Introduction
Vertigo in childhood is not easy to diagnose since
this rare disorder has a number of causes, ranging from traumatic,
infective and malignant disorders of the central nervous system to
a wide variety of otological disorders, including migraine, benign
paroxysmal vertigo (BPV) and psychosomatic disorders. BPV of
childhood is defined as recurrent attacks of severe vertigo
resolving spontaneously after minutes to hours and is referred to
as a periodic syndrome of childhood, migraine equivalent, or
migraine precursor (1,2). Reports of BPV are more common in the
West than in the East (3). Basilar
migraine (BM) is a type of migraine commencing with visual
disturbance, vertigo, ataxia, slurred speech, tinnitus, sensory
disturbance and occipital headache (1,4).
Patients with BM aged <10 years are quite rare. In the current
study, we treated a 6-year-old male with BPV transitioning into
atypical BM.
Case report
A 6-year-old male visited our hospital after
experiencing repeated attacks of vertigo for 3 months. The patient
experienced vertigo forcing the adoption of a crouching position to
maintain balance once every few months for several years. The
attacks of vertigo lasted for several hours and were accompanied by
nausea, vomiting, intense fear and loss of consciousness continuing
for ∼30 sec to 1 min immediately after the onset of vertigo. A
diagnosis of delayed endolymphatic hydrops had been made by a
previous physician and the patient was taking isosorbide, although
the symptoms had not improved. The patient’s mother had a history
of migraine for which triptan nasal spray was effective.
No nystagmus was observed during the vertigo
attacks. Blood tests and cervical spine X-rays, as well as computed
tomography and magnetic resonance imaging scans of the brain
revealed no abnormal findings. The results of
electro-nystagmography and the caloric test were unremarkable in
the ears. Pure-tone audiometry revealed profound right-side
sensorineural hearing loss (SNHL; Fig.
1). Auditory brain stem responses to 105 dB nHL clicks were
absent in the right ear.
Among the differential diagnoses, delayed
endolymphatic hydrops, epilepsy and BM were considered. Delayed
endolymphatic hydrops was considered unlikely since the caloric
test results were unremarkable, no nystagmus occurred during the
vertigo attacks, the loss of consciousness during vertigo attacks
was an atypical symptom, there was no change in hearing and the
treatment for delayed endolymphatic hydrops demonstrated no effect.
In addition, electroencephalography revealed no epileptic seizure
waves. The patient became aware of the unilateral SNHL before the
patient’s family noticed. After the family reported right-side
SNHL, subclinical mumps infection was diagnosed based on elevated
levels of mumps virus IgG antibodies, although there were no clear
clinical symptoms of mumps. Finally, the patient was considered
atypical BM due to the attacks of vertigo. The vertigo forcing the
adoption of a crouching position once every few months was
considered to be a manifestation of BPV due to the unremarkable
electronystagmographic and electroencephalographic results. Since
the attacks of vertigo were accompanied by a loss of consciousness,
we concluded that this patient had atypical BM transitioning from
BPV.
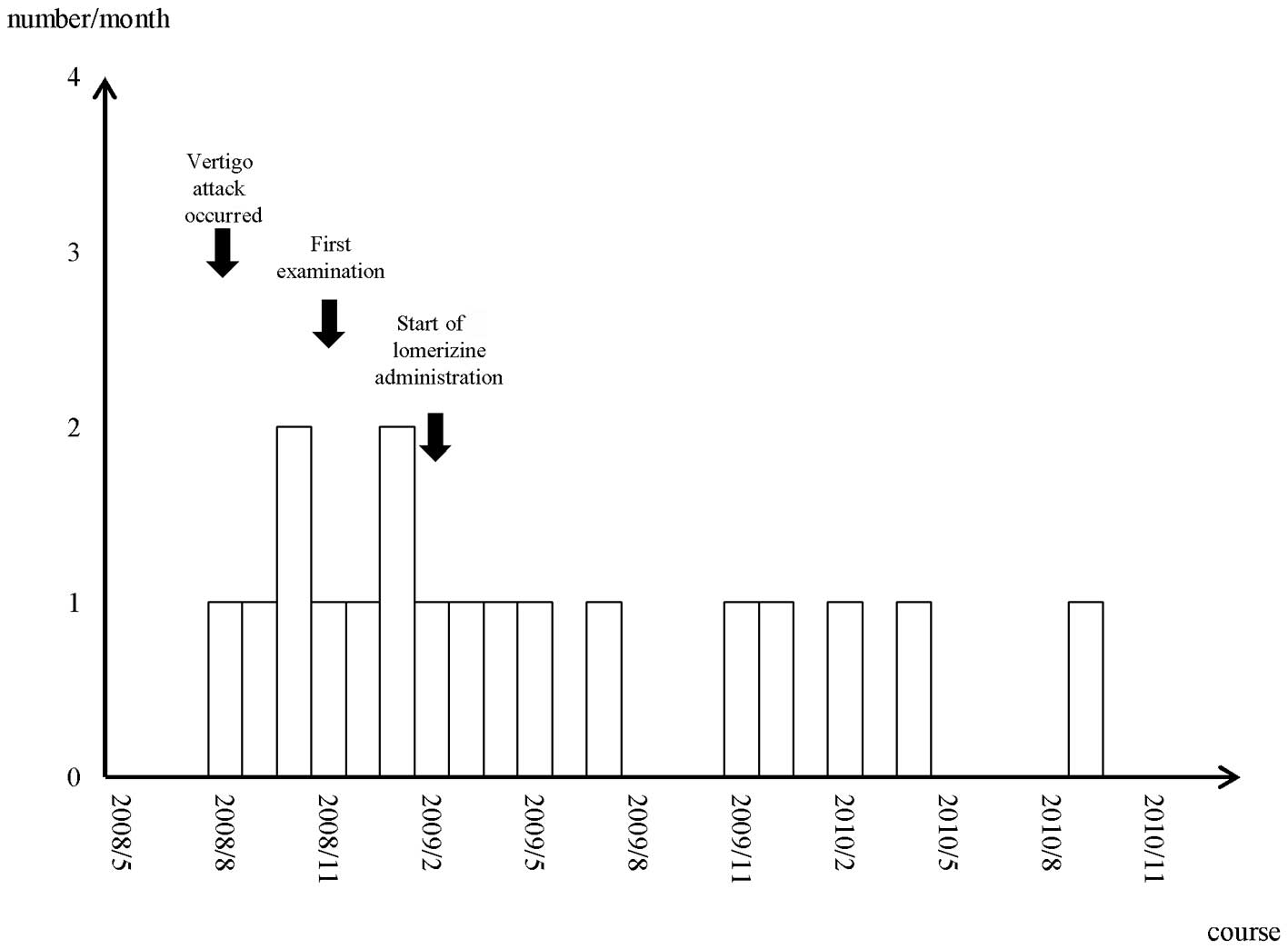
Based on our diagnosis, lomerizine (5 mg)
administration was initiated to prevent the attacks and
cyproheptadine (2 mg) was added during attacks. The number and
severity of vertigo attacks was reduced following the initiation of
therapy (Fig. 2). The patient’s
attacks of vertigo are currently well-controlled with lomerizine.
Informed consent was obtained from the patient’s family.
Discussion
According to the International Classification of
Headache Disorders second edition (ICHD-II), BPV is defined as
recurrent (>5) attacks of severe vertigo resolving spontaneously
after minutes to hours (1). BPV is
not accompanied by hearing loss and thus we regarded the patient’s
unilateral SNHL as congenital deafness or mumps-related
deafness.
BPV was defined by Basser in 1964 (2). BPV begins early, at 1–4 years old and
is equally distributed across genders. Vertigo is associated with
nystagmus, ataxia and other accompanying signs, including
phonophobia, photophobia and visual disturbances (5). Russell and Abu-Arafeh reported that
the prevalence of BPV is ∼2.1% (6). BPV has a good prognosis and usually
disappears with age, although it is occasionally associated with
migraine later in life. In the present study, the patient’s mother
had migraine; BPV in patients with a family history of migraine may
have similar clinical features and trigger factors (6). It has been reported that BPV is
closely related to migraine; however, only 4 cases of BM
transitioning from BPV have been reported. Golden and French
identified that 1 in 8 patients with BM have an original diagnosis
of BPV following the first examination (7). Dieterich and Brandt reported that
three children with BM in their study could have been diagnosed
with BPV following the first attacks (8). Therefore, we conclude that the
patient in the current study had BM transitioning from BPV when the
vertigo attacks were accompanied by a loss of consciousness.
In the literature, BPV transitioning to BM was
observed in 1 of 8 patients in one study (7) and in 3 of 90 patients in another
study (8). Therefore, the
frequency of transition was 12.5 and ∼3.3%, respectively. Dieterich
and Brandt identified a family history of migraine for 71 of 90
patients and of those 71 patients it was the mothers of 29 patients
who had migraines (8). Golden and
French determined a family history of migraines in 7 of the 8
pediatric patients and 5 of the patient’s mothers had migraines
(7). In the present study, the
patient’s mother also had migraines, therefore the most important
background factor in BPV transitioning to BM appears to be a family
history of migraines, particularly in the mother. The trigger of
the vertigo attacks remains uncertain; however, an increase in
light stimulation may have affected the change in symptoms.
Chang and Young reported that caloric/vestibular
evoked myogenic potential (VEMP) test results indicated that upper
and lower brain stem lesions occurred in pediatric patients with
BPV (9). Dieterich and Brandt
indicated that the brain stem was involved as the originating site
of vertigo (8). The patient in the
present study demonstrated unremarkable responses in caloric
testing. Chang and Young also reported that the combined caloric
and VEMP test results show abnormalities in 70% of childhood BPV
patients (9). Liao and Young
identified that 75% of BM patients present abnormalities when the
results of caloric and VEMP testing were combined (4). These results did not differ
significantly, indicating the similarity of the two disorders. In
addition, these results demonstrate that the VEMP test may serve as
a diagnostic tool in evaluating vertigo in childhood.
Although BPV attacks are generally so brief that the
subsequent administration of drugs is unnecessary, one report
commented that analgesics and antiserotonergic drugs may be useful
for preventing or treating attacks of headache (5). To the best of our knowledge, this is
the first report of lomerizine treatment in a pediatric patient
with BPV. Our results suggest that lomerizine administration is one
treatment option for particularly severe cases of BPV.
BM was defined by Bickerstaff in 1961 (10). The symptoms include visual
disturbances, vertigo, ataxia, slurred speech, tinnitus, sensory
disturbances and occipital headache (4). The mechanism of premonitory migraine
symptoms was attributed to dysfunction of the brainstem or the
occipital cortex. The first BM attack was reported to occur between
the ages of 10–72 (mean, 38) years in females and 7–72 (mean, 42)
years in males (8). In the
literature, few cases of BM developed in patients aged <10
years. Thus, our 6-year-old patient with BM is a rare example.
According to the ICHD-II, headache attack is
essential for the diagnosis of BM (1). In the present study, the patient had
a stiff neck and shoulders; however, an evident headache did not
appear as part of the disorder during the clinical course.
Alternatively, the occurrence of headache may not necessarily be
required for a diagnosis of BM. Dieterich and Brandt reported that
vertigo was not associated with headache in 17 of 90 patients
(8). Moreover, the authors
suggested monosymptomatic episodic vertigo without accompanying
headache and the disappearance of vertigo after receiving treatment
for migraine substantiated the diagnosis of migraine. Additionally,
Brantberg et al identified that 21 of 40 patients with
migraine-associated vertigo (MAV) experienced headache with attacks
of vertigo (11).
Ergotamine and sumatriptan are contraindicated for
the medical treatment of BM since they contract the cerebrovascular
system, resulting in the occurrence of aura and other symptoms.
Lomerizine, a calcium channel blocker that markedly improves the
vertebrobasilar circulation, prevents vertigo attacks. Iwasaki
et al reported that 27 of 33 adult patients with MAV
responded to lomerizine (12). The
patient in the present study received lomerizine and the attacks of
vertigo are now well-controlled. We administered half an adult dose
since the patient was 6-years-old and weighed 24 kg. The frequency
of attacks may be reduced by preventive medication with β-receptor
blockers, serotonin antagonists, antidepressants and
anticonvulsants (8,13).
The patient in the current study appeared to
experience attacks of vertigo more often after meals, late at night
and early in the morning. Future studies should investigate whether
thermal stimulation or brain hypoperfusion affect the onset of
vertigo. Lifestyle guidance, including advising patients not to
overeat and avoid becoming too cold at bedtime and upon awakening,
may be effective in preventing attacks.
In conclusion, we experienced a rare case of a
6-year-old male with atypical BM. Children who present with attacks
of vertigo and have a family history of migraine, particularly in
their mothers, require long-term observation.
Acknowledgements
The authors thank Dr Hiroki Hasumi and
Dr Mitsuhiko Hara for clinical support.
References
|
1.
|
Headache Classification Subcommittee of
the International Headache Society: The International
Classification of Headache disorders: 2nd edition. Cephalalgia.
24(Suppl 1): S9–S160. 2004.
|
|
2.
|
Basser LS: Benign paroxysmal vertigo of
childhood (A variety of vestibular neuronitis). Brain. 87:141–152.
1964. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Choung YH, Park K, Moon SK, Kim CH and Ryu
SJ: Various causes and clinical characteristics in vertigo in
children with normal eardrums. Int J Pediatr Otorhinolaryngol.
67:889–894. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Liao LJ and Young YH: Vestibular evoked
myogenic potentials in basilar artery migraine. Laryngoscope.
114:1305–1309. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Lanzi G, Balottin U, Fazzi E, Tagliasacchi
M, Manfrin M and Mira E: Benign paroxysmal vertigo of childhood: a
long-term follow up. Cephalalgia. 14:458–460. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Russell G and Abu-Arafeh I: Paroxysmal
vertigo in children - an epidemiological study. Int J Pediatr
Otorhinolaryngol. 49(Suppl 1): S105–S107. 1999. View Article : Google Scholar
|
|
7.
|
Golden GS and French JH: Basilar artery
migraine in young children. Pediatrics. 56:722–726. 1975.PubMed/NCBI
|
|
8.
|
Dieterich M and Brandt T: Episodic vertigo
related to migraine (90 cases): vestibular migraine? J Neurol.
246:883–892. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Chang CH and Young YH: Caloric and
vestibular evoked myogenic potential tests in evaluating children
with benign paroxysmal vertigo. Int J Pediatr Otorhinolaryngol.
71:495–499. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Bickerstaff ER: Basilar artery migraine.
Lancet. 1:15–17. 1961. View Article : Google Scholar
|
|
11.
|
Brantberg K, Trees N and Baloh RW:
Migraine-associated vertigo. Acta Otolaryngol. 125:276–279. 2005.
View Article : Google Scholar
|
|
12.
|
Iwasaki S, Ushio M, Chihara Y, Ito K,
Sugasawa K and Murofushi T: Migraine-associated vertigo: clinical
characteristics of Japanese patients and effect of lomerizine, a
calcium channel antagonist. Acta Otolaryngol Suppl. 559:45–49.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Neuhauser H, Leopold M, von Brevern M,
Arnold G and Lempert T: The interrelations of migraine, vertigo,
and migrainous vertigo. Neurology. 56:436–441. 2001. View Article : Google Scholar : PubMed/NCBI
|