Introduction
With the increasing incidence of coronary artery
disease (CAD), coronary angiography, as the gold standard for CAD
diagnosis, has obtained growing popularity. An increasing number of
hospitals have acquired the ability and qualifications to perform
coronary angiography. Through clinical studies, it has been
identified that multivessel lesions are common in stable angina and
acute coronary syndrome (1,2), and
are an independent predictor of CAD that affects the prognosis of
patients (3). Controversy remains
with regard to the treatment strategies for patients with
multivessel complex coronary artery disease (MCCAD), particularly
in recent years. Since the one-step implantation of multi-stents
has been charged and limited, it remains inconclusive whether
patients with MCCAD should undergo single complete
revascularization (CR), fractionated revascularization (FR) or
partial revascularization (PR). The present retrospective study
compared the effects of the various revascularization modes
(complete, fractionated or partial) with regard to the long-term
prognosis of patients with MCCAD. Similarities and differences in
the medical costs were compared with the aim of screening the
optimal treatment program for patients with MCCAD.
Materials and methods
Study population
A total of 2,309 patients with CAD that had been
admitted to the Department of Cardiology at the Provincial Hospital
Affiliated to Shandong University (Jinan, China) between December
2003 and October 2009 were selected for the study. The patients
were aged between 41 and 78 years with a mean age of 59±10 years.
Patients were divided into the CR (1,020 cases), FR (856 cases) and
PR groups (433 cases). The three groups all underwent selective
coronary angiography and percutaneous coronary intervention (PCI)
surgery due to the severe coronary artery stenosis; each patient
was implanted with at least one stent. Exclusion criteria included
acute ST-segment elevation-induced myocardial infarction, valvular
heart disease accompanied with heart failure and congenital heart
disease accompanied with clearly diagnosed cancer. In addition, if
the patient or their families refused the stent implantation, or
were unable to be followed-up for various reasons, these patients
were excluded from the study. Written informed consent was obtained
from the patient’s family.
Assessment of coronary angiography and
stent implantation
Surgical procedures were performed strictly in
accordance with the American Heart Association/American Heart
Association Coronary Angiography Guidelines. A Philips
cardiovascular imaging machine (Koninklijke Philips N.V.,
Amsterdam, Netherlands) and Siemens cardiovascular imaging machine
(Siemens AG, Munich, Germany) were used for selective coronary
angiography via puncture of the right femoral artery or right
radial artery. The surgical procedures were conducted strictly in
accordance with the standard interventional procedures (4). CAD diagnosis was determined based on
the results of the coronary angiography, namely, ≥50% stenosis of
at least one major coronary artery. MCCAD included unprotected left
main coronary artery disease, multivessel disease (MVD), chronic
total occlusion disease (CTO), diffuse long lesion and bifurcated
disease, among which MVD was defined as at least two main branches
of the epicardial coronary artery or the major branches with ≥50%
stenotic lesions (5). Diffuse long
lesion was defined as a lesion with >20 mm single length. CTO
was diagnosed if the coronary artery was completely occlusive and
lasted for more than three months. Successful intracoronary
stenting criteria were as follows: <20% post-stenting residual
stenosis of the target vessel lumen and Thrombolysis In Myocardial
Infarction Grade Flow III. CR referred to <50% post-PCI residual
stenosis of all the major coronary arteries and their branches
(6), while ≥50% residual stenosis
of any coronary artery and its branches was defined as PR. FR
referred to the achievement of CR of the target coronary vessel via
a FR procedure.
Drug therapy
All patients underwent preoperative drug therapy
with aspirin (100 mg/day) and clopidogrel (75 mg/day). Clopidogrel
(300–600 mg loading dose) was administered one day prior to surgery
to all patients excluding those who had obtained long-term
antiplatelet therapy outside the Provincial Hospital Affiliated to
Shandong University. Postoperative clopidogrel (75 mg/day) was
administered for at least one year and long-term administration of
aspirin (100 mg/day) and blood fat-regulating drugs, including
statin-category drugs, was recommended.
Follow-up and end-point
determination
The follow-up time was 36 months maximum and was
conducted via regular clinics, telephone contact or recoronary
angiography. The occurrence of angina pectoris and major adverse
cardiac events was recorded, including nonfatal myocardial
infarction, heart failure and mortality (cardiac or non-cardiac),
rehospitalization due to the aforementioned reasons and
revascularization by coronary artery bypass grafting or recoronary
artery stenting. End-point determination primarily relied on
inquiring with the patients or their families, consulting the
medical admission doctors, evaluating medical records and
associated auxiliary examinations and laboratorially examining the
indexes. The primary end point was all-cause mortality within three
years, while secondary end points were complex end-point events,
including nonfatal myocardial infarction, heart failure,
rehospitalization due to the aforementioned reasons and
revascularization (coronary artery bypass grafting and recoronary
artery stenting). All-cause mortality included cardiac and
non-cardiac mortality. Myocardial infarction included ST-segment
elevation-induced and non-ST-segment elevation-induced myocardial
infarction and was defined as an increase or decrease in the levels
of cardiac biomarkers (preferably cardiac troponin) by >99% of
the upper reference limit of 0.09 ng/ml. It was also accompanied by
at least one of the following symptoms of myocardial ischemia:
Ischemic symptoms, electrocardiography (ECG)-prompted new ischemic
changes, ECG-prompted pathological Q wave or radiographic evidence
indicating new regional wall motion abnormalities or the loss of
viable myocardium. Revascularization was vascularization performed
more than three months after the first vascularization, including
target and non-target vessel-revascularization.
Statistical methods
SPSS 13.0 software (SPSS, Inc., Chicago, IL, USA)
was used for statistical analysis. Measurement data are expressed
as the mean ± SD and were analyzed with the t-test. The
χ2 test was used to analyze the counting data. Logistic
regression multivariate correlation analysis was also performed and
P<0.05 was considered to indicate a statistically significant
difference. The survival curves were estimated with
Kaplan-Meier.
Results
Comparison of clinical features
No significant differences were identified with
regard to the gender ratio, hypertension, hypercholesterolemia and
smoking habits among the three groups (P>0.05). However, the
average age, prevalence of diabetes and incidence of remote
myocardial infarction and left ventricular dysfunction in the PR
and FR groups were higher than those in the CR group and the
differences were statistically significant (P<0.05; Table I).
 | Table IComparison of the clinical data of
among three groups. |
Table I
Comparison of the clinical data of
among three groups.
| Group | Cases, n | Age, years | Males, n (%) | Smoker, n (%) | Hypertension, n
(%) | Hypercholesterolemia,
n (%) | Diabetes, n (%) | CAD family history, n
(%) | Left ventricle
ejection ratio, % | Remote myocardial
infarction, n (%) | Unstable angina, n
(%) |
|---|
| CR | 1020 | 58±10 | 753 (73.8) | 247 (24.2) | 676 (66.3) | 623 (61.1) | 268 (26.3) | 196 (19.3) | 64±11 | 180 (17.6) | 744 (73.0) |
| FR | 856 | 61±9 | 615 (71.9) | 158 (18.5) | 525 (61.3) | 504 (58.9) | 320 (37.4) | 218 (25.5) | 53±10 | 218 (25.5) | 590 (68.9) |
| PR | 433 | 62±9 | 304 (70.4) | 84 (19.4) | 275 (63.5) | 252 (58.2) | 174 (40.2) | 105 (24.2) | 52±11 | 125 (28.9) | 294 (67.9) |
Comparison of CAD, stent implantation and
medical costs
Compared with the CR group, the mean number of
lesions, average lesion stenosis and the number of patients with
severe stenosis, complex lesions, three-branch lesions, left main
stem disease, bifurcated lesions and CTO in the PR and FR groups
were significantly higher (P<0.05), while the average number of
stents was significantly lower (P<0.05). No significant
differences were observed in the proportion of long lesions and the
average length of the stents among the groups (P>0.05; Table II).
 | Table IIComparison of coronary lesions,
stenting indicators and medical costs. |
Table II
Comparison of coronary lesions,
stenting indicators and medical costs.
| Group | Cases, n | Lesions, n | Average lesion
stenosis, % | Severe stenosis
lesion, n (%) | Complex lesion, n
(%) | Three-branch lesion,
n (%) | Left main stem
lesion, n (%) | Bifurcated lesion, n
(%) | CTO, n (%) | Long lesion, n
(%) | Stents, n | Stent length, mm |
|---|
| CR | 1020 | 2.6±0.9 | 75±11 | 432 (42.4) | 655 (64.2) | 295 (28.9) | 25 (2.5) | 153 (15.0) | 105 (10.3) | 236 (23.1) | 2.5±1.5 | 18.8±5.6 |
| FR | 856 | 3.3±1.2 | 84±10 | 443 (51.8) | 681 (79.5) | 456 (53.2) | 77 (8.9) | 188 (21.9) | 205 (23.9) | 188 (21.9) | 1.4±0.8 | 19.1±6.2 |
| PR | 433 | 3.4±1.2 | 85±10 | 226 (52.2) | 344 (79.4) | 235 (54.2) | 42 (9.7) | 95 (21.9) | 108 (24.9) | 103 (23.8) | 1.9±0.9 | 18.9±5.7 |
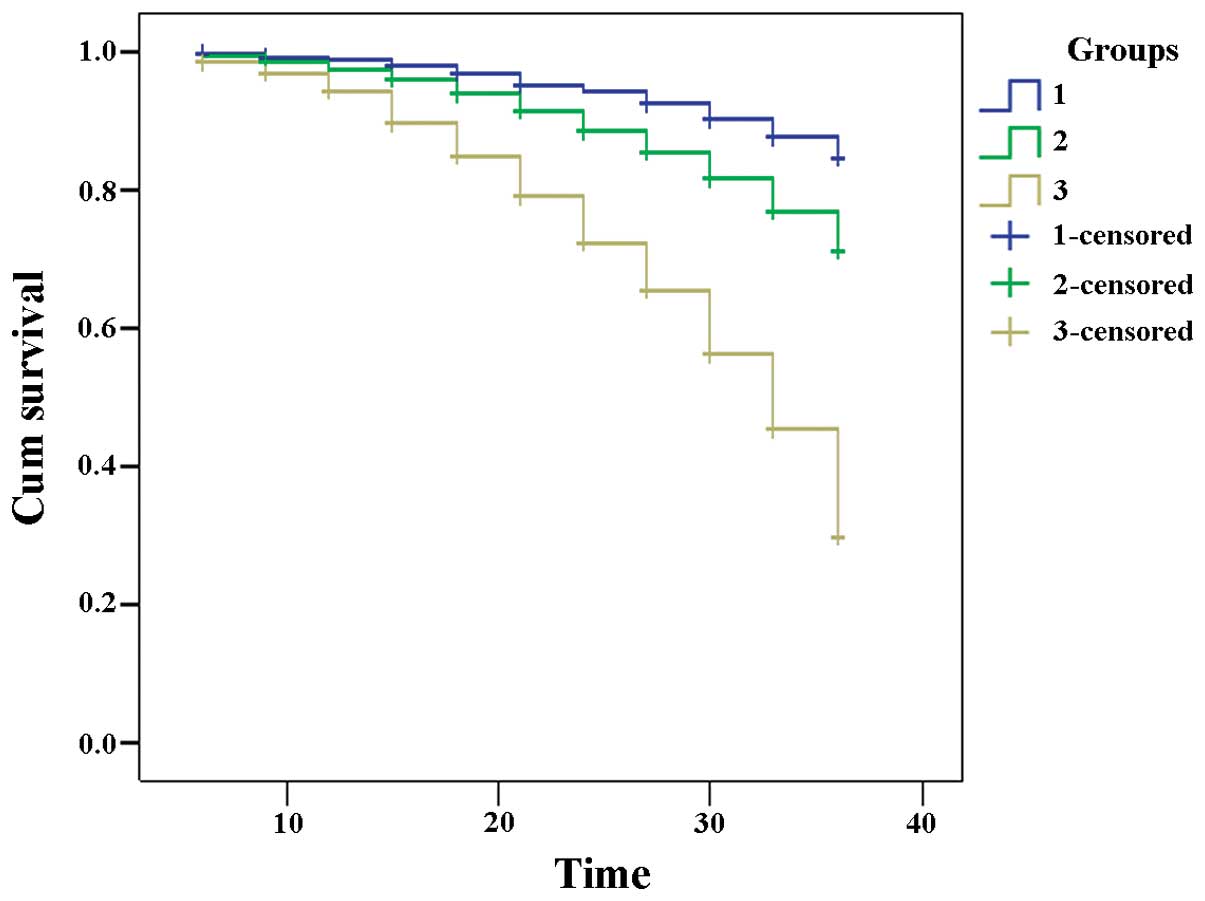
Comparison of follow-up observations
The follow-up period was 36 months. During the
follow-up period, no significant difference was observed in the
in-stent restenosis rate among the three groups (P>0.05), while
statistically significant differences were identified in the number
of cases of recurrent angina, myocardial infarction, heart failure,
revascularization and all-cause mortality among the three groups
(P<0.05; Table III). The
incidence of major adverse cardiac events during the three-year
follow-up period in the CR group (17%) was significantly lower than
that in the FR (29%; P<0.01) and PR groups (67%; P<0.001). In
addition, the three-year survival rate in the CR group was
significantly longer than the rates in the FR and PR groups and the
difference among the survival times was statistically significant
(P<0.001; Table IV; Fig. 1). The three-year medical costs in
the CR group (62,100 RMB) were significantly lower than those in
the FR (83,200 RMB; P<0.001) and PR groups (66,900 RMB;
P<0.01).
 | Table IIIComparison of follow-up results. |
Table III
Comparison of follow-up results.
| Group | Cases, n | In-stent restenosis,
n (%) | Angina, n (%) | Myocardial
infarction, n (%) | Heart failure, n
(%) | Revascularization
(unchanged number), n (%) | All-cause mortality,
n (%) | MACE events, n
(%) | Medical costs,
RMB |
|---|
| CR | 1020 | 121 (11.9) | 307 (30.1) | 18 (1.7) | 67 (6.5) | 142 (13.9) | 12 (1.2) | 173 (17) | 62,100 |
| FR | 856 | 111 (12.9) | 246 (28.7) | 19 (2.2) | 84 (9.8) | 111 (12.9) | 15 (1.8) | 248 (29) | 83,200 |
| PR | 433 | 63 (14.6) | 191 (44.1) | 12 (2.8) | 93 (21.4) | 98 (22.8) | 17 (3.9) | 290 (67) | 66,900 |
 | Table IVStatistical comparison of the survival
times among the three groups. |
Table IV
Statistical comparison of the survival
times among the three groups.
| Group | Mean survival time
(months) | RSD |
|---|
| CR | 34.544 | 0.144 |
| FR | 33.255 | 0.212 |
| PR | 29.449 | 0.397 |
| Overall | 33.153 | 0.130 |
Analysis of the survival rates
Survival times of the three groups were
statistically compared (χ2 = 487.968; P<0.001) and
statistically significant differences were observed. The survival
rate is the highest in CR, and the lowest in partial
revascularization, and the middle is FR.
Discussion
The incidence of CAD has gradually increased and the
age of onset has become increasingly younger. MCCAD is one of the
most serious types of CAD that commonly leads to complications,
including heart enlargement, heart failure, malignant arrhythmias
and cardiac sudden death, which seriously impacts the quality of
life and life expectancy of a patient. The treatment principles of
CAD include drug therapy, reperfusion therapy and heart
transplantation. Drug therapy is the basis in the treatment of CAD.
Based on positive drug intervention, therapy which is able to
timely open the coronary blood vessels and ensure continuous and
effective levels of myocardial reperfusion may significantly reduce
the myocardial ischemic area, rescue heart function, reduce
mortality and complications and improve the prognosis of patients.
PCI treatment has become the most important method of myocardial
revascularization. Patients with MCCAD constitute the high-risk
population for serious cardiovascular events and target vessel
revascularization. Myocardial blood supply should be actively
improved, preventing left ventricular remodeling, protecting the
function of the heart, reducing major cardiac events, including
arrhythmia, heart failure and sudden mortality, and CR should be
achieved to the greatest extent possible. Controversy remains with
regard to achieving CR in patients with MCCAD (7,8). The
risks of postoperative elevated serum creatine kinase levels,
contrast-induced nephropathy and thrombosis are likely to increase
in MCCAD patients, compared with other patients (9–11).
An American three-year follow-up study involving >20,000
individuals identified that the risk of mortality following PR was
significantly increased when compared with CR (12). The majority of foreign studies have
demonstrated that for patients with MCCAD, regardless of the
surgical bypass or medical intervention therapy administered,
achieving CR to the greatest possible extent significantly improves
prognosis (13,14). As for MCCAD patients undergoing a
coronary artery bypass graft, CR was the most successful vascular
reopen strategy (15–18). In the present study, retrospective
analysis was performed to compare the prognoses of three treatment
groups. The results revealed that throughout the follow-up period,
the rates of recurrent angina, nonfatal myocardial infarction,
heart failure, rehospitalization due to the aforementioned reasons
and revascularization (coronary artery bypass grafting and coronary
stent reimplantation) in the PR group were statistically
significantly higher than those in the CR group, indicating that
the short and long-term prognoses of CR were better compared with
those of PR. These results are consistent with the conclusions of
the majority of foreign studies (19–21).
The three-year medical costs of the CR group were significantly
lower than those of the PR and FR groups. The complexity of CAD,
degree of stenosis, previous history of revascularization and cases
of remote myocardial infarction in the PR group were higher
compared with those in the CR group (P<0.05). These observations
indicated that the heart conditions of the PR patients were worse
than those of the CR patients, the risk factors were increased, the
left ventricular ejection fraction was reduced and CR was unable to
be achieved due to the disease condition and technical reasons.
With the current improvements to PCI surgical technology, an
increasing number of patients with MCCAD may achieve CR. Therefore,
the difficulty of performing PCI in PR patients is markedly higher
than in CR patients, which may also be one of the factors causing
the difference in the long-term prognoses. Furthermore, during PCI,
the present study identified that CR was difficult to achieve in
certain coronary arteries due to the following reasons: Diffuse
vascular disease, vascular calcification, distal lesions or small
branch lesions; CTO lesions with long history while the guiding
wire, balloon or stent could not pass; the vessels were seriously
distorted or calcified so that the guiding wire, balloon or stent
could not pass, or the stent expansion was poor, and was not able
to adhere to the walls; and partial left main lesions. Tolerance to
the surgery and economic conditions of the patient were also
factors resulting in a PR outcome. In clinical practice, each case
should be carefully analyzed, the appropriate surgical instruments
selected, the surgical techniques and methods improved and the
positive and negative points fully balanced, thereby improving the
success rate of complex-lesion PCI surgery and reducing
complications. In conclusion, the present study demonstrated that
the long-term prognosis of CR implementation through PCI for
patients with MCCAD was better compared with that of PR.
References
|
1
|
Boden WE, O’Rourke RA, Teo KK, et al;
COURAGE Trial Research Group. Optimal medical therapy with or
without PCI for stable coronary disease. N Engl J Med.
356:1503–1516. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ndrepepa G, Mehilli J, Schulz S, et al:
Prognostic significance of epicardial blood flow before and after
percutaneous coronary intervention in patients with acute coronary
syndromes. J Am Coll Cardiol. 52:512–517. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sorajja P, Gersh BJ, Cox DA, et al: Impact
of multivessel disease on reperfusion success and clinical outcomes
in patients undergoing primary percutaneous coronary intervention
for acute myocardial infarction. Eur Heart J. 28:1709–1716. 2007.
View Article : Google Scholar
|
|
4
|
Yang JH, Gwon HC, Cho SJ, et al:
Comparison of coronary artery bypass grafting with drug-eluting
stent implantation for the treatment of multivessel coronary artery
disease. Ann Thorac Surg. 85:65–70. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Shishehbor MH, Lauer MS, Singh IM, et al:
In unstable angina or non-ST-segment acute coronary syndrome,
should patients with multivessel coronary artery disease undergo
multivessel or culprit-only stenting? J Am Coll Cardiol.
49:849–854. 2007. View Article : Google Scholar
|
|
6
|
Hannan EL, Racz M, Holmes DR, et al:
Impact of completeness of percutaneous coronary intervention
revascularization on long-term outcomes in the stent era.
Circulation. 113:2406–2412. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ijsselmuiden AJ, Ezechiels J, Westendorp
IC, et al: Complete versus culprit vessel percutaneous coronary
intervention in multivessel disease: a randomized comparison. Am
Heart J. 148:467–474. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hannan EL, Racz M, Holmes DR, et al:
Impact of completeness of percutaneous coronary intervention
revascularization on long-term outcomes in the stent era.
Circulation. 113:2406–2412. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chu WW, Kuchulakanti PK, Rha SW, et al:
Impact of three or more versus a single sirolimus-eluting stent on
outcomes in patients who undergo percutaneous coronary
intervention. Am J Cardiol. 97:606–610. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Di Mario C, Mara S, Flavio A, et al:
Single vs. multivessel treatment during primary angioplasty:
results of the multicentre randomised HEpacoat for cuLPrit or
multivessel stenting for Acute Myocardial Infarction (HELP AMI)
Study. Int J Cardiovasc Intervent. 6:128–133. 2004.
|
|
11
|
Zahn R, Hamm CW, Schneider S, et al;
German Cypher Stent Registry. Incidence and predictors of target
vessel revascularization and clinical event rates of the
sirolimus-eluting coronary stent (results from the prospective
multicenter German Cypher Stent Registry). Am J Cardiol.
95:1302–1308. 2005. View Article : Google Scholar
|
|
12
|
Hannan EL, Racz M, Holmes DR, et al:
Impact of completeness of percutaneous coronary intervention
revascularization on long-term outcomes in the stent era.
Circulation. 113:2406–2412. 2006. View Article : Google Scholar
|
|
13
|
Dzavik V, Ghali WA, Norris C, et al;
Alberta Provincial Project for Outcome Assessment in Coronary Heart
Disease (APPROACH) Investigators. Long-term survival in 11,661
patients with multivessel coronary artery disease in the era of
stenting: a report from the Alberta Provincial Project for Outcome
Assessment in Coronary Heart Disease (APPROACH) Investigators. Am
Heart J. 142:119–126. 2001. View Article : Google Scholar
|
|
14
|
Favarato ME, Hueb W, Boden WE, et al:
Quality of life in patients with symptomatic multivessel coronary
artery disease: a comparative post hoc analyses of medical,
angioplasty or surgical strategies-MASS II trial. Int J Cardiol.
116:364–370. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cosgrove DM, Loop FD, Lytle BW, et al:
Determinants of 10-year survival after primary myocardial
revascularization. Ann Surg. 202:480–490. 1985.PubMed/NCBI
|
|
16
|
Bell MR, Gersh BJ, Schaff HV, et al:
Effect of completeness of revascularization on long-term outcome of
patients with three-vessel disease undergoing coronary artery
bypass surgery. A report from the Coronary Artery Surgery Study
(CASS) Registry. Circulation. 86:446–457. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Buda AJ, Macdonald IL, Anderson MJ, et al:
Long-term results following coronary bypass operation. Importance
of preoperative factors and complete revascularization. J Thorac
Cardiovasc Surg. 82:383–390. 1981.PubMed/NCBI
|
|
18
|
Jones EL, Craver JM, Guyton RA, et al:
Importance of complete revascularization in performance of the
coronary bypass operation. Am J Cardiol. 51:7–12. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hannan EL, Racz M, Holmes DR, et al:
Impact of completeness of percutaneous coronary intervention
revascularization on long-term outcomes in the stent era.
Circulation. 113:2406–2412. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kip KE, Bourassa MG, Jacobs AK, et al:
Influence of pre-PTCA strategy and initial PTCA result in patients
with multivessel disease: the Bypass Angioplasty Revascularization
Investigation (BARI). Circulation. 100:910–917. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
van den Brand MJ, Rensing BJ, Morel MA, et
al: The effect of completeness of revascularization on event-free
survival at one year in the ARTS trial. J Am Coll Cardiol.
39:559–564. 2002.PubMed/NCBI
|