Introduction
The coronavirus disease 2019 (COVID-19) pandemic has
significantly affected global health, with varying impacts on
different population groups (1-4).
Pregnant women have been identified as a particularly vulnerable
subgroup due to physiological changes in the immune and
cardiovascular systems, which may influence their response to
severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2)
infection (5). Recent research has
highlighted that not only are pregnant women at a higher risk for
severe outcomes during the acute phase of COVID-19, but they may
also experience lingering post-acute sequelae of SARS-CoV-2
infection, known as Long COVID-19 syndrome (6,7). This
condition, characterized by a range of symptoms persisting beyond
four weeks post-infection (8), has
raised concerns about its impact on maternal health and pregnancy
outcomes.
Long COVID-19 syndrome, also referred to as
post-acute sequelae of COVID-19 (PASC), includes a variety of
symptoms such as fatigue, cognitive dysfunction, respiratory issues
and psychological disturbances (9-12).
The prevalence of these symptoms and their intensity appear to vary
among pregnant women depending on factors such as the severity of
the initial infection, pre-existing health conditions and
sociodemographic characteristics (13-15).
Studies have reported that pregnant women often experience distinct
post-infection symptoms, including dyspnea, fatigue and mood
disturbances, which can complicate pregnancy (7,13).
The potential impact of Long COVID-19 on maternal
and fetal health is a growing area of research. Early findings
indicate that pregnant women with severe COVID-19 are more likely
to develop long-term respiratory and neurological symptoms, which
could interfere with their ability to perform daily activities and
care for their newborns (16).
Additionally, the presence of these prolonged symptoms may increase
the risk of adverse pregnancy outcomes, such as preterm birth, low
birth weight and increased need for intensive care for both the
mother and the infant (7,17).
The aim of the present systematic review is to
comprehensively evaluate the prevalence, risk factors and clinical
outcomes of Long COVID-19 syndrome in pregnant women. By
synthesizing findings from multiple studies, the review aims to
provide a clearer understanding of the burden and nature of Long
COVID-19 in this unique population. The results will inform
healthcare providers and policymakers, facilitating the development
of targeted interventions and strategies to support maternal health
during and after the pandemic.
Materials and methods
The present systematic review was conducted
following the Preferred Reporting Items for Systematic Reviews and
Meta-Analyses (PRISMA) guidelines (18) to evaluate the prevalence, risk
factors and clinical outcomes of Long-COVID-19 in pregnant women.
Studies were included if they reported original data on
post-COVID-19 symptoms and outcomes specifically in the context of
pregnancy. The review included studies utilizing prospective,
retrospective, pilot, longitudinal and cross-sectional designs to
ensure comprehensive coverage of the topic. In addition, the
present systematic review has been registered in the International
Register of Systematic Review Protocols (PROSPERO) under accession
number CRD42024600019 (https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=600019).
Inclusion and exclusion criteria
Studies were included if they met the following
criteria: i) reported on pregnant women diagnosed with COVID-19
during pregnancy, ii) provided information on Long COVID-19 or
PASC, iii) included a minimum follow-up duration of at least four
weeks post-acute infection, and iv) were peer-reviewed articles
published in English. Exclusion criteria included review articles,
case reports, or studies not focused on Long COVID-19 outcomes.
Studies with insufficient data on clinical outcomes or missing
critical methodological details were also excluded.
Search strategy
A systematic search was conducted in the PubMed,
Scopus and Google Scholar databases, covering literature published
between January 2020 and October 2024. Search terms included
combinations of ‘COVID-19’, ‘pregnancy’, ‘Long COVID’, ‘post-acute
sequelae’, ‘PASC’, ‘pregnant’, ‘SARS-CoV-2’ and ‘maternal
outcomes’.
PRISMA process
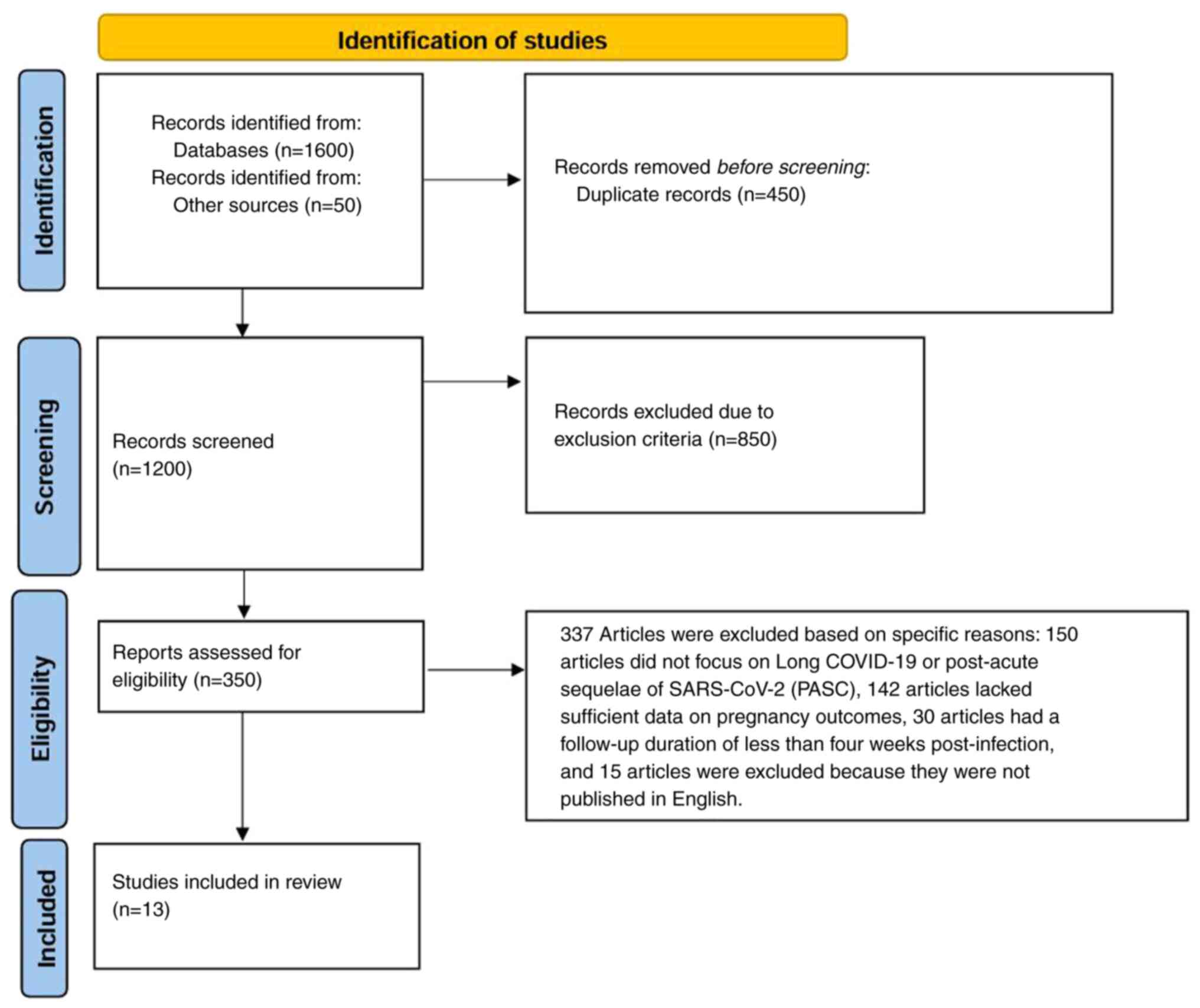
The PRISMA process is illustrated in Fig. 1. Identification: A total of 1,600
records were identified through systematic searches in PubMed
(https://pubmed.ncbi.nlm.nih.gov/),
Scopus (https://www.scopus.com/home.uri) and Google Scholar
(https://scholar.google.com/). An
additional 50 records were identified from reference lists of
relevant articles and other databases, resulting in a total of
1,650 records for initial consideration.
Screening: After removing 450 duplicate records,
1,200 unique records were screened based on their titles and
abstracts. During this screening phase, 850 records were excluded
for not meeting the inclusion criteria. The excluded records
comprised review articles, case reports and studies that did not
focus on pregnancy or Long COVID-19.
Eligibility: The eligibility assessment included a
review of 350 full-text articles. Out of these, 337 articles were
excluded based on specific reasons: 150 articles did not focus on
Long COVID-19 or PASC, 142 articles lacked sufficient data on
pregnancy outcomes, 30 articles had a follow-up duration of <4
weeks post-infection, and 15 articles were excluded because they
were not published in English.
Included studies: A total of 13 studies were deemed
suitable for narrative synthesis due to the heterogeneity in study
designs and outcome measures. These studies provided the most
comprehensive data on Long COVID-19 in pregnant and postpartum
women, which was crucial for synthesizing meaningful
conclusions.
Data extraction and synthesis
Data from each study was extracted independently by
two reviewers using a standardized data extraction form. Key
variables included study design, sample size, population
characteristics, outcome measures and results related to Long
COVID-19 symptoms and associated risk factors. Disagreements were
resolved through discussion or consultation with a third
reviewer.
The extracted information included: i) author, year
and type of study; ii) population characteristics (for example,
number of participants, demographics and inclusion criteria); iii)
measurements (for example, diagnostic tools and questionnaires used
to assess post-COVID-19 symptoms); and iv) key findings (for
example, prevalence of specific symptoms and identified risk
factors).
Quality assessment
The quality of included studies was assessed
independently by two reviewers using validated tools. Cohort and
case-control studies were evaluated using the Newcastle-Ottawa
Scale (19), which assesses
selection, comparability and outcome domains. Each study was
assigned a score, and the quality was categorized as high (7-9
stars), moderate (4-6 stars), or low (<4 stars).
Data analysis
Due to the heterogeneity of study designs and
reported outcomes, a narrative synthesis was used to describe key
findings across studies. Where applicable, the prevalence of Long
COVID symptoms was summarized, and risk factors were identified.
Meta-analyses were not conducted due to significant variability in
symptom assessment tools and follow-up durations across
studies.
The present systematic review synthesizes evidence
on the impact of Long COVID in pregnant women, highlighting
prevalent symptoms, risk factors and the need for targeted
management strategies.
Results
Study characteristics
The systematic review included 13 studies (6,7,13-15,17,20-26),
encompassing a total of 13,729 participants. Studies varied in
design, with most employing prospective or cross-sectional
approaches. The sample sizes ranged from 33 to 5,397 participants,
and studies were conducted across diverse geographical regions,
including the United States, Brazil, China, Turkey, Ecuador and
Russia. Study populations included pregnant women at various
gestational stages and postpartum women. The characteristics of the
included studies and the quality assessment are summarized in
Table I.
 | Table ICharacteristics of the included
studies. |
Table I
Characteristics of the included
studies.
| First author/s,
year | Type of study | Population | Measurements | Key findings | Quality
assessment | (Refs.) |
|---|
| Backes et al,
2024 | Pilot study | 773 women enrolled in
CRONOS registry: 110 completed follow-ups | Web-based
questionnaire for follow-up data on Long-COVID-19 symptoms,
including fatigue, and quality of life (EuroQoL EQ-5D-5L) | 63.6% reported
Long-COVID-19 symptoms, 55% experienced fatigue more than one-year
post-infection, 76% rated their quality of life as ‘good’ or ‘very
good’ | Moderate quality
(NOS: 5/9 stars, based on low response rate and potential reporting
bias) | (7) |
| Bruno et al,
2024 | Retrospective cohort
study | 5397 pregnant women
and 83,915 non-pregnant women with lab-confirmed SARS-CoV-2
infection | Electronic Health
Records (EHR) data from 19 U.S. health systems; computable Long
COVID-19 phenotype; adjusted hazard ratios using IPTW | SARS-CoV-2 infection
acquired during pregnancy associated with lower Long COVID-19 risk
(aHR 0.85, 95% CI 0.80-0.91); increased risk of thromboembolism,
abdominal pain, and abnormal heartbeat; decreased risk for
cognitive problems, malaise, and fatigue. | High quality (NOS:
9/9 stars; Validated comput able phenotype, large sample size,
adjustment for confounders using IPTW) | (20) |
| Ghizzoni et
al, 2024 | Retrospective cohort
study | 880 pregnant women
(385 COVID-19 positive, 495 COVID-19 negative) admitted to the
maternity ward of a tertiary care hospital in Brazil | Clinical
characteristics and obstetric outcomes collected through hospital
charts; persistent symptoms evaluated through follow-up calls at 3
and 6 months | COVID-19 positive
pregnant women had higher risk of adverse outcomes (preterm birth,
ICU admission, mechanical ventilation, maternal and neonatal
death); 30% had persistent symptoms for 6+ months (fatigue,
myalgia, olfactory disorders). | High quality (NOS:
8/9; The scoring considers strong representativeness and reliable
follow-up, with a minor deduction due to potential biases) | (17) |
| Gu et al,
2023 | Retrospective cohort
study | 155 pregnant women
with prior COVID-19 infection and 76 COVID-19 negative controls,
Affiliated Maternity and Child Health Care Hospital of Nantong
University, China | Liver function tests
(ALT, AST, ALP, GGT) assessed via routine biochemical tests;
abnormal liver function defined based on hospital standards | 40.6% of COVID-19
positive patients had elevated liver enzymes; gestational age and
BMI were independent risk factors for liver injury. Liver function
normalized within 4-26 days. | High quality (NOS:
7/9 stars; The scoring reflects a well-conducted study with
limitations in follow-up and adjustment for confounders.) | (21) |
| Muñoz-Chápuli
Gutiérrez et al, 2024 | Prospective
observational cohort study | 409 pregnant women
with confirmed COVID-19 infection during pregnancy or at
delivery | Systematic clinical
surveys via telephone using the Delphi consensus; long-term
follow-up over a median of 100 weeks | 34.2% had at least
one post-COVID-19 symptom after 3 months; neurological (60%) and
cutaneous (55%) symptoms were most common; risk factors include
multiparity, non-vaccination, and severe acute infection. | High quality (NOS:
7/9 stars based on selection bias and follow-up limitations) | (15) |
| Kandemir et
al, 2024 | Cross-sectional,
retrospective cohort study | 99 COVID-19
positive pregnant women and 99 COVID-19 negative controls, Akdeniz
University, Turkey | Clinical surveys
via telephone interviews; acute and long-term symptoms recorded
systematically | 74.7% of COVID-19
positive women had long COVID-19 symptoms, primarily fatigue
(54.5%), myalgia/arthralgia (49.5%), and anosmia/ageusia (31.3%).
Severe acute disease increased the likelihood of long COVID-19 (aOR
= 13.3). | High quality (NOS:
7/9 stars based on follow-up bias, lack of control for
confounders) | (22) |
| Oliveira et
al, 2022 | Longitudinal
comparative cohort study | 588 pregnant women
(259 COVID-19 symptomatic, 131 COVID-19 positive serology, 198
COVID-19 negative serology) | Custom-built
fatigue questionnaires at multiple timepoints (6 weeks, 3 months, 6
months post-infection/delivery) | Higher fatigue
prevalence in symptomatic women (G1) compared with G2 and G3 at all
timepoints; increased risk with severe acute disease (HR =
2.43). | High quality (NOS:
7/9 stars based on follow-up loss and lack of confounder
adjustment) | (13) |
| Metz et al,
2024 | Multicenter
prospective cohort study | 1,502 pregnant
individuals enrolled across multiple U.S. centers | NIH
RECOVER-Pregnancy Cohort criteria; symptoms evaluated 6+ months
post-infection using standardized questionnaires | 9.3% had long
COVID-19 at a median of 10.3 months post-infection; key risk
factors included obesity (aOR 1.65), depression/anxiety (aOR 2.64),
economic hardship (aOR 1.57), and severe acute infection requiring
oxygen (aOR 1.86). | High quality (NOS:
8/9 stars, with minor bias due to enrollment timing and potential
loss to follow-up) | (14) |
| Vásconez-González
et al, 2023 | Cross-sectional
study | 457 women (16
pregnant, 441 non-pregnant) in Ecuador | Online
self-reported survey with 37 items covering demographics, lifestyle
habits, and long COVID-19 symptoms | 54.1% of
respondents had long COVID-19symptoms; common symptoms in pregnant
women included fatigue (10.6%), hair loss (9.7%), and difficulty
concentrating (6.2%). No statistically significant differences
between pregnant and non-pregnant women. | Moderate quality
(NOS: 4/9 stars; limitations include self-reporting bias, low
representation of pregnant women, and limited confounder
adjustment) | (23) |
| Vetrugno et
al, 2023 | Prospective
observational study | 33 unvaccinated
pregnant women with COVID-19 at any gestational age admitted to
University Hospital of Udine, Italy | SF-36 and IES-R to
evaluate health-related quality of life (HRQoL) and PTSD at 1-year
follow-up | 30% tested positive
for PTSD; physical impairment reported in HRQoL scores. Lower
scores in bodily pain and physical function. Previous cardiac,
pulmonary, or kidney disease significantly worsened HRQoL. | High quality (NOS:
7/9 stars; limitations include small sample size and self-report
bias) | (24) |
| Belokrinitskaya
et al, 2023 | Cross-sectional
observational study | 111 pregnant women
and 181 non-pregnant women with PCR-confirmed SARS-CoV-2
infection | Symptom assessment
using a 10-point questionnaire; comparison of Long COVID-19
symptoms between groups | 93.7% of pregnant
and 97.2% of non-pregnant women had Long COVID-19. Pregnant women
reported higher dyspnea rates (37.8% vs 26.5%, OR=1.69) and lower
rates of hair loss (46.8% vs. 60.8%) and headache (30.6% vs.
43.1%). | High quality (NOS:
7/9 stars; limitations include self-reporting bias and potential
selection bias due to lack of diverse population) | (25) |
| Malgina et
al, 2023 | Prospective
observational cohort study | 200 pregnant women
with mild and moderate COVID-19 (I: n=22, II: n=76, III: n=102) and
99 non-COVID-19 controls | Symptom assessment
using a 40-item questionnaire and Hamilton Depression Scale | 93.0% of pregnant
women in the study group had Long COVID-19 vs. 38.4% in the control
group; significant symptoms: cognitive impairment, distortion of
smell/taste, dry mouth, fatigue, and psychological disorders. | High quality (NOS:
7/9 stars; limitations include single-center design and potential
selection bias) | (6) |
| Yao et al,
2024 | Retrospective
cohort | 623 pregnant women:
209 acute COVID-19, 72 long-term COVID-19, 342 non-COVID-19 | Epidemiological and
clinical characteristics, maternal and fetal complications, blood
coagulation indicators | Long-term COVID-19
associated with higher rates of gestational hypertension (OR
3.344), gestational diabetes (OR 2.301), and fetal intrauterine
growth restriction (OR 2.817). No significant differences in
premature rupture of membranes, preterm delivery, neonatal
asphyxia, or NICU transfer. Slightly lower platelet count in
long-term COVID-19 group. | High quality (NOS:
8/9 stars; ethically approved, robust statistical methods) | (26) |
Prevalence of Long COVID-19 in
pregnant women
Across the included studies, the prevalence of Long
COVID-19 in pregnant women varied widely, ranging from 9.3-93%. The
variation in prevalence can be attributed to differences in study
design, follow-up duration and the definition of Long COVID-19.
Studies such as Metz et al (14), a large multicenter cohort study,
reported a lower prevalence of Long COVID-19 at 9.3% when
evaluating symptoms at a median follow-up of 10.3 months. By
contrast, smaller single-center studies, such as Malgina et
al (6), observed a
significantly higher prevalence (93%) in pregnant women compared
with non-COVID-19 controls (38.4%).
Persistent symptoms
The reported symptoms of Long COVID-19 in pregnant
women encompassed a wide spectrum, with fatigue, cognitive
dysfunction, respiratory symptoms and psychological disturbances
being the most reported. Fatigue was the most frequently observed
symptom across studies, with prevalence rates ranging from 54.5%
(22) to 76% (7). Cognitive impairment and memory loss
were prominent in studies such as Malgina et al (6), affecting nearly 50% of the affected
women. Psychological symptoms, including depression and anxiety,
were highlighted by both Vetrugno et al (24) and Muñoz-Chápuli et al
(15), indicating a significant
impact on health-related quality of life (HRQoL).
Some studies also identified unique symptoms or
sequelae associated with Long COVID-19 in pregnancy. Gu et
al (21) found a high incidence
of liver function abnormalities in 40.6% of pregnant women,
suggesting a potential organ-specific impact of COVID-19 during
pregnancy. Vásconez-González et al (23) noted difficulty concentrating and
hair loss as distinctive symptoms among pregnant women, although no
significant difference was observed compared with non-pregnant
controls. These findings underscore the variability and complexity
of Long COVID-19 symptomatology in the maternal population.
Impact of Long COVID-19 on maternal
and perinatal outcomes
The severity of acute COVID-19 symptoms appears to
be a significant predictor of Long COVID-19 development and its
impact on pregnancy outcomes. Bruno et al (20) demonstrated that women who contracted
SARS-CoV-2 during pregnancy had a lower overall risk of Long
COVID-19 (adjusted hazard ratio=0.85), but those who experienced
severe symptoms were more likely to develop thromboembolic events
and abnormal heart rhythms. Similarly, Yao et al (26) reported that pregnant women with
long-term COVID-19 had a significantly higher risk of developing
gestational hypertension [odd ratio (OR)=3.344], gestational
diabetes (OR=2.301) and fetal intrauterine growth restriction
(OR=2.817). No significant differences were observed in the rates
of premature rupture of membranes, preterm delivery, or neonatal
asphyxia between the long-term COVID-19 and non-COVID-19
groups.
Ghizzoni et al (17) similarly reported a higher rate of
adverse pregnancy outcomes, including preterm birth and neonatal
complications, in women with persistent symptoms.
In addition to obstetric outcomes, Long COVID-19
also influenced maternal HRQoL. Vetrugno et al (24) used the SF-36 and IES-R scales to
assess HRQoL and post-traumatic stress disorder (PTSD) symptoms,
revealing that 30% of participants tested positive for PTSD
one-year post-infection. Women with underlying comorbidities such
as cardiac or pulmonary disease had significantly poorer HRQoL
scores, suggesting that pre-existing health conditions may
exacerbate the long-term impact of COVID-19.
Risk factors for long COVID in
pregnancy
Several studies identified risk factors associated
with an increased likelihood of developing Long COVID-19 among
pregnant women. Metz et al (14) highlighted that obesity, pre-existing
mental health conditions, and severe acute infection were
significantly associated with higher odds of Long COVID-19.
Similarly, Muñoz-Chápuli et al (15) identified non-vaccination and
multiparity as key risk factors. Oliveira et al (13) found that women who experienced
severe acute COVID-19 were at a 2.43-fold increased risk of
persistent fatigue compared with those with milder symptoms,
emphasizing the importance of acute symptom management to
potentially mitigate long-term sequelae. Risk factors and outcomes
of Long COVID-19 in pregnant women are illustrated in Fig. 2.
Discussion
The present systematic review highlights the
significant prevalence and variability of Long COVID-19 in pregnant
women, with rates ranging from 9.3-93%. The wide range in
prevalence is due to differences in study designs, definitions and
timing of symptom assessment. Common symptoms included fatigue,
dyspnea, cognitive impairment and psychological issues such as
anxiety and depression, emphasizing the need for mental health
support. The severity of acute COVID-19 was found to be a key
predictor of Long COVID-19, with severe cases linked to prolonged
symptoms such as liver dysfunction and thromboembolic events. The
clinical impact of Long COVID-19 on pregnancy extends beyond
persistent symptoms. It is associated with adverse maternal and
perinatal outcomes, such as preterm birth, low birth weight and an
increased need for neonatal intensive care. The presence of
long-term respiratory and neurological symptoms, such as
thromboembolic events, may complicate daily activities and
postpartum care, further stressing the need for targeted follow-up
and support for pregnant women with Long COVID-19. This highlights
the need for comprehensive care models that integrate physical,
mental and perinatal health (27).
Several studies within the review identified key risk factors for
developing Long COVID-19 in pregnancy, such as severe acute
infection, obesity and non-vaccination. Additionally, pre-existing
mental health conditions were significantly linked to prolonged
psychological symptoms including anxiety and depression. The
identified risk factors for Long COVID-19 in pregnancy (severe
acute infection, obesity, non-vaccination and pre-existing mental
health conditions) are not unique to pregnant women but are also
well-established risk factors for Long COVID in the general
population (28-31).
Identifying key risk factors for Long COVID-19 in pregnancy, such
as severe acute infection, obesity, non-vaccination and
pre-existing mental health conditions, highlights the need for
targeted clinical interventions. Pregnant women with these risk
factors should receive closer monitoring during and after pregnancy
to detect and manage prolonged symptoms early. Emphasizing COVID-19
vaccination is crucial to reducing severe infection and long-term
complications, while addressing obesity through lifestyle
interventions during pregnancy can help lower the risk of Long
COVID-19(32). Additionally, women
with pre-existing mental health conditions require tailored
postpartum mental health support, and understanding these risk
factors enables more efficient resource allocation to prioritize
care for high-risk individuals (33).
The management of pregnant women with Long COVID-19
should largely mirror that of non-pregnant individuals, with a
focus on self-management and medical care. Self-management includes
daily pulse oximetry, optimizing general health through adequate
sleep, nutrition, smoking cessation and reducing alcohol and
caffeine intake. A gradual increase in exercise should be
encouraged, as tolerated, alongside setting realistic goals.
Medical management involves treating symptoms, managing
pre-existing conditions, prescribing antibiotics for secondary
infections, and referring patients to specialists such as mental
health professionals and pulmonary rehabilitation programs. Social
and financial support should also be prioritized (34).
Pregnancy introduces additional complexities to the
management of Long COVID-19. Women with severe symptoms should seek
pre-conception counseling to optimize their health before
pregnancy. The impact of pregnancy on Long COVID-19 remains
uncertain, though symptoms such as fatigue and breathlessness may
worsen, particularly in the third trimester. During pregnancy,
symptom tracking via a diary can help identify new or worsening
symptoms, which should not be automatically attributed to Long
COVID-19 without thorough evaluation. Regular fetal growth
monitoring is recommended for women with severe symptoms. The
approach to labor and delivery should be individualized, especially
for those with significant fatigue or cardiovascular and
respiratory symptoms, reserving caesarean sections for obstetric
indications (35).
The present systematic review is, to the best of our
knowledge, the first to provide insights from Long COVID-19
syndrome in pregnant women. However, the present systematic review
has several limitations that should be considered when interpreting
the findings. First, there was significant heterogeneity in study
designs, sample sizes, follow-up durations and definitions of Long
COVID, which limited the ability to synthesize results
quantitatively and may have contributed to the observed variability
in prevalence estimates. Numerous included studies relied on
self-reported data, which is subject to recall bias and may not
accurately capture the true burden of symptoms, particularly for
psychological and cognitive outcomes. Additionally, the lack of
standardized diagnostic criteria for Long COVID in pregnant
populations further complicates the comparison of results across
studies. Most studies were conducted in single centers or specific
regions, limiting the generalizability of findings to broader, more
diverse populations. Finally, the exclusion of non-English language
studies and potential publication bias may have resulted in the
omission of relevant data, particularly from regions with a high
burden of COVID-19, such as Latin America and Asia, potentially
skewing the overall D of Long COVID's impact on pregnancy.
Future studies should aim to address these
limitations by adopting longitudinal study designs with larger
sample sizes and standardized symptom assessment tools. Research
should also focus on the long-term impact of Long COVID on both
maternal and fetal health, with particular attention to the role of
vaccination in mitigating the severity and duration of symptoms.
Furthermore, exploring geographically diverse populations could
provide a more comprehensive understanding of Long COVID's impact
on global maternal health.
The present systematic review highlights the
significant burden and complexity of Long COVID in pregnant women.
The findings suggest that the prevalence and severity of Long
COVID-19 are influenced by multiple factors, including the severity
of the acute infection, pre-existing conditions and vaccination
status. The wide range in prevalence estimates across studies
reflects the need for standardized definitions and diagnostic
criteria for Long COVID-19 in this population. Pregnant women with
severe or moderate COVID-19 appear to be at the highest risk for
persistent symptoms, which may impact not only maternal health but
also perinatal outcomes such as preterm birth and neonatal
complications. Psychological symptoms, such as anxiety and
depression, were prominent in several studies, emphasizing the
importance of comprehensive post-infection care that includes
mental health support. Despite the valuable insights provided, the
review's findings are limited by the heterogeneity of study designs
and reliance on self-reported data. Future research should focus on
longitudinal studies with larger sample sizes and diverse
populations to provide a clearer understanding of the long-term
impact of COVID-19 during pregnancy and inform evidence-based
guidelines for managing Long COVID in this vulnerable
population.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
AS and VEG conceptualized the study. AS, CT, VEG and
DAS made a substantial contribution to data interpretation and
analysis and wrote and prepared the draft of the manuscript. AS and
VEG analyzed the data and provided critical revisions. All authors
contributed to manuscript revision, read and approved the final
version of the manuscript. Data authentication is not
applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
DAS is the Editor-in-Chief for the journal, but had
no personal involvement in the reviewing process, or any influence
in terms of adjudicating on the final decision, for this article.
The other authors declare that they have no competing
interests.
Use of artificial intelligence tools
During the preparation of this work, artificial
intelligence tools were used to improve the readability and
language of the manuscript, and subsequently, the authors revised
and edited the content produced by the artificial intelligence
tools as necessary, taking full responsibility for the ultimate
content of the present manuscript.
References
|
1
|
Sawicka B, Aslan I, Della Corte V,
Periasamy A, Krishnamurthy SK, Mohammed A, Tolba Said MM, Saravanan
P, Del Gaudio G, Adom D, et al: The coronavirus global pandemic and
its impacts on society. Coronavirus Drug Discov. 1:267–311.
2022.
|
|
2
|
Georgakopoulou VE, Gkoufa A, Makrodimitri
S, Tsakanikas A, Basoulis D, Voutsinas PM, Karamanakos G, Eliadi I,
Samara S, Triantafyllou M, et al: Risk factors for the in-hospital
and 1-year mortality of elderly patients hospitalized due to
COVID-19-related pneumonia. Exp Ther Med. 27(22)2023.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Chowdhury S, Bappy MH, Desai S, Chowdhury
S, Patel V, Chowdhury MS, Fonseca A, Sekzer C, Zahid S, Patousis A,
et al: COVID-19 and pregnancy. Discoveries (Craiova).
10(e147)2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Lempesis IG, Karlafti E, Papalexis P,
Fotakopoulos G, Tarantinos K, Lekakis V, Papadakos SP, Cholongitas
E and Georgakopoulou VE: COVID-19 and liver injury in individuals
with obesity. World J Gastroenterol. 29:908–916. 2023.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Berumen-Lechuga MG, Leaños-Miranda A,
Molina-Pérez CJ, García-Cortes LR and Palomo-Piñón S: Risk Factors
for severe-critical COVID-19 in pregnant women. J Clin Med.
12(5812)2023.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Malgina GB, Dyakova MM, Bychkova SV,
Shikhova EP and Klimova LE: Post-COVID syndrome in pregnant women
with a history of mild and moderate COVID-19. Obstet Gynecol.
87–94. 2023.
|
|
7
|
Backes C, Pecks U, Keil CN, Zöllkau J,
Scholz C, Hütten M, Rüdiger M, Büchel J, Andresen K and Mand N:
Post-COVID in women after SARS-CoV-2 infection during pregnancy-a
pilot study with follow-up data from the COVID-19-related obstetric
and neonatal outcome study (CRONOS). Z Geburtshilfe Neonatol.
228:74–79. 2024.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Nalbandian A, Sehgal K, Gupta A, Madhavan
MV, McGroder C, Stevens JS, Cook JR, Nordvig AS, Shalev D, Sehrawat
TS, et al: Post-acute COVID-19 syndrome. Nat Med. 27:601–615.
2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Georgakopoulou VE, Makrodimitri S, Gkoufa
A, Apostolidi E, Provatas S, Papalexis P, Spandidos DA, Lempesis
IG, Gamaletsou MN and Sipsas NV: Lung function at three months
after hospitalization due to COVID-19 pneumonia: Comparison of
alpha, delta and omicron variant predominance periods. Exp Ther
Med. 27(83)2024.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Efstathiou V, Stefanou MI, Demetriou M,
Siafakas N, Makris M, Tsivgoulis G, Zoumpourlis V, Kympouropoulos
SP, Tsoporis JN, Spandidos DA, et al: Long COVID and
neuropsychiatric manifestations (review). Exp Ther Med.
23(363)2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kampouridou K, Georgakopoulou VE, Chadia
K, Nena E and Steiropoulos P: Evaluating sleep disturbances in
patients recovering from COVID-19. Pneumon. 37(35)2024.
|
|
12
|
Karampitsakos T, Sotiropoulou V, Katsaras
M, Tsiri P, Georgakopoulou VE, Papanikolaou IC, Bibaki E, Tomos I,
Lambiri I, Papaioannou O, et al: Post-COVID-19 interstitial lung
disease: Insights from a machine learning radiographic model. Front
Med (Lausanne). 9(1083264)2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Oliveira AMDSS, Carvalho MA, Nacul L,
Cabar FR, Fabri AW, Peres SV, Zaccara TA, O'Boyle S, Alexander N,
Takiuti NH, et al: Post-viral fatigue following SARS-CoV-2
infection during pregnancy: A longitudinal comparative study. Int J
Environ Res Public Health. 19(15735)2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Metz TD, Reeder HT, Clifton RG, Flaherman
V, Aragon LV, Baucom LC, Beamon CJ, Braverman A, Brown J, Cao T, et
al: Post-acute sequelae of severe acute respiratory syndrome
coronavirus 2 (SARS-CoV-2) after infection during pregnancy. Obstet
Gynecol. 144:411–420. 2024.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Muñoz-Chápuli Gutiérrez M, Prat AS, Vila
AD, Claverol MB, Martínez PP, Recarte PP, Benéitez MV, García CA,
Muñoz EC, Navarro M, et al: Post-COVID-19 condition in pregnant and
postpartum women: A long-term follow-up, observational prospective
study. EClinicalMedicine. 67(102398)2024.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Falahi S, Abdoli A and Kenarkoohi A:
Maternal COVID-19 infection and the fetus: Immunological and
neurological perspectives. New Microbes New Infect.
53(101135)2023.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ghizzoni APO, Santos AK, de Braga RSL, Duz
JVV, Bouvier VD, de Souza MS and Silva DR: Clinical
characteristics, outcomes and persistent symptoms of pregnant women
with COVID-19: A retrospective cohort study. Int J Gynaecol Obstet:
Aug 30, 2024 (Epub ahead of print).
|
|
18
|
Page MJ, McKenzie JE, Bossuyt PM, Boutron
I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan
SE, et al: The PRISMA 2020 statement: An updated guideline for
reporting systematic reviews. BMJ. 372(n71)2021.PubMed/NCBI View
Article : Google Scholar
|
|
19
|
Wells GA, Shea B, O'Connell D, Peterson J,
Welch V, Losos M and Tugwell P: The Newcastle-Ottawa Scale (NOS)
for assessing the quality of nonrandomised studies in
meta-analyses. Ottawa Hospital Research Institute, Ottawa, ON,
2016.
|
|
20
|
Bruno AM, Zang C, Xu Z, Wang F, Weiner MG,
Guthe N, Fitzgerald M, Kaushal R, Carton TW, Metz TD, et al:
Association between acquiring SARS-CoV-2 during pregnancy and
post-acute sequelae of SARS-CoV-2 infection: RECOVER electronic
health record cohort analysis. EClinicalMedicine.
73(102654)2024.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Gu Y, Xing Y, Zhu J, Zeng L and Hu X:
Post-coronavirus disease 2019 (COVID-19) liver injury in pregnant
women: A retrospective cohort study. Clin Exp Obstet Gynecol.
50(248)2023.
|
|
22
|
Kandemir H, Bülbül GA, Kirtiş E, Güney S,
Sanhal CY and Mendilcioğlu İİ: Evaluation of long-COVID symptoms in
women infected with SARS-CoV-2 during pregnancy. Int J Gynaecol
Obstet. 164:148–156. 2024.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Vásconez-González J, Fernandez-Naranjo R,
Izquierdo-Condoy JS, Delgado-Moreira K, Cordovez S,
Tello-De-la-Torre A, Paz C, Castillo D, Izquierdo-Condoy N,
Carrington SJ and Ortiz-Prado E: Comparative analysis of long-term
self-reported COVID-19 symptoms among pregnant women. J Infect
Public Health. 16:430–440. 2023.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Vetrugno L, Sala A, Deana C, Meroi F,
Grandesso M, Maggiore SM, Isola M, De Martino M, Restaino S,
Vizzielli G, et al: Quality of life 1 year after hospital discharge
in unvaccinated pregnant women with COVID-19 respiratory symptoms:
A prospective observational study (ODISSEA-PINK study). Front Med
(Lausanne). 10(1225648)2023.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Belokrinitskaya TE, Frolova NI, Mudrov VA,
Kargina KA, Shametova EA, Agarkova MA and Zhamiyanova CT: Postcovid
syndrome in pregnant women. Obstet Gynecol. 6:60–8. 2023.
|
|
26
|
Yao Y, Sun L, Luo J, Qi W, Zuo X and Yang
Z: The effect of long-term COVID-19 infection on maternal and fetal
complications: A retrospective cohort study conducted at a single
center in China. Sci Rep. 14(17273)2024.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Twanow JE, McCabe C and Ream MA: The
COVID-19 pandemic and pregnancy: Impact on mothers and newborns.
Semin Pediatr Neurol. 42(100977)2022.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Marjenberg Z, Leng S, Tascini C, Garg M,
Misso K, El Guerche Seblain C and Shaikh N: Risk of long COVID main
symptoms after SARS-CoV-2 infection: A systematic review and
meta-analysis. Sci Rep. 13(15332)2023.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Xue P, Merikanto I, Delale EA, Bjelajac A,
Yordanova J, Chan RNY, Korman M, Mota-Rolim SA, Landtblom AM,
Matsui K, et al: Associations between obesity, a composite risk
score for probable long COVID, and sleep problems in SARS-CoV-2
vaccinated individuals. Int J Obes (Lond). 48:1300–1306.
2024.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Fatima S, Ismail M, Ejaz T, Shah Z, Fatima
S, Shahzaib M and Jafri HM: Association between long COVID and
vaccination: A 12-month follow-up study in a low- to middle-income
country. PLoS One. 18(e0294780)2023.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Homann S, Mikuteit M, Niewolik J, Behrens
GMN, Stölting A, Müller F, Schröder D, Heinemann S, Müllenmeister
C, El-Sayed I, et al: Effects of pre-existing mental conditions on
fatigue and psychological symptoms post-COVID-19. Int J Environ Res
Public Health. 19(9924)2022.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Ellington S and Jatlaoui TC: COVID-19
vaccination is effective at preventing severe illness and
complications during pregnancy. Lancet. 401:412–413.
2023.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Garapati J, Jajoo S, Aradhya D, Reddy LS,
Dahiphale SM and Patel DJ: Postpartum mood disorders: Insights into
diagnosis, prevention, and treatment. Cureus.
15(e42107)2023.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Machado K and Ayuk P: Post-COVID-19
condition and pregnancy. Case Rep Womens Health.
37(e00458)2023.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Maisonneuve E, Favre G, Boucoiran I,
Dashraath P, Panchaud A and Baud D: Post-COVID-19 condition:
Recommendations for pregnant individuals. Lancet Reg Health Eur.
40(100916)2024.PubMed/NCBI View Article : Google Scholar
|