Introduction
Accessory spleens (AS), also known as supernumerary
spleen, splenules or splenunculi, are commonly accepted as
congenital abnormalities due to the failing of fusion of the
splenic primordium, originating from the left side of the dorsal
mesogastrium during the initial phases of fetal life (1). Although AS affects 10–30% of the
population (2), its pre-operative
diagnosis by gynecologists is challenging due to the rare incidence
of AS located in the pelvis and the asymptomatic pattern of its
manifestation. The present study reports on the case of a pelvic
multiple AS appearing in the para-uterus and the junction between
the double sacral ligament and the posterior wall of the cervix but
no presence of any adnexal mass. The literature was also reviewed
by retrieving and summarizing studies on pelvic AS from the past 30
years. To the best of our knowledge, no previous study has
comprehensively described multiple AS occurring in the pelvis as
well as its differential diagnoses of gynecological diseases.
Case report
A 39-year-old woman with sudden abdominal pain for
one week presented at the Department of Gynaecology, Tongji
Hospital (Wuhan, China) in July 2017. She had a big pelvic mass
behind the uterine that had been incidentally detected during a
routine ultrasound scan test two months ago, but no adnexal mass
was identified. Laboratory tests indicated no abnormality, and
tumor bio-markers cancer antigen (CA)125, α-fetoprotein and
carcinoembryonic antigen (CEA) were within normal limits.
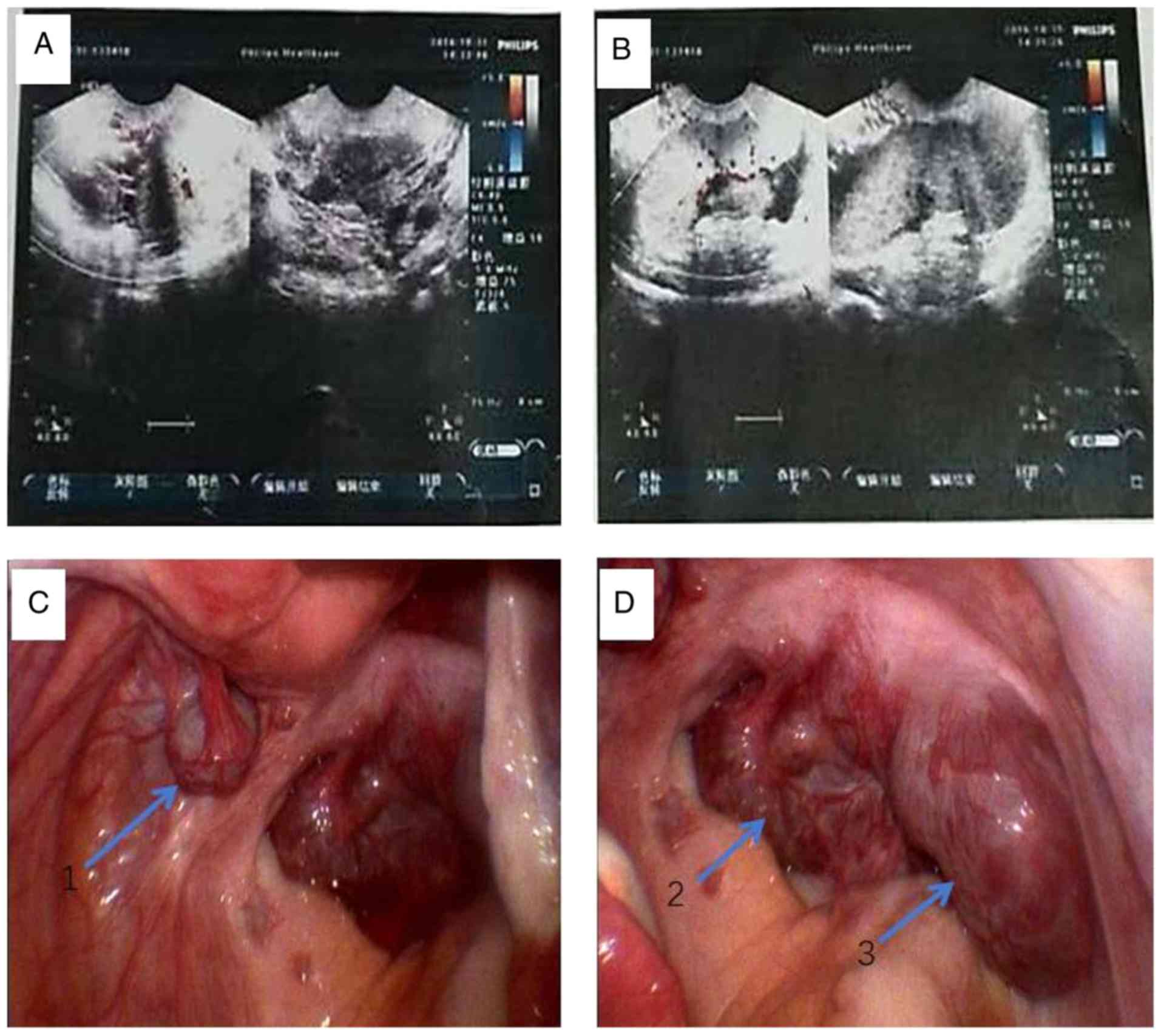
Transvaginal color doppler ultrasonography revealed a post-uterine
mass with a maximum diameter of 73 mm, which presented a
homogeneously hypoechoic pattern and demonstrated no pathological
blood flow (Fig. 1A and B). The
patient's medical history revealed no surgery of the spleen due to
any upper abdominal trauma.
Due to the sudden abdominal pain and the big pelvic
mass, a laparotomy was performed under general anesthesia by
non-invasive procedures in order to reveal the nature of the pelvic
mass and to rule out the suspected diagnosis of pelvic neoplasm or
gastrointestinal tumor. Inspection of the pelvis revealed multiple
solid and firm tumors with a smooth surface of 2–8 cm in diameter.
Apart from a 2-cm diameter kermesinus and pediculated mass next to
the left posterior wall of the uterus, 2 further big masses of ~8
cm in diameter, located next to the junction between the bilateral
utero-sacral ligament and the posterior wall of the cervix, were
present (Fig. 1C and D). There was
no adhesion to the surrounding structures. The bilateral salpinx,
ovary and the uterus were normal on inspection. The mass next to
the left posterior wall of the uterus was resected, following which
the vascular peduncle was isolated and ligated during an open
surgery. Pathological examination of the resected specimens
revealed splenic tissue. Post-operative recovery was
uneventful.
Discussion
AS refers to one or more ectopic splenic tissue
masses with a similar structure and the same endothelial function
to that of the spleen, which is in turn present in its normal
position. In the clinic, AS is detected incidentally and has no
clinical manifestation or causes slight discomfort in most
patients. AS is present in 10–30% of the general population
according to an autopsy-based study (3). In atypical cases, the pre-operative
diagnosis of AS is difficult. To date, the only reported case of a
large pelvic AS was that of a juvenile female with a wandering
congestive mass (13×8×7 cm) with a tortuous vascular pedicle that
originated along the dorsal aspect of the greater omentum situated
in the cul-de-sac (4). The present
study reported on another case of a pelvic large AS in a
39-year-old woman presenting with multiple solid masses.
Ectopic splenic tissue may be either congenital (AS
or splenunculi) or acquired (splenosis). Splenosis is the
auto-transplantation of splenic tissue during splenectomy or
following trauma (5). The patient of
the present study had no history of trauma or splenectomy. AS is a
congenital defect defined as additional ectopic splenic parenchyma
(2). The size of the AS ranges from
microscopic to 4.5 cm in diameter, as observed in previously
reported cases (2,6,7). The
mean age of cases is 20–40 years according to one study (6), while the youngest reported case was 17
years (4,8) and the oldest was 67 years (9). The localization varies widely, but the
most common locations are the splenic hilum (75%) or the pancreas
tail (20%). They may infrequently be located in the greater
omentum, mesenterium, adnexal region, the pouch of Douglas, the
obturator fossa and retroperitoneal area, as well as the pelvic
cavity (2,10). Unver Dogan et al (11) investigated 720 autopsy cases, among
which AS was present in 6.7% of cases, 2 of which were pelvic AS.
The common presentation is that of a single AS (85%), although 20
(14%) and rarely ≥3 (1%) may also be observed (5).
AS located in the pelvis (named as pelvic AS) is not
frequently seen. Multiple pelvic AS is defined as two or more
pelvic AS located to the left broad ligament and the pouch of
Douglas or the obturator fossa except for the adnexal region. A
total of 6 differences prevail between multiple pelvic AS and
single pelvic AS (Table I). Pelvic
AS may be divided into two conditions: One is the wandering spleen,
which is a separate entity, resulting from an elongation or a
defect due to the incomplete development of the ligamentous splenic
apparatus, which is caused by congenital defects during dorsal
mesogastrium development or by acquired defects, such as abdominal
wall laxity, which allow the spleen to migrate within the abdomen
(6). The other condition is
splenosis, which is an acquired abnormality relevant to heterotopic
auto-transplantation of splenic tissue following abdominal trauma
or splenectomy (7). According to the
literature in English language of the past 30 years (from 1987 to
2017) retrieved online from PubMed (https://www.ncbi.nlm.nih.gov/pubmed/), only 16 cases
of pelvic AS have been reported, to the best of our knowledge
(2,4–10,12–19).
 | Table I.The differences between multiple
pelvic AS and single pelvic AS. |
Table I.
The differences between multiple
pelvic AS and single pelvic AS.
| Characteristic | Multiple pelvic
AS | Single pelvic AS |
|---|
| Quantity | ≥2 | 1 |
| Frequency of the
position | Left broad ligament
and Douglas or obturator fossa | Adnexal region |
| Incidence | Extremely rare | Rare |
| Clinical features
during medical detection or operation | Multiple masses | Single mass |
| Diagnosis | Difficult | Easy |
| Differential
diagnosis | Difficult to
some | Difficult |
Although most patients with pelvic AS are
asymptomatic, symptomatic pelvic AS rarely presents clinically as
an abdominal mass causing complications, including torsion,
spontaneous rupture, hemorrhage or cyst formation (6–8,13,16).
Torsion and ischemia of pelvic AS may lead to acute abdomen
(13,16). When the AS is located in the adnexal
area, the differential diagnoses of this adnexal solid mass
comprise the different causes of adnexal masses, including enlarged
lymph nodes, sub-serous fibroid, ovarian tumors, organized hematoma
and tubo-ovarian abscess (5,13,18).
As pelvic AS often mimics adnexal masses or
malignancy (e.g., ovarian tumors or organized hematoma) with
plentiful pulsating blood flow, it may be misdiagnosed during
medical imaging. As pelvic AS does not require treatment unless it
is symptomatic or torsion and infarction of asymptomatic AS occur,
accurate diagnosis is important. Thus, differentiation of this
benign splenic abnormality from pathological disorders at the
pre-operative stage is often a diagnostic dilemma for gynecologists
(5). AS is generally detected during
radiological investigations or during open or laparoscopic
surgeries (5–7,13).
Abdominal computed tomography (CT), magnetic resonance imaging and
scintigraphy with Tc-99 m are helpful in making the diagnosis of
pelvic AS (14,17). Ota et al (14) concluded that 77.8% (7/9) of feeding
vessels of a pelvic AS originated from the great omentum or
splendid hilum, and thus, delineating the feeding blood vessels on
dynamic CT may be useful for diagnosing AS in the pelvis. For most
pelvic AS, regular monitoring by ultrasound inspection is
recommended instead of invasive over-treatment. Abdominal
sonography and Doppler imaging may be applied to avoid unnecessary
examinations if ectopic spleen is considered as a differential
diagnosis of pelvic masses (7–9). In
addition, tumor markers including CEA and CA199 are always within
normal limits in patients with AS, which allows for ruling out any
malignant gynecological diseases. Owing to the fact that in the
present case, the pelvic masses was suspected to be a malignancy
prior to surgery and due to their deep localization, open surgery
was preferred. Although open surgery has been the most frequently
reported method in previously published reports, the laparoscopic
approach may also be used for the diagnosis and treatment of large
AS. This approach also enables the ability to observe new
information in the abdominal cavity that may not be visible by
pre-operative diagnostic imaging alone.
In conclusion, the clinician should be aware of the
rare possibility of a pelvic AS in patients who present with
adnexa, pelvic discomfort or a pelvic mass. Pelvic AS is finally
diagnosed during radiological investigations, or during open or
laparoscopic surgeries.
Acknowledgements
Not applicable.
Funding
This study was supported by grants from the National
Natural Foundation of China (grant no. 81172467) and the Foundation
of Health and family Planning Commission of Hubei Province (grant
no. WJ2015MB153).
Availability of data and materials
All data generated or analyzed during this case are
included in this published article.
Authors' contributions
YF and YS contributed to drafting the manuscript. BW
and JL contributed to the data collection of the case. SW and DM
contributed to the interpretation of the data as well as the
editing of the manuscript. MW conceived and designed the study and
drafted and revised the manuscript. All authors have critically
reviewed this manuscript and approved the last version.
Ethics approval and consent to
participate
The patient provided their written informed consent
for inclusion within the present study.
Consent for publication
The patient provided their written consent for the
publication of their data as part of the present study.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
AS
|
accessory spleen
|
|
CT
|
computed tomography
|
References
|
1
|
Dodds WJ, Taylor AJ, Erickson SJ, Stewart
ET and Lawson TL: Radiologic imaging of splenic anomalies. AJR Am J
Roentgenol. 155:805–810. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhou JS, Chen X, Zhu T, Ding GJ and Zhang
P: Pelvic accessory spleen caused dysmenorrhea. Taiwan J Obstet
Gynecol. 54:445–446. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Halpert B and Gyorkey F: Lesions observed
in accessory spleens of 311 patients. Am J Clin Pathol. 32:165–168.
1959. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hsiao SM, Lee LC and Chang MH: Large
pelvic accessory spleen mimicking an adnexal malignancy in a
teenage girl. J Formos Med Assoc. 100:565–567. 2001.PubMed/NCBI
|
|
5
|
Taskin MI, Baser BG, Adali E, Bulbul E and
Uzgoren E: Accessory spleen in the pelvis: A case report. Int J
Surg Case Rep. 12:23–25. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Perin A, Cola R and Favretti F: Accessory
wandering spleen: Report of a case of laparoscopic approach in an
asymptomatic patient. Int J Surg Case Rep. 5:887–889. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Vural M, Kacar S, Koşar U and Altin L:
Symptomatic wandering accessory spleen in the pelvis: Sonographic
findings. J Clin Ultrasound. 27:534–536. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tendler R, Farah RK, Kais M, Odeh M and
Bornstein J: Symptomatic pelvic accessory spleen in a female
adolescent: Case report. J Clin Ultrasound. 45:600–602. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Iorio F, Frantellizzi V, Drudi FM,
Maghella F and Liberatore M: Locally vascularized pelvic accessory
spleen. J Ultrasound. 19:141–144. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tu C, Lin Q, Zhu J, Shao C, Zhang K, Jiang
C, Ding Z, Zhou X, Tu J, Zhu W and Chen W: Isolated sarcoidosis of
accessory spleen in the greater omentum: A case report. Exp Ther
Med. 11:2379–2384. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Unver Dogan N, Uysal II, Demirci S, Dogan
KH and Kolcu G: Accessory spleens at autopsy. Clin Anat.
24:757–762. 2011. View
Article : Google Scholar
|
|
12
|
Wood TW and Mangelson N: Urological
accessory splenic tissue. J Urol. 137:1219–1220. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Obuchi T, Takagane A, Sato K, Yonezawa H,
Funato O and Kobayashi M: Single-incision laparoscopic excision of
symptomatic accessory spleen in the pelvis: An initial report. J
Minim Access Surg. 13:321–322. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ota H, Ojima Y, Sumitani D and Okajima M:
Dynamic computed tomography findings of an accessory spleen in the
pelvis: A case report. Surg Case Rep. 2:232016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cowles RA and Lazar EL: Symptomatic pelvic
accessory spleen. Am J Surg. 194:225–226. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
d'Halluin G, Menard J, Dessard P, Dauphin
H, Deshayes M, Pierre F and Magnin G: Torsion of the accessory
spleen: An atypical etiology for acute abdomen. Gynecol Obstet
Fertil. 29:821–823. 2001.(In French). PubMed/NCBI
|
|
17
|
Nishiguchi S, Habu D, Ishizu H, Iwata Y,
Tatsumi N, Enomoto M, Minamitani S, Fukuda K, Tamori A, Takeda T,
et al: Accessory spleen in the pelvis diagnosed by Tc-99m phytate
scintigraphy. Ann Nucl Med. 15:263–265. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Azar GB, Awwad JT and Mufarrij IK:
Accessory spleen presenting as adnexal mass. Acta Obstet Gynecol
Scand. 72:587–588. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chen JS, Lin CL, Tsai CC, Lee KT, Ker CG
and Sheen PC: Giant ectopic pelvic spleen: Report of a case and
review of the literature. Gaoxiong Yi Xue Ke Xue Za Zhi. 9:54–60.
1993.PubMed/NCBI
|