Introduction
The frequency of benign and malignant thyroid tumors
has experienced a significant rise in the last 20 years in the
Mainland of China, partially due to an increase in public
awareness, utilization of diagnostic tools and routine physical
examinations. Conventional thyroidectomy (ConT) through a
skin-crease incision in the anterior neck has been the proven,
efficacious surgical method for treating various thyroid tumors for
the past few decades. ConT requires a cervical collar incision,
leaving an unsightly scar. However, numerous patients with thyroid
tumors who require operation are young women and they are often
concerned about the cosmetic appearance of the scar. Consequently,
the demand for surgical procedures which avoid visible scars while
maintaining optimal functional and ideal cosmetic results is
increasing.
The goals of endoscopic thyroidectomy (ET) are to
limit external scarring and improve cosmesis, to reduce
postoperative pain, to enhance postoperative recovery and to
achieve these ends without compromising treatment efficacy. ET was
first described by Hüscher et al (1) in 1997. Most of the earlier endoscopic
approaches to the thyroid gland employed small cervical incisions
in the midline or laterally. To avoid a visible scar in the neck,
non-cervical approaches to the thyroid gland have been employed.
The most commonly used non-cervical approaches are the axillary
(2), the breast (3), the lateral (4) and also certain hybrid approaches
(5), such as the
axillary-bilateral breast approach, the bilateral axillo-breast
approach, the unilateral axillo-breast approach, and the
postauricular and axillary approach. Among these, the breast
approach has emerged as the clear favorite as evidenced by its
exponential growth in number in the Mainland of China (6).
It may be due to the Chinese culture that avoidance
of a cervical neck scar justifies the expense of technological
investment combined with a lengthy procedure to approach the
thyroid compartment remotely, which has promoted the widespread
application of ET in the Mainland of China (6). The preponderance of females among
patients requiring thyroid surgery has probably been another
influence in the development and patient acceptance of ET. In our
department, ET via breast approach was developed in 2007 and, since
then, approximately 300 operations have been performed. The aim of
this retrospective study was to compare the surgical results of
patients who underwent ET and to those of patients who underwent
ConT. Herein, we summarize the results of the ET and demonstrate
its feasibility and safety via breast approach for the treatment of
benign thyroid tumors.
Materials and methods
Patients
From January 2007 to December 2010, 285 patients
were treated with ET via breast approach. All were concerned with
the cosmetic appearance of the neck and chose this procedure as the
preferred surgical treatment. Another group of 352 patients treated
with ConT during the same period in our department served as
matched controls. The characteristics of the patients are shown in
Table I. This was a retrospective
analysis of the surgical outcomes for two types of thyroidectomy
(ET and ConT), performed by the same group of surgeons. All
operations in both groups were performed by a single surgeon (F.
Cao) assisted by two of the authors (B. Xie and B. Cui). All cases
were identified from a thyroid surgery patient database,
prospectively maintained by one of the authors (D. Xu). Informed
consent was obtained from each patient before surgery in all cases.
The study was approved by the Institutional Review Board of our
hospital.
 | Table I.Clinical data and surgical outcomes of
the patients. |
Table I.
Clinical data and surgical outcomes of
the patients.
| ET (n=285) | ConT (n=352) | P-value |
|---|
| Age (years) | | | <0.001 |
| Mean (SD) | 35.7 (12.59) | 40.0 (11.14) | |
| Range | 17–55 | 22–68 | |
| Gender | | | |
| Male (n/%) | 10/3.5 | 42/11.9 | |
| Female (n/%) | 275/96.5 | 310/88.1 | |
| Operative
methods | | | |
| Unilateral
lobectomy (n/%) | 126/44.2 | 163/46.3 | |
| Bilateral total
thyroidectomy (n/%) | 159/55.8 | 189/53.7 | |
| Operative time
(min) | | | |
| Unilateral
lobectomy (mean/SD) | 79.9/20.10 | 45.4/11.90 | <0.001 |
| Bilateral total
thyroidectomy (mean/SD) | 89.9/14.60 | 60.0/8.44 | <0.001 |
| Postoperative
hospital stay (days, mean /SD) | 5.5/0.50 | 5.3/0.75 | 0.002 |
| Conversion to open
surgical procedure | None | None | |
| RLN
identification | All | All | |
| PG
identification | All | All | |
All patients were evaluated pre-operatively using
ultrasonography, computed tomographic scan and fine-needle
aspiration cytology. All patients underwent pre-operative direct
laryngoscopy to assess vocal cord motility. The inclusion criteria
used for ET are shown in Table II.
The ConT group was chosen with the same inclusion criteria used for
ET. The main surgical outcome measures were operative time (the
interval from the skin incision to closure of the skin),
postoperative hospital stay, identification of recurrent laryngeal
nerves (RLN), identification of parathyroid glands, conversion to
an open surgical procedure, postoperative calcemia, postoperative
vocal alteration, postoperative complications and the pathological
characteristics. The following complications were analyzed:
transient or permanent RLN palsy, transient or permanent
hypocalcemia, reoperation for hemorrhage and postoperative pain.
Patients were tested for hypocalcemia pre-operatively and on
postoperative days 1 and 30. All patients with postoperative
calcium level below the lower limit of the normal range (8.2–10.6
mg/dl) were considered as having hypocalcemia. In this study,
hypocalcemia and RLN palsy were defined as permanent when there was
no evidence of recovery within 30 days after surgery. The patients
in both groups were followed up at days 7 and 30 through office
visits or phone calls. Follow-up examination included hoarse voice,
swallowing difficulty, hypesthesia or paresthesia and cosmetic
satisfaction. The patients were asked to grade the cosmetic
appearance of their wound 1 month after surgery. All patients were
provided with four ratings of cosmetic satisfaction: poor,
acceptable, good and excellent. The data were analyzed for
statistical significance using a Student's t-test and Chi-square
test; p-values <0.05 were considered significant.
 | Table II.Inclusion criteria. |
Table II.
Inclusion criteria.
| No suspicion of
malignancy |
| A fine-needle
aspiration cytology report of a benign thyroid lesion |
| Thyroid goiter or
nodules <5 cm in diameter |
| Thyroid gland volume
<25 ml |
| No history of
thyroiditis |
| No history of
hyperthyroidism |
| No previous neck
surgery |
| No irradiation |
Surgical procedure
ET procedure
Under general anesthesia and endotracheal
intubation, ET via breast approach was performed. Patients were
placed in the supine position with extension of the neck. A 15-mm
incision in the presternal region (for placement of the Hanson
trocar), and two 5-mm incisions in the superior areas of both
mammary areolas were selected (Fig.
1). A dilute epinephrine saline solution (1:200,000) was
injected into the subcutaneous space in the breast and subplatysmal
space in the neck to ease flap dissection and to prevent bleeding.
Using a vascular tunneler (GORE Tunneler-Standard Curve Access;
W.L. Gore & Associates, Inc., Flagstaff, AZ, USA), the working
space was extended. After blunt dissection of the subcutaneous
tissue of the anterior chest wall through this incision, a 15-mm
trocar was inserted. The working area was maintained with low
pressure CO2 insufflation at a pressure of 6 mmHg, and a
30-degree 5-mm flexible endoscope (Olympus, Tokyo, Japan) was
inserted through the trocar. The working space was made widely to
the level of the thyroid cartilage cranially and to the medial edge
of each of the sternocleidomastoid muscles laterally with the
visual guidance of the endoscope. After the working space was set
up, two 5-mm incisions were made and two 5-mm trocars were inserted
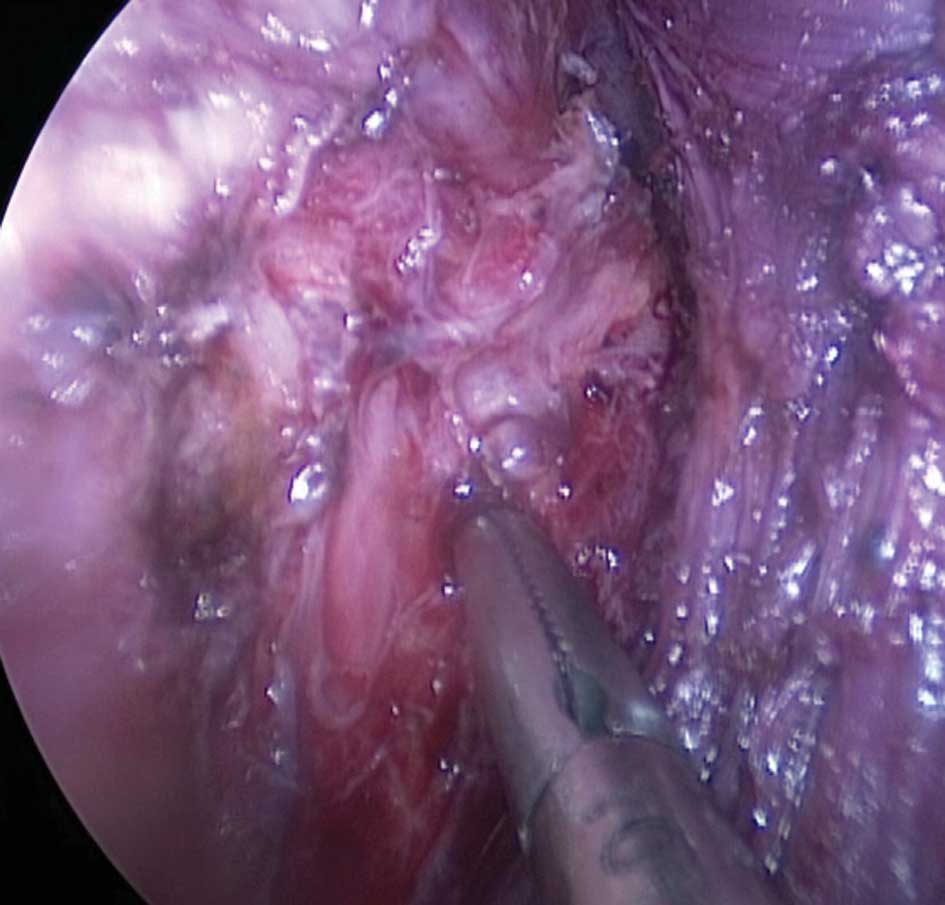
(Fig. 2). Thyroid vessel
management and thyroidectomy were performed endoscopically using a
5-mm ultrasonic coagulation device (Harmonic Scalpel; Ethicon
Endosurgery, USA). After dissecting the strap muscles in the
midline endoscopically, the isthmus was divided. Traction over the
ipsilateral strap muscles was then oriented laterally to reveal the
right lobe. After cutting the inferior thyroid arteries and veins
and the middle thyroid vein, the lobe was retracted downward to
expose the superior thyroid arteries, which were then dissected by
the Harmonic Scalpel. After that, the lobe was gently lifted up and
the whole cervical course of the RLN up to the inferior constrictor
of the pharynx was traced and protected, as well as both the
inferior and superior parathyroid glands. The magnification of the
endoscope allowed easy identification of the RLN and the
parathyroid glands (Figs. 3 and
4). Lastly, the lobe was excised
from the inferior pole up towards the superior pole. The left lobe
was excised in the same manner to the right lobe. The resected
specimen was inserted into a retrieval bag and retrieved through
the 15-mm port. A frozen section of the resected specimen was
examined intraoperatively for pathological confirmation.
Homeostasis was checked at the end of dissection. After cleaning
the cavity with physiological saline solution, the strap muscles
were sutured. An aspiration drainage tube was left in situ
in the central compartment, and it was removed 48 h after surgery
(Fig. 5).
ConT procedure. Under general anesthesia, the
patient was placed in a supine position and the neck was extended.
A 5- to 8-cm transverse collar skin incision was made in the
mid-line of the anterior neck 2 cm above the sternal notch, and the
lower layer of the platysma was exposed under direct vision.
Subplatysmal flap dissection was performed to achieve adequate
working space from the sternal notch to the hyoid bone level
superiorly, and both the medial side of the anterior border of the
sternocleidomastoid muscle laterally. The midline of the strap
muscles was divided vertically and the thyroid gland was exposed. A
bilateral total thyroidectomy or unilateral lobectomy was performed
manually in the same manner as the endoscopic procedure. Before
concluding the operation, a 3-mm closed suction drain was placed
through the separate skin incision. The wounds were closed with
absorbable suture material by a continuous subcutis suture
method.
Results
Two hundred and eighty-five patients underwent ET
via breast approach (ET group), and 352 patients underwent ConT
(ConT group). The mean ages of the patients were 35.7±12.59 years
(range 17–55) in the ET group and 40.0±11.14 years (range 22–68) in
the ConT group (P<0.001). The male-to-female gender ratios were
10:275 (1:27.5) in the ET group and 42:310 (1:7.38) in the ConT
group (P<0.001). A unilateral lobectomy was performed in 126
patients (44.2%) of the ET group and in 163 patients (46.3%) of the
ConT group. A bilateral total thyroidectomy was performed in 159
patients (55.8%) of the ET group and in 189 patients (53.7%) of the
ConT group. Patient characteristics are presented in Table I.
The total operative time for the ET group was
significantly longer compared to the ConT group (79.9±20.10 vs.
45.4±11.90 min, P<0.001, for unilateral lobectomy; and
89.9±14.60 vs. 60.0±8.44 min, P<0.001, for bilateral total
thyroidectomy) (Table I). The
length of postoperative hospital stay of the ET group was
significantly longer compared to that of the ConT group (5.5±0.50
vs. 5.3±0.75 days, P=0.002). There was no case of conversion to the
conventional open surgery in the ET group. RLN and parathyroid
glands were identified in all cases (Table I).
An endoscopic approach provides better, magnified
views of the RLN and the parathyroid glands resulting in fewer
complications. The postoperative complications of both groups are
shown in Table III. Transient
hypocalcemia was found in 1.4% (4/285) of the ET group and 4.3%
(15/352) of the ConT group cases. No permanent hypocalcemia
occurred in the ET group, but one occurred in the ConT group.
Transient RLN palsy occurred in 3.2% (9/285) of the ET group and
3.7% (13/352) of the ConT group. No permanent RLN palsy occurred in
each group. Postoperative pain in the ET and ConT groups occurred
in 4.6% (13/285) and 4.3% (15/352), respectively, at 24 h after
operation.
 | Table III.Postoperative complications. |
Table III.
Postoperative complications.
| ET (n=285) | ConT (n=352) | |
|---|
|
|---|
| Postoperative
complications | n (%) | n (%) | P-value |
|---|
| Transient RLN
palsy | 9 (3.2) | 13 (3.7) | 0.713 |
| Permanent RLN
palsy | 0 | 0 | |
| Transient
hypocalcemia | 4 (1.4) | 15 (4.3) | 0.035 |
| Permanent
hypocalcemia | 0 | 1 (0.3) | 0.368 |
| Reoperation for
hemorrhage | 0 | 0 | |
| Postoperative
pain | 13 (4.6) | 15 (4.3) | 0.854 |
| Hoarse voice | 5 (1.8) | 6 (1.7) | 0.962 |
| Swallowing
difficulty | 0 | 0 | |
| Hypesthesia or
paresthesia | 1 (0.4) | 2 (0.6) | 0.690 |
To evaluate the cosmetic results, a simple
questionnaire was used (Table IV).
Among the 282 responses in the ET group, 78.7% (222/282) were
‘Excellent’, 13.9% (39/282) were ‘Good’, 7.4% (21/282) were
‘Acceptable’ and there were no ‘Poor’ responses. Among the 352
responses in the ConT group, 7.4% (26/352) were ‘Excellent’, 51.4%
(181/352) were ‘Good’, 37.5% (132/352) were ‘Acceptable’ and 3.7%
(13/352) were ‘Poor’. Patients in the ET group had statistically
significantly better cosmetic results compared to the ConT group
(Table IV). No tracheal and
esophageal injury occurred in each group.
 | Table IV.Patient satisfaction with cosmetic
results. |
Table IV.
Patient satisfaction with cosmetic
results.
| ET (n=282) | ConT (n=352) | |
|---|
|
|---|
| Cosmetic effects | n (%) | n (%) | P-value |
|---|
| Excellent | 222 (78.7) | 26 (7.4) | <0.001 |
| Good | 39 (13.9) | 181 (51.4) | <0.001 |
| Acceptable | 21 (7.4) | 132 (37.5) | <0.001 |
| Poor | 0 | 13 (3.7) | 0.001 |
Two hundred and twenty-one patients (77.5%) in the
ET group and 256 patients (72.7%) in the ConT group had nodular
goiter on histopathological examination (Table V). Forty-one patients (14.4%) in
the ET group and 57 patients (16.2%) in the ConT group had
follicular adenoma, and 20 patients (7.0%) in the ET group and 39
patients (11.1%) in the ConT group had Hurthle cell adenoma. Only 3
patients (1.1%) in the ET group had cystic lesions (Table V).
 | Table V.Histopathological findings. |
Table V.
Histopathological findings.
| ET (n=285) | ConT (n=352) |
|---|
|
|---|
| Histopathology | n (%) | n (%) |
|---|
| Nodular goiter | 221 (77.5) | 256 (72.7) |
| Adenoma | | |
| Follicular
adenoma | 41 (14.4) | 57 (16.2) |
| Hurthle cell
adenoma | 20 (7.0) | 39 (11.1) |
| Cystic lesions | 3 (1.1) | 0 |
Discussion
A new surgical technique when developed has to face
up to its conventional standard and be comparable when it comes to
results achieved, complications, safety, technical feasibility and
cost-to-benefit ratio. A considerable recent surge has occurred in
the development of endoscopic techniques in thyroid surgery. Since
Gagner (7) and Hüscher et
al (1) first reported
successful endoscopic neck surgery in 1996 and 1997, several
endoscopic thyroid surgical techniques have been developed
(8–14). Minimizing surgical stress, cosmetic
concerns and improving the postoperative quality of life are the
main motivations for developing novel endoscopic thyroid surgical
techniques. According to the insertion site of surgical
instruments, endoscopic surgery can be classified as cervical
(15,16), anterior chest wall (10), breast (17), axillary (18–20)
and axillary breast approaches (21). These various techniques of
endoscopic thyroidectomy have their own advantages and pitfalls.
There were five published series involving 169 patients of ET
performed via breast approach (17). We carried out this clinical
observation after conducting 285 cases with ET via breast approach
to provide an adequate match with our experience in conventional
open surgery.
The mean operative time of ET in our series was
79.9±20.10 min for unilateral lobectomy and 89.9±14.60 min for
bilateral total thyroidectomy (Table
I). The acceptable operative time achieved was due to the short
learning curve, the good surgical view, magnification of the
surgical field, excellent instrumentation and the breast approach
to the thyroid gland. Operative time is the only factor in our
series that did not compare favorably to the open surgical
procedure. However, the longer operative time compared to the open
surgery group could be possibly reduced further through the
accumulation of experience.
Although the conversion rates of ET via breast
approach are reported to be 0–13% (22–24),
we did not have any conversions. This directly relates to the prior
endoscopic experience of the main surgeon in endoscopic thyroid
surgery with formal training as well as his own experience with
previous open thyroid lobectomies. As is the case with open
surgery, exposure to a high volume of cases enables one to be
comfortable with the surgical anatomy.
The common complications of endoscopic thyroidectomy
were transient/permanent hypocalcemia and transient/permanent RLN
palsy. With the lateral view of the thyroid gland and the
paratracheal region, we easily identified and preserved the RLN and
parathyroid glands while performing the ET. In the present study,
the superior parathyroid gland was often easier to identify and
dissect from the thyroid gland on a vascular pedicle than in open
thyroidectomy. We experienced a lower incidence of transient
hypocalcemia in the ET group than previous reports (22–24)
(Table III). All patients with
transient hypocalcemia recovered within 1 month. Several patients
who underwent our endoscopic thyroid surgery reported mild
hypesthesia and paresthesia in the neck and anterior chest wall. In
addition, some of the patients reported discomfort while swallowing
(Table III). Therefore, the
invasiveness of significant dissection to achieve an adequate
working space should be improved through the accumulation of
experience.
Cosmetic results are difficult to evaluate because
of the reliance on the subjective judgment of the patient. However,
most of the patients in the ET group were satisfied with the
operative scars (Table IV), and
222 patients (78.7%) were extremely satisfied with their cosmetic
results.
ET via breast approach was not pioneered by Chinese
endoscopic surgeons, but we did contribute towards improvement in
technical details. Firstly, prior injection of 300 ml of diluted
epinephrine saline solution into the subcutaneous space by a long
needle (modified from a Veress needle) along the prospective
operative tunnel up to the sternal notch greatly facilitates the
creation of an adequate working space, which results in better pain
and bleeding control. Secondly, low-pressure CO2 (6
mmHg) was applied and was still able to obtain a satisfactory
operative view. No subcutaneous emphysema occurred. Therefore, we
believe that CO2 insufflation for endoscopic thyroid
surgery is safe if insufflation is maintained at a low pressure.
Thirdly, the Harmonic Scalpel exclusively for hemostasis was used
in ET without any ties or clips, and no postoperative hemorrhage or
hematoma occurred in the ET group. The advantage of this device is
that it does not smoke, causes minimal tissue injury, is safe for
the surgeon and patient and facilitates dissection (22,25,26).
Fourthly, the 30° endoscope was used, as it has a larger visual
field, and thus makes the best use of operating space. Lastly, some
major improvements and safer technologies, such as intraoperative
neuromonitoring to prevent RLN paralysis and early measurement of
quick intraoperative parathyroid hormone to avert symptomatic
hypocalcemia, have been proposed and would be considered for
application to thyroid surgery in subsequent years.
In conclusion, ET performed via breast approach is a
technically feasible and safe procedure with excellent cosmetic
results for patients with benign thyroid tumors. In addition to
improved cosmesis, numerous patients experience decreased pain and
faster recovery, and are at no increased risk for
complications.
Acknowledgements
This study was supported by the
Science Research Fund of Taizhou.
References
|
1.
|
Hüscher CS, Chiodini S, Napolitano C and
Recher A: Endoscopic right thyroid lobectomy. Surg Endosc.
11:8771997.
|
|
2.
|
Duncan TD, Rashid Q, Speights F and Ejeh
I: Endoscopic transaxillary approach to the thyroid gland: our
early experience. Surg Endosc. 21:2166–2171. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Cho YU, Park IJ, Choi KH, Kim SJ, Choi SK,
Hur YS, Lee KY, Ahn SI, Hong KC, Shin SH, Kim KR and Woo ZH:
Gasless endoscopic thyroidectomy via an anterior chest wall
approach using a flap-lifting system. Yonsei Med J. 48:480–487.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Palazzo FF, Sebag F and Henry JF:
Endocrine surgical technique: endoscopic thyroidectomy via the
lateral approach. Surg Endosc. 20:339–342. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Lee KE, Kim HY, Park WS, Choe JH, Kwon MR,
Oh SK and Youn YK: Postauricular and axillary approach endoscopic
neck surgery: a new technique. World J Surg. 33:767–772. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Ng WT: Endoscopic thyroidectomy in China.
Surg Endosc. 23:1675–1677. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Gagner M: Endoscopic subtotal
parathyroidectomy in patients with primary hyperparathyroidism. Br
J Surg. 83:8751996. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Miccoli P, Pinchera A, Cecchini G, Conte
M, Bendinelli C, Vignali E, Picone A and Marcocci C: Minimally
invasive, video-assisted parathyroid surgery for primary
hyperparathyroidism. J Endocrinol Invest. 20:429–430. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Yeung GH: Endoscopic surgery of the neck:
a new frontier. Surg Laparosc Endosc. 8:227–232. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Shimizu K, Akira S, Jasmi AY, Kitamura Y,
Kitagawa W, Akasu H and Tanaka S: Video-assisted neck surgery:
endoscopic resection of thyroid tumors with a very minimal neck
wound. J Am Coll Surg. 188:697–703. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Bellantone R, Lombardi CP, Raffaelli M,
Rubino F, Boscherini M and Perilli W: Minimally invasive, totally
gasless video-assisted thyroid lobectomy. Am J Surg. 177:342–343.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Yeh TS, Jan YY, Hsu BR, Chen KW and Chen
MF: Video-assisted endoscopic thyroidectomy. Am J Surg. 180:82–85.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Ikeda Y, Takami H, Niimi M, Kan S, Sasaki
Y and Takayama J: Endoscopic thyroidectomy by the axillary
approach. Surg Endosc. 15:1362–1364. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Yamashita H, Watanabe S, Koike E, Ohshima
A, Uchino S, Kuroki S, Tanaka M and Noguchi S: Video-assisted
thyroid lobectomy through a small wound in the submandibular area.
Am J Surg. 183:286–289. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Miccoli P, Berti P, Bendinelli C, Conte M,
Fasolini F and Martino E: Minimally invasive video-assisted surgery
of the thyroid: a preliminary report. Langenbecks Arch Surg.
385:261–264. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Gagner M and Inabnet WB III: Endoscopic
thyroidectomy for solitary thyroid nodules. Thyroid. 11:161–163.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Tan CT, Cheah WK and Delbridge L:
‘Scarless’ (in the neck) endoscopic thyroidectomy (SET): an
evidence-based review of published techniques. World J Surg.
32:1349–1357. 2008.
|
|
18.
|
Ikeda Y, Takami H, Sasaki Y, Kan S and
Niimi M: Endoscopic resection of thyroid tumors by the axillary
approach. J Cardiovasc Surg. 41:791–792. 2000.PubMed/NCBI
|
|
19.
|
Ikeda Y, Takami H, Sasaki Y, Kan S and
Niimi M: Endoscopic neck surgery by the axillary approach. J Am
Coll Surg. 191:336–340. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Yoon JH, Park CH and Chung WY: Gasless
endoscopic thyroidectomy via an axillary approach: experience of 30
cases. Surg Laparosc Endosc Percutan Tech. 16:226–231. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Chung YS, Choe JH, Kang KH, Kim SW, Chung
KW, Park KS, Han W, Noh DY, Oh SK and Youn YK: Endoscopic
thyroidectomy for thyroid malignancies: comparison with
conventional open thyroidectomy. World J Surg. 31:2302–2306. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Ohgami M, Ishii S, Arisawa Y, Ohmori T,
Noga K, Furukawa T and Kitajima M: Scarless endoscopic
thyroidectomy: breast approach for better cosmesis. Surg Laparosc
Endosc Percutan Tech. 10:1–4. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Park YL, Han WK and Bae WG: 100 cases of
endoscopic thyroidectomy: breast approach. Surg Laparosc Endosc
Percutan Tech. 13:20–25. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Sasaki A, Nakajima J, Ikeda K, Otsuka K,
Koeda K and Wakabayashi G: Endoscopic thyroidectomy by the breast
approach: a single institution's 9-year experience. World J Surg.
32:381–385. 2008.PubMed/NCBI
|
|
25.
|
Amaral JF: The experimental development of
an ultrasonically activated scalpel for laparoscopic use. Surg
Laparosc Endosc. 4:92–99. 1994.PubMed/NCBI
|
|
26.
|
Voutilainen PE, Haapiainen RK and Haglund
CH: Ultrasonically activated shears in thyroid surgery. Am J Surg.
175:491–493. 1998. View Article : Google Scholar : PubMed/NCBI
|