Introduction
Systemic lupus erythematosus (SLE) is associated
with a broad spectrum of clinical and immunologic manifestations
(1), of which lupus nephritis (LN)
is the most common cause of morbidity and mortality. LN affects
~40% of patients with SLE and requires prompt treatment with
immunosuppressants (2). Although
induction treatment with glucocorticoids combined with
mycophenolate mofetil (MMF) or cyclophosphamide (CTX) may cause
partial remission (PR) or complete remission (CR) in patients
(3), renal recurrence during
maintenance treatment, including glucocorticoids combined with MMF,
Tripterygium wilfordii, leflunomide, tacrolimus or
azathioprine, remains very common and is observed in up to 30% of
patients with LN (4). Renal
recurrence causes an increase in urinary protein and serum
creatinine levels, the development of active urinary sediments or a
decrease in the glomerular filtration rate, as well as other
complications (5). A large
proportion of patients with LN that experience renal recurrence may
achieve remission again following prompt treatment; thus, the early
identification and prevention of renal recurrence is essential
(6). To the best of our knowledge, a
reliable and useful clinical predictor or marker of renal
recurrence has not yet been identified (7). Therefore, the aim of the present study
was to analyze the baseline clinical data of patients with LN type
IV to identify any clinical indices that may be used to predict
renal recurrence.
Patients and methods
Patients
A total of 244 patients were enrolled in the present
study between May 1998 and May 2013, providing they met the
following conditions: Diagnosis of SLE and further diagnosis of LN
type IV by renal biopsy in the Second Hospital Affiliated to
Lanzhou University (Gansu, China), with complete clinical,
pathological and laboratory test records and the achievement of
clinical remission following induction therapy. Patients with or
without renal recurrence were included in the current study.
Baseline clinical features, laboratory indexes, pathological
results and treatment situations were compared between patients
with LN type IV with or without renal recurrence.
Pathological classification of renal
biopsy
LN glomerular pathological classification was based
on the International Society of Nephrology/Renal Pathology Society
2003 classification system (8). LN
type IV was diagnosed when the affected glomerular area was
>50%. LN Type IV with diffuse lesions was identified by
observation under a light microscope revealing fuchsinophilic
protein deposition or rete pegs occurring on the lateral side of
the glomerular basement membrane; immunofluorescence revealing fine
granular deposits of immunoglobulin and complement along the
glomerular basement membrane or electron microscopy revealing that
electron dense or rete pegs forming on the lateral side of the
basement membrane, and was classified as LN type IV + V. Scoring of
the renal active index and chronic index was based on a method
outlined in a previous study (9).
Atherosclerosis was confirmed when arterial intima fibrous
thickening and hyaline degeneration were observed under a light
microscope; necrosis, thrombosis and inflammatory cell infiltration
were not observed and there was no immunoglobulin (Ig) deposition
observed via immunofluorescence. Non-inflammatory necrotic
vasculopathy (NNV) was confirmed when vascular wall necrosis was
observed using a light microscope, no inflammatory cell
infiltration was observed on the vessel wall or in the surrounding
area, and immunoglobulin and complement and fibrin-related antigen
were observed on the vascular walls, as well as in the lumen via
immunofluorescence. Immune complex deposition was determined when
morphology was normal under light microscopy, there was no thrombus
and necrosis and the vascular lumen had no stenosis, and vascular
wall immune deposits were found to contain IgG, IgA, IgM and/or
complement components via immunofluorescence. Vasculopathy-free was
classified when the morphology of interstitial blood vessels was
normal and no IgG, IgA, IgM and complement deposition were found on
the blood vessel wall via immunofluorescence (10).
Clinical data
The following clinical and laboratory indicators
were collected: Sex, age, SLE course, LN course, laboratory results
and immunological indexes.
Treatments
All patients underwent immunosuppressant therapy,
including prednisone (0.5–0.6 mg/kg for 4 weeks then tapered to a
maintenance dose; Hubei Pharmaceutical Co., Ltd., Wuhan, China)
combined with IV CTX (500–1,000 mg/m2 body surface area
monthly; Purdue Pharma, Stamford, CT, USA), MMF (1,500–2,000 mg
daily. Roche Diagnostics, Basel, Switzerland) tacrolimus (FK;
0.05–0.1 mg/kg daily. Fujisawa Ireland Ltd., Kerry, Ireland).
Maintenance treatment included the combination treatment of
prednisone (5 mg, daily), Tripterygium wilfordii
polyglycoside (60 mg daily; Jiangsu Taizhou Pharmaceutical Co.,
Ltd., Nanjing, China), leflunomide (20 mg daily; Suzhou Xinkai
Pharmaceutical Co., Ltd., Suzhou, China), MMF (500–1,000 mg daily),
FK (0.05 mg/kg daily) or azathioprine (50–10 mg daily).
Renal recurrence
Renal recurrence refers to the phenomenon when
patients with LN that have achieved complete remission (CR) or
partial remission (PR) for >3 months experience a rapid increase
in serum creatinine levels or albuminuria (11). Renal recurrence includes nephritis
recurrence and nephrotic recurrence. In the current study,
nephritis recurrence was classified as an increase of ≥25% in serum
creatinine levels with or without an increase in urinary protein.
Nephrotic recurrence was classified when urinary protein increased
≥1 g following CR or when urinary protein increased by >2 times
that of the previous level following PR (11). Patients were divided into 2 groups
depending on whether they experienced renal recurrence or not.
There were 100 patients with renal recurrence (83 females and 17
males; mean age, 30.86 years) and 144 patients without renal
recurrence (125 female and 19 males; mean age, 29.74 years).
Curative effects
CR was achieved when urinary protein levels were
≤0.4 g/D and levels of serum albumin and serum creatinine were ≥35
g/l and ≤120 mmol/l, respectively. PR referred to a ≥50% decrease
in levels of urinary protein and serum creatinine compared with
base values and plasma albumin ≥30 g/l. Clinical remission referred
to patients that achieved CR or PR. No remission referred to no
improvement in urine test results or renal functions (an increase
or decrease in serum creatinine that was <50% of the base value)
(12).
Follow-up
Patients were followed-up once every 2–3 months. A
follow-up with a ≥6 month duration was defined as a follow-up. A
follow-up with a duration of <6 months was defined as withdrawal
from the study.
Statistical analysis
All data were analyzed using SPSS 19.0 software (IBM
Corp., Armonk, NY, USA). Normally distributed measurement data were
expressed as the mean ± standard deviation and non-normally
distributed measurement data were expressed as the median (lower
quartile-upper quartile). Count data were compared using the
χ2 test and measurement data were compared using
Student's t test. The recurrence survival curve was estimated using
the Kaplan Meier-method and survival curves between groups were
compared using the Log-Rank test. Risk factors for recurrence were
analyzed using univariate and multivariate analyses with the Cox
proportional hazard model. P<0.05 was determined to indicate a
statistically significant difference.
Results
Renal recurrence in patients with LN
type IV
A total of 351 patients with LN type IV with
complete clinical information and follow-ups were included in the
current study. Among these patients, 100 patients (28.49%) relapsed
and 144 patients (41.03%) did not relapse. The remaining patients
either only received initial treatment (53; 15.10%) or did not
respond to follow up (54; 15.38%).
The average follow-up duration of patients who
relapsed was 49.50 months (range, 13–207 months). The average age
of patients who relapsed was 30.86±9.74 years (range, 12–54 years).
Among these patients, 83 (83%) were female and 17 (17%) were male.
Mean SLE course was 19.50 months (range, 4.25–60 months), mean LN
course was 9 months (range, 2–24 months) and average recurrence
time was 31.15±26.74 months. The average follow-up duration of
non-relapsed patients was 33 months (range, 13–220 months) and the
average age of these patients was 29.74±9.68 years (range, 4–53
years). Among these patients, 125 (86.81%) were female and 19
(13.19%) were male. Mean SLE course was 23.50 months (range, 4–60
months) and the mean LN course was 7.50 months (range, 1–36
months). Differences in age, sex, SLE and LN courses between the
two groups were not significant (Table
I). In the recurrence group the average recurrence time was
31.15±26.74 months. A total of 66 (66%) patients had nephrotic
recurrence, 31 (31%) patients had nephritis recurrence, and average
recurrence times were 26.67±20.17 and 38.22±35.46 months,
respectively (P>0.05). A total of 3 (3%) patients exhibited
extra-renal recurrence and average renal recurrence time was
56.67±30.14 months. Recurrence rates at months 12, 24, 36 and 60
were 8, 23, 31 and 48%, respectively. In the recurrence group, 31
patients (31%) had increased levels of creatinine, 9 (9%) developed
end-stage renal failure (ESRF) and 5 (5%) succumbed. The survival
rates of patients in the relapse group in years 1, 5 and 10 were
97, 92 and 70.9%, respectively; whereas the survival rates of
patients that did not experience renal recurrence were 99, 95.2 and
80.4% in years 1, 5 and 10, respectively. The incidence of
increased levels of creatinine, ESRF and mortality rates were
significantly higher in patients with recurrence than in patients
without recurrence.
 | Table I.Comparison of baseline clinical data
between the two groups. |
Table I.
Comparison of baseline clinical data
between the two groups.
|
| Groups |
|
|---|
|
|
|
|
|---|
| Factors | Group with renal
recurrence (n=100) | Group without renal
recurrence (n=144) | P-value |
|---|
| General
information |
|
|
|
| Sex,
male/female (%) | 17 (17)/83 (83) | 19 (13.19)/125
(86.81) | 0.41 |
| Onset age
(years old) | 27.45±9.178 | 25.98±9.911 | 0.241 |
| Age
(years old) | 30.86±9.744 | 29.74±9.678 | 0.377 |
| Course of
SLE (months) | 19.5 (4.25–60) | 23.50 (4–60) | 0.772 |
| Course of
LN (months) | 9.00 (2–24) | 7.50 (1–36) | 0.763 |
| Manifestation of
kidney and others |
|
|
|
| Facial
erythema (%) | 51/99 (51.52) | 70/144 (48.61) | 0.656 |
| Discoid
erythema (%) | 6/100 (6) | 7/144 (4.86) | 0.697 |
| Fever
(%) | 51/100 (51) | 58/144 (40.28) | 0.098 |
|
Arthralgia (%) | 72/100 (72) | 69/144 (47.92) | 0.001 |
|
Alopecia (%) | 27/100 (27) | 24/144 (16.67) | 0.051 |
| Spleen
(%) | 11/100 (11) | 7/144 (4.86) | 0.071 |
|
Intestine (%) | 3/100 (3) | 0/144 (0) | 0.068 |
|
Hypertension (%) | 44/100 (44) | 69/143 (48.25) | 0.513 |
|
Malignant hypertension
(%) | 7/100 (7) | 9/143 (6.29) | 0.827 |
| Gross
hematuria (%) | 26/100 (26) | 27/143 (18.88) | 0.186 |
| Massive
proteinuria (%) | 40/100 (40) | 77/144 (53.47) | 0.038a |
|
Hypoproteinemia (%) | 74/100 (74) | 94/141 (66.67) | 0.222 |
|
Abnormal renal function
(%) | 21/100 (21) | 31/141 (21.99) | 0.855 |
| Laboratory
examination |
|
|
|
| Hb
(g/dl) | 9.01±2.14 | 9.56±2.19 | 0.053 |
| PLT
(/mm3) | 11.60 (8–16.6) | 12.10
(8.7–17.6) | 0.331 |
| ALB
(g/l) | 25.59±6.83 | 26.60±7.47 | 0.284 |
| GLO
(g/l) | 24.6
(13.4–54.8) | 22.50
(10–45.1) | 0.022a |
| CREA
(mg/dl) | 1
(0.42–8.12) | 0.91
(0.26–4.90) | 0.309 |
| BUN
(mg/dl) | 14.94 (2.4–74) | 14.28
(2.5–96.) | 0.729 |
| UA
(µmol/l) | 422
(350.25–521.50) | 400.5
(333.75–504.50) | 0.402 |
| UPR
(g/24 h) | 3.09
(1.64–5.49) | 3.64
(2.17–5.34) | 0.207 |
| Urine
NAG | 39.2
(28.85–58.68) | 44.00
(24.40–65.10) | 0.422 |
| Urine
C3 | 2 (0~43) | 2.09 (0~32) | 0.015a |
| Urine
α2m (µg/l) | 2 (0~32) | 3.44 (0~200) | 0.004a |
| Autoantibody
(%) |
|
RNP | 37/97 (38.14) | 25/133
(18.80) | 0.001a |
|
SSA | 22/70 (31.43) | 35/109
(32.11) | 0.924 |
|
SSB | 12/70 (17.14) | 11/109
(10.09) | 0.169 |
| RF | 3/59 (5.08) | 10/114 (8.77) | 0.570 |
|
ANCA | 3/71 (4.23) | 3/106
(2.83) | 0.937 |
|
ANA | 93/100 (93) | 130/143
(90.91) | 0.559 |
Effects of renal and extra-renal
manifestations at onset of renal recurrence
Patients with LN type IV with recurrence had
significantly higher incidences of arthralgia compared with
patients without recurrence and the incidence of proteinuria was
significantly decreased in patients with LN type IV with recurrence
compared with patients with LN type IV without recurrence
(P<0.05; Table I). However,
analysis by the Kaplan-Meier method indicated that arthralgia,
alopecia and proteinuria had no influence on the recurrence rate
(data not shown). Patients with LN type IV that affected the
digestive tract also had higher renal recurrence rates (P=0.003;
Fig. 1).
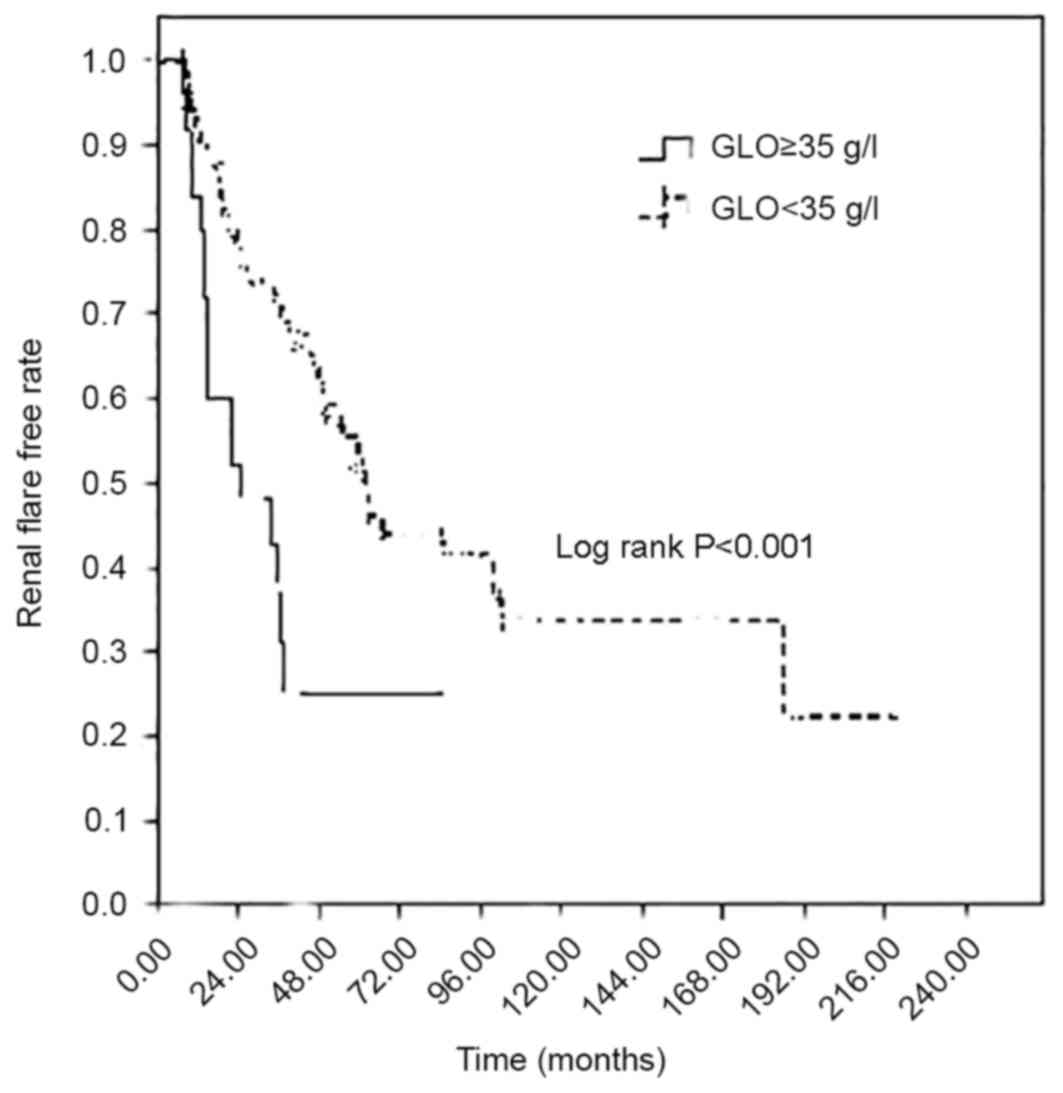
Effect of different laboratory tests
at the onset on renal recurrence
Patients with LN type IV that experienced recurrence
had significantly increased globulin levels compared with patients
without recurrence; furthermore, levels of urinary C3 and
macroglobulin were significantly decreased in relapsed patients
compared with non-relapsed patients (all P<0.05, Table I). Further analysis by the
Kaplan-Meier method demonstrated that the renal recurrence rate was
higher in patients with high globulin levels (P<0.01; Fig. 2) however, levels of urinary C3 and
α2m had no effect on recurrence rates (data not shown).
Effect of different serum
auto-antibody profiles at the onset on renal recurrence
Patients with LN type IV with recurrence had a
significantly increased level of positive ribonucleoprotein (RNP)
antibody compared with patients without recurrence (P=0.001;
Table I). Further analysis by the
Kaplan-Meier method demonstrated that patients with positive
anti-RNP and anti-SSB antibodies had significantly increased
recurrence rates (P=0.006; Fig.
3).
Effects of different renal
histopathology at the onset on renal recurrence
Loop thrombus and NNV were significantly increased
in patients with LN type IV with recurrence compared with patients
without recurrence (both P<0.05; Table II). Further analysis by the
Kaplan-Meier method revealed that patients with thrombus in the
loop or NNV had a significantly higher recurrence rate (P<0.05;
data not shown).
 | Table II.Pathological characteristics of renal
tissue of patients with lupus nephritis type IV. |
Table II.
Pathological characteristics of renal
tissue of patients with lupus nephritis type IV.
|
| Groups |
|
|---|
|
|
|
|
|---|
| Factors | Group with renal
recurrence (n=100) | Group without renal
recurrence (n=144) | P-values |
|---|
| AI, % | 8
(6–11) | 8
(5–10) | 0.436 |
| CI, % | 1 (0–3) | 1 (0–2) | 0.151 |
| Ratio of global
sclerosis, % | 0
(0–7.1) | 0 (0–7.56) | 0.366 |
| Ratio of segmental
sclerosis, % | 0 (0) | 0 (0) | 0.254 |
| Loop necrosis
(%) | 41/100 (41) | 58/141 (41.13) | 0.983 |
| Wire-loops (%) | 29/100 (29) | 37/140 (26.43) | 0.660 |
| Loop thrombus
(%) | 31/100 (31) | 28/141 (19.86) | 0.047a |
| Vasculopathy
(%) | 62/100 (62) | 88/144 (61.11) | 0.888 |
| AS (%) | 37/100 (37) | 67/144 (46.53) | 0.139 |
| IM (%) | 15/100 (15) | 17/144 (11.81) | 0.467 |
| NNV (%) | 10/100 (10) | 4/144 (2.78) | 0.017a |
Effect of different treatment schemes
and curative efficacies on renal recurrence
The number of patients receiving each type of
treatment in each group is displayed in Table III. The difference between the
group with recurrence and the group without recurrence during the
induction treatment and maintenance treatment periods was not
significant, Analysis by the Kaplan-Meier method revealed that the
difference in recurrence rate between patients receiving different
induction period treatment schemes was not significant and patients
who used glucocorticoids alone for maintenance treatment had a
higher recurrence rate compared with patients who used other
treatment schemes. However, the difference in the recurrence rate
between patients using glucocorticoids combined with different
immunosuppressants for maintenance treatment was not significant
(P>0.05; data not shown).
 | Table III.Comparison of induction and
maintenance treatment. |
Table III.
Comparison of induction and
maintenance treatment.
| Factors | Group with renal
recurrence (n=100) | Group without renal
recurrence (n=144) | P-value |
|---|
| Induction
treatment |
|
|
|
| P+CTX (%) | 44/100 (44.0) | 60/144 (41.6) | 0.845 |
| P+MMF (%) | 25/100 (25.0) | 27/144 (18.4) | 0.284 |
| P (%) | 24/100 (24.0) | 39/144 (27.0) | 0.679 |
| P+FK (%) | 5/100 (5.0) | 13/144 (9.0) | 0.385 |
| MMF+FK (%) | 2/100 (2) | 5/144 (3.0) | 0.405 |
| Maintenance
treatment |
|
|
|
| P+TW (%) | 63/82 (76.83) | 83/114 (72.81) | 0.524 |
| P (%) | 7/82 (8.54) | 7/114 (6.14) | 0.521 |
| P+MMF (%) | 5/82 (6.09) | 7/114 (6.14) | 0.990 |
| P+LFMT (%) | 3/82 (3.66) | 8/114 (7.02) | 0.488 |
| P+AZA (%) | 2/82 (2.44) | 4/114 (3.51) | 0.992 |
| P+CSA (%) | 1/82 (1.22) | 1/114 (0.87) | 0.896 |
| P+FK (%) | 1/82 (1.22) | 4/114 (3.51) | 0.587 |
Curative efficacies on renal
recurrence
A total of 18 patients achieved CR in the group with
renal recurrence, with an average CR time of 7 months (range,
4–10.25 months) and 82 patients achieved PR with an average PR time
of 6 months (range, 4–8.75 months). A total of 67 patients achieved
CR in the group without renal recurrence with an average CR time of
10 months (range, 6–12 months) and 77 patients achieved PR, with an
average PR time of 5 months (range, 2.5–7 months). PR durations
were significantly longer in patients experiencing recurrence
(P<0.01; Table IV). Analysis
using the Kaplan-Meier method indicated that patients achieving PR
had a higher recurrence rate than patients achieving CR (P=0.01;
data not shown).
 | Table IV.Rates and time of remission. |
Table IV.
Rates and time of remission.
| Factors | Group with renal
recurrence (n=100) | Group without renal
recurrence (n=144) | P-values |
|---|
| PR rate (%) | 82 (82) | 77 (51.39) | 0.023a |
| CR rate (%) | 18 (18) | 67 (46.53) | 0.001a |
| PR time | 6 (4–8.75) | 5 (2.5–7) | 0.002a |
| CR time | 7 (4–10.25) | 10 (6–12) | 0.318 |
Cox regression analysis of risk
factors for renal recurrence in patients with LN type IV
Univariate and multivariate Cox's regression
analysis indicated that SLE affecting the gastrointestinal tract,
increased levels of serum globulin and positive serum anti-SSB
antibody from the onset were risk factors for renal recurrence in
patients with LN type IV (Table
V).
 | Table V.Cox regression analysis of risk
factors for renal recurrence in patients with lupus nephritis type
IV. |
Table V.
Cox regression analysis of risk
factors for renal recurrence in patients with lupus nephritis type
IV.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Factors | RR (95% CI) | P-values | RR (95% CI) | P-values |
|---|
| Arthralgia | 0.519
(0.335–0.804) | 0.003a | 0.689
(0.232–1.253) | 0.198 |
| Globulin | 1.049
(1.021–1.077) | 0.001a | 1.038
(1.004–1.073) | 0.028a |
| Anti-SSB
antibody | 0.353
(0.186–0.671) | 0.001a | 0.386
(0.191–0.778) | 0.008a |
| Gastrointestinal
tract | 0.202
(0.063–0.648) | 0.007a | 0.192
(0.058–0.640) | 0.007a |
Discussion
The present study demonstrated that patients with LN
type IV had a renal recurrence rate of ≤28.5% and the average
recurrence time was 30 months. Following the induction period, 244
patients achieved remission; however 100 patients experienced renal
recurrence during maintenance treatment, which is consistent with
the results of a previous study (12). The current study also demonstrated
that patients with LN type IV who achieved PR rather than CR were
more likely to experience relapse, which was also demonstrated in a
study by Illei et al (13).
It has previously been demonstrated that male
patients with SLE and early renal damage and/or hypertension who
received incorrect treatment with cytotoxic drugs and underwent a
shorter induction treatment course were prone to renal recurrence
during the disease course (14).
Additionally, African Americans with LN type IV have a high risk of
recurrence ≤1 year following remission (15). However, to the best of our knowledge,
it remains unknown whether certain ethnicities are more likely to
experience renal recurrence.
Age at onset may also affect renal recurrence. A
study conducted in South Korea demonstrated that patients with LN
type IV aged <28 years old were more likely to experience renal
recurrence (16). However, the
results of the present study did not identify an association
between age and renal recurrence in patients with LN type IV.
Furthermore, baseline clinical manifestations and associated
laboratory indicators in patients with or without renal recurrence
were compared and it was demonstrated that hypertension, renal
impairment, hemuresis, extra renal damage to the blood system and
skin damage at onset had no effect on the incidence of renal
recurrence. However, patients with LN type IV that affected the
gastrointestinal tract had higher renal recurrence rates during the
course of the disease. Varying degrees of anorexia, nausea,
vomiting and other gastrointestinal symptoms are present in ~50% of
patients with SLE. In addition to the direct effects of SLE, the
aforementioned manifestations are often associated with the toxic
side effects of drugs (17). The
results of the present study differ to those of previous studies
(17), as no differences in renal
recurrence were observed between patients with or without
gastrointestinal syndrome. Therefore, it remains controversial
whether gastrointestinal symptoms indicate the presence of renal
recurrence in the course of LN type IV for patients at onset or in
stable conditions following remission and further studies are
required to determine this. The present study demonstrated that
differences in laboratory indices, including proteinuria, serum
creatinine and plasma albumin did not influence the likelihood of
renal recurrence. However, patients with LN type IV experiencing
recurrence had higher globulin levels compared with patients
without recurrence and patients with high globulin levels had
increased renal recurrence rates. Therefore, increased levels of
serum globulin may be a risk factor for renal recurrence in
patients with LN type IV. Furthermore, the present study
demonstrated that patients with LN type IV with NNV or thrombus in
the loop were prone to experiencing renal recurrence. Thus,
increased clinical attention should be given to patients with this
form of the disease.
The presence of positive anti-nucleosome antibody or
a significant increase in levels of anti-double stranded-DNA
(anti-ds-DNA) antibody may be used to predict recurrence (18). It has been demonstrated that
anti-ds-DNA antibody titer significantly increases 8–10 weeks prior
to recurrence (18). Normal serum
complement levels and low anti-ds-DNA antibody titer in patients
with SLE at onset indicates a reduction in the risk of recurrence
(19). Coremans et al
(20) identified that a titer of
anti-C1q antibody may predict the recurrence of LN and that this
value may be superior to anti-ds-DNA antibody. However, the results
of the present study did not identify any effect of the differences
in the aforementioned antibody levels on renal recurrence in
patients with LN type IV. This may be explained by the number and
ethnicity of the patients in the current study, as well as the
method of antibody detection. The current study demonstrated that
patients with LN type IV and recurrence had higher levels of
positive RNP antibody compared with patients without recurrence and
patients with positive anti-RNP and anti-SSB antibodies experienced
increased recurrence rates. The anti-RNP antibody is associated
with Raynaud's phenomenon and pulmonary arterial hypertension,
which are risk factors for mixed connective tissue disease (MCTD)
and may also indicate vasculopathy (21). Furthermore, anti-RNP antibodies serve
a role in inherent and adaptive immune responses and indicate the
possible pathogenesis of MCTD (21).
Anti-RNP antibodies are also associated with kidney damage
(22) however their role in LN type
IV and whether they are able to predict renal recurrence remains
unknown. Anti-SSA antibodies are closely associated with anti-SSB
antibodies, which are associated with blood system disorders,
proteinuria, rash and pericarditis in SLE (23). Further studies are required to
determine whether the occurrence of anti-SSB antibodies at the
onset of the disease in patients with LN type IV influences the
outcome of renal recurrence.
The effect of the combination treatment of
glucocorticoids with routine immunodepressants on the recurrence of
LN remains controversial. It has been identified that patients
undergoing combination treatment of glucocorticoids with
acetazolamide have a higher recurrence rate compared with patients
receiving glucocorticoids combined with CTX as an induction therapy
(24). Chan et al (25) demonstrated that the recurrence rates
in patients with proliferative LN did not differ significantly
between patients using glucocorticoids with MMF for induction and
maintenance treatment, and those using glucocorticoids and CTX for
induction treatment and AZA for maintenance treatment over a 5-year
follow-up period. Dooley et al (26) demonstrated that, after 6 months
induction therapy with combination treatment of glucocorticoids and
MMF or CTX, patients who used glucocorticoids with MMF for
maintenance treatment had a significantly lower recurrence rate
compared with patients who used glucocorticoids with AZA. Yap et
al (27) demonstrated that
following MMF induction treatment, patients receiving AZA for
maintenance treatment had an increased renal recurrence rate. In
addition, a recent study based on Chinese populations with LN
indicated that if AZA replaced MMF during the first 24 months of
induction treatment, the risk of renal recurrence increased
(28).
The use of antimalarial drugs may also reduce
recurrence rates, including the renal recurrence rate (29). Subsequently, the American College of
Rheumatology and European League Against Rheumatism guidelines
recommend that unless there are contraindications, all patients
with LN should be treated with antimalarial drugs (30). However, it remains unclear whether
the use of hydroxychloroquine in the Asian population reduces
recurrence and only a small number of related studies have been
conducted (30). To determine
whether prolonged maintenance treatment reduces renal recurrence
rate, one study demonstrated that the use of CTX for maintenance
treatment extended to 30 months may lower the renal recurrence rate
(31). Patients with LN undergoing
treatment MMF for <24 months were more prone to renal recurrence
compared with patients with LN who received MMF for induction
therapy and continued to use MMF for a longer duration (31). However, a longer period of
maintenance treatment may result in an increased risk of side
effects caused by the accumulation of drugs (32). The present study demonstrated that
among routine induction treatment schemes using glucocorticoids
with various immunosuppressants, the difference in renal recurrence
was not significant. However, the renal recurrence rate in patients
who used glucocorticoids alone for maintenance treatment was higher
than in patients who used glucocorticoids with immunosuppressants.
At present, it remains controversial whether the use of
glucocorticoids combined with immunosuppressant therapy decreases
the risk of renal recurrence. Thus, routine immunosuppressant
therapy has limited effects in reducing renal recurrence.
Individual target therapies for the pathogenesis of LN, such as
treatment with rituximab, may reduce renal recurrence rates in the
future (33).
There were certain limitations of the current study.
The participants consisted solely of patients with LN type IV and
the clinical predictors analyzed included baseline clinical,
pathological and laboratory results and treatment situations only.
The association between changes in the aforementioned indicators
during follow-up and the time of renal recurrence was not included
in this analysis. Furthermore, these data came only from a
single-center analysis and thus require further validation.
In conclusion, the current study comprehensively
evaluated a series of clinical indicators of LN type IV, including
clinical manifestations and laboratory indices, histopathological
changes and the combination treatment of glucocorticoids with
immunosuppressants. It was demonstrated that the number of clinical
indicators that may be used to predict renal recurrence in patients
with LN remains limited. Therefore, further investigations into
novel biomarkers for the early prediction of LN renal recurrence
are required.
Acknowledgements
The present study was supported by the National
Natural Science Foundation of China, (grant no. 81100521).
References
|
1
|
Tan EM, Cohen AS, Fries JF, Masi AT,
McShane DJ, Rothfield NF, Schaller JG, Talal N and Winchester RJ:
The 1982 revised criteria for the classification of systemic lupus
erythematosus. Arthritis Rheum. 25:1271–1277. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hochberg MC: Updating the American College
of Rheumatology revised criteria for the classification of systemic
lupus erythematosus. Arthritis Rheum. 40:17251997. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tsang-A-Sioje MW and Bultink IE: Systemic
lupus erythematosus: Review of synthetic drugs. Expert Opin
Pharmacother. 16:2793–2806. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chan RW, Lai FM, Li EK, Tam LS, Chow KM,
Li PK and Szeto CC: The effect of immunosuppressive therapy on the
messenger RNA expression of target genes in the urinary sediment of
patients with active lupus nephritis. Nephrol Dial Transplant.
21:1534–1540. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Alarcón GS, Calvo-Alén J, McGwin G Jr,
Uribe AG, Toloza SM, Roseman JM, Fernández M, Fessler BJ, Vilá LM,
Ahn C, et al: Systemic lupus erythematosus in a multiethnic cohort:
LUMINA XXXV. Predictive factors of high disease activity over time.
Ann Rheum Dis. 65:1168–1174. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Griffiths B, Mosca M and Gordon C:
Assessment of patients with systemic lupus erythematosus and the
use of lupus disease activity indices. Best Pract Res Clin
Rheumatol. 19:685–708. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lisnevskaia L, Murphy G and Isenberg D:
Systemic lupus erythematosus. Lancet. 384:1878–1888. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Weening JJ, D'Agati VD, Schwartz MM,
Seshan SV, Alpers CE, Appel GB, Balow JE, Bruijn JA, Cook T,
Ferrario F, et al: The classification of glomerulonephritis in
systemic lupus erythematosus revisited. Kidney Int. 65:521–530.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Austin HA III, Muenz LR, Joyce KM,
Antonovych TT and Balow JE: Diffuse proliferative LN:
Identification of specific pathologic features affecting renal
outcome. Kidney Int. 25:689–695. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Descombes E, Droz D, Drouet L, Grünfeld JP
and Lesavre P: Renal vascular lesions in lupus nephritis. Medicine
(Baltimore). 76:355–368. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Parikh SV, Nagaraja HN, Hebert L and Rovin
BH: Renal flare as a predictor of incident and progressive CKD in
patients with lupus nephritis. Clin J Am Soc Nephrol. 9:279–284.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hahn BH, McMahon MA, Wilkinson A, Wallace
WD, Daikh DI, Fitzgerald JD, Karpouzas GA, Merrill JT, Wallace DJ,
Yazdany J, et al: American College of Rheumatology guidelines for
screening, treatment, and management of lupus nephritis. Arthritis
Care Res (Hoboken). 64:797–808. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Illei GG, Takada K, Parkin D, Austin HA,
Crane M, Yarboro CH, Vaughan EM, Kuroiwa T, Danning CL, Pando J, et
al: Renal flares is common in patients with severe proliferative
lupus nephritis treated with pulse immunosuppressive therapy:
Long-term followup of a cohort of 145 patients participating in
randomized controlled studies. Arthritis Rheum. 46:995–1002. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gibson KL, Gipson DS, Massengill SA,
Dooley MA, Primack WA, Ferris MA and Hogan SL: Predictors of
relapse and end stage kidney disease in proliferative lupus
nephritis: Focus on children, adolescents, and young adults. Clin J
Am Soc Nephrol. 12:1962–1967. 2009. View Article : Google Scholar
|
|
15
|
Contreras G, Tozman E, Nahar N and Metz D:
Maintenance therapies for proliferative lupus nephritis:
Mycophenolate mofetil, azathioprine and intravenous
cyclophosphamide. Lupus. 14 Suppl 1:S33–S38. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Moon SJ, Park HS, Kwok SK, Ju J, Choi BS,
Park KS, Min JK, Kim HY and Park SH: Predictors of renal relapse in
Korean patients with lupus nephritis who achieved remission six
months following induction therapy. Lupus. 22:527–537. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Imran TF, Yick F, Verma S, Estiverne C,
Ogbonnaya-Odor C, Thiruvarudsothy S, Reddi AS and Kothari N: Lupus
nephritis: An update. Clin Exp Nephrol. 20:1–13. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Pan N, Amigues I, Lyman S, Duculan R, Aziz
F, Crow MK and Kirou KA: A surge in anti-dsDNA titer predicts a
severe lupus flare within six months. Lupus. 23:293–298. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Borg Ter EJ, Horst G, Hummel EJ, Limburg
PC and Kallenberg CG: Measurement of increases in
anti-double-stranded DNA antibody levels as a predictor of disease
exacerbation in systemic lupus erythematosus: A long-term,
prospective study. Arthritis Rheum. 33:634–643. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Coremans IE, Spronk PE, Bootsma H, Daha
MR, van der Voort EA, Kater L, Breedveld FC and Kallenberg CG:
Changes in antibodies to C1q predict renal relapses in systemic
lupus erythematosus. Am J Kidney Dis. 26:595–601. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Valões CC, Molinari BC, Pitta AC,
Gormezano NW, Farhat SC, Kozu K, Sallum AM, Appenzeller S, Sakamoto
AP, Terreri MT, et al: Anti-ribosomal P antibody: A multicenter
study in childhood-onset systemic lupus erythematosus patients.
Lupus. 26:484–489. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Keith MP, Moratz C and Tsokos GC: Anti-RNP
immunity: Implications for tissue injury and the pathogenesis of
connective tissue disease. Autoimmunity Rev. 6:232–236. 2007.
View Article : Google Scholar
|
|
23
|
Lu R, Robertson JM, Bruner BF, Guthridge
JM, Neas BR, Nath SK, Kelly JA, Sivils Moser KL, Chakravarty EF,
Kamen DL, et al: Multiple autoantibodies display association with
lymphopenia, proteinuria, and cellular casts in a large, ethnically
diverse SLE patient cohort. Autoimmune Dis.
2012:8196342012.PubMed/NCBI
|
|
24
|
Grootscholten C, Ligtenberg G, Hagen EC,
van den Wall Bake AW, de Glas-Vos JW, Bijl M, Assmann KJ, Bruijn
JA, Weening JJ, van Houwelingen HC, et al:
Azathioprine/methylprednisolone versus cyclophosphamide in
proliferative lupus nephritis. Kidney Int. 70:732–742. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Chan TM, Tse KC, Tang CS, Mok MY and Li
FK: Hong Kong Nephrology Study Group: Long-term study of
mycophenolate mofetil as continuous induction and maintenance
treatment for diffuse proliferative lupus nephritis. J Am Soc
Nephrol. 16:1076–1084. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Dooley MA, Jayne D, Ginzler EM, Isenberg
D, Olsen NJ, Wofsy D, Eitner F, Appel GB, Contreras G, Lisk L, et
al: Mycophenolate versus azathioprine as maintenance therapy for
lupus nephritis. N Engl J Med. 365:1886–1895. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yap DY, Ma MK, Mok MM, Tang CS and Chan
TM: Long-term data on corticosteroids and mycophenolate mofetil
treatment in lupus nephritis. Rheumatology (Oxford). 52:480–486.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Yap DY and Chan TM: Lupus nephritis in
asia: Clinical features and management. Kidney Dis (Basel).
2:100–109. 2015. View Article : Google Scholar
|
|
29
|
Ponticelli C and Moroni G:
Hydroxychloroquine in systemic lupus erythematosus (SLE). Expert
Opin Drug Saf. 3:411–419. 2017. View Article : Google Scholar
|
|
30
|
Bertsias GK, Tektonidou M, Amoura Z,
Aringer M, Bajema I, Berden JH, Boletis J, Cervera R, Dörner T,
Doria A, et al: Joint European League Against Rheumatism and
European Renal Association-European Dialysis and Transplant
Association (EULAR/ERA-EDTA) recommendations for the management of
adult and paediatric lupus nephritis. Ann Rheum Dis. 71:1771–1782.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Boumpas DT, Austin HA III, Vaughn EM,
Klippel JH, Steinberg AD, Yarboro CH and Balow JE: Controlled trial
of pulse methylprednisolone versus two regimens of pulse
cyclophosphamide in severe lupus nephritis. Lancet. 340:741–745.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chen Y, Sun J, Zou K, Yang Y and Liu G:
Treatment for lupus nephritis: An overview of systematic reviews
and meta-analyses. Rheumatol Int. 7:1089–1099. 2017. View Article : Google Scholar
|
|
33
|
Rovin BH and Parikh SV: Lupus nephritis:
The evolving role of novel therapeutics. Am J Kidney Dis.
63:677–690. 2014. View Article : Google Scholar : PubMed/NCBI
|