Introduction
Myocardial infarction (MI) leading to heart failure
(HF) is a major cause of death in the world. The main center of HF
is cardiac remodeling including cardiomyocyte hypertrophy,
apoptosis and cardiac fibrosis (1).
Cardiac fibrosis plays a great role in development of mid- and
late-stage of HF, and it is a result of fibroblast proliferation
and excessive extracellular collagen matrix deposition which leads
to cardiac hypertrophy (2,3). Thus, inhibition of cardiac fibrosis is
a critical therapeutic approach to treat HF after MI
clinically.
MicroRNAs (miRNAs) are a relatively new class of
22-nt nonprotein-coding single-strand RNAs that control several
cellular processes, such as cell growth, proliferation and
differentiation. miRNAs have been shown to play a central role in
the pathogenesis of cardiac fibrosis (4). Related research has been done
previously. Li et al (5)
reported that miR-29a-3p inhibited ET-1-induced cardiomyocyte
hypertrophy via directly targeting the 3′-UTR of NFATc4 mRNA and
silencing NFATc4 expression. Besides, Zhang et al (6) found that miR-151-5p could bind to the
3′-UTR of FXYD1 and inhibit its expression, then influence
cardiovascular diseases. However, molecularly targeted therapy for
MI in clinic has not been sufficiently studied.
Recently, several studies showed that miR-30a could
inhibit myocardial fibrosis by regulating CTGF (7,8). The
five miR-30 family members (miR-30a through miR-30e) are
evolutionarily conserved and abundantly expressed in the mature
heart, but they are significantly dysregulated in human HF, in
experimental I/R, and in vitro after oxidative stress
(9,10). Further, it has been reported that
miR-30a levels are reduced in mouse models of hypertrophy, and
in vitro downregulated miR-30a aggravates
phenylephrine-induced cardiomyocyte hypertrophy by activating
autophagy (11). However, the
molecular mechanism of miR-30 attenuating cardiac fibrosis has not
been reported previously.
In the present study, the aim was to test whether
the putative miR-30a target sequence directly regulates protein
levels of CTGF. We first constructed the Adeno Associated Virus
(AAV) plasmid vector which carried the miR-30a gene of rat, then,
we transfected the miR-30a into the left ventricular cavity of
heart in MI rats. The 3′-UTR of CTGF was transfected into
COS1 cells, miR-30a and control miRNA were cotransfected into COS1
cells, respectively. The expression of luciferase was detected
before and after knockdown of the binding site of the miR-30a and
the 3′-UTR of CTGF. The cardioprotective effect of miR-30a and the
expression of luciferase in these hypertrophy models were observed.
Last, we tried to explore possible miR-30a-regulated mechanism.
Materials and methods
Animals
Rats were purchased from Jiancheng Bioengineering
Institute (Nanjing, China). Treatment of the rats used in this
investigation conformed to the recommendations in the Guide for the
Care and Use of Laboratory Animals published by the United States
National Institutes of Health (NIH Publication no. 85-23, revised
1996) and the protocol was approved by the Animal Care Committee of
Nanjing First Hospital (Nanjing, China).
rAAV9-miR-30a construction
RAAV9-miR-30a construction procedure was carried out
as previously described in detail (12). Briefly, the expression vector was
linearized and digested by restriction enzyme HindIII. After
handled with calf intestinal alkaline phosphatase (CIP) for 1 h,
the 5451 bp vector fragment was recycled to amplify the target
gene. Primer design was as follows: Primer 1 was used to isolate
miRNA-30a by PCR, its forward strand was
5′-GATCTCGAGCTCAAGTAGGGGCATATCTGAACGAGGCT-3′, and its reverse
strand was 5′-GATTATCGATAAGCTTCAATGCTATAACACATTTCTTTGC-3′. Primer 2
was used to identify transformation by colony PCR, its forward
strand was 5′-CATGGTCCTGCTGGAGTTCGTG-3′, and its reverse strand was
5′-CATAGCGTAAAAGGAGCAACA-3′. Then, miRNA30a DNA fragment was
recombined with line carrier. After the sequence identified by
colony PCR was correct, plasmid was extracted from inoculated
colony.
In vivo miR-30a heart transfection and
MI induction
At the beginning, we randomly divided 100 rats into
four groups: Sham operation group, control group (injected with
PBS), miR-30a-NC group (injected with blank AAV plasmid vector) and
miR-30a group (injected with rAAV9-miR-30a). Before surgery, rats
were anesthetized by intraperitoneal injection, intubated and
supported by small animal ventilator. After that we opened the
chest and exposed the heart. Then, PBS buffer, blank AAV plasmid
vector and rAAV9-miR-30a were injected into left ventricular
cavities of rats through the heart apex according to the grouping,
respectively. Then the ascending aorta was clamped for 5–8 sec by
non-traumatic hemostatic forceps gently for hemostasis, and
immediately released after the heart rate was down (13). If the rats still had no signs of
death after 10 min, MI model was established by left coronary
artery ligation as reported. Briefly, the left anterior descending
coronary artery was occluded with a nylon (6.0) suture at
approximately 1 mm from its origin below the tip of the left
atrium. Except that MI was not induced in rats of sham group, other
rats underwent the same procedures. The chest was closed with a
silk suture (14).
Echocardiographic evaluation
Four weeks after surgery, echocardiographic
evaluation was performed by a blinded observer. Rats were firstly
anaesthetized with 50 mg/kg sodium pentobarbital (Dolethal,
Vétoquinol, France) via intraperitoneal injection, and then images
were obtained using a Vevo 770 cardiac system (VisualSonics, Inc.,
Toronto, ON, Canada). The following parameters were evaluated: the
left ventricular end-systolic dimension (LVESD), the left ventrical
end-diastolic dimension (LVEDD), the fractional shortening (FS) and
ejection fraction (EF) (15).
Masson's staining
The heart tissue sample was fixed in 10% buffered
formalin and embedded in paraffin. Sections at 4 µm were stained
with Masson's staining. The deposition of total collagen (green
distributional area) was semi-quantitatively analyzed by ImageJ
system software. The collagen volume fraction was calculated as the
ratio of the total area of interstitial fibrosis to the entire
visual field of the section. A minimum of 5 randomly selected areas
per sample were observed at ×200 magnification, and the average
value was calculated for statistical analysis (16).
Immunohistochemical analysis
The heart sections were deparaffinized in xylene
(Thermo Fisher Scientific, Darmstadt, Germany) and rehydrated in
graded ethanol, and then rinsed in PBS. After blocking endogenous
peroxidase activity with 3% H2O2 for 10 min,
tissue sections were boiled for the antigen epitope retrieval in
0.1 mol/l citrate buffer (pH 6.0) for 10 min. Then the sections
were interacted with the 1:100 diluted primary antibodies (rabbit
anti-rat collagen I, III polyclonal antibodies; ab34710, ab7778;
Abcam, Cambridge, MA, USA) overnight at 4°C. After washing with
PBS, the slides were then incubated with secondary antibody (goat
anti-rabbit IgG polyclonal antibodies; 1:800; cat. no. DE0601;
Biodee Biotechnology Co., Beijing, China)) for 1 h, following by a
15-min-incubation with Streptavidin Peroxidase (Lab Vision Corp.,
Fremont, CA, USA) and 1-min hematoxylin-stain (C.I. 75290, B.S.C.
certification no. AcH-10; Aldrich, Milwaukee, WI, USA). Then, the
slides were dehydrated by graded ethanol, dehydrated by xylene, and
mounted with rhamsan gum.
The depositions of collagen I and collagen III (a
yellow to brown color) were semi-quantitatively analyzed by ImageJ
system software. The method of calculating collagen I and III
volume fraction were the same as the total collagen (17).
Real-time PCR
Total RNA was extracted with the TRIzol reagent
(Invitrogen, Carlsbad, CA, USA) according to the manufacturer's
instructions, and it was reverse transcribed into cDNA by using
PrimeScript RT reagent kit (Takara Bio, Kyoto, Japan). Real-time
PCR was performed using a 7500 Real-time PCR System (Applied
Biosystems) with SYBR Premix Ex Taq kit (Takara Bio). PCR primer
sequences were as followed: β-actin: (forward:
5′-GGTGGGAATGGGTCAGAAGG-3′, reverse: 5′-GGGGTACTTCAGGGTCAGGA-3′);
CTGF (forward: 5′-GTGTGATGAGCCCAAGGAC-3′, reverse:
5′-TGACAATACCTTCTGCAGGC-3′). The miRNA-30 primer was introduced in
the above-mentioned content. The following amplification conditions
were used: predenaturation at 95°C for 15 sec, denaturation at 94°C
for 30 sec, annealing at 60°C for 20 sec and extension at 72°C for
40 sec for 40 cycles. The relative changes of mRNA levels were
normalized to β-actin and the miRNA-30 relative change was
normalized to U6 (18).
Luciferase reporter gene assay
The CTGF 3′-UTR was inserted into a
luciferase expression plasmid (pMir-report), then transfected into
COS1 cells. miR-30a and control miRNA were transfected into COS1
cells (ICLC ATL01002, ATCC, USA) respectively. Then maintained in
DMEM supplemented with 10% FBS, and 2 mM L-Glutamine at 37°C in 5%
CO2 for 24 h. The expression levels of luciferase were
tested by 1X CCLR (cell lysis reagent) luciferase assay reagent.
Besides, after knockdown of the binding site of the miR-30a and the
3′-UTR of CTGF, miR-30a and control miRNA were transfected
into COS1 cells, respectively, then the expression levels of
luciferase were tested.
Western blot analysis
Protein was extracted from heart tissue and COS1
cells, respectively. The concentration of protein was measured
using the Bradford method. The expression of CTGF and β-actin in
heart tissue was detected, while the expression of CTGF and GAPDH
in COS1 cells were detected by western blotting. The extracted
protein (50 g) was electrophoresed on 10% SDS polyacrylamide gels
and then transferred to nitrocellulose membranes. After blocking
for 2 h at 4°C in buffer (10% fat-free milk in TBS-T), the membrane
was incubated overnight with anti-CTGF (1:1,000; Abcam, ab6992),
anti-β-actin (1:4,000; KeyGen Biotech, Nanjing, China), and
anti-GAPDH (1:1,000; Abbkine, Redlands, CA, USA, A01025),
respectively. The membranes were washed and incubated for 2 h at
4°C and conjugated with respective horseradish peroxidase
(HRP)-conjugated secondary antibodies (goat anti-mouse IgG 1:5,000
and goat anti-rat IgG 1:5,000; Jackson ImmunoResearch Laboratories,
West Grove, PA, USA) for 2 h at room temperature. Detection was
performed using enhanced chemiluminescence (Thermo Fisher
Scientific, Frederick, MD, USA) and photography (19).
Statistical analysis
Data are expressed as mean values ± standard
deviation. Differences among groups were analyzed by one-way ANOVA
using SPSS 13.0 (SPSS Inc., Chicago, IL, USA). The
Student-Newman-Keul's test was used for pairwise comparisons of
data. P<0.05 was considered to indicate a statistically
significant difference.
Results
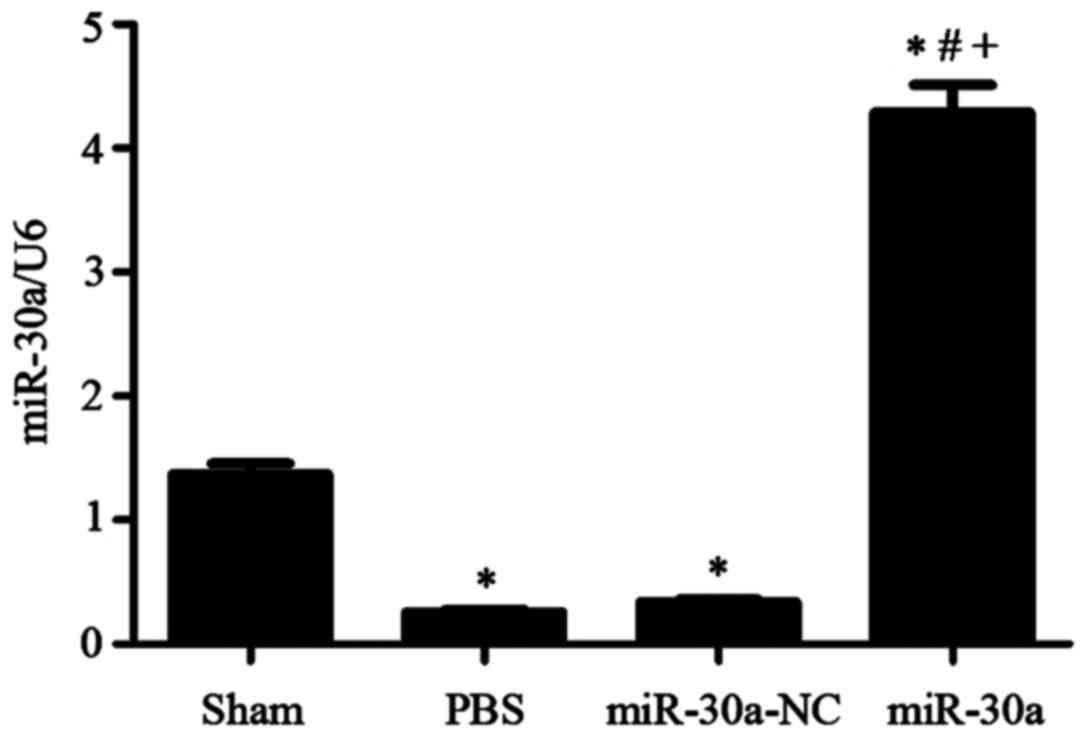
Heart miR-30a level changes in
experimental groups
Four weeks after MI surgery, we used RT-PCR to
measure the levels of miR-30a in different groups. miR-30a levels
were both obviously reduced in PBS group and miR-30a-NC group
(P<0.01 versus sham group). After injected with rAAV9-miR-30a in
rat cavities, miR-30a level was notably increased compared with
other three groups (P<0.01), suggesting that miR-30a was
successfully transfected into rat hearts (Fig. 1).
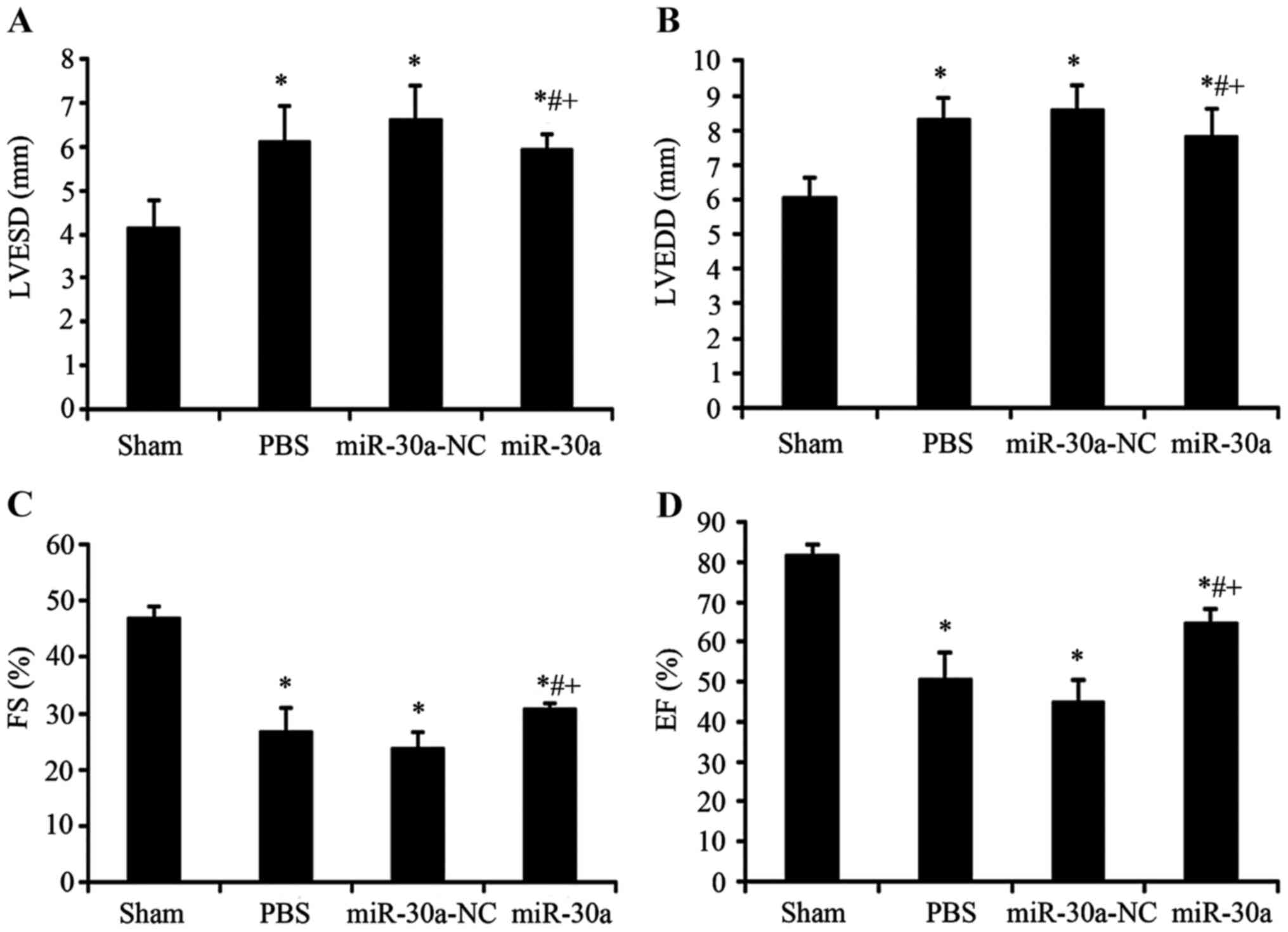
Effect of miR-30a on heart function in
MI rats
Before these rats were sacrificed, we used
echocardiography to determine heart diastolic and systolic
function. LVESD and LVEDD, as indexes of diastolic function, were
markedly increased in PBS group, miR-30a-NC group and miR-30a group
(P<0.01 versus sham group). After injected with rAAV9-miR-30a,
heart diastolic function was significantly improved (P<0.01
versus PBS group and miR-30a-NC group). Heart systolic function
reflected by EF and FS was evidently decreased in PBS group,
miR-30a-NC group and miR-30a group (P<0.01 versus sham group),
and these indexes of miR-30a group were notably increased
(P<0.01 versus PBS group and miR-30a-NC group). In conclusion,
these results showed that miR-30a transfected into heart could
significantly inhibit the changes of heart diastolic and systolic
function in MI rats (Fig. 2).
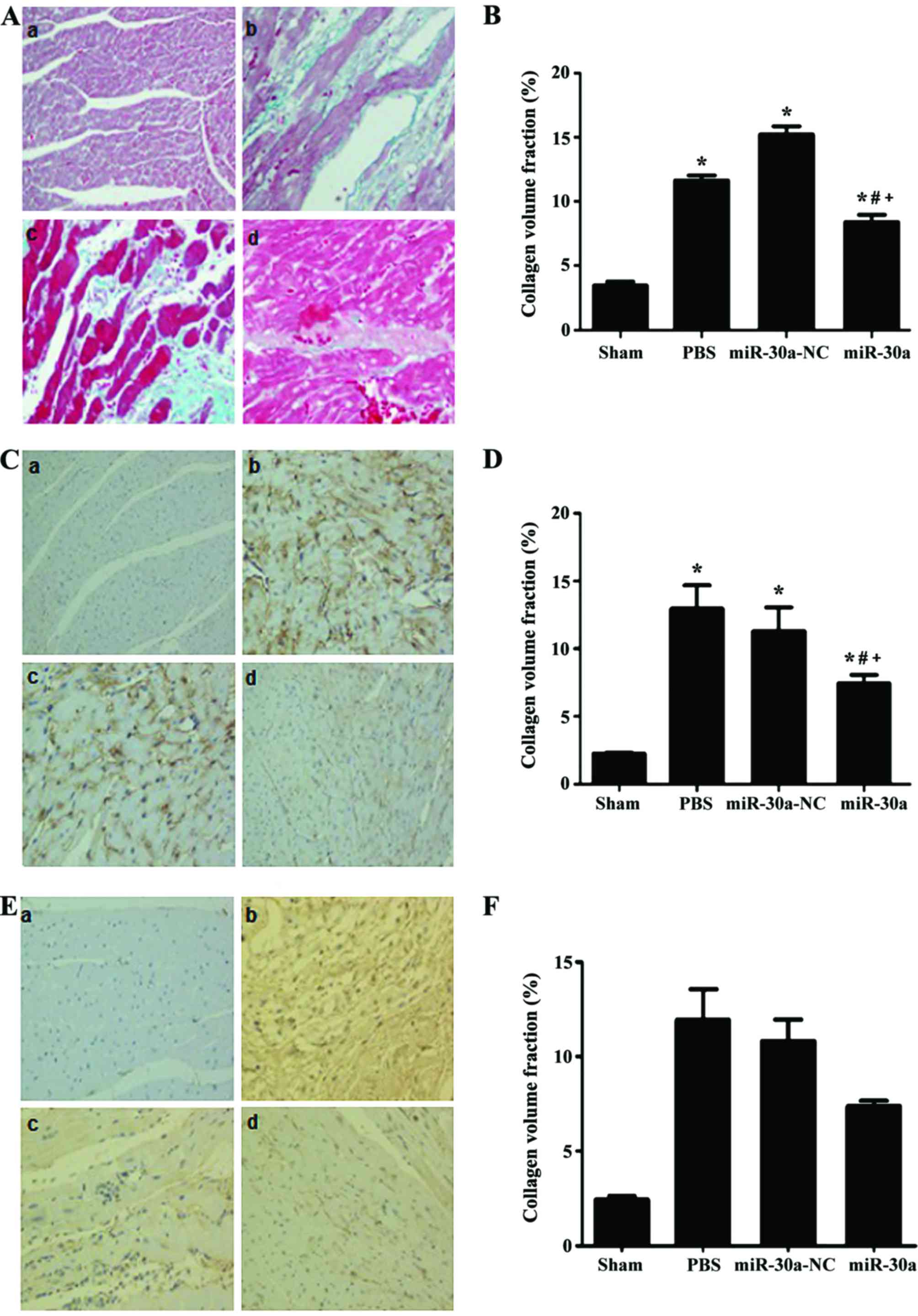
Effect of miR-30a on collagen
deposition in hearts of MI rats
The Masson's staining and immunohistochemical
staining were performed to analyze the distribution of total
collagen, collagen I and III. As a result, total collagen, collagen
I and III were all obviously increased in PBS group and miR-30a-NC
group and miR-30a group (P<0.01 versus sham group). However,
they were all significantly ameliorated in miR-30a treatment group
(P<0.01 versus PBS group and miR-30a-NC group). Altogether,
these results indicated that miR-30a could attenuate cardiac
fibrosis in MI rats (Fig. 3).
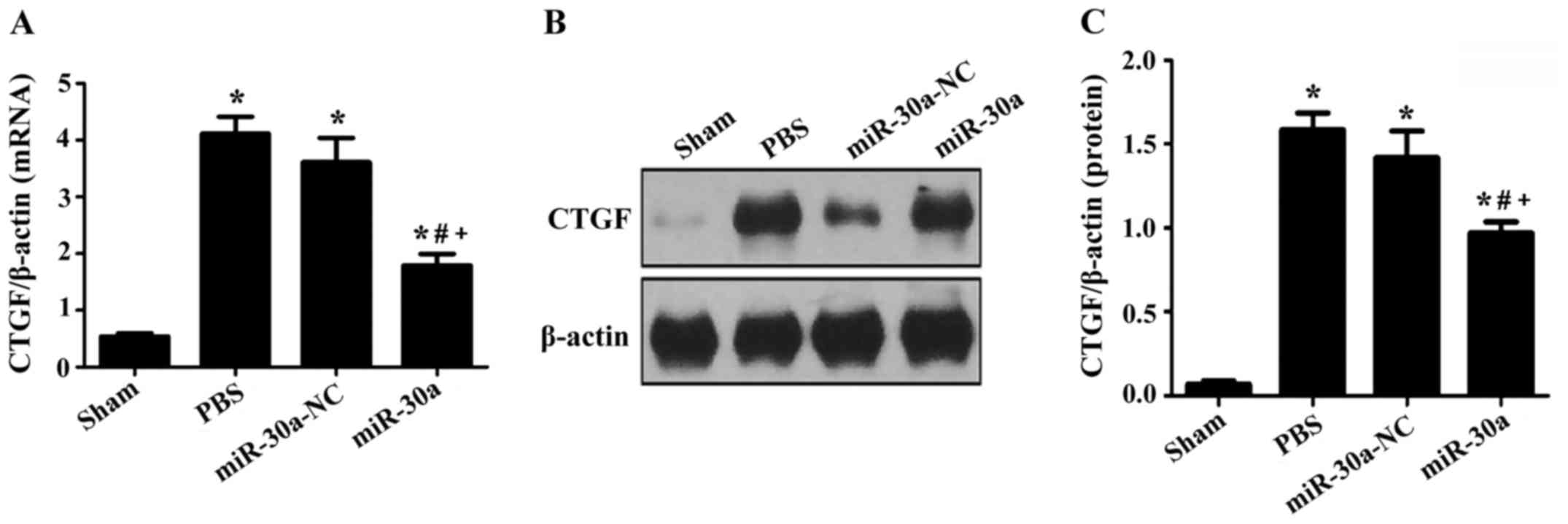
Effect of miR-30a on CTGF expression
levels in hearts of MI rats
RT-PCR and western blotting were used to measure
CTGF expression. In PBS group, miR-30a-NC group and miR-30a group,
CTGF expression was markedly upregulated both at the
transcriptional and translational level (P<0.01 versus sham
group), but it was downregulated after treated with miR-30a,
suggesting that miR-30a could ameliorate myocardial fibrosis
through inhibition of CTGF expression in MI rats (Fig. 4).
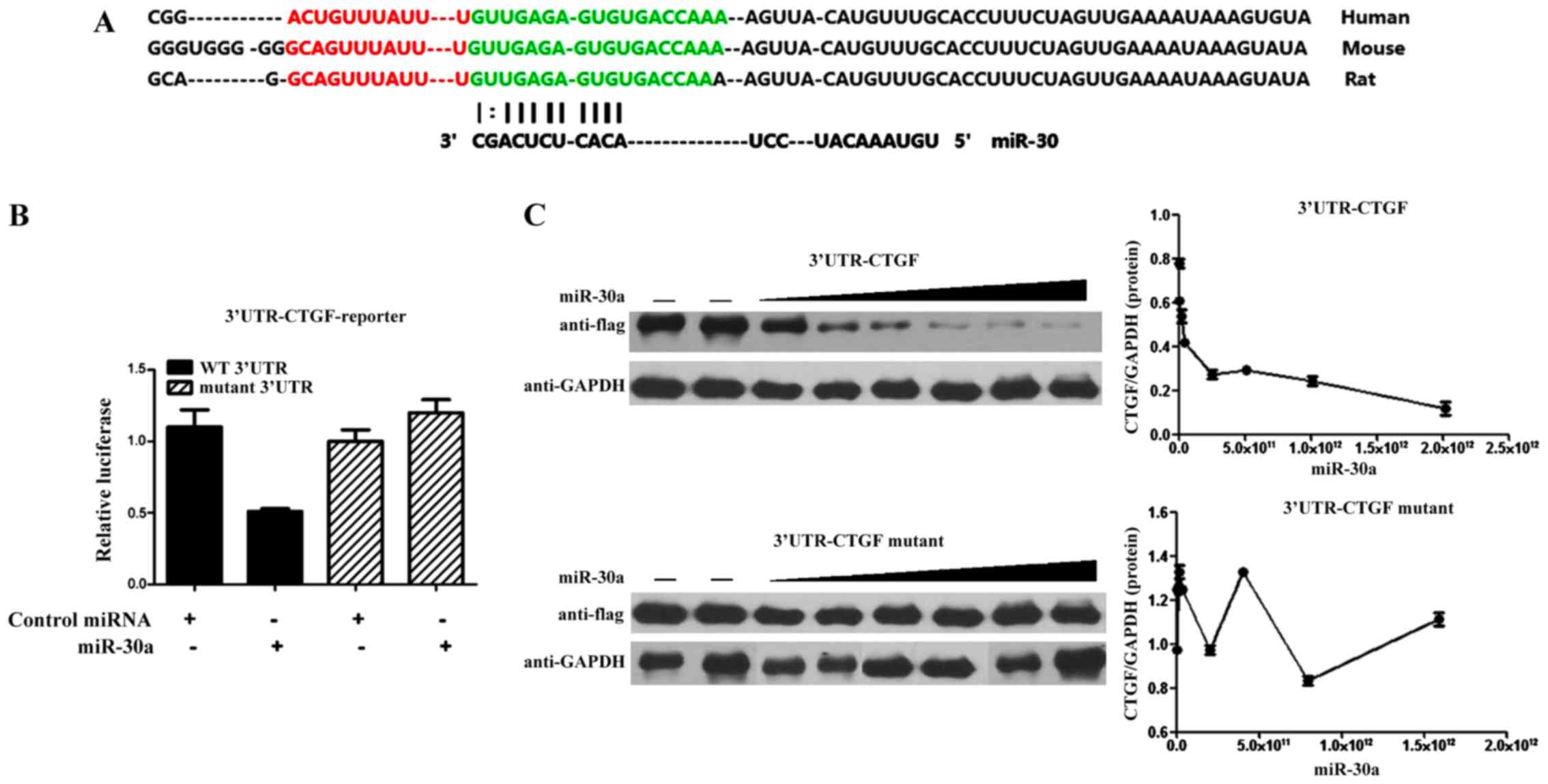
CTGF is a direct target of
miR-30a
The above suggests that CTGF is regulated by miR-30a
(8). Deletion of the miRNA binding
site abrogated the repressive effect of miR-30a on luciferase
activity, which indicated that the expression of CTGF was extremely
sensitive to the miR-binding sequence within the 3′-UTR. miR-30a
also dose-dependently inhibited the synthesis of Flag-tagged MEF2C
expression cassette which linked to the CTGF 3′-UTR binding
sequence. However, there was no significant difference in the
mutant CTGF 3′-UTR group with the miR-30a target site deleted
(Fig. 5).
Discussion
In this study, we found that miR-30a could improve
cardiac dysfunction and myocardial fibrosis in rats with MI by
inhibiting CTGF expression, which was previously unreported. AAV9
is proven to be the strong cardiotropic serotype in mouse and rat
as compared to AAV1, 6, 7 and 8. AAV9. The transcoronary gene
delivery is a more high-efficiency method than gene delivery by
tail vein injection. Thus, we used AAV9 to transfer miR-30a to the
heart by this method in the investigation. Four weeks after the
operation, we found that the level of heart miR-30a after injected
with rAAV9-miR-30a was obviously increased, indicating that heart
miR-30a transfection was successful.
Yin et al (11) reported that miR-30a levels are
reduced in transverse aortic constriction mice, and downregulated
miR-30a aggravates phenylephrine-induced cardiomyocyte hypertrophy
by activating autophagy in H9c2 cells. Liu and his colleges
revealed that miR-30a could attenuate the Angiotensin II-induced
upregulation of hypertrophy-related genes and decrease the
cardiomyocyte surface area via targeting beclin 1 (20). Cardioprotective effect of
triiodothyronine was associated with restored levels of miR-30a
expression that correspond to p53 mRNA downregulation in rats with
cardiac ischemia/reperfusion (9).
miR-30a levels in this study were significantly reduced 4 weeks
after MI surgery, and heart function and cardiac fibrosis were
severely deteriorated, which was reversed by treatment with
miR-30a. Besides, the expression level of serum miR-30a was closely
correlated with the cardiac function, therefore it could be as a
biomarker for indicating heart failure (21). Therefore, maintenance of miR-30a
level may be associated with cardioprotection.
CTGF, a mitogen secreted by vascular endothelial
cells, acts as integrins, proteoglycans, or tyrosine kinases
(22). In normal physiological
environment, CTGF is mainly involved in angiogenesis and cell
differentiation. It is worth noting that CTGF could mediate the
process of tissue repair and fibrosis under pathological conditions
(23). Many experiments in
vitro showed that CTGF could stimulate the proliferation of
cardiac fibroblasts and increase the production of extracellular
matrix (24). In the process of
myocardial injury, repair and fibrosis, CTGF is an obvious
activation sign for fibroblasts. Though the pro-fibrogenic effect
of CTGF was weak, it provided a beneficial environment for other
fibrotic stimuli (25,26). In our study, we measured heart CTGF
expression in experimental groups. CTGF expression was markedly
increased both at the transcriptional and translational level,
which was decreased by miR-30 injection, revealing that miR-30 may
also improve cardiac fibrosis. Related studies found that miR-30
could directly influence CTGF levels (27,28). In
our study, luciferase expression in COS1 cells decreased
significantly, after knockdown of miR-30a and CTGF binding sites.
This indicated that the miR-30a regulated protein levels of CTGF
combined with 3′-UTR directly, revealing that miR-30 may also
improve cardiac fibrosis via binding 3-UTR of CTGF. Similarly to a
previous study, miR-30 through specific binding to its 3-UTR
influences CTGF levels (29).
In summary, miR-30a may inhibit the expression of
CTGF in myocardium after MI by directly combining with the 3′-UTR
of CTGF in myocardium after MI, thereby reducing the production of
collagen in myocardia, inhibiting myocardial fibrosis, then
improving cardiac functions.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LC and NT contributed to the conception and design
of the study. LC drafted the manuscript. QJ performed the data
analyses. HZ and YR performed Masson's staining and
immunohistochemical analysis. ZF performed and analyzed real-time
PCR. NT reviewed the manuscript and gave his approval to the
submitted and final versions. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Nanjing First Hospital (Nanjing, China).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
van Berlo JH, Maillet M and Molkentin JD:
Signaling effectors underlying pathologic growth and remodeling of
the heart. J Clin Invest. 123:37–45. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chen C, Li R, Ross RS and Manso AM:
Integrins and integrin-related proteins in cardiac fibrosis. J Mol
Cell Cardiol. 93:162–174. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Koshman YE, Patel N, Chu M, Iyengar R, Kim
T, Ersahin C, Lewis W, Heroux A and Samarel AM: Regulation of
connective tissue growth factor gene expression and fibrosis in
human heart failure. J Card Fail. 19:283–294. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Creemers EE and van Rooij E: Function and
therapeutic potential of non-coding RNAs in cardiac fibrosis. Circ
Res. 118:108–118. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Li M, Wang N, Zhang J, He HP, Gong HQ,
Zhang R, Song TF, Zhang LN, Guo ZX, Cao DS, et al: MicroRNA-29a-3p
attenuates ET-1-induced hypertrophic responses in H9c2
cardiomyocytes. Gene. 585:44–50. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhang Y, Wang R, Du W, Wang S, Yang L, Pan
Z, Li X, Xiong X, He H, Shi Y, et al: Downregulation of miR-151-5p
contributes to increased susceptibility to arrhythmogenesis during
myocardial infarction with estrogen deprivation. PLoS One.
8:e729852013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chen LW, Zhu LL, Ji Q, Zhu H, Ren YZ, Fan
ZG, Li XB, Gao XF, Zhang YJ and Tian NL: Relationship between
myocardial microRNA-30a expression and myocardial fibrosis in rats
post myocardial infarction. Zhonghua Xin Xue Guan Bing Za Zhi.
44:443–449. 2016.(In Chinese). PubMed/NCBI
|
|
8
|
Yuan CT, Li XX, Cheng QJ, Wang YH, Wang JH
and Liu CL: MiR-30a regulates the atrial fibrillation-induced
myocardial fibrosis by targeting snail 1. Int J Clin Exp Pathol.
8:15527–15536. 2015.PubMed/NCBI
|
|
9
|
Forini F, Kusmic C, Nicolini G, Mariani L,
Zucchi R, Matteucci M, Iervasi G and Pitto L: Triiodothyronine
prevents cardiac ischemia/reperfusion mitochondrial impairment and
cell loss by regulating miR30a/p53 axis. Endocrinology.
155:4581–4590. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gutiérrez-Escolano A, Santacruz-Vázquez E
and Gómez-Pérez F: Dysregulated microRNAs involved in
contrast-induced acute kidney injury in rat and human. Ren Fail.
37:1498–1506. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yin X, Peng C, Ning W, Li C, Ren Z, Zhang
J, Gao H and Zhao K: miR-30a downregulation aggravates pressure
overload-induced cardiomyocyte hypertrophy. Mol Cell Biochem.
379:1–6. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gao X, Ma YT, Yang YN, Xiang Y, Chen BD,
Liu F and Du L: Recombinant adeno-associated virus serotype 9
transfection of rats H9C2 cells in vitro. Xi Bao Yu Fen Zi Mian Yi
Xue Za Zhi. 26:18–20. 2010.(In Chinese). PubMed/NCBI
|
|
13
|
Bish LT, Morine K, Sleeper MM, Sanmiguel
J, Wu D, Gao G, Wilson JM and Sweeney HL: Adeno-associated virus
(AAV) serotype 9 provides global cardiac gene transfer superior to
AAV1, AAV6, AAV7, and AAV8 in the mouse and rat. Hum Gene Ther.
19:1359–1368. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kalisz M, Baranowska B, Wolinska-Witort E,
Maczewski M, Mackiewicz U, Tulacz D, Gora M, Martynska L and Bik W:
Total and high molecular weight adiponectin levels in the rat model
of post-myocardial infarction heart failure. J Physiol Pharmacol.
66:673–680. 2015.PubMed/NCBI
|
|
15
|
Bagno LL, Carvalho D, Mesquita F, Louzada
RA, Andrade B, Kasai-Brunswick TH, Lago VM, Suhet G, Cipitelli D,
Werneck-de-Castro JP, et al: Sustained IGF-1 secretion by
adipose-derived stem cells improves infarcted heart function. Cell
Transplant. 25:1609–1622. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chen J, Huang C, Zhang B, Huang Q, Chen J
and Xu L: The effects of carvedilol on cardiac structural
remodeling: The role of endogenous nitric oxide in the activity of
carvedilol. Mol Med Rep. 7:1155–1158. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Abdel-Hamid AAM and Firgany A-D:
Atorvastatin alleviates experimental diabetic cardiomyopathy by
suppressing apoptosis and oxidative stress. J Mol Histol.
46:337–345. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Parimala M, Debjani M, Vasanthi HR and
Shoba FG: Nymphaea nouchali Burm. f. hydroalcoholic seed
extract increases glucose consumption in 3T3-L1 adipocytes through
activation of peroxisome proliferator-activated receptor gamma and
insulin sensitization. J Adv Pharm Technol Res. 6:183–189. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wojcik B, Harasim E, Zabielski P,
Chabowski A and Gorski J: Effect of tachycardia on lipid metabolism
and expression of fatty acid transporters in heart ventricles of
the rat. J Physiol Pharmacol. 66:691–699. 2015.PubMed/NCBI
|
|
20
|
Pan W, Zhong Y, Cheng C, Liu B, Wang L, Li
A, Xiong L and Liu S: MiR-30-regulated autophagy mediates
angiotensin II-induced myocardial hypertrophy. PLoS One.
8:e539502013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Xia X: The relationship of serum miR-30a
and heart failure in children with congenital heart disease. J Clin
Pediatr. 32:607–609. 2014.http://www.jcp-sh.org.cn/EN/abstract/abstract8665.shtml
|
|
22
|
Leask A and Abraham DJ: All in the CCN
family: Essential matricellular signaling modulators emerge from
the bunker. J Cell Sci. 119:4803–4810. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Shimo T, Nakanishi T, Nishida T, Asano M,
Kanyama M, Kuboki T, Tamatani T, Tezuka K, Takemura M, Matsumura T,
et al: Connective tissue growth factor induces the proliferation,
migration, and tube formation of vascular endothelial cells in
vitro, and angiogenesis in vivo. J Biochem. 126:137–145. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wang B, Haldar SM, Lu Y, Ibrahim OA, Fisch
S, Gray S, Leask A and Jain MK: The Kruppel-like factor KLF15
inhibits connective tissue growth factor (CTGF) expression in
cardiac fibroblasts. J Mol Cell Cardiol. 45:193–197. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hayata N, Fujio Y, Yamamoto Y, Iwakura T,
Obana M, Takai M, Mohri T, Nonen S, Maeda M and Azuma J: Connective
tissue growth factor induces cardiac hypertrophy through Akt
signaling. Biochem Biophys Res Commun. 370:274–278. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Bonniaud P, Martin G, Margetts PJ, Ask K,
Robertson J, Gauldie J and Kolb M: Connective tissue growth factor
is crucial to inducing a profibrotic environment in
‘fibrosis-resistant’ BALB/c mouse lungs. Am J Respir Cell Mol Biol.
31:510–516. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wang J, Duan L, Guo T, Gao Y, Tian L, Liu
J, Wang S and Yang J: Downregulation of miR-30c promotes renal
fibrosis by target CTGF in diabetic nephropathy. J Diabetes
Complications. 30:406–414. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Su Z, Wei G, Wei L, Liu J and Li X:
Effects of rhBNP on myocardial fibrosis after myocardial infarction
in rats. Int J Clin Exp Pathol. 8:6407–6415. 2015.PubMed/NCBI
|
|
29
|
Duisters RF, Tijsen AJ, Schroen B,
Leenders JJ, Lentink V, van der Made I, Herias V, van Leeuwen RE,
Schellings MW, Barenbrug P, et al: miR-133 and miR-30 regulate
connective tissue growth factor: Implications for a role of
microRNAs in myocardial matrix remodeling. Circ Res. 104:170–178.
2009. View Article : Google Scholar : PubMed/NCBI
|