Introduction
Ectopic pregnancy is the implantation of a
fertilized egg outside the uterine cavity (1). It is a complication of the first
trimester of pregnancy that arises in 1.3–2.4% of all pregnancies
(1). The most common site of ectopic
pregnancy is the fallopian tube (97% of ectopic pregnancies)
(2), and the second most common is
the ovary and broad ligament (3).
Ectopic pregnancy may also, although rarely, occur in the liver
(4), spleen (5), omentum (6), peritoneum (7), terminal ileum and colon (8).
Once an ectopic pregnancy ruptures, bleeding and
other serious complications such as shock and even death (9) often ensue. If the condition is not
diagnosed and treated in a timely manner, it can be
life-threatening. As a common gynecological emergency, ectopic
pregnancy is a focus of considerable attention by clinicians. The
diagnostic means for ectopic pregnancy include clinical
examination, imaging examination [for example, ultrasonography,
computed tomography (CT), magnetic resonance imaging (MRI)], blood
human chorionic gonadotropin (hCG) determination, blood
progesterone assay and diagnostic curettage, which are often
combined in clinical use (1,2).
The choices of treatment for ectopic pregnancy are
expectant treatment (close monitoring) (10), drug therapy (11) and surgery (1). Interventional treatment is another
alternative for ectopic uterine and extra-uterine pregnancies,
although non-tubal ectopic pregnancy, particularly that which is
cervical, abdominal, ovarian or in a cesarean scar, represents a
major clinical challenge (12).
The present case report describes the case of a
31-year-old women with an ectopic pregnancy in the liver and her
US, CT and positron emission tomography (PET)-CT imaging results,
from which a timely diagnosis of ectopic pregnancy was made. The
study participant provided informed written consent prior to the
study. The study was reviewed and approved by the Institutional
Review Board of Second Xiangya Hospital, Central South University
(Changsha, China).
Case report
A 31-year-old woman was admitted to the Second
Xiangya Hospital, Central South University in December 2015 with
the complaint of amenorrhea for 40 days, abdominal distention for
27 days. She was admitted to a local hospital 6 days earlier and a
CT scan found a liver mass.
The patient had experienced one cesarean delivery in
2008, and had undergone curettage because of embryo damage in 2009,
where histopathological analysis revealed denatured villus tissue
and decidual tissue. A contraceptive ring had been in place in the
uterine cavity for 6 years.
The patient's blood pressure was 117/68 mmHg and her
heart rate was 93 beats/min. In addition, the hemoglobin
concentration was 109 g/l (normal level >120 g/l) and the serum
hCG level was 49,198 U/l (normally level <2.7 mlU/ml) (13). Gynecological examination revealed no
evident abnormalities.
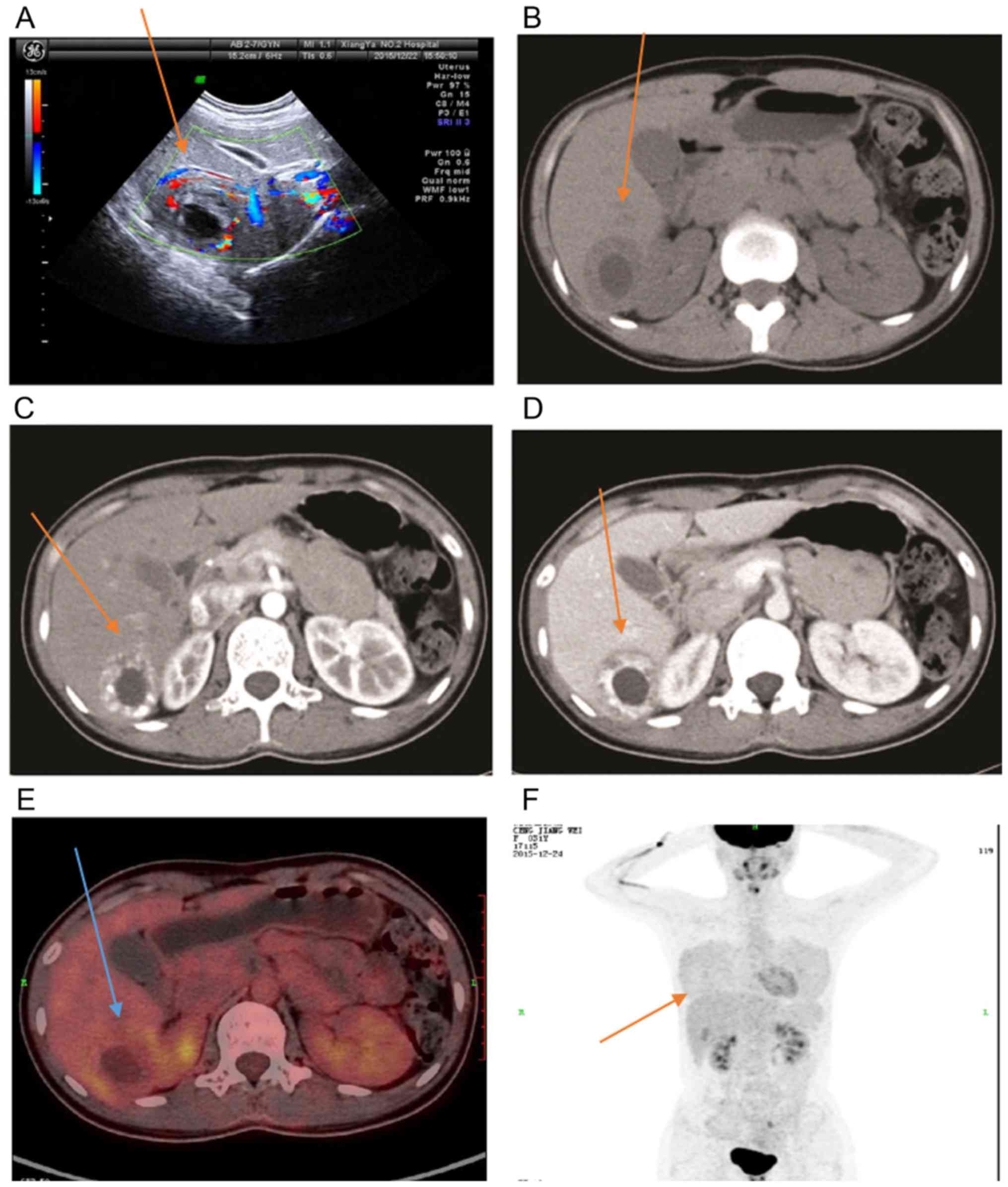
An ultrasound (US) examination of the abdomen
revealed no obvious gestational sac in the uterine cavity, but
detected a 5.4×4.6-cm hyperechoic mass in the right hepatic lobe
and a fluid sonolucent area of 2.7×2.1 cm within the mass. The
cystic sonolucent area within the fluid sonolucent area (Fig. 1A) was suggestive of an ectopic
pregnancy. The intrauterine contraceptive ring was observed to be
in a normal position.
CT scanning revealed a mass in the right hepatic
lobe with a slightly low-density peripheral portion and oval
lower-density central portion (Fig.
1B) in the plain scan, a peripheral portion with a
significantly increased density in the arterial phase of the
enhanced scan (Fig. 1C), a
peripheral portion with a slightly increased density compared with
that of the liver parenchyma in the venous phase of the enhanced
scan (Fig. 1D), and a non-enhanced
lower-density central portion in the enhanced scan.
18F-FDG PET-CT revealed a mass in the
right hepatic lobe with envelope of 4.2×4.8 cm and a cystic
hypo-dense lesion of 1.9×2.7 cm within it. The intake of FDG was
not increased in the cystic areas but that in the residual portion
was increased; the maximum standard uptake value (SUVmax) was 5.7
(Fig. 1E and F).
After 3 days of preoperative preparation,
hysteroscopy and laparoscopy were performed. Retro-positioning of
the uterus was observed with an increased size, as would be
expected for a pregnancy of ≥40 days. The bilateral fallopian tubes
and ovaries appeared normal, but there were some adhesions between
the posterior uterine wall and the recto-uterine pouch and greater
omentum. The adhesions were surgically separated. A T-type
contraceptive ring placed with left part deletion in the uterine
cavity was detected. There were some decidual changes of the
endometrium, but no villus tissue in the uterine cavity. A
curettage was undertaken with a curette until the suction tube
sensed some roughness, and the curettage was then stopped. The
right section of the liver was dissected by hepatobiliary surgeons.
There was a mass of 3.0×4.0 cm rich with blood extending out of the
liver surface. Histopathologically, the mass was found to be an
ectopic pregnancy. The patient was followed up for 3 months and
recovered post-surgery without any more treatments.
Discussion
Ectopic pregnancies typically implant on the
peritoneal surface following the partial disruption of the initial
site of implantation in the fallopian tube. The pelvic cavity is
the most common site, but ectopic pregnancies have been reported to
occur in various sites within the peritoneal cavity (14). Primary hepatic pregnancy is an
extremely rare condition with an incidence rate of 1:15,000 per
inner uterus pregnancy (15). Over
the past 50 years, only 21 cases have been reported in the English
language medical literature, among which only 29% progressed beyond
the first trimester (4,16–36).
Ectopic pregnancy is one of the common acute
abdominal conditions in clinical obstetrics and gynecology (2% of
pregnancies), and comprises implantation anywhere outside the
uterine cavity, including tubal pregnancy, ovarian pregnancy and
abdominal cavity pregnancy (for example, mesenteric pregnancy,
hepatic pregnancy, broad ligament pregnancy, cervical pregnancy,
uterine rudimentary horn pregnancy and cesarean scar pregnancy);
among these, the most common is tubal pregnancy, accounting for
~97% of cases, while the incidence of abdominal pregnancy is <1%
(2,37).
Ectopic pregnancy in the abdominal cavity is often
misdiagnosed because of its low incidence, specific location and
atypical clinical manifestations and signs. Worley et al
reported that only 6 of 10 women with advanced extrauterine
pregnancies were discovered preoperatively, and hemorrhage was
common with 9 of 10 patients requiring blood transfusions (7). Hepatic pregnancy is a rare type of
abdominal cavity pregnancy. The majority of the previously reported
cases of hepatic pregnancy involved liver rupture and bleeding
(38) and the consequences were very
dangerous. Hepatic pregnancy is frequently not diagnosed in early
pregnancy and so the best treatment period is missed; the majority
of patients are admitted for surgery following liver rupture. The
patient in the present case soon recovered because of early
diagnosis and prompt treatment.
Abdominal pregnancies usually present with acute
hemoperitoneum (39) and the
pre-operative diagnosis is extremely difficult. Imaging plays an
important role in the diagnosis of ectopic pregnancy, particularly
that of hepatic pregnancy. Although US is the primary modality used
in the diagnosis of ectopic pregnancy, various forms of this
condition and their complications may occasionally be further
evaluated with CT or MRI. After the patient in the present case
study was admitted to hospital, US, plain and enhanced CT, and
PET-CT were carried out. The examinations using the three different
types of imaging all prompted the diagnosis of liver ectopic
pregnancy. The US scan revealed a hyper-echoic mass in the right
hepatic lobe with a cystic sonolucent area within a fluid
sonolucent area. In a previous case of ectopic pregnancy in the
liver, Wang et al reported that US revealed only a small
amount of effusion in the pelvic cavity (40). Jiang et al used a
three-dimensional high-definition live rendering image to diagnosis
interstitial ectopic pregnancy (41). In the present case, CT of the patient
revealed a mass in the right hepatic lobe with a slightly
low-density peripheral region and oval central portion with lower
density in the plain scan, and a significantly enhanced peripheral
portion and non-enhanced center in the enhanced scan. Wang et
al reported that CT plain scanning displayed a polygonal,
moderate density shadow of the left liver lobe, while enhanced CT
exhibited no signs of intensification (40). Kuai et al also reported that
CT transverse imaging for a patient with ectopic liver pregnancy
showed a mixed density lesion within the right liver lobe under the
diaphragm (42). MRI is one of the
modalities typically used in the diagnosis of ectopic pregnancy.
Wang et al reported that on T1-weighted imaging (WI), the
lesion appeared round with a low signal intensity, while on T2WI,
the lesion exhibited a high signal; with enhanced MRI, the lesion
exhibited irregular mild plaque-like intensification during the
venous phase (40). The PET-CT
appearance of hepatic pregnancy has rarely been reported before.
The present study revealed a mass in the right hepatic lobe for
which the peripheral portion had increased glucose metabolism
(SUVmax, 5.7) while the central portion did not exhibit increased
glucose metabolism. Familiarity with the typical and atypical US,
CT, MRI and PET-CT appearances of various forms of ectopic
pregnancy facilitates the prompt and accurate diagnosis and
treatment of this condition (43).
The risk of ectopic pregnancy has been found to be
associated with previous adnexal surgery [adjusted odds ratio
(OR)=3.99, 95% confidence interval (CI): 2.40–6.63], uncertainty of
previous pelvic inflammatory disease (adjusted OR=6.89, 95% CI:
3.29–14.41), and positive CT IgG serology (adjusted OR=5.26, 95%
CI: 3.94–7.04); a history of infertility including tubal
infertility (adjusted OR=3.62, 95% CI: 1.52–8.63), non-tubal
infertility (adjusted OR=3.34, 95% CI: 1.60–6.93) and in
vitro fertilization treatment (adjusted OR=5.96, 95% CI:
1.68–21.21) correlated with the risk of ectopic pregnancy; and
women who had previously used condoms were less likely to have an
ectopic pregnancy during the current cycle (adjusted OR=0.27, 95%
CI: 0.21–0.36) (44). The mechanism
of hepatic pregnancy has not yet been clearly elucidated, but may
be due to reverse tubal peristalsis causing the gestational sac to
be delivered into the abdominal cavity where it plants into the
upper surface of the liver through the clockwise peristalsis of the
intestinal canal prior to being absorbed by the peritoneum
(45). The liver has rich blood
circulation, and the surface tension is not strong and is easily
penetrated; thus, the early fetus grows normally, until
mid-pregnancy, when liver rupture and bleeding may occur (4). Intrauterine devices (IUDs) are
potentially an etiological factor. Børlum and Blom reported one
case with primary hepatic pregnancy with a history of IUD use
(14). The patient described in the
present case report also had a history of IUD placement. Another
possible cause of hepatic pregnancy has been suggested to be pelvic
inflammatory disease, such as salpingitis, resulting in perihepatic
adhesion (46).
Hepatic pregnancy is difficult to diagnose due to
its particular location and the lack of specific clinical symptoms.
The majority of cases are identified due to the bleeding caused by
rupture of the liver, but by that time, it is difficult to save the
patient. The present case did not develop bleeding or other serious
consequences due to the timely diagnosis and surgery achieved
through the use of imaging data. It serves as a reminder to be
vigilant for patients with rare ectopic pregnancy by conducting
comprehensive examinations, in order to gain valuable time for the
timely application of the appropriate treatment.
In conclusion, for women of childbearing age with
amenorrhea and elevated β-hCG levels, for whom US or radiographic
imaging show a mixed density mass in the liver edge, but no
gestational sac can be found in the uterus or by bilateral
salpingo-oophorectomy, the possibility of hepatic ectopic pregnancy
must be considered.
Acknowledgements
The present study was supported by the Second
Xiangya Hospital, Central South University.
References
|
1
|
Taran FA, Kagan KO, Hübner M, Hoopmann M,
Wallwiener D and Brucker S: The diagnosis and treatment of ectopic
pregnancy. Dtsch Arztebl Int. 112:693–704. 2015.PubMed/NCBI
|
|
2
|
Fylstra DL: Ectopic pregnancy not within
the (distal) fallopian tube: Etiology, diagnosis, and treatment. Am
J Obstet Gynecol. 206:289–299. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Goksedef BP, Kef S, Akca A, Bayik RN and
Cetin A: Risk factors for rupture in tubal ectopic pregnancy:
Definition of the clinical findings. Eur J Obstet Gynecol Reprod
Biol. 154:96–99. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Brouard KJ, Howard BR and Dyer RA: Hepatic
pregnancy suspected at term and successful delivery of a live
neonate with placental attachment to the right lobe of the liver.
Obstet Gynecol. 126:207–210. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhang Y, Kang D, Zhang B, Yang L and Fan
Z: Ectopic pregnancy causing splenic rupture. Am J Emerg Med.
34:1184.e1–1184.e2. 2016. View Article : Google Scholar
|
|
6
|
Chen L, Qiu L, Diao X, Yue Q and Gong Q:
CT findings of omental pregnancy: A case report. Jpn J Radiol.
33:499–502. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Worley KC, Hnat MD and Cunningham FG:
Advanced extrauterine pregnancy: Diagnostic and therapeutic
challenges. Am J Obstet Gynecol. 198:297.e1–297.e7. 2008.
View Article : Google Scholar
|
|
8
|
Bashir RM, Montgomery EA, Gupta PK, Nauta
RM, Crockett SA, Collea JV and al-Kawas FH: Massive
gastrointestinal hemorrhage during pregnancy caused by ectopic
decidua of the terminal ileum and colon. Am J Gastroenterol.
90:1325–1327. 1995.PubMed/NCBI
|
|
9
|
Centers for Disease Control and Prevention
(CDC), . Ectopic pregnancy - United States, 1990–1992. MMWR Morb
Mortal Wkly Rep. 44:46–48. 1995.PubMed/NCBI
|
|
10
|
van Mello NM, Mol F, Hajenius PJ, Ankum
WM, Mol BW, van der Veen F and van Wely M: Randomized comparison of
health-related quality of life in women with ectopic pregnancy or
pregnancy of unknown location treated with systemic methotrexate or
expectant management. Eur J Obstet Gynecol Reprod Biol. 192:1–5.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Song T, Kim MK, Kim ML, Jung YW, Yun BS
and Seong SJ: Single-dose versus two-dose administration of
methotrexate for the treatment of ectopic pregnancy: A randomized
controlled trial. Hum Reprod. 31:332–338. 2016.PubMed/NCBI
|
|
12
|
Fornazari VA, Szejnfeld D, Júnior J Elito
and Goldman SM: Interventional radiology and endovascular surgery
in the treatment of ectopic pregnancies. Einstein (Sao Paulo).
13:167–169. 2015.(In English, Portuguese). View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang C, Cheng L, Zhang Z and Yuan Z:
Imaging diagnosis of hepatic ectopic pregnancy: A report of one
cas. Intractable Rare Dis Res. 1:40–44. 2012.PubMed/NCBI
|
|
14
|
Børlum KG and Blom R: Primary hepatic
pregnancy. Int J Gynaecol Obstet. 27:427–429. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lu JH, Yang BL and Lin QD: Liver ectopic
pregnancy: A case report and analysis. Chin J Obstet Gynecol.
40:699–700. 2005.
|
|
16
|
Chui AK, Lo KW, Choi PC, Sung MC and Lui
JW: Primary hepatic pregnancy. ANZ J Surg. 71:260–261. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Deladrousse E, Site O, Le Mouel A,
Riethmuller D and Kastler B: Intrahepatic pregnancy: Sonography and
CT findings. AJR AmJ Roentgenol. 173:1377–1378. 1999. View Article : Google Scholar
|
|
18
|
Shukla VK, Pandey S, Pandey LK, Roy SK and
Vaidya MP: Primary hepatic pregnancy. Postgrad Med J. 61:831–832.
1985. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kirby NG: Primary hepatic pregnancy. Br
Med J. 1:2961969. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Luwuliza-Kirunda JM: Primary hepatic
pregnancy. Case report. Br J Obstet Gynaecol. 85:311–313. 1978.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gordeev V: Extrauterine pregnancy with
fetal implantation in the liver. Klin Khir. 67–68. 1980.(In
Russian). PubMed/NCBI
|
|
22
|
Hietala SO, Andersson M and Emdin SO:
Ectopic pregnancy in the liver. Report of a case and angiographic
findings. Acta Chir Scand. 149:633–635. 1983.PubMed/NCBI
|
|
23
|
Mitchell RW and Teare AJ: Primary hepatic
pregnancy. A case report and review. S Afr Med J.
65:2201984.PubMed/NCBI
|
|
24
|
Paulino-Netto A and Roselli A: Hepatic
ectopic pregnancy: Successful surgical treatment of a patient with
hepatic pregnancy and acute hemorrhage. Mt Sinai J Med. 53:514–517.
1986.PubMed/NCBI
|
|
25
|
Veress B and Wallmander T: Primary hepatic
pregnancy. Acta Obstet Gynecol Scand. 66:563–564. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Schlatter MF, DePree B and VanderKolk K:
Hepatic abdominal pregnancy. J Reprod Med. 33:921–924. 1988.
|
|
27
|
Borlum KG and Blom R: Primary hepatic
pregnancy. Int J Gynecol Obstet. 27:427–429. 1988. View Article : Google Scholar
|
|
28
|
Harris GJ, Al-Jurf AS, Yuh WT and
Abu-Yousef MM: Intrahepatic pregnancy. A unique opportunity for
evaluation with sonography, computed tomography, and magnetic
resonance imaging. JAMA. 261:902–904. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Barbosa Ade A Júnior, de Frietas LA and
Mota MA: Primary pregnancy in the liver. A case report. Pathol Res
Pract. 187:329–333. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Nichols C, Koong D, Faulkner K and Thomas
G: A hepatic ectopic pregnancy treated with direct methotrexate
injection. Aust N Z J Obstet Gynaecol. 35:221–223. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Shippey SH, Bhoola SM, Royek AB and Lonng
ME: Diagnosis and management of hepatic ectopic pregnancy. Obstet
Gynecol. 109:544–546. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chin PS, Wee HY and Chern BS: Laparoscopic
management of primary hepatic pregnancy. Aust N Z J Obstet
Gynaecol. 50:95–98. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Qiao JC, Chang ZG, Wei JM, Liu YN, Cui HY
and Zhang Y: Hepatic ectopic pregnancy treated successfully by
hepatectomy. Chin Med J (Engl). 126:4806–4807. 2013.PubMed/NCBI
|
|
34
|
Yadav R, Raghunandan C, Agarwal S, Dhingra
S and Chowdhary S: Primary hepatic pregnancy. J Emerg Trauma Shock.
5:367–369. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Ramphal SR, Moodley J and Rajaruthnam D:
Hepatic pregnancy managed conservatively. Trop D. 40:121–122. 2010.
View Article : Google Scholar
|
|
36
|
Ma J, Zhou C, Duan Z and Jiang Y:
Successful management of primary hepatic pregnancy with selective
hepatic artery embolization and intra-arterial methotrexate
infusion. Int J Gynaecol Obstet. 122:78–79. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Delabrousse E, Site O, Le Mouel A,
Riethmuller D and Kastler B: Intrahepatic pregnancy: Sonography and
CT findings. AJR Am J Roentgenol. 173:1377–1378. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Darkhaneh R Faraji, Asgharnia M, Porkar N
Farahmand and Alipoor AA: Predictive value of maternal serum β-hCG
concentration in the ruptured tubal ectopic pregnancy. Iran J
Reprod Med. 13:101–106. 2015.PubMed/NCBI
|
|
39
|
Bohiltea R, Radoi V, Tufan C, Horhoianu IA
and Bohiltea C: Abdominal pregnancy-case presentation. J Med Life.
8:49–51. 2015.PubMed/NCBI
|
|
40
|
Wang CL, Cheng XY, Yuan ZD and Wang JJ:
Imaging diagnosis of ectopic pregnancy in the liver. Rare and
Uncommon Diseases. 14:1–5. 2008.
|
|
41
|
Jiang LY, Wang PH, Lee HY and Chen CY:
Diagnosis of interstitial ectopic pregnancy using a
three-dimensional high-definition live rendering image. Taiwan J
Obstet Gynecol. 54:465–466. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Kuai XP, Wang SY and Qiu JM: Ectopic
pregnancy implanted in the liver under the diaphragm. Taiwan J
Obstet Gynecol. 52:586–587. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Kao LY, Scheinfeld MH, Chernyak V,
Rozenblit AM, Oh S and Dym RJ: Beyond ultrasound: CT and MRI of
ectopic pregnancy. AJR Am J Roentgenol. 202:904–911. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Li C, Meng CX, Zhao WH, Lu HQ, Shi W and
Zhang J: Risk factors for ectopic pregnancy in women with planned
pregnancy: A case-control study. Eur J Obstet Gynecol Reprod Biol.
181:176–182. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Jing Nie: A case of liver pregnancy. Clin
Med. 21:55–56. 2001.
|
|
46
|
Ali V, Lilja JF, Chuang AZ, Mogallapu RV
and Sabonghy E: Incidence of perihepatic adhesions in ectopic
gestation. Obstet Gynecol. 92:995–998. 1998. View Article : Google Scholar : PubMed/NCBI
|