Introduction
Anaplastic lymphoma kinase (ALK)-positive diffuse
large B-cell lymphoma (ALK+ DLBCL) is a rare novel
subtype of DLBCL that was recognized as a separate entity in the
2008 World Health Organization (WHO) classification of lymphoid
neoplasms (1). Since it was first
described in 1997 (2), to the best
of our knowledge, ~60 cases have been reported to date.
Morphologically, the lymphoma is composed of immunoblastic or
plasmablastic cells and exhibits a sinusoidal growth pattern.
Immunohistochemical staining of the tumor cells reveals a distinct
profile, including a lack of B-lineage (CD20 and CD79α) and
T-lineage (CD3) markers and CD30, but the expression of CD138 and
CD38 (plasmacytic markers), variable expression levels of CD4 and
CD57, and single light-chain cytoplasmic immunoglobulin A (IgA).
Notably, a previous study demonstrated that lymphoma cells were
strongly positive for ALK in a cytoplasmic granular staining
pattern, which was different to the cytoplasmic and/or nuclear
pattern characteristics of the T/null anaplastic large cell
lymphoma (ALCL) (3).
Initially, an ALK gene rearrangement was not
detected in ALK+ DLBCL and the full-length ALK protein
was considered to be the pathogenesis of the lymphoma (2). However in 2003, Gascoyne et al
(4) and De Paepe et al
(5) described six and three cases,
respectively, of ALK+ DLBCL. They were characterized by
t(2;17)(p23;q23), which results in the fusion of the ALK gene at
chromosome band 2p23 and the clathrin gene (CLTC) at 17q2.
Subsequent studies revealed chromosome translocation at
t(2;5)(p23;q35), which was frequently associated with ALCL, and a
cryptic insertion of the ALK gene into chromosome 4 at band 4q22-24
fusion in certain cases of ALK+ DLBCL (6–8).
Although extranodal sites, including the nasopharynx
and stomach, may be involved (7,9,10),
it is the lymph nodes that are consistently primarily involved in
cases of ALK+ DLBCL. The present study reports, to the
best of our knowledge, the first case of primary extranodal
ALK+ DLBCL presenting as a duodenal mass.
Case report
Case summary
A 26-year-old male presented with a principal
complaint of abdominal distension and vomiting for almost three
weeks. Computed tomography (CT) scans revealed an irregular mass in
the lower part of the duodenum, abdominal and retroperitoneal
lymphadenopathy, and multiple low-density foci in the spleen.
However, there was no evidence of disease elsewhere. The endoscopic
biopsy was reported as lymphoma, although a definitive diagnosis
was not reached. A subsequent palliative pancreaticoduodenectomy
was performed.
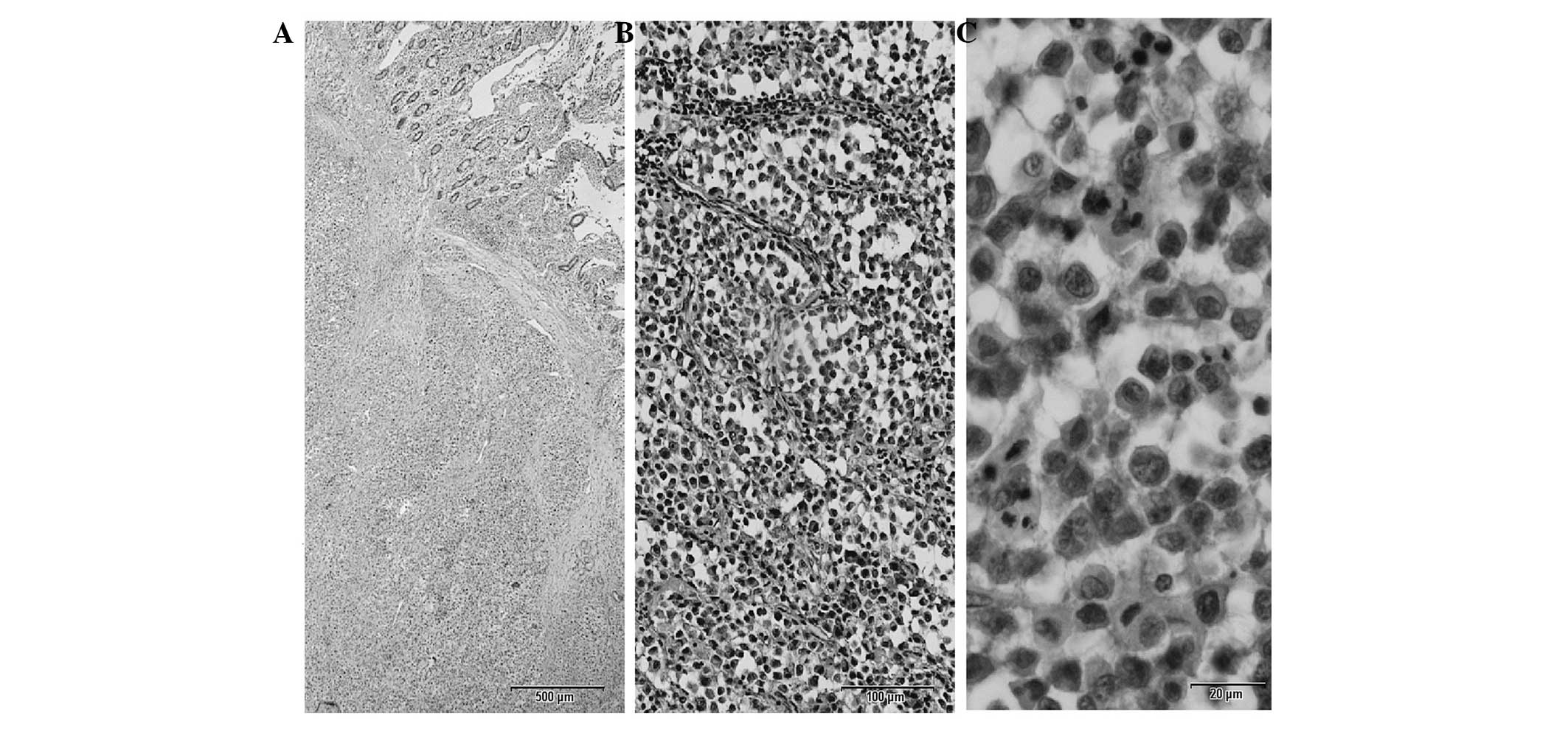
Histological examination of the tumor revealed a
diffuse infiltration of tumor cells from the mucosa to the serosa.
The neoplastic cells were large, with centrally or eccentrically
located round nuclei, prominent single nucleoli and moderately
eosinophilic cytoplasm (Fig. 1).
Regional lymph nodes were also invaded. Bone marrow biopsy revealed
no evidence of infiltrations by the lymphoma. The patient was
assessed as being at stage IIa according to the Ann Arbor staging
system.
Eight cycles of cyclophosphamide, doxorubicin,
vincristine, prednisone and etoposide (CHOPE) were administered to
the patient over nine months. The patient responded to the therapy
and the disease was partially regressed, although without the
achievement of tumor-free status.
The use of human tissue samples for this study was
approved by the Institutional Review Board of the Affiliated
Hospital of Qingdao University Medical College (Qingdao, China).
The patient provided written informed consent for their
participation in the study.
Immunohistochemistry
Immunohistochemical staining was performed on
paraffin-embedded tissue sections (5 μm) with the EnVision method.
The analyses were conducted with a large panel of monoclonal
antibodies, including antibodies against CD20, CD79α (both from
ZSGB-BIO, Beijng, China), CD3 (BD Biosciences, Heidelberg,
Germany), CD138, CD38, CD56, epithelial membrane antigen (EMA),
AE1/AE3, CD30, multiple myeloma oncogene 1 (Mum-1), CD10 (all from
ZSGB-BIO), B-cell lymphoma 6 (Bcl-6; BD Biosciences),
immunoglobulin A (IgA; DAKO, Glostrup, Denmark) and Ki67
(ZSGB-BIO), following antigen retrieval. For detection of the ALK
(BD Biosciences) protein, the monoclonal antibody anti-ALK was
used.
In situ hybridization
In situ hybridization was performed,
according to standard methods (11), on 4-μm paraffin-embedded tissue
sections with specific digoxigenin-labeled probes (ZSGB-BIO) that
were complementary to Epstein-Barr virus (EBV)-encoded RNA nuclear
transcripts.
Fluorescence in situ hybridization
(FISH)
FISH was performed on 4 μm paraffin-embedded tissue
sections following deparaffinization and digestion. The slides were
washed in saline-sodium citrate (SSC) buffer, fixed in 10%-buffered
formalin for 5 min, dehydrated in graded alcohol and allowed to air
dry. Hybridization was performed using a dual-color break-apart
rearrangement probe (ZSGB-BIO) for the ALK gene on chromosome 2.
The probes were denatured by incubation at 78°C for 5 min in a
humidified box, after which they were hybridized overnight at
42°C.
Immunohistochemistry and in situ
hybridization results
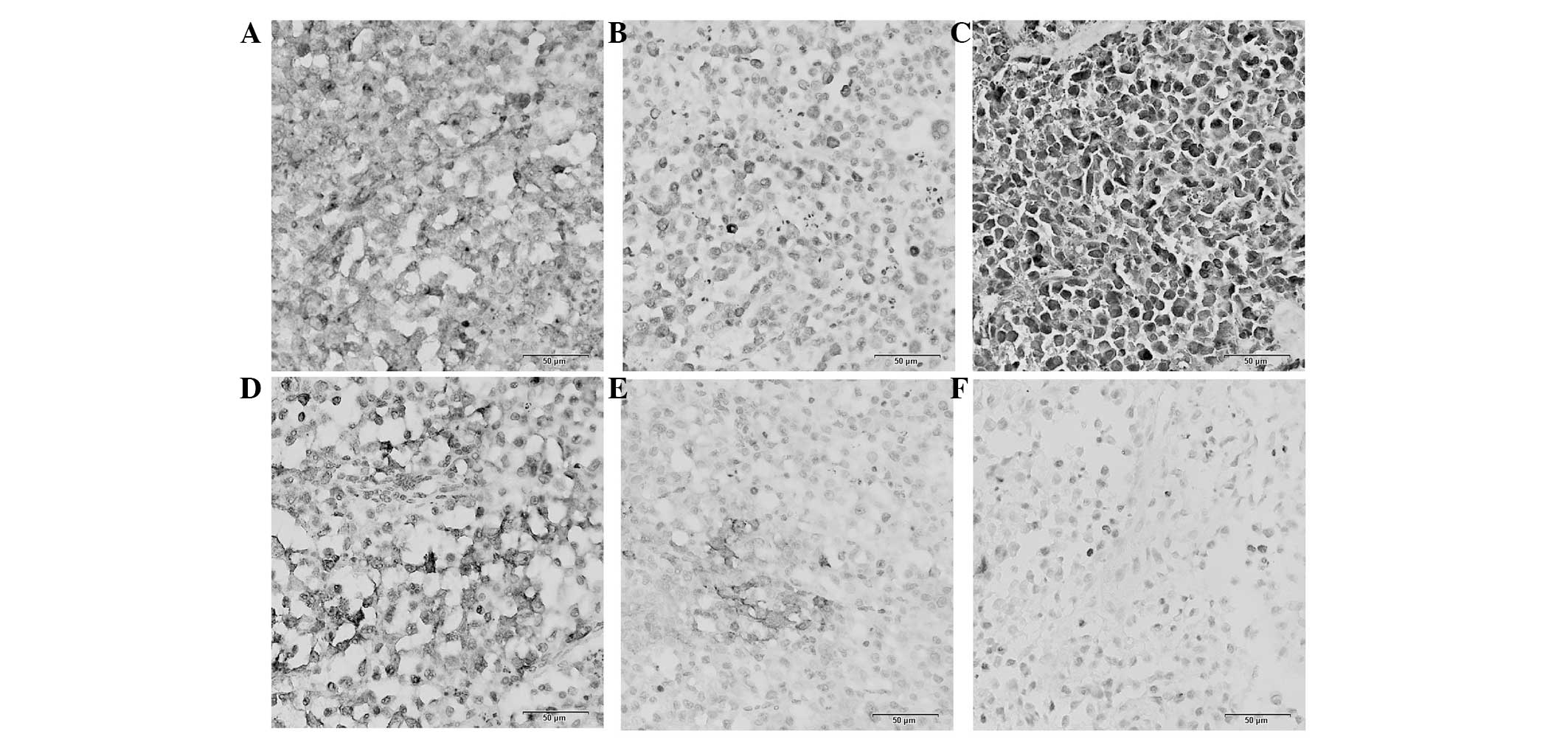
Immunohistochemistry demonstrated that the tumor
cells were positive for CD138, IgA and CD79α (Fig. 2), but negative for CD3, CD38, CD20,
CD10, Bcl-6, CD56 and cytokeratin. Mum-1, CD30 and EMA revealed a
patchy reactivity (Fig. 2).
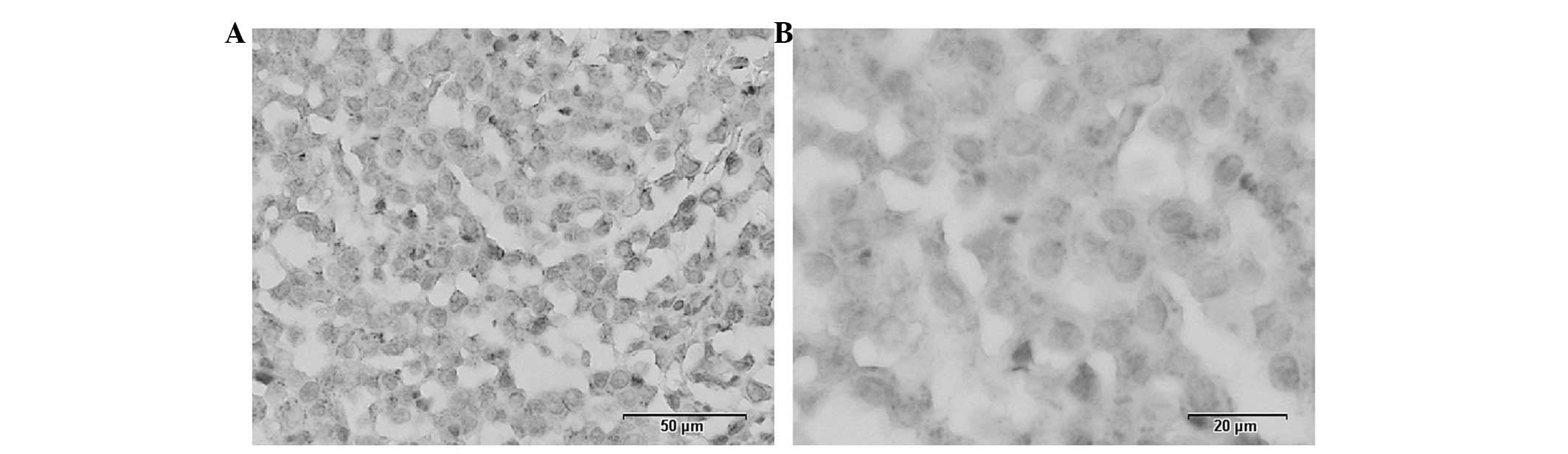
Furthermore, immunohistochemistry with the monoclonal antibody
anti-ALK1, revealed a granular cytoplasmic expression of the ALK
protein by neoplastic cells (Fig.
3). The EBV in situ hybridization staining was
negative.
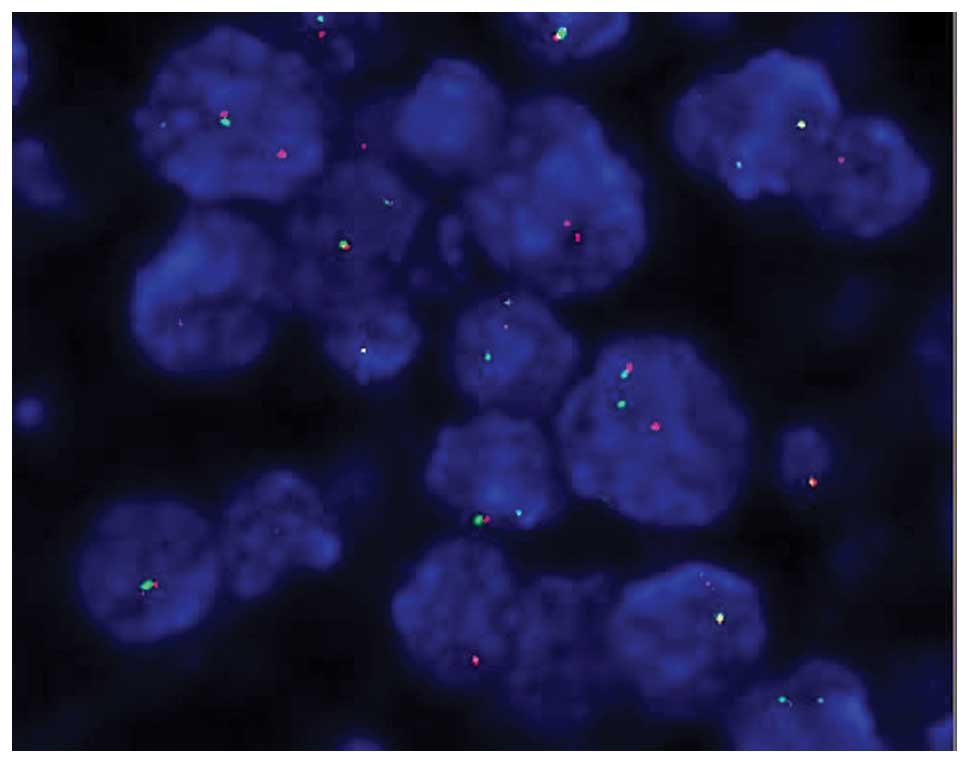
FISH results indicate ALK gene
rearrangements
FISH analysis demonstrated that gene rearrangement
of ALK were present in the patient. Fig. 4 shows clearly separated green and
red signals indicating the translocation of the ALK gene. The
normal ALK gene signal is shown as a fused yellow signal or joined
green and red signals.
Discussion
ALK+ DLBCL was originally described by
Delsol et al (2) in 1997,
based on a series of seven cases. It spans all age groups (9–72
years), with a median of 38 years, and occurs with a male
predominance (male:female ratio, 3:1). ALK+ DLBCL
frequently presents with an aggressive clinical course, a poor
response to therapy and a short survival time (12). Histologically, the tumor cells
exhibit an immunoblastic and/or plasmablastic morphology with a
sinusoidal growth pattern. Immunohistochemically, ALK+
DLBCL does not express B-lineage markers (CD20 and CD79α),
T-lineage markers (CD3), cytotoxic granular proteins (granzyme B
and TIA-1) or CD30. However, plasmacytic markers, including CD138,
CD38 and EMA, are characteristically expressed, which demonstrates
the terminally differentiated B-lineage origin of the tumor cells
(13). In the majority of reported
cases of ALK+ DLBCL, monotypic IgA λ was expressed, and
EBV was not detected by in situ hybridization (3,5,6,9,10,13,14).
In concordance with the results of these studies, the present case
tested positive for the expression of CD138 and IgA.
Although a unique immunophenotypic profile has been
established for ALK+ DLBCL, there remains a certain
immunophenotypic heterogeneity. For example, CD79α is not usually
expressed in tumor cells; however, in certain cases, including the
case reported in the present study, the tumor cells were positive
for CD79α (10,14). Similarly, although usually
negative, the current case and one case described in the study by
De Paepe et al (5) were
focally positive for CD30.
Lymph nodes are consistently primarily involved in
ALK+ DLBCL; however, cases of extranodal involvement,
including in the stomach, nasal cavity, ovary and brain, have been
described (7,9,10,14).
While the gastrointestinal tract (GI) is the most common site of
extranodal lymphoma, only one case of an extranodal lymphoma in the
stomach has been reported, which was in the study by McManus et
al (9). The study described a
gastric ALK+ DLBCL without the involvement of bone
marrow or adjacent organs in a patient aged 21 years (9). To the best of our knowledge, the
current study describes the first case of ALK+ DLBCL in
the duodenum, which represents the second reported occurrence of
ALK+ DLBCL in the GI tract.
ALK+ DLBCL exhibits a distinct staining
pattern for the ALK protein according to the underlying gene
rearrangement. The majority of reported cases with clathrin
heavy-chain (CLTC)-ALK gene translocation exhibit granular
cytoplasmic staining (2,3,7,13,14),
while a number of cases with nucleophosmin (NPM1)-ALK translocation
exhibit cytoplasmic and nuclear staining (6,7).
Furthermore, certain other staining patterns have been observed.
Lee et al (13) observed a
case demonstrating a unique nuclear membrane-staining pattern for
the ALK protein, which indicated a novel ALK gene rearrangement
involving another translocation partner gene. A cryptic 3′-ALK gene
insertion into chromosome 4 was identified by Stachurski et
al (8), which represented a
novel cytogenetic alteration of ALK+ DLBCL. The current
case demonstrated a typical cytoplasmic and granular ALK staining
pattern and the corresponding rearrangement of the ALK gene.
Clinically, ALK+ DLBCL is more aggressive
and reveals a worse response rate to standard chemotherapy compared
with typical DLBCL. Laurent et al (14) reviewed a large cohort of 38 cases
of ALK+ DLBCL and observed that the majority of patients
experienced an aggressive clinical course, with a 5-year survival
rate of 25% following treatment with the CHOPE regimen. Since tests
for CD20 are negative in the majority of cases of ALK+
DLBCL, rituximab plays no therapeutic role. Therefore, it is
important to develop novel and effective alternative treatments for
ALK+ DLBCL, including front-line intensification with or
without autologous stem-cell transplantation, and the application
of new biological agents such as anti-CD138 monoclonal antibodies
and ALK inhibitors (14,15).
References
|
1
|
Delsol G, Campo E and Gascoyne RD:
ALK-positive large B-cell lymphoma. WHO Classification of Tumours
of Haematopoietic and Lymphoid Tissues. Swerdlow S, Campo E, Harris
N, et al: Lyon: International Agency for Research on Cancer; pp.
254–255. 2008
|
|
2
|
Delsol G, Lamant L, Mariamé B, et al: A
new subtype of large B-cell lymphoma expressing the ALK kinase and
lacking the 2;5 translocation. Blood. 89:1483–1490. 1997.PubMed/NCBI
|
|
3
|
Morris SW, Kirstein MN, Valentine MB,
Dittmer K, Shapiro DN, Look AT and Saltman DL: Fusion of a kinase
gene, ALK, to a nucleolar protein gene, NPM, in non-Hodgkin’s
lymphoma. Science. 267:316–317. 1995.
|
|
4
|
Gascoyne RD, Lamant L, Martin-Subero JI,
et al: ALK-positive diffuse large B-cell lymphoma is associated
with Clathrin-ALK rearrangements: report of 6 cases. Blood.
102:2568–2573. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
De Paepe P, Baens M, van Krieken H, et al:
ALK activation by the CLTC-ALK fusion is a recurrent event in large
B-cell lymphoma. Blood. 102:2638–2641. 2003.PubMed/NCBI
|
|
6
|
Adam P, Katzenberger T, Seeberger H, et
al: A case of a diffuse large B-cell lymphoma of plasmablastic type
associated with the t(2;5)(p23;q35) chromosome translocation. Am J
Surg Pathol. 27:1473–1476. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Onciu M, Behm FG, Downing JR, et al:
ALK-positive plasmablastic B-cell lymphoma with expression of the
NPM-ALK fusion transcript: report of 2 cases. Blood. 102:2642–2644.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Stachurski D, Miron PM, Al-Homsi S,
Hutchinson L, Harris NL, Woda B and Wang SA: Anaplastic lymphoma
kinase-positive diffuse large B-cell lymphoma with a complex
karyotype and cryptic 3’ ALK gene insertion to chromosome 4 q22-24.
Hum Pathol. 38:940–945. 2007.PubMed/NCBI
|
|
9
|
McManus DT, Catherwood MA, Carey PD,
Cuthbert RJ and Alexander HD: ALK-positive diffuse large B-cell
lymphoma of the stomach associated with a clathrin-ALK
rearrangement. Hum Pathol. 35:1285–1288. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Reichard KK, McKenna RW and Kroft SH:
ALK-positive diffuse large B-cell lymphoma: report of four cases
and review of the literature. Mod Pathol. 20:310–319. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Luo B, Wang Y, Wang XF, Liang H, Yan LP,
Huang BH and Zhao P: Expression of Epstein-Barr virus genes in
EBV-associated gastric carcinomas. World J Gastroenterol.
11:629–633. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Beltran B, Castillo J, Salas R, et al:
ALK-positive diffuse large B-cell lymphoma: report of four cases
and review of the literature. J Hematol Oncol. 2:112009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lee HW, Kim K, Kim W and Ko YH:
ALK-positive diffuse large B-cell lymphoma: report of three cases.
Hematol Oncol. 26:108–113. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Laurent C, Do C, Gascoyne RD, et al:
Anaplastic lymphoma kinase-positive diffuse large B-cell lymphoma:
a rare clinicopathologic entity with poor prognosis. J Clin Oncol.
27:4211–4216. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tassone P, Goldmacher VS, Neri P, et al:
Cytotoxic activity of the maytansinoid immunoconjugate B-B4-DM1
against CD138+ multiple myeloma cells. Blood. 104:3688–3696.
2004.PubMed/NCBI
|