Introduction
Imbalances in offensive factors (including acid,
pepsin, and Helicobacter pylori infection) and defensive
factors (including mucin, prostaglandin, bicarbonate, nitric oxide,
and growth factors) serve an important role in the pathology of
chronic gastric ulcers, which are associated with the development
of gastric cancer (1). The
prevalence of chronic gastric disease, in particular gastric
ulcers, is increasing (2); however,
the etiology is currently unclear. Lifestyle factors, including
alcohol consumption, tobacco use and stress, are widely accepted as
causative factors in the pathogenesis of chronic gastric ulcers
(2).
Neuropeptides are a type of small protein-like
molecule that are associated with a wide range of brain functions
and have also been demonstrated to regulate gastric juice
secretion, motility and contractions (3). These neuropeptides, including
vasoactive intestinal peptide (VIP), substance P (SP), somatostatin
(SS), motilin (MOT) and endothelin-1 (ET-1), are widely distributed
in the gastrointestinal tract and modulate the immune reaction in
the intestinal mucosa (3,4). Abnormal levels of these neuropeptides
have previously been observed in patients with gastrointestinal
mucosal lesions and hemorrhage (5).
At present, the primary clinical treatment for
gastric ulcers is the administration of histamine-2 receptors
antagonist (including cimetidine and ranitidine) or proton-pump
inhibitors (including lansoprazole) to reduce gastric juice
secretion (6). However, long-term
use of these agents may cause serious side effects, including
hypergastrinemia, nausea, abdominal pain, constipation, diarrhea
and increased risk of hip fracture (7). Therefore, the development of more
effective pharmacological agents to treat gastric ulcers with fewer
side effects is of great importance.
Insect tea, which is produced using insect feces, is
a traditional drink that has long been used by ethnic minorities in
southwest China (8). Insect tea
contains no tea leaves, rather the name is derived from the color
of the drink (9). A number of
previous studies have reported that insect tea has health benefits,
including anticancer (8,10), antioxidant (11), hypoglycemic and antihypertensive
effects (8). Insect tea has also
been reported to reduce inflammation-induced colonic mucosa injury
and promote duodenal motility activity (8). The aim of the present study was to
investigate the potential protective effect of insect tea on the
gastrointestinal tract and to elucidate the mechanisms underlying
these effects using HCl/ethanol-induced gastric ulcers in mice.
Materials and methods
Preparation of raw tea and insect tea
aqueous extracts
Fresh raw tea (Ilex kudingcha C. J. Tseng)
and insect tea were purchased from Guizhou Chishui Green Ecology
Industry Co., Ltd. (Zunyi, China), freeze-dried and subsequently
ground into separate fine powders, the raw tea (Kuding tea) and
insect tea was identified by Professor Huayi Suo (Southwest
University, Chongqing, China). Powdered samples (1 kg) were added
to 10 l ethanol (70%, vol/vol) and extracted at 37°C for 2 h. Each
solution was filtered and condensed using a vacuum rotary
evaporator (1,490 × g for 10 min) (Eyela N-1100V-W; Tokyo Rikakikai
Co. Ltd, Tokyo, Japan) at 37°C, freeze-dried and stored at −80°C
for further experiments.
Amino acid assay
A total of 800 mg of each type of tea was mixed with
3 ml sulfosalicylic acid solution (6%, w/v; Shanghai Zhanyun
Chemical Company Limited, Shanghai, China), sonicated (26 kHz) for
60 min at 37°C and cooled to 4°C for 12 h. The extract was
centrifuged at 13,000 × g for 2 min at 4°C and filtered using a
0.45-µm milliporefilter (EMD Millipore, Billerica, MA, USA). The
amino acids in raw tea and insect tea were determined using an
automatic amino acid analyzer (L-8800; Hitachi, Ltd., Tokyo, Japan)
equipped with a Hitachi Packed Column (2620MSC-PS; inner diameter,
4.6 mm; length, 80 mm) filled with a Na+-form sulfonic
resin (Langfang Miaoyang Chemical Company Limited, Langfang,
China). The amount of total amino acids were identified and
quantified against a standard compound based on its retention time
and peak areas. The amino acid standards were purchased from
National Institute for Food and Drug Control (Beijing, China).
Animal groups and acute gastric ulcer
induction
A total of 35 male ICR mice (6 weeks old, 25–30 g)
were purchased from the Experimental Animal Center of Chongqing
Medical University (Chongqing, China). Mice were housed with a
standard 12-h light/dark cycle at 23±1°C with relative humidity
50±5% and had ad libitum access to food and water. Mice were
randomly divided into five groups (n=7 in each) and treated as
follows: Group 1 (normal group), administered 0.9% normal saline;
group 2 (control group), HCl/ethanol (0.1 ml HCl or ethanol per 10
g; 60% in 150 mM HCl on the last day); group 3 (raw tea group),
HCl/ethanol-treated mice administered with raw tea (100 mg/kg/day
for 28 days) and group 4 (insect tea group), HCl/ethanol-treated
mice administered with insect tea (100 mg/kg/day for 28 days; group
5 (ranitidine), HCl/ethanol-treated mice administered with
ranitidine (50 mg/kg/day for 28 days, Sigma-Aldrich; Merck KGaA,
Darmstadt, Germany). All treatments were administered via oral
gavage. On experimental day 29, all mice had developed jejunitis
and were denied food but allowed to drink water ad libitum.
Mice in groups 3, 4 and 5 were gavaged with a stomach injury
inducer (0.1 ml HCl or ethanol per 10 g; 60% in 150 mM HCl) on day
30 and sacrificed after 1 h (12).
Blood samples were harvested from the inferior vena cava,
centrifuged at 3,000 × g for 10 min at 4°C and stored at −80°C
until required for further study. The animal protocol used in the
present study was approved by the Animal Ethics Committee of
Chongqing University of Education.
Evaluation of antiulcer activity
The volume of gastric secretions from each mouse was
measured with a 10-ml measuring cylinder following sacrifice and
the pH of gastric juice was determined using a SevenEasy pH meter
(Mettler Toledo GmbH, Greifensee, Switzerland). The stomachs were
harvested using hemostatic forceps, and the isolated stomachs were
inflated by injecting 10 ml 1% formalin solution for 10 min to fix
the tissues at 25°C and opened along the greater curvature. Gastric
tissue was observed using digital camera (D550; Canon, Tokyo,
Japan), and the gastric injury area was measured using ImageJ 1.44
software (National Institutes of Health, Bethesda, MD, USA). The
gastric injury inhibitory rate (%) = (1 - gastric injury area of
sample treated mice / gastric injury area of control mice) ×
100.
Measurement of gastric neuropeptide
levels
Serum levels of MOT (H182; MOT assay kit), SP (H218;
substance P assay kit), VIP (H219; vasoactive intestinal peptide
assay kit), SS (H092; somatostatin assay kit) and ET-1 (H093;
endothelin-1 assay kit) were measured with radioimmunoassay kits
(all Beijing Puer Weiye Biotechnology Co., Ltd., Beijing, China)
according to the manufacturer's protocols.
Measurement of superoxidase (SOD),
nitric oxide (NO) and malondialdehyde (MDA) in gastric tissue
Gastric levels of SOD (A001-3), NO (A012) and MDA
(A003-1) were respectively measured using commercial ELISA kits
(Nanjing Jiancheng Bioengineering Institute, Nanjing, Jiangsu,
China) according to the manufacturer's protocols.
Protein extraction and western blot
analysis
A total of 100 mg gastric tissue was washed with
ice-cold PBS, homogenized with ice-cold modified
radioimmunoprecipitation assay buffer (Sigma-Aldrich; Merck KGaA)
and centrifuged at 13,000 × g for 30 min at 4°C. Protein
concentrations were determined using a bicinchoninic acid protein
assay kit (Bio-Rad Laboratories, Inc., Hercules, CA, USA). For
western blot analysis, 50 µg protein extracts were separated by 10%
SDS-PAGE and electrotransferred onto a nitrocellulose membrane. The
membrane was blocked with 10% skimmed milk at 4°C for 8 h. Blots
were subsequently incubated with antibodies against nuclear factor
(NF)-κB (#8214), inhibitor of NF-κB (IκB-α) (#8219), epidermal
growth factor (EGF) (#2237), EGF receptor (EGFR) (#11862),
endothelial nitric oxide synthase (eNOS) (#32027), neuronal NOS
(nNOS) (#4231), inducible NOS (iNOS) (#13120), Mn-SOD (#13141),
Cu/Zn-SOD (#4266), catalase (CAT) (#14097) and β-actin (#12262)
(all 1:5,000; all Cell Signaling Technology, Inc., Danvers, MA,
USA) for 4 h at 4°C. Membranes were washed with PBS (3 times for 15
min) containing 0.05% Tween 20 (PBS-T) and subsequently incubated
with horseradish peroxidase-conjugated goat-anti-rabbit or
anti-mouse immunoglobulin G (#14709; 1:1,000; Cell Signaling
Technology, Inc.) for 1 h at room temperature. Blots were washed
three times with PBS-T (3 times for 15 min) and antibody binding
was visualized by enhanced chemiluminescence (ECL Western Blotting
Detection kit; GE Healthcare Life Sciences, Little Chalfont, UK).
Protein expression was quantified using ImageJ 1.44 software
(National Institutes of Health).
Statistical analysis
Data are presented as the mean ± standard deviation.
Differences between groups were assessed using one-way analysis of
variance with Duncan's multiple range tests. The SAS v9.1
statistical software package (SAS Institute, Inc., Cary, NC, USA)
was used for the analysis. P<0.05 was considered to indicate a
statistically significant difference.
Results
Accumulation of amino acids in insect
tea
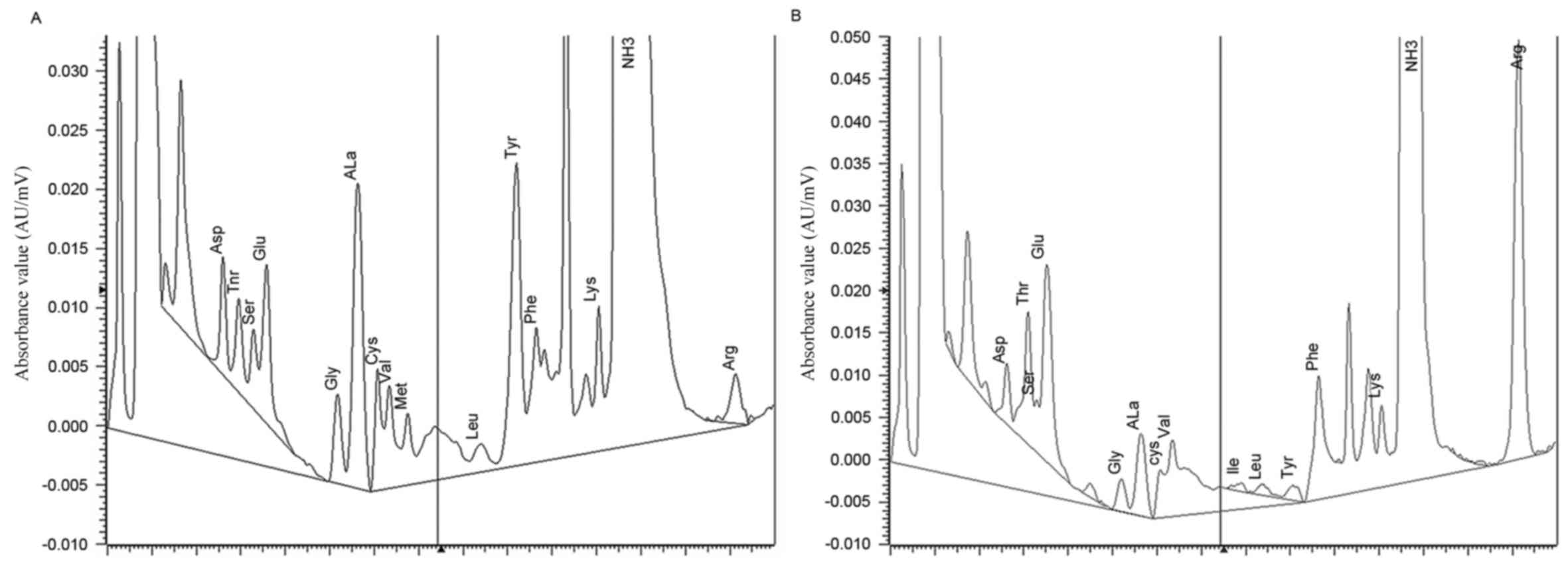
The amino acid contents of raw tea and insect tea as
determined by an automatic amino acid analyzer are presented in
Fig. 1 and Table I. Compared with the raw tea, insect
tea contained a markedly higher level of total amino acids. The
insect tea also contained higher levels of human essential amino
acids including threonine, valine, isoleucine, phenylalanine and
lysine. However, levels of methionine and leucine were lower in
insect tea compared with raw tea. Furthermore, tryptophan was not
detected in either of the preparations, and insect tea contained
higher levels of glutamate, arginine and proline compared with raw
tea.
 | Table I.Amino acid components of raw tea and
insect tea. |
Table I.
Amino acid components of raw tea and
insect tea.
|
| Content (mg per 100
g) |
|---|
|
|
|
|---|
| Amino acid | Raw tea | Insect tea |
|---|
| Aspartate |
0.329 |
0.315 |
| Threonine |
0.320 |
0.785 |
| Serine |
0.219 |
0.166 |
| Glutamate |
0.660 |
1.454 |
| Glycine |
0.227 |
0.146 |
| Alanine |
1.241 |
0.532 |
| Cysteine |
0.772 |
0.539 |
| Valine |
0.494 |
1.525 |
| Methionine |
0.407 |
0.000 |
| Isoleucine |
0.000 |
0.077 |
| Leucine |
0.244 |
0.123 |
| Tyrosine |
2.806 |
0.249 |
| Phenylalanine |
0.903 |
2.122 |
| Lysine |
0.534 |
0.550 |
| Histidine |
0.000 |
0.000 |
| Arginine |
0.457 |
5.280 |
| Proline |
0.294 |
1.478 |
| Total amino
acids | 33.414 | 34.159 |
Insect tea attenuates
HCl/ethanol-induced gastric ulcer
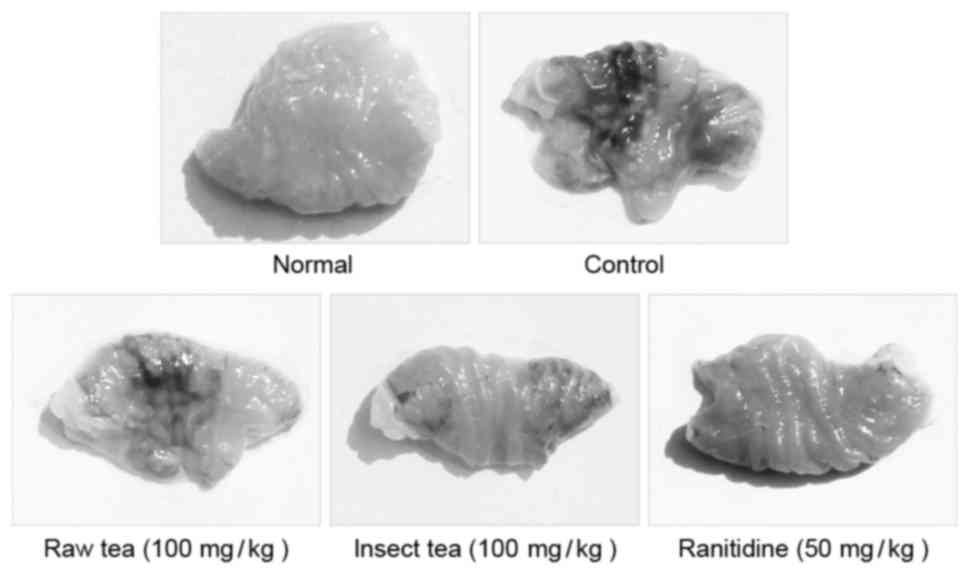
HCl/ethanol treatment significantly induced the
formation of gastric ulcers and bleeding in mice (P<0.05;
Fig. 2 and Table II). Administration of 100 mg/kg raw
tea or insect tea significantly reduced area of HCl/ethanol-induced
acute gastric ulcer in mice (P<0.05; Table II); the level of inhibition was
56.3% (gastric ulcer area, 3.65±0.43 mm2) and 72.1%
(gastric ulcer area, 2.33±0.48 mm2) with raw tea and
insect tea treatment, respectively. These results suggest that the
two treatments exhibited a significant protective effect against
HCl/ethanol-induced gastric ulcers; however, their effect was
weaker than that observed in ranitide-treated mice (gastric ulcer
area, 1.05±0.27 mm2; inhibition, 87.4%). In addition,
HCl/ethanol treatment significantly increased gastric juice
secretion compared with normal mice (P<0.05; Table II). Following the administration of
100 mg/kg raw tea or insect tea for 28 days, gastric juice
secretion was significantly reduced compared with the control group
(P<0.05; Table II). Raw tea and
insect tea treatment also significantly increased the pH of gastric
juice compared with control mice (P<0.05; Table II). All mice in all groups survived
the total experimental period.
 | Table II.Stomach appearance, gastric secretion
volume, and pH of gastric juice of insect tea treated
HCl/ethanol-induced gastric injury mice. |
Table II.
Stomach appearance, gastric secretion
volume, and pH of gastric juice of insect tea treated
HCl/ethanol-induced gastric injury mice.
|
| Gastric mucosal
injury |
|
|
|---|
|
|
|
|
|
|---|
| Group | Area
(mm2) | Inhibitory rate
(%) | Gastric secretion
volume (ml) | Gastric juice
pH |
|---|
| Normal |
0.0±0.0 |
100±0.0 |
0.28±0.04 |
3.5±0.1 |
| Control |
8.35±0.81a |
0.0±0.0a |
1.87±0.36a |
1.0±0.2a |
| Raw tea |
3.65±0.43a,b |
56.3±4.1a,b |
0.85±0.16a,b |
2.4±0.2a,b |
| Insect tea |
2.33±0.48a–c |
72.1±4.4a–c |
0.60±0.11a–c |
2.9±0.2a–c |
| Ranitidine |
1.05±0.27a–d |
87.4±2.2a–d |
0.36±0.07a–d |
3.3±0.3a–d |
Effect of insect tea on serum
neuropeptide levels in HCl/ethanol-induced gastric ulcer mice
HCl/ethanol treatment was observed to significantly
increase the acute gastric ulcer-related serum neuropeptide levels
of MOT, SP and ET-1 compared with normal mice (P<0.05; Table III). Administration of 100 mg/kg
raw tea or insect tea significantly attenuated the serum levels of
MOT, SP and ET-1 compared with control mice (P<0.05; Table III). In addition, treatment with
raw tea or insect tea significantly increased the serum levels of
SS and VIP compared with the control group (P<0.05; Table III). Furthermore, the results
indicated that insect tea modulated the neuropeptide levels to a
greater extent than raw tea (Table
III).
 | Table III.Serum MOT, SS, SP, VIP and ET-1
levels of Insect tea treated HCl/ethanol-induced gastric injury
mice. |
Table III.
Serum MOT, SS, SP, VIP and ET-1
levels of Insect tea treated HCl/ethanol-induced gastric injury
mice.
| Group | MOT (µg/l) | SS (µg/l) | SP (µg/l) | VIP (µg/l) | ET-1 (µg/l) |
|---|
| Normal |
48.2±2.6 |
133.0±15.3 |
57.1±2.9 |
110.6±9.7 |
66.9±1.8 |
| Control |
131.3±13.1a |
48.2±6.3a |
137.9±18.2a |
52.3±2.2a |
105.6±5.1a |
| Raw tea |
89.5±7.2a,b |
92.6±4.8a,b |
101.2±7.3a,b |
80.9±5.2a,b |
86.6±1.1a,b |
| Insect tea |
66.3±4.2a–c |
107.5±4.0a–c |
80.6±4.8a–c |
91.2±4.7a–c |
78.9±2.3a–c |
| Ranitidine |
55.6±2.3a–d |
122.5±6.1a–d |
68.9±2.6a–d |
101.2±2.1a–d |
72.5±1.6a–d |
Effect of insect tea on gastric levels
of SOD, NO and MDA in HCl/ethanol-induced gastric ulcer mice
HCl/ethanol treatment significantly reduced the
gastric activity of the antioxidant enzyme SOD (69%) and
significantly induced the lipid peroxidation related MDA generation
(5.0-fold) compared with normal mice (P>0.05; Table IV). Treatment with 100 mg/kg raw tea
or insect tea significantly increased the levels of SOD (to
225.6±31.2 and 291.6±25.5 kU/l, respectively) and NO (to 8.2±0.4
and 12.2±0.4 µmol/l, respectively) compared with control mice
(P<0.05; Table IV). In addition,
raw tea and insect tea significantly reduced MDA generation
compared with the control group (P<0.05; Table IV). Raw tea had a weaker effect in
regulating antioxidant activity compared with insect tea (Table IV).
 | Table IV.Gastric tissues SOD, NO and MDA
activities of insect tea treated HCl/ethanol-induced gastric injury
mice. |
Table IV.
Gastric tissues SOD, NO and MDA
activities of insect tea treated HCl/ethanol-induced gastric injury
mice.
| Group | SOD (kU/l) | NO (µmol/l) | MDA (µmol/l) |
|---|
| Normal |
347.9±40.5 |
15.2±0.3 |
17.8±2.1 |
| Control |
107.1±24.3a |
3.1±0.2a |
89.2±4.2a |
| Raw tea |
225.6±31.2a,b |
8.2±0.4a,b |
50.2±3.6a,b |
| Insect tea |
291.6±25.5a–c |
12.2±0.4a–c |
32.5±2.3a–c |
| Ranitidine |
321.3±22.6a–d |
13.8±0.3a–d |
24.7±1.8a–d |
Effect of insect tea on the gastric
expression of Mn-SOD, Cu/Zn-SOD, and CAT in HCl/ethanol-induced
gastric ulcer mice
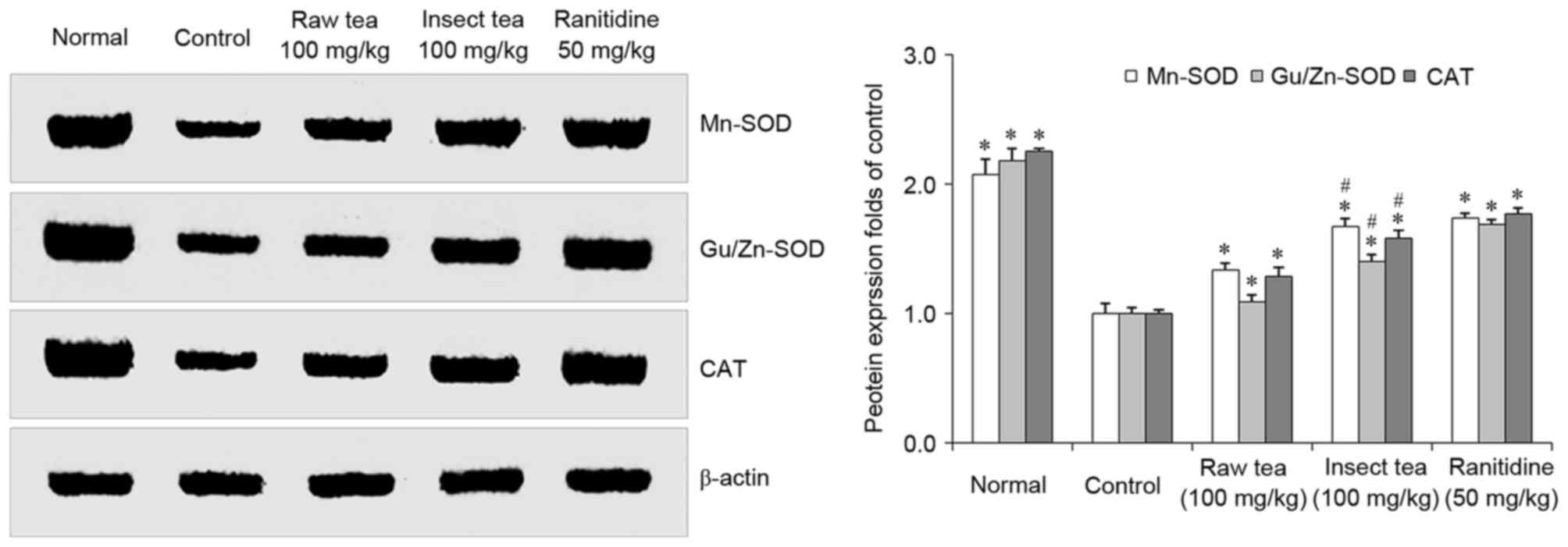
In HCl/ethanol-treated mice, the gastric levels of
Mn-SOD, Cu/Zn-SOD, and CAT were significantly decreased compared
with that in normal mice (P<0.05; Fig. 3). Mice treated with 100 mg/kg raw tea
or insect tea exhibited significant increases in the gastric levels
of Mn-SOD, Cu/Zn-SOD, and CAT compared with the control mice
(P<0.05; Fig. 3). SOD, Cu/Zn-SOD
and CAT protein expression were significantly higher in the gastric
tissue of insect tea treated mice compared with raw tea treated
mice. (P<0.05; Fig. 3).
Effect of insect tea on the gastric
expression of nNOS, eNOS, and iNOS in HCl/ethanol-induced gastric
ulcer mice
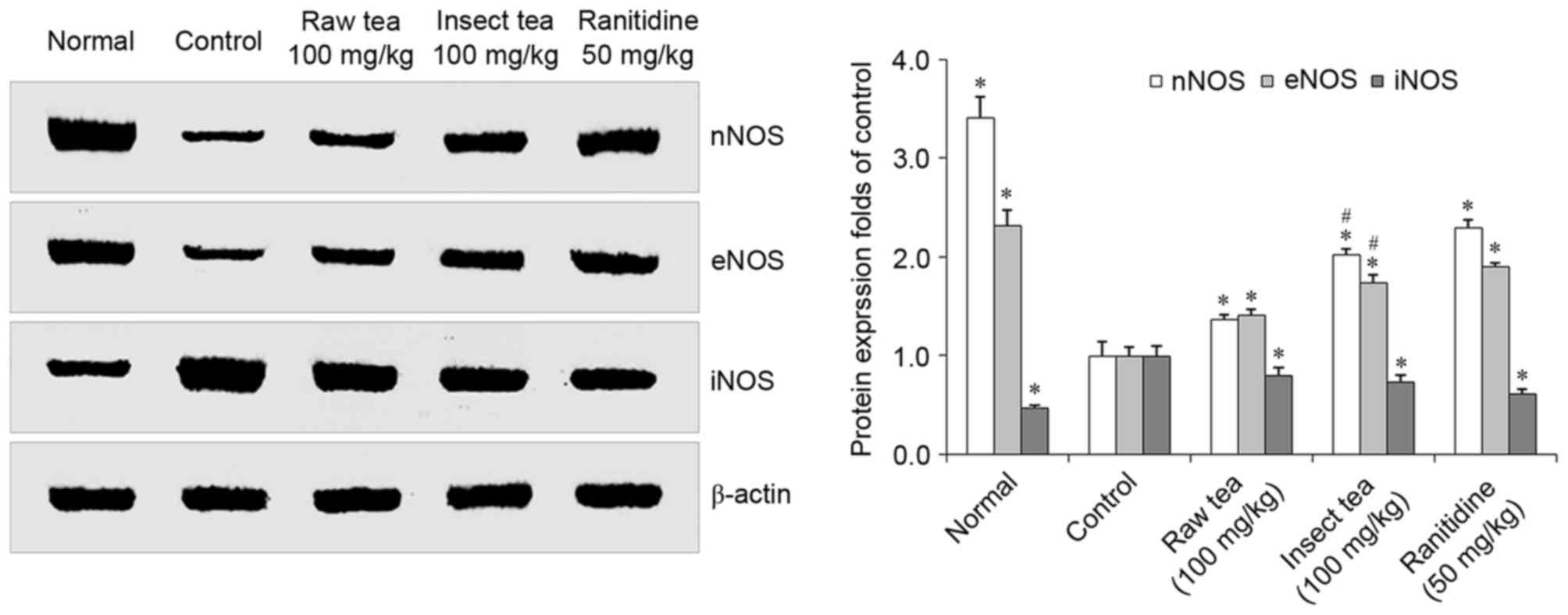
HCl/ethanol treatment significantly increased
gastric iNOS expression and significantly decreased gastric nNOS
and eNOS expression compared with normal mice (P<0.05; Fig. 4). However, mice treated with 100
mg/kg raw tea or insect tea were demonstrated to have significantly
lower iNOS protein expression compared with control mice
(P<0.05; Fig. 4). Furthermore,
mice in the raw tea and insect tea groups exhibited significant
increases in levels of nNOS and eNOS compared with control mice
(P<0.05; Fig. 4). Furthermore,
nNOS and eNOS protein expression in gastric tissue of insect tea
treated mice was significantly higher compared with raw tea treated
mice (P<0.05; Fig. 4).
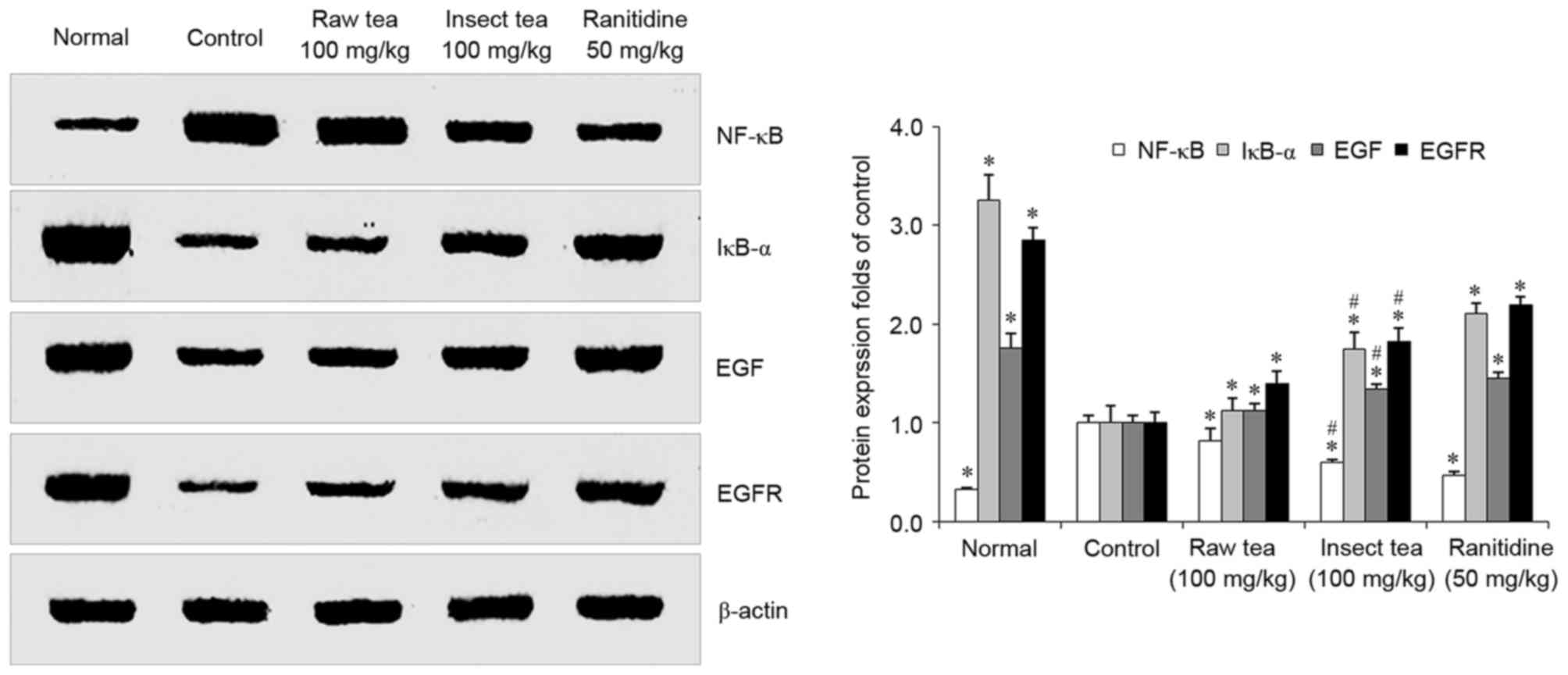
Effect of insect tea on the gastric
expression of NF-κB, IκB-α, EGF and EGFR in HCl/ethanol-induced
gastric ulcer mice
HCl/ethanol treatment significantly increased the
expression of gastric NF-κB compared with normal mice (P<0.05;
Fig. 5). Treatment with raw tea or
insect tea significantly reduced the levels of NF-κB compared with
control mice, and tea samples also significantly increased the
gastric IκB-α expression compared with control mice (P<0.05;
Fig. 5). Levels of EGF and its
receptor EGFR were significantly downregulated in
HCl/ethanol-treated mice compared with the normal group (P>0.05;
Fig. 5). However, EGF and EGFR were
significantly increased in the raw tea and insect tea groups
compared with the control group (P<0.05; Fig. 5). In the insect tea group, levels of
IκB-α, EGF and EGFR were significantly higher and NF-κB expression
was significantly lower compared with the raw tea group (P<0.05;
Fig. 5).
Discussion
Insect tea is a type of non-Camellia tea with a long
history in China (8). Previous
studies have reported that insect tea contains high levels of amino
acids (13,14). In the present study, it was
demonstrated that insect tea contains higher levels of human
essential amino acids (such as threonine, valine, isoleucine,
phenylalanine, and lysine) compared with raw tea. Glutamate and its
derivative, proglumide, have been reported to have anticholinergic
effects as gastrin receptor antagonists that decrease gastric acid
secretion and have a healing effect on gastric ulcers (15). Arginine is a substrate for nitric
oxidesynthase and has previously exhibited gastroprotective and
ulcer healing effects in animal and human studies (16–18). The
amino acids leucine, isoleucine and valine constitute a
branched-chain amino acid (BCAA), which is an amino acid with
aliphatic side-chains (19). BCAAs
have been reported to have therapeutic effects, promoting muscle
and wound healing in a previous animal study (20). In the present study, it was
demonstrated that insect tea treatment increased the pH of gastric
juice in HCl/ethanol-treated mice. Maintaining a higher gastric
juice pH reduces the activity of pepsin, which is a risk factor for
gastric ulcers (21,22), and improves healing of the gastric
mucosa (23).
Excess gastric acid secretion is an important risk
factor that promotes the development of gastric ulcers (24,25), and
reducing gastric juice secretion is a useful strategy to prevent
and treat gastric ulcers (5).
Gastric juice secretion is regulated by the central nervous system
(CNS), in particular the vagus nerve system (26). Neuropeptides are able to influence
CNS activity and maintain gastric mucosal homeostasis (3). Some neuropeptides, including SP, MOT,
SP, VIP and ET-1, are associated with the regulation of gastric
acid secretion and serve important roles in gastric tissue repair
under normal physiological conditions (27). In the present study, it was observed
that administration of 100 mg/kg insect tea significantly decreased
serum levels of SP, MOT and ET-1 in gastric ulcer mice. SP
stimulates gastric juice secretion (28) and decreases gastric contractions
(29), resulting in delayed gastric
emptying and aggravating gastric ulcers in patients with gastritis
(30,31). MOT is a powerful inducer of
gastrointestinal motor activity (32) and intestinal contractilities, and
stimulates the secretion of human gastric pepsin (33,34).
ET-1 is a potent vasoconstrictor that is produced by vascular
endothelial cells (35). Submucosal
injections of ET-1 have previously been demonstrated to induce
gastric ulcers in rats (36).
Increased levels of ET-1 have previously been observed in
critically ill patients with stress ulcers (37). Increased ET-1 generation is
associated with the progression of gastric mucosal injury in rodent
models, and inhibiting ET-1 activity has been demonstrated to
reduce chemically-induced gastric ulcers (38,39). In
the present study, it was demonstrated that the administration of
100 mg/kg insect tea significantly increased serum levels of SS and
VIP in gastric ulcer mice. SS is a type of amino acid peptide that
is distributed in the brain and the peripheral organs (3) and is able to inhibit chemically
(pentagastrin, bethanechol, or histamine)-induced gastric acid
secretion in rats via activating somatostatin type 2 receptors
(40–42). Peripheral injection of VIP has been
demonstrated to decrease gastric acid secretion via inhibiting
vagus nerve activation in rats (43,44).
This suggests that insect tea may influence gastric juice secretion
in HCl/ethanol-induced gastric ulcers by increasing the serum
levels of VIP and SS, as well as reducing the serum levels of SP,
MOT and ET-1.
Chemically-induced or ischemia-associated
overgeneration of reactive oxygen species (ROS) results in lipid
peroxidation of gastric ulcers (45–47). The
administration of SOD has been reported to significantly protect
against gastric mucosal injury (48). In the present study, administration
of insect tea was observed to increase total SOD enzyme activity
and the levels of Mn-SOD and Cu/Zn-SOD proteins in gastric ulcer
mice. Insect tea also significantly increased the level of CAT in
gastric mice. In a previous study, combined treatment with SOD and
CAT was reported to reduce gastric lipid peroxidation levels in
indomethacin-treated gastric ulcers in rats (47). In the present study, insect tea
treatment significantly decreased the HCl/ethanol-induced
generation of gastric MDA, which is one of the final products of
lipid peroxidation and is widely used as an indicator to evaluate
levels of tissue damage (49).
NO is a gas signaling molecule generated from NOS,
and has been reported to serve a beneficial role during gastric
ulcer healing in animals (50).
There are three subtypes of NOS in human gastric mucosa, namely
nNOS, iNOS and eNOS (51). In the
present study, insect tea treatment significantly increased the
gastric levels of NO and enhanced the protein expressions of nNOS
and eNOS in gastric tissues. Insect tea also reduced the iNOS
protein expression in ulcer mice. The low concentration of NO
produced by eNOS has been observed to reduce gastric juice
secretion, promoting wound healing by increasing blood flow and
angiogenesis and protecting the gastric mucosa in gastric ulcer
models (52,53). Increased expression of eNOS promotes
ulcer healing via its effects on angiogenesis in the gastric tissue
of rats (54,55).
NF-κB is a classic inflammation-associated protein
that promotes inflammatory diseases and cancer (56). In the present study, insect tea
treatment reduced the gastric levels of NF-κB protein in mice.
Increasing the protein expressions of IκB-α, which is a cytoplasmic
inhibitor of NF-κB, reduces the inflammatory reaction and
carcinogenesis in gastric disease (57). Insect tea treatment significantly
increased the gastric protein expression of IκB-α in the present
study.
EGF stimulates cell growth, proliferation and
differentiation by binding to EGFR, which is secreted by the
salivary glands, Brunner's glands in the duodenum and pancreas
(58). In the present study, insect
tea treatment significantly increased the levels of EGF and EGFR in
the gastric tissue of ulcer mice. Under normal physiological
conditions, EGF inhibits gastric acid secretion, reducing the
activity of gastric protease, promoting gastric epithelial cell
proliferation and preventing ulcer formation (58,59). EGF
also accelerates healing in gastric ulcers by promoting cell DNA
synthesis in the gastric mucosa (59,60).
In conclusion, the results of the present study
demonstrate that insect tea exhibits a protective effect against
HCl/ethanol-induced gastric ulcers in ICR mice. Insect tea
administration was able to attenuate HCl/ethanol-induced gastric
acid secretion and increase the pH of gastric juice. Treatment with
insect tea also modulated serum levels of MOT, SP, VIP, SS, and
ET-1, and increased the activity of antioxidant enzymes to reduce
lipid peroxidation in gastric tissues. In addition, insect tea
modulated the protein expressions of iNOS, nNOS, and eNOS, and
promoted NO secretion to protect the gastric mucosa. Insect tea
also modulated NF-κB and IκB-α to reduce the inflammatory reaction
and increased the gastric expressions of EGF and EGFR in the
gastric mucosa of mice. These results indicate that the potential
mechanism underlying the protective effects of insect tea may
involve reducing gastric juice secretion, modulating neuropeptides,
and regulating antioxidant activity and inflammatory reactions in
the gastric mucosa. Insect tea represents a potential beneficial
agent for the prevention of HCl/ethanol-induced gastric ulcers
in vivo.
Acknowledgements
The present study was supported by the Construction
Program of Chongqing Engineering Research Center (grant no.
cstc2015yfpt_gcjsyjzx0027), the Scientific Research Foundation for
Returned Overseas Chinese Scholars, State Education Ministry [grant
no. Jiaowaisiliu (2014)1685], the Program for Innovation Team
Building at Institutions of Higher Education in Chongqing (grant
no. CXTDX201601040) and the Introduction of High-level Personnel
Research Start-up Fund of Chongqing University of Education (grant
no. 2013BSRC001).
Glossary
Abbreviations
Abbreviations:
|
VIP
|
vasoactive intestinal peptide
|
|
SP
|
substance P
|
|
SS
|
somatostatin
|
|
MOT
|
motilin
|
|
ET-1
|
endothelin-1
|
References
|
1
|
Malfertheiner P, Chan FK and McColl KE:
Peptic ulcer disease. Lancet. 374:1449–1461. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hsu CC, Hsu YC, Chang KH, Lee CY, Chong
LW, Lin CL, Shang CS, Sung FC and Kao CH: Depression and the risk
of peptic ulcer disease: A nationwide population-based study.
Medicine (Baltimore). 94:e23332015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gyires K: Neuropeptides and gastric
mucosal homeostasis. Curr Top Med Chem. 4:63–74. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chen CY and Tsai CY: Ghrelin and motilin
in the gastrointestinal system. Curr Pharm Des. 18:4755–4765. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Long DM, Leonard AS, Story J and French
LA: Hypothalamus and gastric ulceration: II. production of
gastrointestinal ulceration by chronic hypothalamic Stimulation.
Arch Neurol. 7:167–183. 1962. View Article : Google Scholar
|
|
6
|
Mejia A and Kraft WK: Acid peptic
diseases: Pharmacological approach to treatment. Expert Rev Clin
Pharmacol. 2:295–314. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
Thomson AB, Sauve MD, Kassam N and
Kamitakahara H: Safety of the long-term use of proton pump
inhibitors. World J Gastroenterol. 16:2323–2330. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhao X, Wang R, Qian Y, Li G, Zhou Y and
Sun P: In vivo preventive effects of insect tea on buccal mucosa
cancer in ICR mice. J Cancer Res Ther. 10:651–657. 2014.PubMed/NCBI
|
|
9
|
Xu L, Pan H, Lei Q, Xiao W, Peng Y and
Xiao P: Insect tea, a wonderful work in the Chinese tea culture.
Food Res Int. 53:629–635. 2013. View Article : Google Scholar
|
|
10
|
Qian Y, Li GJ, Wang R, Zhou YL, Sun P and
Zhao X: In vitro anticancer effects of insect tea in TCA8113 cells.
J Cancer Res Ther. 10:1045–1051. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ao C: Scavenging effects of sandy-tea
ethanol extract on super oxide anion and hydroxyl radical. Meat
Res. 4:60–64. 2010.
|
|
12
|
Zhao X, Wang Q, Qian Y and Song JL: Ilex
kudingcha C.J. Tseng (Kudingcha) prevents HCl/ethanol-induced
gastric injury in Sprague-Dawley rats. Mol Med Rep. 7:1613–1616.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wen L, Guo H, Li J, Yin R and Duan Z:
Analyse of thebiological safety and major chemical components of
Sanye insect tea. J Hunan Agric Univ. 22:574–579. 1996.
|
|
14
|
Guo S, Xu W, Wen L, Huang Y and Wang F:
The nutrient analysis and evaluation of Sanye insect-fermented tea.
Chin Bull Entomol. 45:128–132. 2008.
|
|
15
|
Beauchamp RD, Townsend CM, Singh P, Glass
EJ and Thompson JC: Proglumide, a gastrin receptor antagonist,
inhibits growth of colon cancer and enhances survival in mice. Ann
Surg. 202:303–309. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Brzozowski T, Konturek SJ, Sliwowski Z,
Drozdowicz D, Zaczek M and Kedra D: Role of arginine, a substrate
for nitric oxide-synthase, in gastroprotection and ulcer healing. J
Gastroenterol. 32:442–452. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yatabe J, Saito F, Ishida I, Sato A, Hoshi
M, Suzuki K, Kameda T, Ueno S, Yatabe MS, Watanabe T and Sanada H:
Lower plasma arginine in enteral tube-fed patients with pressure
ulcer and improved pressure ulcer healing after arginine
supplementation by arginaid water. J Nutr Health Aging. 15:282–286.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Desneves KJ, Todorovic BE, Cassar A and
Crowe TC: Treatment with supplementary arginine, vitamin C and zinc
in patients with pressure ulcers: A randomized controlled trial.
Clin Nutr. 24:979–987. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhenyukh O, Civantos E, Ruiz-Ortega M,
Sánchez MS, Vázquez C, Peiró C, Egido J and Mas S: High
concentration of branched-chain amino acids promotes oxidative
stress, inflammation and migration of human peripheral blood
mononuclear cells via mTORC1 activation. Free Radic Biol Med.
104:165–177. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhang XJ, Chinkes DL and Wolfe RR: Leucine
supplementation has an anabolic effect on proteins in rabbit skin
wound and muscle. J Nutr. 134:3313–3318. 2004.PubMed/NCBI
|
|
21
|
Alphin RS, Vokac VA, Gregory RL, Bolton PM
and Tawes JW III: Role of intragastric pressure, pH and pepsin in
gastric ulceration in the rat. Gastroenterology. 73:495–500.
1977.PubMed/NCBI
|
|
22
|
Venables CW: Mucus, pepsin, and peptic
ulcer. Gut. 27:233–238. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yamamoto O, Okada Y and Okabe S: Effects
of a proton pump inhibitor, omeprazole, on gastric secretion and
gastric and duodenal ulcers or erosions in rats. Dig Dis Sci.
29:394–401. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Delaney JP, Cheng JW, Butler BA and
Ritchie WP Jr: Gastric ulcer and regurgitation gastritis. Gut.
11:715–719. 1970. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Guth PH: Pathogenesis of gastric mucosal
injury. Annu Rev Med. 33:183–196. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sandor A, Kidd M, Lawton GP, Miu K, Tang
LH and Modlin IM: Neurohormonal modulation of rat
enterochromaffin-like cell histamine secretion. Gastroenterology.
110:1084–1092. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Xie XZ, Zhao ZG, Qi DS and Wang ZM: Assay
of gastrin and somatostatin in gastric antrum tissues of children
with chronic gastritis and duodenal ulcer. World J Gastroenterol.
12:2288–2290. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Geoghegan JG and Pappas TN: Central
peptidergic control of gastric acid secretion. Gut. 40:164–166.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Taché Y, Garrick T and Raybould H: Central
nervous system action of peptides to influence gastrointestinal
motor function. Gastroenterology. 98:517–528. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Holzer P: Neural emergency system in the
stomach. Gastroenterology. 114:823–839. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Erin N, Türker S, Elpek Ö and Yıldırım B:
Differential changes in Substance P, VIP as well as neprilysin
levels in patients with gastritis or ulcer. Peptides. 35:218–224.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Brown JC and Parkes CO: Effect on fundic
pouch motor activity of stimulatory and inhibitory fractions
separated from pancreozymin. Gastroenterology. 53:731–736.
1967.PubMed/NCBI
|
|
33
|
Ruppin H, Domschke S, Domschke W, Wünsch
E, Jaeger E and Demling L: Effects of 13-nle-motilin in
man-inhibition of gastric evacuation and stimulation of pepsin
secretion. Scand J Gastroenterol. 10:199–202. 1975.PubMed/NCBI
|
|
34
|
Itoh Z, Honda R, Hiwatashi K, Takeuchi S,
Aizawa I, Takayanagi R and Couch EF: Motilin-induced mechanical
activity in the canine alimentary tract. Scand J Gastroenterol
Suppl. 39:93–110. 1976.PubMed/NCBI
|
|
35
|
Yanagisawa M, Kurihara H, Kimura S, Tomobe
Y, Kobayashi M, Mitsui Y, Yazaki Y, Goto K and Masaki T: A novel
potent vasoconstrictor peptide produced by vascular endothelial
cells. Nature. 332:411–415. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Lazaratos S, Kashimura H, Nakahara A,
Fukutomi H, Osuga T, Urushidani T, Miyauchi T and Goto K: Gastric
ulcer induced by submucosal injection of ET-1: Role of potent
vasoconstriction and intraluminal acid. Am J Physiol.
265:G491–G498. 1993.PubMed/NCBI
|
|
37
|
Michida T, Kawano S, Masuda E, Kobayashi
I, Nishimura Y, Tsujii M, Takei Y, Tsuji S, Nagano K, Fusamoto H,
et al: Endothelin-1 in the gastric mucosa in stress ulcers of
critically ill patients. Am J Gastroenterol. 92:1177–1181.
1997.PubMed/NCBI
|
|
38
|
Masuda E, Kawano S, Nagano K, Tsuji S,
Takei Y, Hayashi N, Tsujii M, Oshita M, Michida T, Kobayashi I, et
al: Role of endogenous endothelin in pathogenesis of
ethanol-induced gastric mucosal injury in rats. Am J Physiol.
265:G474–G481. 1993.PubMed/NCBI
|
|
39
|
Lloyd KC, Wang J, Aurang K, Grönhed P, Coy
DH and Walsh JH: Activation of somatostatin receptor subtype 2
inhibits acid secretion in rats. Am J Physiol. 268:G102–G106.
1995.PubMed/NCBI
|
|
40
|
Aurang K, Wang J and Lloyd K: Somatostatin
inhibition of acid and histamine release by activation of
somatostatin receptor subtype 2 receptors in rats. J Pharmacol Exp
Ther. 281:245–252. 1997.PubMed/NCBI
|
|
41
|
Martinez V, Curi AP, Torkian B, Schaeffer
JM, Wilkinson HA, Walsh JH and Taché Y: High basal gastric acid
secretion in somatostatin receptor subtype 2 knockout mice.
Gastroenterology. 114:1125–1132. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Saadé NE, Abdallah LE, Barada KA, Atweh SF
and Nassar CF: Effects of intracerebral injections of VIP on
jejunal alanine absorption and gastric acid secretion in rats.
Regul Pept. 55:269–276. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Nassar CF, Abdallah LE, Barada KA, Atweh
SF and Saadé NE: Effects of intravenous vasoactive intestinal
peptide injection on jejunal alanine absorption and gastric acid
secretion in rats. Regul Pept. 55:261–267. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Yoshikawa T, Ueda S, Naito Y, Takahashi S,
Oyamada H, Morita Y, Yoneta T and Kondo M: Role of oxygen-derived
free radicals in gastric mucosal injury induced by ischemia or
ischemia-reperfusion in rats. Free Radic Res Commun. 7:285–291.
1989. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Yoshikawa T, Naito Y, Ueda S, Oyamada H,
Takemura T, Yoshida N, Sugino S and Kondo M: Role of oxygen-derived
free radicals in the pathogenesis of gastric mucosal lesions in
rats. J Clin Gastroenterol. 12 Suppl 1:S65–S71. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Yoshikawa T, Naito Y, Kishi A, Tomii T,
Kaneko T, Iinuma S, Ichikawa H, Yasuda M, Takahashi S and Kondo M:
Role of active oxygen, lipid peroxidation, and antioxidants in the
pathogenesis of gastric mucosal injury induced by indomethacin in
rats. Gut. 34:732–737. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Itoh M and Guth PH: Role of oxygen-derived
free radicals in hemorrhagic shock-induced gastric lesions in the
rat. Gastroenterology. 88:1162–1167. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Jung HK, Lee KE, Chu SH and Yi SY:
Reactive oxygen species activity, mucosal lipoperoxidation and
glutathione in Helicobacter pylori-infected gastric mucosa. J
Gastroenterol Hepatol. 16:1336–1340. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Akiba Y, Nakamura M, Mori M, Suzuki H, Oda
M, Kimura H, Miura S, Tsuchiya M and Ishii H: Inhibition of
inducible nitric oxide synthase delays gastric ulcer healing in the
rat. J Clin Gastroenterol. 27 Suppl 1:S64–S73. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Rajnakova A, Goh PM, Chan ST, Ngoi SS,
Alponat A and Moochhala S: Expression of differential nitric oxide
synthase isoforms in human normal gastric mucosa and gastric cancer
tissue. Carcinogenesis. 18:1841–1845. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Barrachina M, Esplugues J, Martinezcuesta
M, Calatayud S, Bello R and Wittle B: Nitric-oxide donors
preferentially inhibit neuronally stimulated gastric-acid
secretion. Gastroenterology. 47:1994.
|
|
52
|
Takeuchi K, Ohuchi T and Okabe S:
Nitric-oxide mediates inhibition of gastric-acid secretion in the
damaged stomach-interaction with endogenous prostaglandins.
Gastroenterology. 1921994.
|
|
53
|
Ma L and Wallace JL: Endothelial nitric
oxide synthase modulates gastric ulcer healing in rats. Am J
Physiol Gastrointest Liver Physiol. 279:G341–G346. 2000.PubMed/NCBI
|
|
54
|
Guo JS, Cho CH, Wang WP, Shen XZ, Cheng CL
and Koo MW: Expression and activities of three inducible enzymes in
the healing of gastric ulcers in rats. World J Gastroenterol.
9:1767–1771. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Gambhir S, Vyas D, Hollis M, Aekka A and
Vyas A: Nuclear factor kappa B role in inflammation-associated
gastrointestinal malignancies. World J Gastroenterol. 21:3174–3183.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Yanai A, Maeda S, Shibata W, Hikiba Y,
Sakamoto K, Nakagawa H, Ohmae T, Hirata Y, Ogura K, Muto S, et al:
Activation of IKappaB kinase and NF-kappaB is essential for
Helicobacter pylori-induced chronic gastritis in Mongolian gerbils.
Infect Immun. 76:781–787. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Brzozowski T, Konturek SJ, Majka J,
Dembinski A and Drozdowicz D: Epidermal growth factor, polyamines,
and prostaglandins in healing of stress-induced gastric lesions in
rats. Dig Dis Sci. 38:276–283. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Konturek JW, Bielanski W, Konturek SJ,
Bogdal J and Oleksy J: Distribution and release of epidermal growth
factor in man. Gut. 30:1194–1200. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Reeves J, Richards R and Cooke T: The
effects of intracolonic EGF on mucosal growth and experimental
carcinogenesis. Br J Cancer. 63:223–226. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Challacombe DN and Wheeler EE: Trophic
action of epidermal growth factor on human duodenal mucosa cultured
in vitro. Gut. 32:991–993. 1991. View Article : Google Scholar : PubMed/NCBI
|