrent neural networks to evaluate PD-L1 expression in
immunohistochemistry slides of late-stage non-small cell lung
cancer specimens from needle biopsies, reducing manual annotation
workload. | (32) |
4. Challenges and opportunities of using AI
for improving healthcare
Although the advantages of implementing AI in the
healthcare industry are evident, there are noteworthy obstacles
that require resolution. The following challenges are deemed to be
of utmost significance: The ethical implications associated with
the integration of AI technology, such as potential breaches of
data privacy and confidentiality, informed consent and patient
autonomy, must be addressed. In the realm of PM, AI, ML and BD
analysis, establishing robust data protection regulations to
effectively safeguard individual confidentiality, particularly for
those receiving medical treatment, is crucial. Furthermore, the
accurate analysis by AI algorithms heavily depends on the
availability of large amounts of high-quality data. Healthcare data
are often present in a fragmented manner, lacking interoperability
and consistency, which leads to potential issues of completeness
and accuracy. Ensuring the quality, accessibility and
standardization of data poses significant obstacles.
The implementation of AI in healthcare
decision-making processes raises a range of ethical questions. A
conscientious examination of the transparency and accountability of
AI algorithms, potential biases inherent in data and algorithms and
the attribution of liability for AI-generated decisions is
imperative. The dynamic nature of regulatory frameworks and
guidelines aims to tackle these challenges. Furthermore, the
process of integrating AI into pre-existing healthcare systems and
workflows can be challenging. The successful implementation of AI
technologies requires overcoming obstacles such as ensuring smooth
integration and compatibility with legacy systems. Additional
significant challenges to predict include healthcare system
regulations that may limit the full potential of AI technology, as
well as understanding the best practices for applying knowledge
gained from AI in an ethical and optimal manner.
From a clinical perspective, a considerable issue
for healthcare providers will be that they are no longer the sole
authorities in medical treatment delivery. They must also respond
to patients who, in certain cases, may have an understanding of
their medical conditions comparable to that of the experts.
Furthermore, healthcare providers may find themselves required to
consider insights from an AI program that could be more
knowledgeable in certain areas. Nonetheless, in both scenarios, it
is the healthcare providers' responsibility to assess the
information provided and administer the appropriate care, which may
or may not align with the AI technology's recommendations.
5. Conclusion
AI has the potential to enhance healthcare service
delivery in areas such as illness prevention, early diagnosis and
treatment. The provision of health services is already undergoing a
transformation. AI applications may be categorized based on the
specific objectives they serve and the methods they employ to
accomplish these goals. The integration of data from multiple
sources, such as wearable devices, genetic information from genome
sequencing, electronic health records, radiological imaging and
even hospital rooms, has resulted in a surge of valuable data in
healthcare.
For AI to directly impact and improve clinical care
delivery, a corresponding evidence base is required to demonstrate
improved outcomes and the absence of unintended consequences. For
instance, validating the accuracy of AI-enabled imaging
applications against current quality standards for conventional
imaging may serve for clinical use. However, when AI applications
extend to prediction, diagnosis and treatment, the evidence
threshold should increase significantly, so that the wealth of
information provides a fertile ground for AI systems to learn
complex patterns, predict outcomes, and support decision-making
processes that were previously beyond human capability.
Eventually, the integration of AI in healthcare
poses potential benefits and challenges. Successful AI
implementation requires addressing key issues such as data quality
and accessibility, privacy and ethical considerations and seamless
integration. Despite the challenges, the use of AI in healthcare
can offer significant benefits, including improved diagnostic
precision, personalized care, enhanced efficiency and accelerated
medical research. As such, AI has become an invaluable asset in
healthcare transformation and holds promise for improving patient
outcomes. By adeptly navigating the challenges and leveraging the
benefits, healthcare stakeholders can fully harness AI's
capabilities to revolutionize healthcare services. Ethical
considerations and human rights must be at the forefront of AI
health technology design, development and deployment to benefit
public health and medicine.
For AI to effectively integrate into healthcare
systems, it is essential to eliminate existing biases encoded in
the data used to train algorithms. Addressing the digital divide,
or the unequal distribution of access the use of information and
communication technologies is necessary. Global technology
corporations are making substantial investments in data collection,
big data algorithms and AI implementation. When used appropriately,
AI has the potential to empower patients and communities to manage
their healthcare and better understand their evolving needs. Of
note, all of the revolutions seen today in AI are only the
beginning.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
The author confirms sole responsibility for the
following: Study conception and design, data collection and
manuscript preparation. The author has read and approved the final
manuscript. Data authentication is not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The author has no competing interests to
declare.
References
|
1
|
Davenport T and Kalakota R: The potential
for artificial intelligence in healthcare. Future Healthc J.
6:94–98. 2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Muthukrishnan N, Maleki F, Ovens K,
Reinhold C, Forghani B and Forghani R: Brief History of Artificial
Intelligence. Neuroimaging Clin N Am. 30:393–399. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Fogel AL and Kvedar JC: Artificial
intelligence powers digital medicine. NPJ Digit Med.
1(5)2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Yu KH, Beam AL and Kohane IS: Artificial
intelligence in healthcare. Nat Biomed Eng. 2:719–731.
2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Rajpurkar P, Chen E, Banerjee O and Topol
EJ: AI in health and medicine. Nat Med. 28:31–38. 2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Polevikov S: Advancing AI in healthcare: A
comprehensive review of best practices. Clin Chim Acta.
548(117519)2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Jiang F, Jiang Y, Zhi H, Dong Y, Li H, Ma
S and Wang Y, Dong Q, Shen H and Wang Y: Artificial intelligence in
healthcare: Past, present and future. Stroke Vasc Neurol.
2:230–243. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Goirand M, Austin E and Clay-Williams R:
Implementing ethics in healthcare Ai-based applications: A scoping
review. Sci Eng Ethics. 27(61)2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Conn J: Computing better healthcare.
Modern Healthcare, 2013.
|
|
10
|
Aung YYM, Wong DCS and Ting DSW: The
promise of artificial intelligence: A review of the opportunities
and challenges of artificial intelligence in healthcare. Br Med
Bull. 139:4–15. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Mintz Y and Brodie R: Introduction to
artificial intelligence in medicine. Minim Invasive Ther Allied
Technol. 28:73–81. 2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Alowais SA, Alghamdi SS, Alsuhebany N,
Alqahtani T, Alshaya AI, Almohareb SN, Aldairem A, Alrashed M, Bin
Saleh K, Badreldin HA, et al: Revolutionizing healthcare: The role
of artificial intelligence in clinical practice. BMC Med Educ.
23(689)2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Patel D and Kore SA: Artificial
intelligence: future impacts, challenges and recommendations on
healthcare services. Int J Community Med Public Health.
7:1596–1598. 2020.
|
|
14
|
Triantafillou G and Minas MY: Future of
the Artificial Intelligence in Daily Health Applications. The
European Journal of Social & Behavioural Sciences 29, 2020.
|
|
15
|
Mondal B: Artificial Intelligence: State
of the Art. In: Recent Trends and Advances in Artificial
Intelligence and Internet of Things. Intelligent Systems Reference
Library. Balas V, Kumar R and Srivastava R (eds). Vol 172.
Springer, Cham, 2020.
|
|
16
|
Mintz Y and Brodie R: Introduction to
artificial intelligence in medicine. Minim Invasive Ther Allied
Technol. 28:73–81. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Giger ML: Machine Learning in Medical
Imaging. J Am Coll Radiol. 15 (3 Pt B):512–520. 2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Choi KS: Integrating artificial
intelligence into healthcare research. Hu Li Za Zhi. 67:12–18.
2020.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
19
|
Torkamani A, Andersen KG, Steinhubl SR and
Topol EJ: High-Definition Medicine. Cell. 170:828–843.
2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Esteva A, Robicquet A, Ramsundar B,
Kuleshov V, DePristo M, Chou K, Cui C, Corrado G, Thrun S and Dean
J: A guide to deep learning in healthcare. Nat Med. 25:24–29.
2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Abràmoff MD, Lavin PT, Birch M, Shah N and
Folk JC: Pivotal trial of an autonomous AI-based diagnostic system
for detection of diabetic retinopathy in primary care offices. NPJ
Digit Med. 1(39)2018.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Ranjbari D and Abbasgholizadeh Rahimi S:
Implications of conscious AI in primary healthcare. Fam Med
Community Health. 12 (Suppl 1). (e002625)2024.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Akselrod-Ballin A, Chorev M, Shoshan Y,
Spiro A, Hazan A, Melamed R, Barkan E, Herzel E, Naor S, Karavani
E, et al: Predicting breast cancer by applying deep learning to
linked health records and mammograms. Radiology. 292:331–342.
2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Lång K, Josefsson V, Larsson AM, Larsson
S, Högberg C, Sartor H, Hofvind S, Andersson I and Rosso A:
Artificial intelligence-supported screen reading versus standard
double reading in the Mammography Screening with Artificial
Intelligence trial (MASAI): A clinical safety analysis of a
randomised, controlled, non-inferiority, single-blinded, screening
accuracy study. Lancet Oncol. 24:936–944. 2023.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Chaurasia V, Pal S and Tiwari BB:
Prediction of benign and malignant breast cancer using data mining
techniques. J Algorithm Comput Technol. 12:2018.
|
|
26
|
Litjens G, Sánchez CI, Timofeeva N,
Hermsen M, Nagtegaal I, Kovacs I, Hulsbergen-van de Kaa C, Bult P,
van Ginneken B and van der Laak J: Deep learning as a tool for
increased accuracy and efficiency of histopathological diagnosis.
Sci Rep. 6(26286)2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Weng SF, Reps J, Kai J, Garibaldi JM and
Qureshi N: Can Machine-learning improve cardiovascular risk
prediction using routine clinical data? PLoS One.
12(e0174944)2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Veta M, van Diest PJ, Kornegoor R, Huisman
A, Viergever MA and Pluim JP: Automatic Nuclei Segmentation in
H&E Stained Breast Cancer Histopathology Images. PLoS One.
8(e70221)2013.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Senaras C, Niazi MKK, Lozanski G and
Gurcan MN: DeepFocus: Detection of out-of-focus regions in whole
slide digital images using deep learning. PLoS One.
13(e0205387)2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Janowczyk A, Zuo R, Gilmore H, Feldman M
and Madabhushi A: HistoQC: An open-source quality control tool for
digital pathology slides. JCO Clin Cancer Inform. 3:1–7.
2019.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Niazi MKK, Tavolara TE, Arole V, Hartman
DJ, Pantanowitz L and Gurcan MN: Identifying tumor in pancreatic
neuroendocrine neoplasms from Ki67 images using transfer learning.
PLoS One. 13(e0195621)2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Campanella G, Hanna MG, Geneslaw L,
Miraflor A, Werneck Krauss Silva V, Busam KJ, Brogi E, Reuter VE,
Klimstra DS and Fuchs TJ: Clinical-grade computational pathology
using weakly supervised deep learning on whole slide images. Nat
Med. 25:1301–1309. 2019.PubMed/NCBI View Article : Google Scholar
|