Introduction
Cervical spondylosis is the most common spine
disorder in the elderly (1). Certain
patients require anterior cervical fusion (ACF) surgery for
preventing any further impairment of neurological function. Due to
neck pain, cervical spine degeneration and cervical fusion,
numerous cervical spondylosis and ACF patients suffer from
limitations of cervical mobility (2,3) and
cannot maintain their life quality; this includes difficulty of
walking down stairs, washing their hair and driving cars. As an
important indicator of cervical disease and postoperative life
quality (4), the cervical range of
motion (CROM) is routinely measured by clinicians and researchers
to evaluate the cervical impairment, therapeutic effect and
residual disability.
However, due to the complex anatomy of the cervical
spine and the resulting coupled movement, it is challenging to
determine the CROM measurement accurately and reliably (5). At present, clinicians and researchers
utilize various devices to assess CROM. When raters use goniometry
(6), inclinometry (7), radiography (8) or a CROM device (9) for assessment, no continuous angles are
obtained, and scales require to be consulted or complex
calculations must be performed, which are sources of human error.
Furthermore, the CROM device cannot measure the pure CROM but
includes the trunk motion. As to electromagnetic motion analysis
(10), ultrasound motion analysis
(11) and optical motion analysis
(12), they do not achieve ‘good’
reliability and validity in all directions of CROM. Thus, no
optimal device for measuring CROM in clinical and research practice
is currently available.
The Cartesian Optoelectronic Dynamic Anthropometer
(CODA) motion analysis system (Charnwood Dynamics Ltd., Rothley,
UK) is a real-time three-dimensional kinematic analysis instrument.
This system has been employed in the analysis of gait posture
(13), lower and upper extremity
kinematics (14,15) and lumbar spine ROM (16) in various populations and
circumstances, and proved to be reliable and accurate. To the best
of our knowledge, it has not been applied in the assessment of
cervical mobility (17).
Considering the advantages of directly measuring the
CROM as well as the CODA motion system being accurate and reliable
in the analysis of other motions, the present study first applied
the system for measuring the CROM, evaluated the intra- and
inter-rater reliability and verified the construct validity of the
system to discriminate between cervical spondylosis and ACF
patients (known group construct validity).
Materials and methods
Subjects
A total of 26 patients with cervical spondylosis and
22 patients with ACF who presented at the Second Affiliated
Hospital of Xi'an Jiaotong University (Xi'an, China) between
September 2015 and September 2016 were enrolled in the present
study. The demographic data of patients was collected, and the
visual analogue scale (VAS) (18)
and Japanese Orthopaedic Association (JOA) score (19) were recorded. The patients of the
cervical spondylosis group were diagnosed with cervical spondylotic
radiculopathy or cervical spondylotic myelopathy by clinical
systems and magnetic resonance imaging examination. The patients of
the ACF group had received single- or multi-level anterior cervical
discectomy and fusion (ACDF) or anterior cervical corpectomy and
fusion (ACCF) due to cervical spondylosis, and solid cervical
fusion was confirmed by X-ray and computed tomography scan.
Informed consent forms were signed by all participants prior to
measurements and ethical approval was provided by the Ethical
Committee of Xi'an Jiaotong University (Xi'an, China).
Instruments
The CODA motion analysis system was used to collect
the cervical kinematic data. The system is composed of marker
devices, sensor modules and data analysis software. The marker
devices consist of infrared emission markers and drive boxes, which
are attached to the skin. The sensor modules are made up of three
optical sensors, which capture the vertical, horizontal and
rotational movements by tracking the markers' position in
real-time. The data analysis software, CODA motion ODIN, analyzes
the data from the sensor modules and records the three-dimensional
CROM. During the measurements of CROM, two sensor modules were
set-up at two diagonal sides of the test room, and three drive
boxes and seven markers were selected to capture the head, cervical
and thoracic movements. Marker 0 and marker 1 of drive box A were
attached to glabella and mental protuberance, respectively. Markers
0, 1 and 2 of drive box B were attached to the external occipital
protuberance, the seventh cervical vertebra (C7) and the eighth
thoracic vertebra, respectively. Markers 0 and 1 of drive box C
were attached to the incisure jugular and processus xiphoideus,
respectively (Fig. 1).
Procedures
A low-back chair was placed between two sensor
modules and the patients were requested to sit up facing one sensor
module. Their arms rested on the knees and their feet were kept
flat on the ground. The patients were required to wear swimming
caps to prevent interference of head hair. Prior to the
measurements, all patients performed three repetitions of cervical
motion in each direction as a warm-up. During the measurements, the
patients were required to move in the following order: Flexion,
extension, right lateral bending, left lateral bending, right axial
rotation and left axial rotation. They were also asked to move
their heads as much as possible in each direction without any
discomfort of the cervical spine, while the shoulders and trunk
were kept in a static position. At the end of each movement, the
patients remained static for 1 sec in case the sensor module missed
the signal, and then slowly returned to the neutral position.
Two orthopedics postgraduate students of Xi'an
Jiaotong University were selected as the testers (testers A and B).
They were provided with specific training of operating the CODA
motion analysis system prior to the study. The CROM of each patient
was measured with three repetitions, two of which were performed by
tester A (A1, A2) and the other one by tester B (B1). There was a
1-week interval between A1 and A2, and A2 was be performed at the
same time of day as A1 to reduce the influence of diurnal
variation. B1 was performed on the same day as A1 with a 20-min
interval between the two testers, and tester B was blinded to the
previous measurements. The intra-rater reliability was evaluated
from the results of A1 and A2, and inter-rater reliability was
evaluated from the results of A1 and B1.
Statistical analysis
All statistical analyses were performed by using
SPSS 19.0 software (IBM Corp., Armonk, NY, USA). All data were
proved to be normally distributed by the Kolmogorov-Smirnov test
and thus, to assess the differences between groups, independent
samples t-tests were performed. The characteristics of patients
were described as the mean ± standard deviation (SD).
The reliability of the measurements in cervical
spondylosis and ACF patients was calculated. Intra- and inter-rater
reliability was assessed by determining the intraclass correlation
coefficient (ICC) with 95% confidence intervals (95% CI). The
one-way random model was used to calculate the ICC for intra-rater
reliability, and the two-way random model was used for inter-rater
reliability. Standard error of measurement (SEm) was calculated as
SDx√1-ICC, where SD refers to the SD of the combined values of two
tests (20). The minimal detectable
change (MDC) was calculated for a 95% confidence level, and the
formula is MDC=1.96×√2 SEm (21).
Limits of agreements (LOA) were calculated as the mean
difference±1.96 SD of the differences (22). Bland-Altman plots were also generated
to display the graphical differences between the measurements of
two tests (22). According to the
categorization of Shrout (23), an
ICC value of >0.8 was considered as highly reliable.
To verify the known group construct validity
(24), an independent samples t-test
was performed to examine the differences in CROM between cervical
spondylosis and ACF patients, and the value of CROM in each
direction was calculated as the average value of A1, A2 and B1.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Subjects
The characteristics of the patients in the cervical
spondylosis and ACF groups are displayed in Table I. The cervical spondylosis group was
composed of 26 subjects, and the clinical diagnoses of patients
included myelopathy, radiculopathy or both. The ACF group was
composed of 22 subjects and the surgical options included one- or
two-level ACDF and one- or two-level ACCF. The mean follow-up time
in the ACF group was 6.7±2.1 months. The differences in sex
distribution and age between the groups were not significant.
However, significant differences in VAS score and JOA score were
identified between the two groups.
 | Table I.Characteristics of patients. |
Table I.
Characteristics of patients.
| Parameter | Cervical spondylosis
(n=26) | Anterior cervical
fusion (n=22) | P-value |
|---|
| Sex
(female/male) | 12/14 | 13/9 | 0.37 |
| Age (years) | 55.8±12.5 | 56.8±11.3 | 0.26 |
| Diagnosis |
|
|
|
|
Myelopathy | 13 | N/A | N/A |
|
Radiculopathy | 8 | N/A | N/A |
|
Mixed | 4 | N/A | N/A |
| Surgical
option |
|
|
|
|
One-level ACDF | N/A | 4 | N/A |
|
Two-level ACDF | N/A | 6 | N/A |
|
One-level ACCF | N/A | 6 | N/A |
|
Two-level ACCF | N/A | 6 | N/A |
| VAS score | 6.3±1.3 | 2.3±0.8 | <0.001 |
| JOA score | 10.3±1.7 | 14.2±1.4 | <0.001 |
Reliability study on the cervical
spondylosis group
The mean CROM as well as the ICC (95% CI), LOA, SEm
and MDC according to the intra- and inter-rater reliability study
are displayed in Table II. The ROM
in lateral bending ranked lowest, following the extension/flexion,
and the axial rotation ranked highest according to the intra- as
well as the inter-rater analysis. The ICC values according to the
intra-rater reliability analysis, ranging from 0.87 (flexion) to
0.95 (right axial rotation), were slightly better than those
according to the inter-rater reliability analysis, which ranged
from 0.84 (flexion) to 0.95 (right axial rotation), indicating a
high level of reliability. The LOA ranged from −12.86 to 13.70 and
−13.09 to 13.48 according to the intra- and inter-rater analysis,
respectively. The SEm according to the intra- and inter-rater
reliability analysis was similar, ranging from 2.97 to 4.58 and
3.13 to 4.32, respectively. The MDC ranged from 8.23 to 12.69
according to the intra-rater analysis and from 8.67 to 11.97
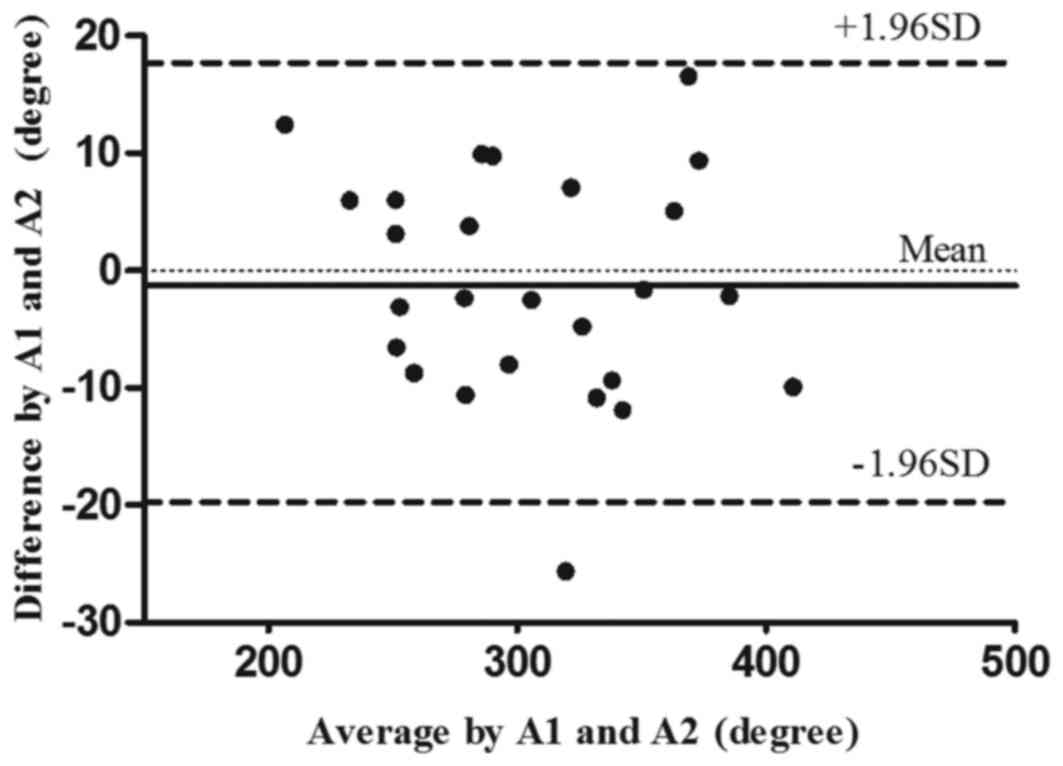
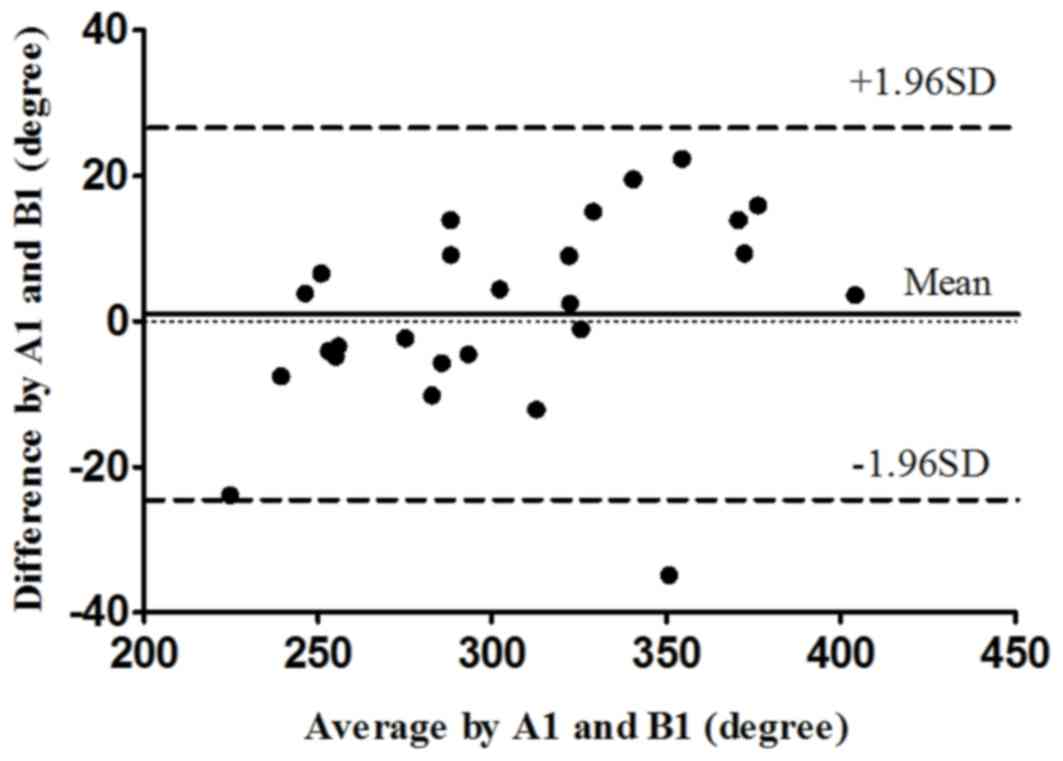
according to the inter-rater analysis. Figs. 2 and 3
display the intra- and inter-rater LOA plots for total CROM in the
cervical spondylosis group, respectively.
 | Table II.Mean ROM and reliability statistics
for the cervical spondylosis group. |
Table II.
Mean ROM and reliability statistics
for the cervical spondylosis group.
|
| Intra-rater
study | Inter-rater
study |
|---|
|
|
|
|
|---|
| Direction | Mean (SD) | ICC (95%CI) | LOA | SEm | MDC | Mean (SD) | ICC (95%CI) | LOA | SEm | MDC |
|---|
| Flexion | 49.61 (9.52) | 0.87
(0.73–0.94) | −10.42,9.20 | 3.43 | 9.50 | 48.00 (9.75) | 0.84
(0.67–0.92) | −8.26,13.48 | 3.90 | 10.80 |
| Extension | 47.75 (13.22) | 0.88
(0.75–0.94) | −12.86,13.70 | 4.58 | 12.69 | 48.19 (12.45) | 0.89
(0.76–0.95) | −12.3,11.37 | 4.13 | 11.44 |
| Right lateral
bending | 39.49 (13.81) | 0.94
(0.88–0.97) | −8.15,9.31 | 3.38 | 9.36 | 39.06 (12.40) | 0.92
(0.82–0.96) | −8.61,11.49 | 3.51 | 9.72 |
| Left lateral
bending | 40.84 (14.89) | 0.93
(0.86–0.97) | −11.55,10.42 | 3.94 | 10.91 | 41.66 (13.58) | 0.92
(0.84–0.97) | −12.30,7.89 | 3.84 | 10.64 |
| Right axial
rotation | 65.69 (13.30) | 0.95
(0.89–0.98) | −8.28,9.23 | 2.97 | 8.23 | 65.34 (14.02) | 0.95
(0.89–0.98) | −7.49,9.84 | 3.13 | 8.67 |
| Left axial
rotation | 62.51 (13.21) | 0.91
(0.81–0.96) | −12.41,9.57 | 3.96 | 10.97 | 62.39 (13.02) | 0.89
(0.78–0.95) | −13.09,10.70 | 4.32 | 11.97 |
| Total CROM | 305.88 (51.46) | 0.98
(0.96–0.99) | −19.92,17.69 | 7.28 | 20.17 | 305.79 (49.37) | 0.96
(0.92–0.98) | −24.20,26.93 | 9.87 | 27.34 |
Reliability study on the ACF
group
The mean CROM as well as the ICC (95% CI), LOA, SEm
and MDC according to the intra- and inter-rater reliability
analysis are displayed in Table
III. The highest ROM was in the axial rotation direction and
the lowest ROM was in the lateral bending direction according to
the intra- as well as the inter-rater analysis. The ICC values
ranged from 0.88 (extension) to 0.97 (right axial rotation)
according to the intra-rater analysis and 0.86 (extension) to 0.96
(right lateral bending) according to the inter-rater analysis,
revealing almost perfect reliability. According to the intra-rater
analysis, the LOA ranged from −10.65 to 11.08, the SEm ranged from
2.10 to 3.77 and the MDC ranged from 5.82 to 10.44. Similar to the
inter-rater analysis results, the LOA ranged from −10.91 to 13.66,
the SEm ranged from 2.20 to 4.45 and the MDC ranged from 6.09 to
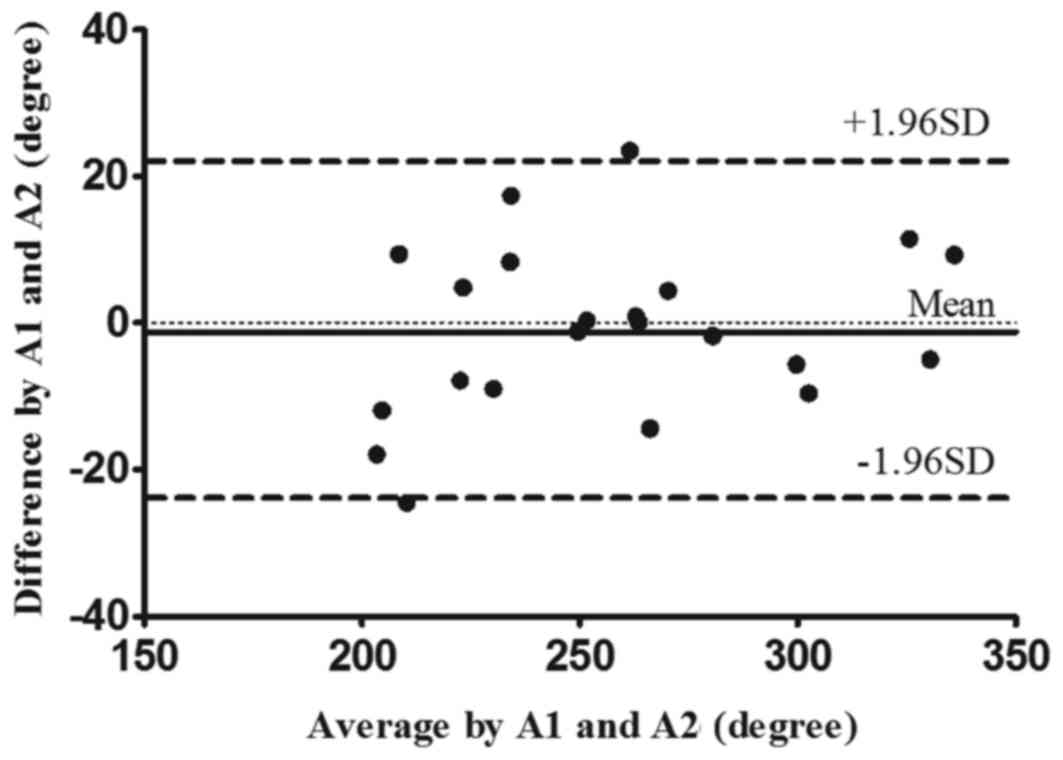
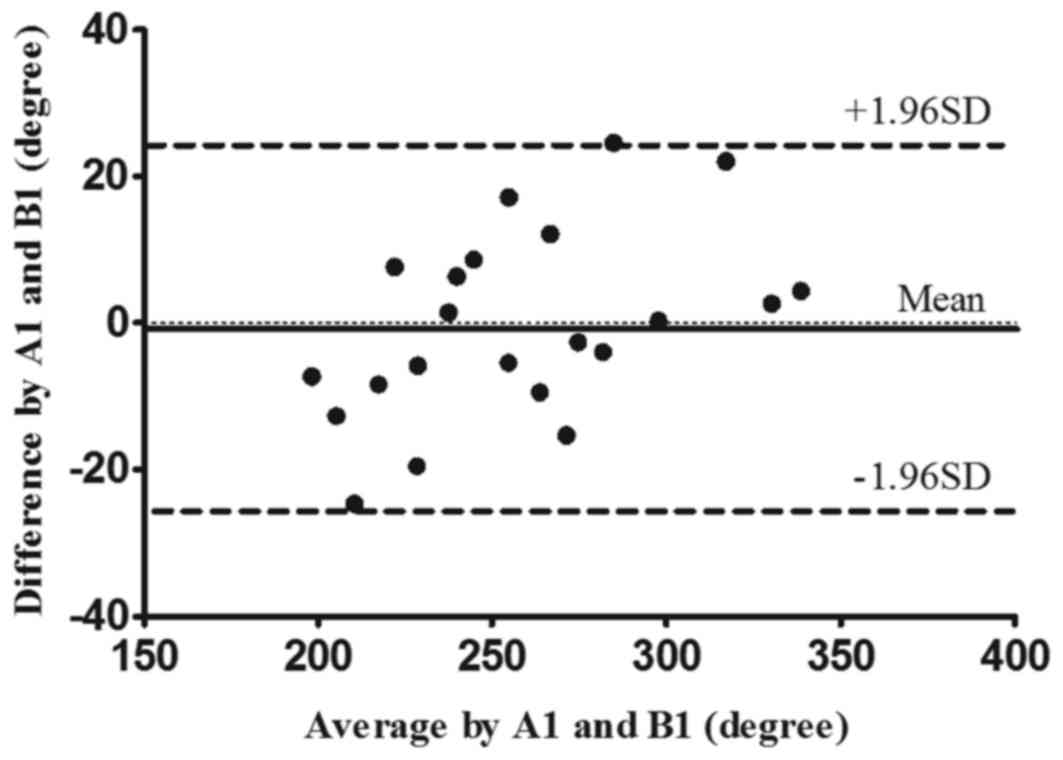
12.33. Figs. 4 and 5 display the intra- and inter-rater LOA
plots for the total CROM in the ACF group, respectively.
 | Table III.Mean ROM and reliability statistics
for the anterior cervical fusion group. |
Table III.
Mean ROM and reliability statistics
for the anterior cervical fusion group.
|
| Intra-rater
study | Inter-rater
study |
|---|
|
|
|
|
|---|
| Direction | Mean (SD) | ICC (95%CI) | LOA | SEm | MDC | Mean (SD) | ICC (95%CI) | LOA | SEm | MDC |
|---|
| Flexion | 40.40 (10.84) | 0.91
(0.81–0.96) | −9.57,8.65 | 3.25 | 9.00 | 40.63 (9.45) | 0.89
(0.75–0.95) | −9.87,8.04 | 3.13 | 8.67 |
| Extension | 40.06 (9.43) | 0.88
(0.73–0.95) | −10.07,8.74 | 3.27 | 9.06 | 39.76 (8.74) | 0.86
(0.70–0.94) | −9.18,9.06 | 3.27 | 9.06 |
| Right lateral
bending | 31.44 (9.67) | 0.95
(0.88–0.98) | −4.59,7.16 | 2.16 | 5.98 | 32.62 (10.98) | 0.96
(0.92–0.99) | −6.92,4.76 | 2.20 | 6.09 |
| Left lateral
bending | 33.00 (9.16) | 0.92
(0.81–0.96) | −7.10,7.94 | 2.59 | 7.17 | 32.84 (8.49) | 0.90
(0.78–0.96) | −6.69,8.17 | 2.68 | 7.42 |
| Right axial
rotation | 55.75 (12.12) | 0.97
(0.93–0.99) | −6.94,3.67 | 2.10 | 5.82 | 55.13 (11.01) | 0.93
(0.84–0.97) | −8.54,7.72 | 2.91 | 8.06 |
| Left axial
rotation | 57.23 (13.33) | 0.92
(0.82–0.97) | −10.65,11.08 | 3.77 | 10.44 | 56.65 (12.85) | 0.88
(0.74–0.95) | −10.91,13.66 | 4.45 | 12.33 |
| Total CROM | 257.88 (41.02) | 0.96
(0.91–0.98) | (−23.57,21.88) | 8.2 | 22.71 | 257.63 (39.59) | 0.95
(0.88–0.98) | (−25.35,24.64) | 8.85 | 24.51 |
Construct validity
The inter-group differences in CROM are displayed in
Table IV. The CROM regarding
flexion, extension, right lateral bending, left lateral bending and
right axial rotation in the ACF group was significantly lower than
that in the cervical spondylosis group (P≤0.041), and a trend
towards a lower ROM in left axial rotation was also noted in the
ACF group, but the difference between groups was not significant
(P=0.120).
 | Table IV.Differences in CROM between cervical
spondylosis and anterior cervical fusion group. |
Table IV.
Differences in CROM between cervical
spondylosis and anterior cervical fusion group.
| Direction | Cervical
spondylosis group | Anterior cervical
fusion group | P-value |
|---|
| Flexion | 47.4±9.3 | 40.6±9.6 | 0.005 |
| Extension | 48.0±12.6 | 39.9±8.4 | 0.015 |
| Right lateral
bending | 39.1±12.7 | 32.0±10.3 | 0.041 |
| Left lateral
bending | 41.5±13.9 | 32.8±8.6 | 0.015 |
| Right axial
rotation | 65.4±13.4 | 55.6±11.3 | 0.010 |
| Left axial
rotation | 62.7±13.8 | 56.8±12.7 | 0.120 |
| Total CROM | 305.1±51.1 | 257.5±40.3 | 0.012 |
Discussion
Numerous instruments have been used for the
measurement of CROM, but they may cause human error due to the
inclusion of trunk motion or the requirement for a tester to read
the scale (8–10). Therefore, a ‘better’ approach should
be identified to measure cervical mobility in clinical and research
applications. In addition, most studies are currently focused on
measuring the ROM of healthy people or patients with neck pain
(7,17,25),
while the reliability of the measurements among cervical
spondylosis and cervical fusion patients has remained to be
determined. The CODA motion analysis system has not been used for
measuring CROM, but has been reported to reliably and accurately
evaluate the ROM of other joints under different circumstances
(15,16). To the best of our knowledge, the
present study was the first to apply this system for measuring
cervical mobility and proved to be highly reliable in determining
the CROM. Besides, the construct validity was verified because the
system was sensitive enough to distinguish the CROM between
cervical spondylosis and ACF group.
As an important indicator of cervical function, the
three-dimensional CROM of cervical spondylosis patients has been
assessed by various devices in previous studies. Dvir et al
(26) utilized the Zebris system to
assess the ROM of patients with cervical degenerative disease, the
results were 82.5 for flexion-extension, 65.3 for lateral bending,
and 103.9 for axial rotation. Yuan et al (4) used the CROM device to measure the ROM
of patients with cervical myelopathy, and the results were 90.2 for
flexion-extension, 83.2 for lateral bending and 114 for axial
rotation. The CROM of ACF patients was also assessed using other
methods. Cattrysse et al (27) used the electromagnetic tracking
system to assess the ROM of patients who received ACF, and the
results were 46.94–66.87 for lateral bending and 95.81–112.59 for
axial rotation. Bell et al (28) used a virtual reality-assisted
cervical motion tracking device (VR-assisted CMTD) to assess the
ROM of patients who received ACDF, and the ROM was 67.2–89.7 for
flexion-extension, 39.2–65.8 for lateral bending and 83.3–111.7 for
axial rotation. In the present study, the CODA motion analysis
system was utilized to measure the three-dimensional CROM of
cervical spondylosis and ACF patients. Comparison of the present
results with those of the previous studies indicated that in the
cervical spondylosis group, the CODA motion analysis system was
able to obtain a similar ROM to that determined by the CROM device
and Zebris system, and in the ACF group, it determined a similar
ROM to that obtained with an electromagnetic tracking system and
VR-assisted CMTD. The similarity of the ROM assessed by various
devices proved that the CODA motion analysis system is able to
accurately measure the three-dimensional CROM.
Most previous studies only used ICC to assess the
reliability of devices, which greatly reduced the credibility of
their results (25,29). The present study comprehensively
evaluated the reliability of the CODA motion analysis system by
calculating ICC, LOA, SEm and MDC. The intra- and inter-rater ICCs
in the cervical spondylosis group were 0.87–0.95 and 0.84–0.95,
respectively. The intra- and inter-rater ICCs in the cervical
fusion group were 0.88–0.97 and 0.86–0.96, respectively. Therefore,
the reliability of the CODA motion analysis system was sufficiently
high to render it suitable for use in clinical and research
settings for the measurement of CROM in all directions. Various
studies have also assessed the reliability of other devices among
individuals with cervical disorders. Williams et al
(9) assessed the reliability of the
CROM device among cervical whiplash patients and obtained ICC
values of 0.98–0.99 for intra-rater reliability and 0.82–0.92 for
inter-rater reliability. Dvir et al (26) evaluated the reliability of the Zebris
system for patients with degenerative changes, and the ICCs for
intra-rater reliability were in the range of 0.80–0.89. Law and
Chiu (25) assessed the reliability
of the Electronic CROM Goniometer among patients with neck pain,
and the ICCs for inter-rater reliability ranged from 0.81 to 0.92.
In comparison with that of the other devices, the reliability of
the CODA motion analysis system was equal or superior.
In the present study, almost all ICCs of flexion and
extension were <0.90, which was lower than that of the other
four directions. During the measurements, the marker attached to
the incisure jugular was probably obscured by the jaw during the
flexion, while during the extension, the marker attached to the
occipital protuberance was likely obscured by the wrinkle of the
neck skin. This obscuring effect may have resulted in the lower
ICCs of flexion and extension. Furthermore, the ICCs of almost all
directions in the cervical spondylosis group (range, 0.84–0.95)
were lower than those in the cervical fusion group (range,
0.86–0.97). One possible explanation is that the lower CROM in the
cervical fusion group may reduce the obscuring of the markers,
which is beneficial for achieving higher ICCs.
The calculation of the MDC value is essential in
assessing the reliability of a novel device. In the cervical
spondylosis group, MDCs were 8.23–12.69 for intra-rater
reliability, and 8.67–11.97 for inter-rater reliability. In the ACF
group, the MDCs were 5.82–10.44 for intra-rater reliability and
6.09–12.33 for inter-rater reliability. MDC values for CROM have
also been reported in previous studies. Shahidi et al
(30) used a gravity inclinometer to
measure CROM and the MDC ranged from 9 to 21 regarding inter-rater
reliability. The lower MDCs in the present study indicated that the
CODA motion analysis system is sensitive in detecting small changes
in three-dimensional CROM. Therefore, the system is adequate to be
applied in clinical and research practices.
The assessment of construct validity was performed
by comparing the three-dimensional CROM between cervical
spondylosis and ACF groups. The results revealed that the CROM in
the cervical spondylosis group was significantly higher than that
in the ACF group in all directions except for left rotation,
supporting the ability of the CODA motion analysis system to
discriminate between cervical spondylosis and ACF patients. The
lower CROM for the ACF group was in agreement with the results of
studies (31–33). These studies often calculated the
C2-7 ROM of flexion and extension by lateral radiographs. In a
study by Lee et al (31), an
increase in the C0-2 ROM was observed after ACF, although the
difference was not significant. However, the results of
three-dimensional studies were contrary to the above. The study by
Bell et al (28) revealed
that the postoperative CROM in the 1-or 2-level ACDF group was
higher than the preoperative one. A study by Landers et al
(34) revealed that the CROM
increased significantly after ACDF regardless of the number of
levels fused. The reason for the difference in results between
these studies may be attributed to the compensation of the C0-2
ROM, the options of anterior fusion methods and the number of fused
levels. Due to the conflicting results regarding CROM after ACF,
the study of three-dimensional motion of the cervical spine is
gaining importance. In the present study, although the left
rotation ROM in the cervical spondylosis group was higher than that
in the ACF group, the difference between the groups was not
significant. One possible reason for the equal results regarding
left rotation may be that the rotation of the cervical spine is
mainly performed by the upper cervical spine, particularly C1 and
C2 (35,36), while anterior fusion surgery is often
performed between C3 and C7, and the ROM of rotation may thus be
less influenced by the surgery.
The present study had two limitations. First, the
markers are not stationary with respect to the underlying bone due
to the soft tissue between the markers and the bone landmarks.
Therefore, the system may not be suitable for measuring the ROM of
obese patients, since the soft tissue may be thicker. Furthermore,
the system is expensive, which may limit its application in
clinical practice. However, taking into account its various uses,
such as assessing gait posture (13), lower and upper extremity kinematics
(14,15) and lumbar spine ROM, the high price
may not restrict its application in clinical practice.
In conclusion, the present study confirmed the high
reliability of the CODA motion analysis system in the measurement
of CROM among cervical spondylosis and ACF patients. The construct
validity of the CODA motion analysis system was verified, as the
system was sufficiently sensitive to distinguish between cervical
spondylosis and ACF based on the CROM.
References
|
1
|
Takagi I, Eliyas JK and Stadlan N:
Cervical spondylosis: An update on pathophysiology, clinical
manifestation, and management strategies. Dis Mon. 57:583–591.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nagamoto Y, Ishii T, Sakaura H, Iwasaki M,
Moritomo H, Kashii M, Hattori T, Yoshikawa H and Sugamoto K: In
vivo three-dimensional kinematics of the cervical spine during head
rotation in patients with cervical spondylosis. Spine (Phila Pa
1976). 36:778–783. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Miyazaki M, Hong SW, Yoon SH, Zou J, Tow
B, Alanay A, Abitbol JJ and Wang JC: Kinematic analysis of the
relationship between the grade of disc degeneration and motion unit
of the cervical spine. Spine (Phila Pa 1976). 33:187–193. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yuan W, Zhu Y, Liu X, Zhu H, Zhou X, Zhou
R, Cui C and Li J: Postoperative three-dimensional cervical range
of motion and neurological outcomes in patients with cervical
ossification of the posterior longitudinal ligament: Cervical
laminoplasty versus laminectomy with fusion. Clin Neurol Neurosurg.
134:17–23. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bogduk N and Mercer S: Biomechanics of the
cervical spine I: Normal kinematics. Clin Biomech (Bristol, Avon).
15:633–648. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Maksymowych WP, Mallon C, Richardson R,
Conner-Spady B, Jauregui E, Chung C, Zappala L, Pile K and Russell
AS: Development and validation of a simple tape-based measurement
tool for recording cervical rotation in patients with ankylosing
spondylitis: Comparison with a goniometer-based approach. J
Rheumatol. 33:2242–2249. 2006.PubMed/NCBI
|
|
7
|
Lachtman DS, Bartha DA, Beltran MM,
Dominguez DN, Messerli AR, Miller SE, Davis AM and Nelson-Wong E:
Rater reliability and concurrent validity of single and dual bubble
inclinometry to assess cervical lateral flexion. J Manipulative
Physiol Ther. 38:572–580. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dvorák J, Panjabi MM, Grob D, Novotny JE
and Antinnes JA: Clinical validation of functional
flexion/extension radiographs of the cervical spine. Spine (Phila
Pa 1976). 18:120–127. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Williams MA, Williamson E, Gates S and
Cooke MW: Reproducibility of the cervical range of motion (CROM)
device for individuals with sub-acute whiplash associated
disorders. Eur Spine J. 21:872–878. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jordan K, Dziedzic K, Jones PW, Ong BN and
Dawes PT: The reliability of the three-dimensional FASTRAK
measurement system in measuring cervical spine and shoulder range
of motion in healthy subjects. Rheumatology (Oxford). 39:382–388.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Cagnie B, Cools A, De Loose V, Cambier D
and Danneels L: Reliability and normative database of the Zebris
cervical range-of-motion system in healthy controls with
preliminary validation in a group of patients with neck pain. J
Manipulative Physiol Ther. 30:450–455. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bulgheroni MV, Antonaci F, Ghirmai S,
Sandrini G, Nappi G and Pedotti A: A 3D kinematic method for
evaluating voluntary movements of the cervical spine in humans.
Funct Neurol. 13:239–245. 1998.PubMed/NCBI
|
|
13
|
Exell TA, Gittoes MJ, Irwin G and Kerwin
DG: Gait asymmetry: Composite scores for mechanical analyses of
sprint running. J Biomech. 45:1108–1111. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Delahunt E, Cusack K, Wilson L and Doherty
C: Joint mobilization acutely improves landing kinematics in
chronic ankle instability. Med Sci Sports Exerc. 45:514–519. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Levanon Y, Gefen A, Lerman Y, Givon U and
Ratzon NZ: Validity and reliability of upper extremity
three-dimensional kinematics during a typing task. Gait Posture.
32:469–474. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
O'Sullivan K, Clifford A and Hughes L: The
reliability of the CODA motion analysis system for lumbar spine
analysis: A pilot study. Physiotherapy Pract Res. 31:16–22.
2010.
|
|
17
|
Williams MA, McCarthy CJ, Chorti A, Cooke
MW and Gates S: A systematic review of reliability and validity
studies of methods for measuring active and passive cervical range
of motion. J Manipulative Physiol Ther. 33:138–155. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Price DD, McGrath PA, Rafii A and
Buckingham B: The validation of visual analogue scales as ratio
scale measures for chronic and experimental pain. Pain. 17:45–56.
1983. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Fukui M, Chiba K, Kawakami M, Kikuchi S,
Konno S, Miyamoto M, Seichi A, Shimamura T, Shirado O, Taguchi T,
et al: Japanese orthopaedic association cervical myelopathy
evaluation questionnaire (JOACMEQ): Part 2. Endorsement of the
alternative item. J Orthop Sci. 12:241–248. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Stratford PW and Goldsmith CH: Use of the
standard error as a reliability index of interest: An applied
example using elbow flexor strength data. Phys Ther. 77:745–750.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Beaton DE, Bombardier C, Katz JN and
Wright JG: A taxonomy for responsiveness. J Clin Epidemiol.
54:1204–1217. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bland JM and Altman DG: Agreed statistics:
Measurement method comparison. Anesthesiology. 116:182–185. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Shrout PE: Measurement reliability and
agreement in psychiatry. Stat Methods Med Res. 7:301–317. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Nussbaumer S, Leunig M, Glatthorn JF,
Stauffacher S, Gerber H and Maffiuletti NA: Validity and
test-retest reliability of manual goniometers for measuring passive
hip range of motion in femoroacetabular impingement patients. BMC
Musculoskelet Disord. 11:1942010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Law EY and Chiu TT: Measurement of
cervical range of motion (CROM) by electronic CROM goniometer: A
test of reliability and validity. J Back Musculoskelet Rehabil.
26:141–148. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Dvir Z, Gal-Eshel N, Shamir B, Prushansky
T, Pevzner E and Peretz C: Cervical motion in patients with chronic
disorders of the cervical spine: A reproducibility study. Spine
(Phila Pa 1976). 31:E394–E399. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Cattrysse E, Moens M, Schaillée E, D'Haens
J and Van Roy P: Changed cervical kinematics after fusion surgery.
Eur Spine J. 21:1353–1359. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Bell KM, Bechara BP, Hartman RA, Shively
C, Frazier EC, Lee JY, Kang JD and Donaldson WF: Influence of
number of operated levels and postoperative time on active range of
motion following anterior cervical decompression and fusion
procedures. Spine (Phila Pa 1976). 36:263–268. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Quek J, Brauer SG, Treleaven J, Pua YH,
Mentiplay B and Clark RA: Validity and intra-rater reliability of
an android phone application to measure cervical range-of-motion. J
Neuroeng Rehabil. 11:652014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Shahidi B, Johnson CL, Curran-Everett D
and Maluf KS: Reliability and group differences in quantitative
cervicothoracic measures among individuals with and without chronic
neck pain. BMC Musculoskelet Disord. 13:2152012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Lee SH, Lee JC, Tauchi R and Daniel Riew
K: Influence of the number of cervical fusion levels on cervical
spine motion and health-related quality of life. Spine (Phila Pa
1976). 41:E474–E480. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chien A, Lai DM, Wang SF, Cheng CH, Hsu WL
and Wang JL: Differential segmental motion contribution of single-
and two-level anterior cervical discectomy and fusion. Eur Spine J.
24:2857–2865. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Mao N, Wu J, Zhang Y, Gu X, Wu Y, Lu C,
Ding M, Lv R, Li M and Shi Z: A comparison of anterior cervical
corpectomy and fusion combined with artificial disc replacement and
cage fusion in patients with multilevel cervical spondylotic
myelopathy. Spine (Phila Pa 1976). 40:1277–1283. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Landers MR, Addis KA, Longhurst JK, Vom
Steeg BL, Puentedura EJ and Daubs MD: Anterior cervical
decompression and fusion on neck range of motion, pain and
function: A prospective analysis. Spine J. 13:1650–1658. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Takasaki H, Hall T, Oshiro S, Kaneko S,
Ikemoto Y and Jull G: Normal kinematics of the upper cervical spine
during the Flexion-Rotation Test-In vivo measurements using
magnetic resonance imaging. Man Ther. 16:167–171. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Rudolfsson T, Björklund M and Djupsjöbacka
M: Range of motion in the upper and lower cervical spine in people
with chronic neck pain. Man Ther. 17:53–59. 2012. View Article : Google Scholar : PubMed/NCBI
|