Introduction
Excessive alcohol consumption is a global problem
that accounted for 3.3 million deaths in 2012 (World Health
Organization 2014). Alcoholic liver disease (ALD) starts with a
fatty liver, fibrosis and cirrhosis, as well as a severe form of
ALD known as alcoholic hepatitis, and/or eventually hepatocellular
carcinoma (HCC) (1). There were
approximately 75,766 cases of alcohol-related death in 2001 in the
United States according to the National Institute on Alcohol Abuse
and Alcoholism (NIAAA) (2).
Epithelial-mesenchymal transition (EMT) is involved
in chronic liver injury; evidence shows that hepatocytes in the
adult liver undergo EMT. EMT is a complicated process, with the
loss of cell-cell junctions and polarity, and results in the
formation of migratory mesenchymal cells with invasive
characteristics (3). Transforming
growth factor-beta (TGF-β) initiates intracellular signals that
bind to its receptors through the activation of downstream mediator
Mothers Against DPP Homolog (Smad) proteins (4). Smads are important intracellular
effectors of the TGF-β1 signaling superfamily (5). Generally, Smad2 and Smad3 are
phosphorylated by TGF-β receptors and are then translocated to the
nucleus after forming a complex with Smad4 (6). TGF-β/Smad3 plays a critical role in EMT
during fibrosis, and therefore, a potential therapeutic approach
for preventing and treating fibrosis is to develop TGF-β/Smad3
signaling inhibitors by targeting EMT.
Qinggan huoxue recipe (QGHXR), a traditional Chinese
medicinal (TCM) formula, consists of bupleurum, scutellaria, red
sage, carapax trionycis and radix puerariae, and shows
pharmacological effects in treating ALD, including reversible
steatosis, improving lipid peroxidation and inflammatory cytokines
(7,8). A recent study showed that QGHXR
improved the pathological changes of ALD rats through the
Lipopolysaccharides (LPS)-Kupffer cells signal pathway (9). Furthermore, an in vivo study
detected that QGHXR inhibited EMT in ALD rats by regulating the
TGF-β1/Smad pathway (10).
In the present study, we detected the expression of
molecules related to the TGF-β/Smad3 signaling and EMT in
acetaldehyde-treated L02 cells. Baicalin, salvianic acid, puerarin,
and saikosaponin are the major components from the QGHXR formula,
and recent studies show their roles in improving liver injury. For
example, baicalin exerts a hepatoprotective role in alcohol-induced
liver injury by inhibiting oxidative stress, the inflammatory
response, and the regulation of the sonic hedgehog pathway
(11). Salvianic acid produces a
protective role on acute hepatic injury induced by CCl4 via an
antioxidative mechanism (12).
Puerarin improves chronic alcohol-induced liver injury in mice via
antioxidant, anti-inflammatory, and anti-apoptotic mechanisms
(13). Saikosaponin exerts a
protective role in the septic process by suppressing TNF-α and IL-6
concentrations in the intestines of septic rats via inhibiting the
NOD2/NF-κB signaling pathway (14).
However, it is unclear whether those components improve alcoholic
liver injury via EMT or not. Therefore, we analyzed the effect of
the four major components of QGHXR on TGF-β/Smad3 proteins and EMT
proteins. Furthermore, snail siRNA was transferred into
acetaldehyde-treated HepG2 cells to illustrate the changes to the
TGF-β/Smad3 pathway by the four components.
Materials and methods
Cell culture and treatment
The cells were purchased from Cell Resource Center,
Shanghai Science Research Center, Chinese Academy of Sciences
(Shanghai, China). L02 and HepG2 (human liver cancer cells) cells
were seeded in Dulbecco's modified Eagle's medium (DMEM) with 10%
fetal bovine serum (FBS) and 100 units/ml penicillin/streptomycin
(Sigma-Aldrich; Merck KGaA, Darmstadt, Germany). The cells were
incubated at 37°C in 5% CO2.
Cell proliferation
The proliferation of the L02 s cells was evaluated
using the 3-(4,5-Dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium
bromide (MTT) method. The cells were seeded at 2 × 105
cells per well in 200 µl of DMEM into 96-well culture plates and
were cultured overnight. The medium was replaced with 20 µl of
fresh medium containing 5 mg/ml MTT (Sigma-Aldrich; Merck KGaA) at
different time points. The supernatants were removed four h later.
Each well was supplemented with 100 µl of dimethylsulfoxide to
dissolve the crystals. Cell viability was determined at 490 and 630
nm. All the experiments were performed in triplicate. Therapeutic
agents clinically used against acetaldehyde were examined for
efficacy by determining the 50% inhibitory concentration (IC50)
values.
RNA preparation and reverse
transcription-quantitative polymerase chain reaction (RT-qPCR)
analysis
Total RNA was extracted from the cells using the
Trizol reagent (Invitrogen; Thermo Fisher Scientific, Inc.,
Waltham, MA, USA) and was diluted to 200 ng/ml. Then, the PCR
amplification was performed using the SYBR® PrimeScript™
RT-PCR kit (Takara Biotechnology Co., Ltd., Dalian, China) and was
conducted using the Applied Biosystems real-time PCR machine
(ABI7500; Applied Biosystems; Thermo Fisher Scientific, Inc.). The
reactions were performed as follows: 95°C for 3 min, with 34 cycles
of 95°C for 30 sec; 65°C for 40 sec; and 72°C for 40 sec. The
results were analyzed using the comparative threshold cycle value
method (2−ΔΔCq) (15). The primer sequences are listed in
Table I. Glyceraldehyde 3-phosphate
dehydrogenase (GAPDH) was used as the loading control.
 | Table I.Sequence of primers. |
Table I.
Sequence of primers.
| Genes | Sequence | Bp |
|---|
| E-cadherin |
|
|
| F |
5′-TGAGAACGAGGCTAACG-3′ | 358 |
| R |
5′-GCTGTGGAGGTGGTGAG-3′ |
|
| Vimentin |
|
|
| F |
5′-CGCCAGATGCGTGAAAT-3′ | 119 |
| R |
5′-CGAAGGTGACGAGCCATT-3′ |
|
| Fibronectin |
|
|
| F |
5′-CAGGACGGACATCTTTG-3′ | 232 |
| R |
5′-TCTGGTCGGCATCATAG-3′ |
|
| TGF-β1 |
|
|
| F |
5′-GCGATACCTCAGCAACCG-3′ | 121 |
| R |
5′-AAGGCGAAAGCCCTCAAT-3′ |
|
| Smad3 |
|
|
| F |
5′-CCTTTCAGGTAACCGTCTT-3′ | 168 |
| R |
5′-TTAGCCCATCATCTCCC-3′ |
|
| Snail |
|
|
| F |
5′-CCCCACAGGACTTTGATG-3′ | 212 |
| R |
5′-GTGAGTCTGTCAGCCTTTGTC-3′ |
|
| Occludin |
|
|
| F |
5′-TCAGGGTGTTTCTGTTGG-3′ | 123 |
| R |
5′-GAAATGGAAGGGATGTCG-3′ |
|
| ZO-1 |
|
|
| F |
5′-AGATGAACGGGCTACGC-3′ | 173 |
| R |
5′-ACCGCTGGTCAGGAGAT-3′ |
|
| Claudin-1 |
|
|
| F |
5′-CAGTTAGGAGCCTTGATGC-3′ | 128 |
| R |
5′-CGGCACAGGGAGTAGGA-3′ |
|
Western blot analysis
The cells were collected and homogenized in cell
lysis buffer (Beyotime Institute of Biotechnology, Haimen, China).
The supernatants were collected after centrifugation at 12,000 × g
for 30 min at 4°C. The bicinchoninic acid (BCA) protein assay kit
(Beyotime Institute of Biotechnology) was used to measure the
concentration of the protein. A total of 60 µg of the protein
samples was separated electrophoretically by 10% SDS-PAGE and was
then transferred onto polyvinylidene difluoride membranes.
Non-specific binding was blocked with 5% nonfat milk in
Tris-buffered saline containing Tween 20 (TBST) for 2 h at room
temperature, and then, the membranes were incubated with a primary
antibody against snail (1:1,000; Abcam, Cambridge, MA, USA) at 4°C
overnight. The membranes were then incubated with a secondary
antibody. Finally, the blots were visualized with an enhanced
chemical luminescence (ECL) system (GE Healthcare, Chicago, IL,
USA).
Transfection of small interfering RNA
(siRNA)
To further analyze the role of snail in EMT, the
siRNAs targeting snail was obtained from Shanghai GenePharma Co.,
Ltd, (Shanghai, China). When the HepG2 cells were grown to almost
30% confluency, the siRNAs were transfected using lipofectamine
2000 (Invitrogen; Thermo Fisher Scientific, Inc.). To verify the
transfection efficiency, RT-qPCR and western blotting were
performed.
Statistical analysis
The group values are shown as the mean ± standard
deviation (SD). A one-way analysis of variance with post hoc tests
by Student-Newman-Keuls test was used to evaluate the significance
of the differences with SPSS v.17 software (SPSS, Inc., Chicago,
IL, USA). P<0.05 was considered to indicate a statistically
significant difference. The histograms were generated with GraphPad
Prism v.5.0 software (GraphPad Software, Inc., La Jolla, CA,
USA).
Results
Acetaldehyde-induced EMT in human L02
cells
To establish an EMT model, different concentrations
of acetaldehyde, including 0.0, 0.5, 1.0, 2.0, and 4.0 mmol/l were
added into the L02 cells. Cell proliferation was evaluated by an
MTT assay. We found that 2.127 mmol/l was the IC50 concentration of
the acetaldehyde as shown in Fig. 1.
Therefore, we used ¼ of the IC50, i.e., 0.532 mmol/l acetaldehyde,
for the subsequent experiment of the EMT model of L02.
Concentration selection of the four
medicines
Furthermore, in order to select the best
concentration of the four medicines, cell proliferation was
analyzed by an MTT assay after treatments with different
concentrations. As shown in Fig. 2,
the IC50 concentration of baicalin, salvianic acid, puerarin and
saikosaponin, was 150, 79, 695, and 66.3 µg/ml respectively. Thus,
½ of the IC50 concentration of the four medicines, i.e., 75, 39.5,
347.5, and 33.15 µg/ml, was added into the acetaldehyde-treated L02
cells for 3, 6, 12, 24, and 48 h. Inhibition of cell proliferation
was found at 48 h, and thus, cells in the 48-h treatment were
collected for further experiments.
Baicalin and puerarin counteract
acetaldehyde-induced EMT in L02 cells
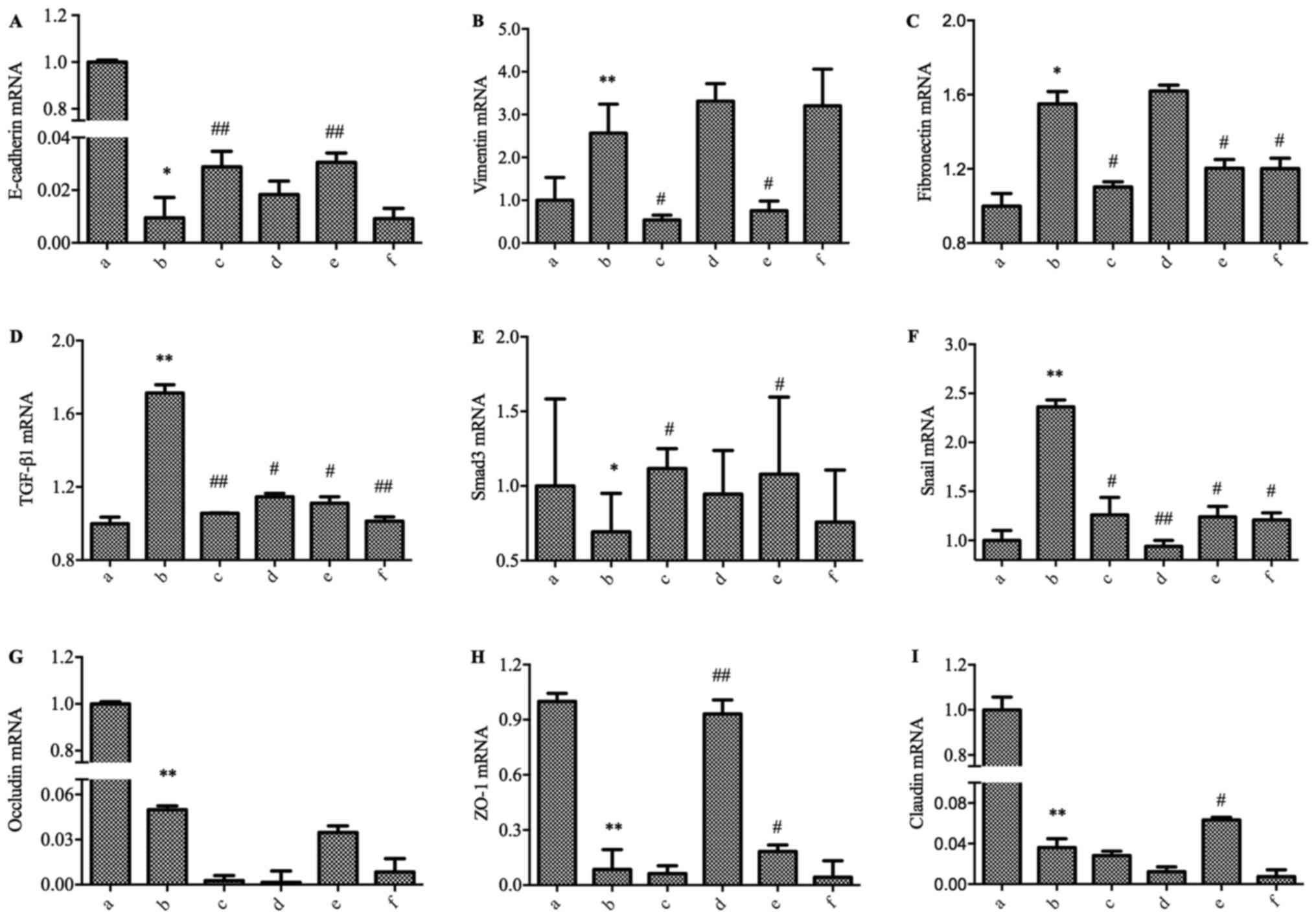
We treated the L02 cells with acetaldehyde for 48 h
in culture. We then detected the expressions of E-cadherin,
vimentin and fibronectin using RT-qPCR. The gene expression of
E-cadherin was significantly downregulated, and the expression of
vimentin and fibronectin were significantly increased in the L02
cells with acetaldehyde treatment (Fig.
3A-C). These data indicated that EMT occurred in the L02 cells
after the treatment acetaldehyde. To further understand the
involvement of the four medicines in improving acetaldehyde-induced
EMT in L02 cells, the related molecules involved in TGF-β1/Smads
signaling were examined. As shown in Fig. 3D-F, the RT-qPCR experiment indicated
that the mRNA levels of TGF-β1 and Snail were significantly
increased in the acetaldehyde-treated cells, while the level of
Smad3 decreased significantly. These data hinted that TGF-β1/Smad3
signaling might play an important role in the development of EMT.
At the same time, the mRNA expression of the markers of tight
junctions, including occludin, ZO-1 and claudin, decreased
significantly (Fig. 3G-I).
 | Figure 3.Effect of the four medicines in the
TGF-βl-Snail-EMT signal pathway in acetaldehyde-treated L02 cells
by RT-qPCR. The cells were treated with 0.064 mmol/l of
acetaldehyde and were then treated with the four medicines for 48
h. (A) E-cadherin; (B) vimentin; (C) fibronectin; (D) TGF-βl; (E)
Smad3; (F) snail; (G) occludin; (H) ZO-1; (I) claudin. Groups: a,
Normal; b, Model; c, Baicalin; d, Salvianic acid; e, Puerarin; f,
Saikosaponin. *P<0.05, **P<0.01, when compared with the
Normal group; #P<0.05, ##P<0.01, when
compared with the Model group. EMT, epithelial-mesenchymal
transition, RT-qPCR, reverse transcription-quantitative polymerase
chain reaction. |
After treatment with the four medicines in the high
acetaldehyde-treated cells, the related molecules involved in the
TGF-β1/Smad3 pathway were regulated differently (Fig. 3). Barcacin regulated the mRNA level
of TGF-βl, Smad3, and Snail and then suppressed the EMT process,
which was accompanied by the upregulated mRNA level of E-cadherin
and the downregulation of fibronectin and vimentin, but with no
significant regulation of occludin, ZO-1 and claudin. Salvianic
acid did not show an obvious effect on the EMT marker expression,
including E-cadherin, vimentin, and fibronectin. However, salvianic
acid did regulate the mRNA of TGF-βl, Snail, and ZO-1. Puerarin
regulated the mRNA level of TGF-βl, Smad3, and Snail and then
suppressed the EMT process, which was accompanied by an increased
mRNA level of E-cadherin and decreased levels of vimentin and
fibronectin, along with an increased level of ZO-1 and claudin.
Saikosaponin did not show an obvious effect on E-cadherin and
vimentin, but it regulated the mRNA of fibronectin, TGF-βl, and
Snail. None of the treatments regulated the expression of
occludin.
Selection of the snail siRNA
To sift out the best snail siRNA, we verified the
effect of silencing snail using RT-qPCR and western blot methods
(Fig. 4). Then, we transferred six
siRNAs into the cells at a 50 nM or 100 nM concentration.
Twenty-four h later, the mRNA expression of snail was detected by
RT-qPCR, and siRNA6 was the best silencing gene at 100 nM (Fig. 4A). Furthermore, we transferred the
six siRNAs into the cells at a 100 nM concentration, and 48 h
later, a western blot was used to detect the protein expression of
snail. Similar to the PCR result, siRNA6 was the best (Fig. 4B). Then, we used siRNA6 to silence
snail, and the sequence was forward: 5′-GCCUUCAACUGCAAAUACUdTdT-3′
and reverse: 5′-AGUAUUUGCAGUUGAAGGCdTdT-3′.
Baicalin and puerarin counteract
aldehyde-induced EMT in HepG2 cells via snail
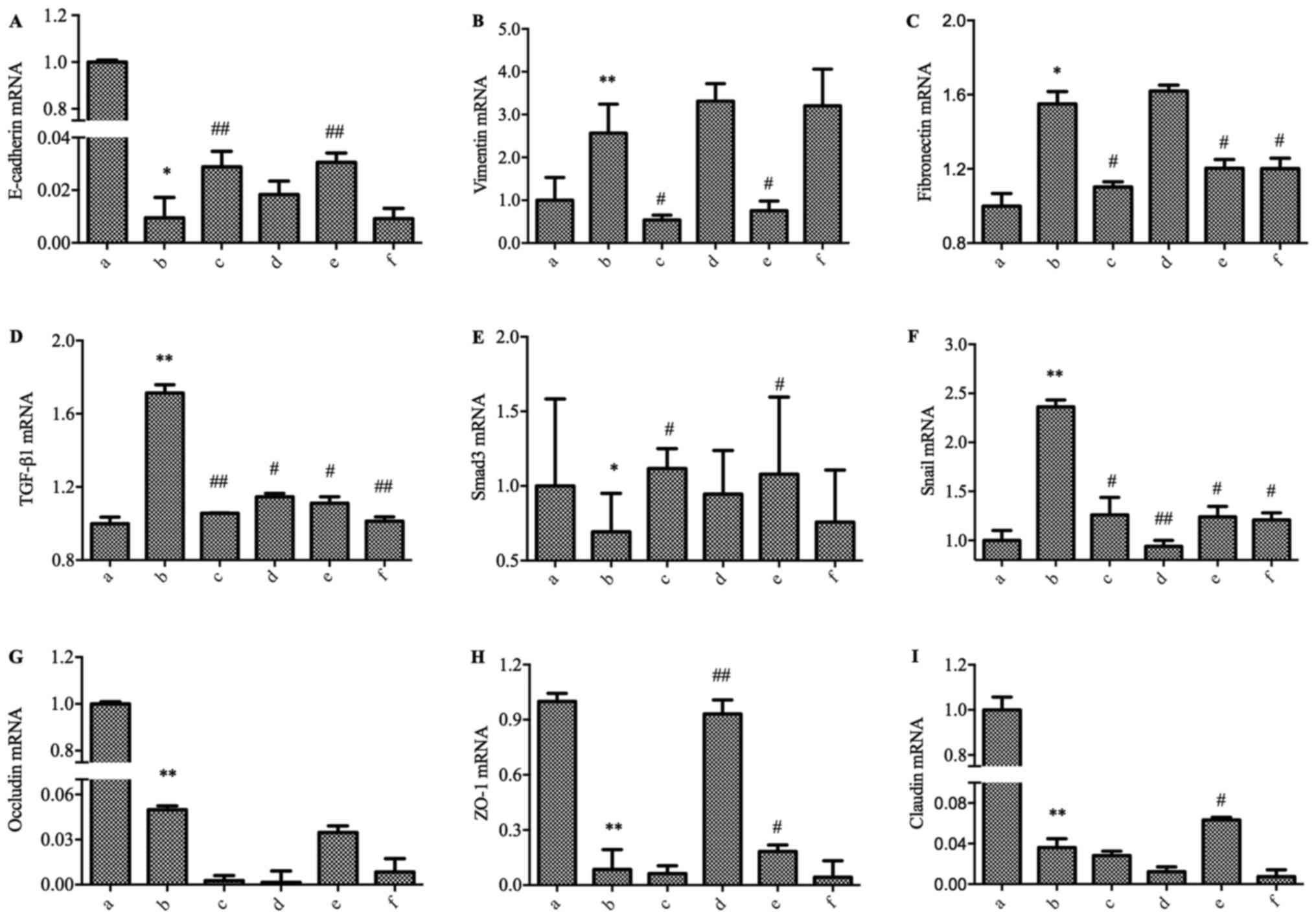
To further understand the role of snail, we used RNA
interference technology to silence the expression of snail. Six
groups were established, including the normal control, model,
snail−/−, balcalin, balcalin + snail−/−,
puerarin, and puerarin + snail−/−groups. As shown in
Fig. 5, the mRNA expression of snail
was significantly decreased in the snail−/− group.
Similar with the former results, in the model group, E-cadherin
mRNA was significantly downregulated, and vimentin and fibronectin
mRNA were significantly upregulated in the HepG2 cells with
acetaldehyde treatment compared to the normal control group
(Fig. 5A-C). As shown in Fig. 5D-F, the RT-qPCR experiment indicated
that the levels of TGF-β1 and snail were significantly increased in
the acetaldehyde-treated cells, while the level of the Smad3 gene
decreased significantly. Furthermore, the mRNA expression of
occludin, ZO-1 and claudin decreased significantly (Fig. 5G-I). When the snail gene was silent,
different changes were found in the mRNA expression of those
related molecules. They did not show results similar to the model
group.
 | Figure 5.Effect of the four medicines on the
TGF-βl-Snail-EMT signal pathway in acetaldehyde-treated
snail−/− HepG2 cells by RT-PCR (A) E-cadherin; (B)
vimentin; (C) fibronectin; (D) TGF-βl; (E) Smad3; (F) snail; (G)
occludin; (H) ZO-1; (I) claudin. Groups: a, Normal; b, Model; c,
Snail−/−; d, Baicalin; e, Baicalin+snail−/−;
f, Puerarin; g, Puerarin+snail−/−. *P<0.05,
**P<0.01, when compared with the Normal group;
#P<0.05, ##P<0.01, when compared with
the Model group. TGF-β, transforming growth factor-beta. |
In summary, barcacin regulated the mRNA level of
TGF-βl and snail and then suppressed the EMT process, which was
accompanied with an increased mRNA level of E-cadherin and
decreased levels of vimentin and fibronectin but with no
significant regulation of Smad3, occludin, ZO-1 and claudin.
Puerarin regulated the mRNA level of TGF-βl, Smad3, and snail and
then suppressed the EMT process, which was accompanied with an
increased mRNA level of E-cadherin and decreased levels of vimentin
and fibronectin, as well as increased levels of occludin, ZO-1 and
claudin. However, when the snail gene was silent, barcacin and
puerarin did not show obvious effects in the acetaldehyde-treated
cells.
Discussion
In the present study, an in vitro
acetaldehyde-induced EMT model was established, and we investigated
the effects of four major compounds on hepatocyte EMT and aimed to
explore the potential molecular mechanisms.
EMT is a process by which the mesenchymal phenotype
is acquired by epithelial cells, with the characteristics of the
loss of cell-cell adhesion, remodeling of the cytoskeleton, and
increased migratory properties (16). EMT is an important step in the
development of hepatic fibrosis. EMT is characterized by the
decreased expression of the epithelial marker E-cadherin and the
increased expression of mesenchymal markers, such as α-SMA,
fibronectin, collagen I and vimentin (17,18). A
recent study showed that hepatic stellate cell (HSC) conditioned
medium activates c-myc through the ERK1/2 signaling pathway in
hepatoma cells, promoting cell proliferation, invasion and
migration, and inducing EMT (19).
In the present study, the expression of E-cadherin decreased, while
vimentin and fibronectin increased in acetaldehyde-treated L02 and
HepG2 cells using high concentrations of acetaldehyde. The results
indicated that an EMT model was successfully established using
acetaldehyde in vitro.
EMT is often associated with increases in the TGF-β
signaling pathway, and TGF-β drives EMT, in part, through
Smad-mediated reprogramming of gene expression (20–23). In
the present study we mainly paid more attention to the role of
Snail in the signaling pathway, thus we blocked Snail and further
explored its role in the pathway.
First, we detected that acetaldehyde induced a
mesenchymal cell characteristic in hepatocytes, which was
accompanied by upregulated vimentin, fibronectin and snail and
downregulated E-cadherin. At the same time, the TGF-β1 gene
expression in the acetaldehyde-treated cells increased.
Acetaldehyde promoted the phosphorylation of Smad-3, and the
TGF-β1/Smad3 pathway was then activated.
More and more evidence shows that TCM exerts effects
in treating fibrosis. For example, curcumin inhibits cobalt
chloride-induced EMT by regulating TGF-β/Smad signaling in
hepatocytes (24), and salvianolic
acid B prevents EMT through the TGF-β 1 pathway in vivo and
in vitro (25). Our results
showed that baicalin and puerarin improved the mesenchymal
characteristics through the TGF-β1/Smad3 pathway. Salvianic acid
and saikosaponin did not show obvious effects on EMT.
EMT is regulated by several transcription factors,
such as snail1, snail2, Twist and Zeb1/2 (22,23,26,27).
Snail serves as is a critical connection in EMT regulation by
repressing E-cadherin expression (28). To further illustrate the role of
snail in EMT, snail siRNA was used. It is well-known that Hep G2 is
a hepatoblastoma-derived cell line but not a HCC (29). The reason why we did not use primary
hepatocytes in the present study is that the proliferative activity
of primary hepatocytes is poor and it is hard to be generated, thus
it is difficult to study the function of related pathways in the
cells. To solve this problem, we then used the Hep-G2 cell line due
to its proliferative activity as well as its stability. Finally it
was shown that when the snail gene was silent, barcacin and
puerarin did not demonstrate obvious effects in the
acetaldehyde-treated cells. These results characterized a novel
mechanism of baicalin and puerarin in the treatment of liver
fibrosis.
However, there are some limitations in the present
study. First, the morphological changes of the cells were absent.
Second, it would be better to evaluate the changes in the protein
expression levels of E-cadherin, vimentin, fibronectin, Smad3,
occludin, ZO-1 and claudin. In a further study, we will perform
related experiments to explore the role of the above
components.
In summary, our present results show that high
acetaldehyde induces EMT via activating the TGF-β1/Smad3 pathway.
Furthermore, baicalin and puerarin reverse the changes. These
results provide a novel target for the prevention and treatment of
alcoholic liver injury.
Acknowledgements
The authors thank Professor Jianwen Liu (East China
University of Science and Technology, Shanghai, China) for help in
performing the experiments and Professor Peiyong Zheng (Longhua
Hospital, Shanghai University of Traditional Chinese Medicine
Shanghai, China) for his help in the writing and revision of the
mansucript.
Funding
The present study was funded by National Natural
Science Foundation of China (grant no. 81620108030), the 3-year
Action Plan of Shanghai Municipal Committee of Health and Family
Planning (grant no. ZY3-CCCX-2-1002), the Shanghai Rising-Star
Project (grant no. 15QA1403500) and the Shanghai Talents
Development Fund Project (grant no. 2017090).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
GJ and TW designed the research. TW and TL performed
the in vitro experiment. TW and LJX performed statistical
analysis. TW wrote the paper. GJ revised the paper. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
The present study is in vitro study, thus no
Ethics approval and consent to participate is provided.
Patient consent for publication
Not applicable.
Competing interests
The authors declare no competing financial
interests.
References
|
1
|
Morgan TR: Treatment of alcoholic liver
disease. Gastroenterol Hepatol (N Y). 13:425–427. 2017.PubMed/NCBI
|
|
2
|
Centers for Disease C and Prevention
(CDC): Alcohol-attributable deaths and years of potential life
lost-United States, 2001. MMWR Morb Mortal Wkly Rep. 53:866–870.
2004.PubMed/NCBI
|
|
3
|
Hur K, Toiyama Y, Takahashi M, Balaguer F,
Nagasaka T, Koike J, Hemmi H, Koi M, Boland CR and Goel A:
MicroRNA-200c modulates epithelial-to-mesenchymal transition (EMT)
in human colorectal cancer metastasis. Gut. 62:1315–1326. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chen CL, Chen YH, Tai MC, Liang CM, Lu DW
and Chen JT: Resveratrol inhibits transforming growth
factor-β2-induced epithelial-to-mesenchymal transition in human
retinal pigment epithelial cells by suppressing the Smad pathway.
Drug Des Devel Ther. 11:163–173. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zimowska M: Signaling pathways of
transforming growth factor beta family members. Postepy Biochem.
52:360–366. 2006.(In Polish). PubMed/NCBI
|
|
6
|
ten Dijke P and Hill CS: New insights into
TGF-beta-Smad signalling. Trends Biochem Sci. 29:265–273. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chen JM, Wang L and Xing LJ: Regulatory
effects of Qinggan Huoxue Recipe on matrix metalloproteinases of
alcoholic liver fibrosis rats. Zhongguo Zhong Xi Yi Jie He Za Zhi.
31:1538–1544. 2011.(In Chinese). PubMed/NCBI
|
|
8
|
Wu T, Liu T, Zheng PY, Xing LJ and Ji G:
Effects of Qinggan Huoxue Recipe and its separated recipes on the
expression of tumor necrosis factor-alpha in rats with alcoholic
liver injury. Zhong Xi Yi Jie He Xue Bao. 6:1145–1151. 2008.(In
Chinese). View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wu T, Liu T, Zhang L, Xing LJ, Zheng PY
and Ji G: Chinese medicinal formula, Qinggan Huoxue Recipe protects
rats from alcoholic liver disease via the
lipopolysaccharide-Kupffer cell signal conduction pathway. Exp Ther
Med. 8:363–370. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wu T, Chen JM, Xiao TG, Shu XB, Xu HC,
Yang LL, Xing LJ, Zheng PY and Ji G: Qinggan Huoxue Recipe
suppresses epithelial-to-mesenchymal transition in alcoholic liver
fibrosis through TGF-β1/Smad signaling pathway. World J
Gastroenterol. 22:4695–4706. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang H, Zhang Y, Bai R, Wang M and Du S:
Baicalin attenuates alcoholic liver injury through modulation of
hepatic oxidative stress, inflammation and sonic hedgehog pathway
in rats. Cell Physiol Biochem. 39:1129–1140. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang CY, Ma FL, Liu JT, Tian JW and Fu FH:
Protective effect of salvianic acid a on acute liver injury induced
by carbon tetrachloride in rats. Biol Pharm Bull. 30:44–47. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhao L, Wang Y, Liu J, Wang K, Guo X, Ji
B, Wu W and Zhou F: Correction to protective effects of genistein
and puerarin against chronic alcohol-induced liver injury in mice
via antioxidant, anti-inflammatory and anti-apoptotic mechanisms. J
Agric Food Chem. 64:84632016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhao H, Li S and Zhang H, Wang G, Xu G and
Zhang H: Saikosaponin A protects against experimental sepsis via
inhibition of NOD2-mediated NF-κB activation. Exp Ther Med.
10:823–827. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Larue L and Bellacosa A:
Epithelial-mesenchymal transition in development and cancer: Role
of phosphatidylinositol 3′kinase/AKT pathways. Oncogene.
24:7443–7454. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Blick T, Widodo E, Hugo H, Waltham M,
Lenburg ME, Neve RM and Thompson EW: Epithelial mesenchymal
transition traits in human breast cancer cell lines. Clin Exp
Metastasis. 25:629–642. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Liu J, Zeng L, Zhao Y, Zhu B, Ren W and Wu
C: Selenium suppresses lipopolysaccharide-induced fibrosis in
peritoneal mesothelial cells through inhibition of
epithelial-to-mesenchymal transition. Biol Trace Elem Res.
161:202–209. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Xie Y, Liao R, Pan L, Fan K, Peng C and Du
C: Hepatic stellate cell conditioned medium induces proliferation
and epithelial-mesenchymal transition via activating ERK1/2
signaling pathway in hepatoma cells. Xi Bao Yu Fen Zi Mian Yi Xue
Za Zhi. 33:210–214. 2017.(In Chinece). PubMed/NCBI
|
|
20
|
Park JH, Park B and Park KK: Suppression
of hepatic epithelial-to-mesenchymal transition by melittin via
blocking of TGFβ/Smad and MAPK-JNK signaling pathways. Toxins
(Basel). 9:2017. View Article : Google Scholar
|
|
21
|
Carl C, Flindt A, Hartmann J, Dahlke M,
Rades D, Dunst J, Lehnert H, Gieseler F and Ungefroren H: Ionizing
radiation induces a motile phenotype in human carcinoma cells in
vitro through hyperactivation of the TGF-beta signaling
pathway. Cellular and molecular life sciences: CMLS. 73:427–443.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Valcourt U, Kowanetz M, Niimi H, Heldin CH
and Moustakas A: TGF-beta and the Smad signaling pathway support
transcriptomic reprogramming during epithelial-mesenchymal cell
transition. Mol Biol Cell. 16:1987–2002. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Muthusamy BP, Budi EH, Katsuno Y, Lee MK,
Smith SM, Mirza AM, Akhurst RJ and Derynck R: ShcA protects against
epithelial-mesenchymal transition through compartmentalized
inhibition of tgf-β-induced smad activation. PLoS Biol.
13:e10023252015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kong D, Zhang F, Shao J, Wu L, Zhang X,
Chen L, Lu Y and Zheng S: Curcumin inhibits cobalt chloride-induced
epithelial-to-mesenchymal transition associated with interference
with TGF-β/Smad signaling in hepatocytes. Lab Invest. 95:1234–1245.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wang QL, Tao YY, Yuan JL, Shen L and Liu
CH: Salvianolic acid B prevents epithelial-to-mesenchymal
transition through the TGF-beta1 signal transduction pathway in
vivo and in vitro. BMC Cell Biol. 11:312010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Puisieux A, Brabletz T and Caramel J:
Oncogenic roles of EMT-inducing transcription factors. Nat Cell
Biol. 16:488–494. 2014. View
Article : Google Scholar : PubMed/NCBI
|
|
27
|
Sciacovelli M, Goncalves E, Johnson TI, Wu
L, Zhang X, Chen L, Lu Y and Zheng S: Fumarate is an epigenetic
modifier that elicits epithelial-to-mesenchymal transition. Nature.
537:544–547. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Xia W, Ma X, Li X, Dong H, Yi J, Zeng W
and Yang Z: miR-153 inhibits epithelial-to-mesenchymal transition
in hepatocellular carcinoma by targeting Snail. Oncol Rep.
34:655–662. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lopez-Terrada D, Cheung SW, Finegold MJ
and Knowles BB: Hep G2 is a hepatoblastoma-derived cell line. Human
Pathol. 40:1512–1515. 2009. View Article : Google Scholar
|