Introduction
Surgical resection is the most efficient treatment
strategy for patients with various types of malignancy at the early
stage, including gastric cancer, and the treatment outcomes are
usually satisfactory (1). Anesthesia
is an unavoidable peri-operative application, and various modes of
anesthesia may have different effects on post-operative recovery,
occurrence of short-term adverse effects or even tumor recurrence
(2). Incisions made during the
surgical operations may induce inflammatory responses by
interrupting the synthesis and secretion of various inflammatory
cytokines. To a large extent, the severity of inflammatory
responses determines treatment outcomes (3), while different modes of anesthesia may
have different effects on inflammatory cytokines induced by
surgical operations (4). In
addition, numerous studies have indicated that various
peri-operative factors may damage cellular immunity to increase
cell immunosuppression so as to induce tumor metastasis and
recurrence, as well as shorten the patients' survival time
(5). Drugs used in anesthesia and
post-operative analgesia may also affect immune function (6). Therefore, it may be hypothesized that
appropriate management of anesthesia and analgesia may inhibit
inflammatory responses and protect immune functions in cancer
patients that underwent surgical resection (7).
In this light, the appropriate management of
anesthesia and analgesia may lower the impact on immune balance and
improve the patients' post-operative immune function, which in turn
improves the prognosis (7). General
anesthesia alone and its combination with epidural anesthesia are
two commonly used anesthetic modes. The present study aimed to
investigate the effects of general anesthesia alone and combined
with epidural anesthesia on the inflammatory response and immune
function of early-stage gastric cancer (EGC) patients who underwent
tumor resection.
Patients and methods
Patients
A total of 107 patients with EGC who underwent
surgery between January 2014 and January 2017 at the General
Hospital of Daqing Oil Field of Heilongjiang (Daqing, China) were
enrolled in the present study. All patients were preliminary
diagnosed by pathological examinations. EGC was defined as a
malignant tumor confined to the submucosa and mucosa regardless of
the absence and presence of lymph node metastasis (LNM) according
to the classification of the Japanese Gastric Cancer Association
(8). Inclusion criteria: i) Patients
with EGC; ii) Patients diagnosed and treated for the first time;
iii) Patients completed the whole treatment procedure in the stated
hospital hospital; iv) Patients willing to participate. Exclusion
criteria: i) Patients with other types of malignancies; ii)
Patients received treatment prior to admission; iii) Patients
allergic to drugs used in the study. The patients included 72 males
and 35 females, and the age ranged from 27 to 75 years, with an
average age of 49±12.4 years. All patients received endoscopic
submucosal dissection according to the methods described by Abe
et al (9).
Grouping and anesthetic methods
The 107 patients were randomly divided into a
control group (n=53) and an observation group (n=54) to receive
different types of anesthesia. Patients in the control group
received tracheal intubation and general anesthesia. Infusion of
propofol (3–4 µg/ml; Claris Injectables Ltd., Ahmedabad, India)
using a target-controlled micropump was performed to induce
anesthesia. A single injection of fentanyl (2–4 µg/kg) and
cisatracurium (0.02 mg/kg; both Yichang Renfu Pharmaceutical Co.,
Ltd., Yichang, China) was performed. Tracheal intubation was
performed to maintain anesthesia and remifentanil (Jiangsu Nhwa
Pharmaceutical Co., Ltd., Xuzhou, China; approval no. H20143314)
was injected at a dose of 0.1–0.2 µg/kg/min. Intravenous injection
of fentanyl (0.1 mg) was performed 5 min prior to the surgery.
Patients in the observation group received combined epidural and
general anesthesia. An epidural tube (21Gx1000; cat. no.
79.8089.150; Sarstedt, Inc., Newton, NC, USA) was placed into the
T8-10 intervertebral space prior to induction of anesthesia.
Lidocaine (3 ml; Jincheng Hayes Pharmaceutical Co., Ltd., Jincheng,
China; approval no. H14023559) was injected. The block was
confirmed to be successful when it reached T4-T12. Subsequently,
general anesthesia was performed using the same method. Epidural
administration of 1% lidocaine (5–10 ml) and 0.375% ropivacaine
(Guangdong Shunfeng Pharmaceutical Co., Ltd., Shunde, China;
approval no. H20050325) was performed using a micropump (5–8 ml/h).
After the surgery, patients in the control group were treated with
intravenous analgesia by infusion of sufentanil (1 µg/ml; Yichang
Renfu Pharmaceutical Co., Ltd.; approval no. H20054172) at a speed
of 5 ml/h. Patients in the observation group were subjected to
epidural analgesia by injecting ropivacaine (0.12%) and sufentanil
(0.2 µg/ml) at a rate of 5 ml/h. Post-operative analgesia was
performed for 2–6 days depending on the individual condition of
each patient.
Blood extraction
Venous blood (5 ml) was extracted from each
participant immediately prior to anesthesia (T1), 2 h after the
beginning of the surgery (T2), immediately after the surgery (T3),
24 h after surgery (T4), 48 h after surgery (T5) and 72 h after
surgery (T6).
Detection of T-lymphocyte subsets and
natural killer cells
Percentages of viable T lymphocyte subsets,
including CD3+, CD4+ and CD8+
cells, were measured by flow cytometry (BD Accuri™ C6 Plus; BD
Biosciences, Franklin Lakes, NJ, USA). The
CD4+/CD8+ ratio was calculated.
Detection of tumor markers
Levels of carcinoembryonic antigen (CEA) in the
serum were measured using CA15-3 levels determined using AN
automatic electrochemistry luminescence immunoassay system (ROCHE
E170; Roche Diagnostics GmbH, Mannheim, Germany) according to the
manufacturer's instructions.
Detection of inflammatory
cytokines
The levels of pro-inflammatory cytokines interleukin
(IL)-1, IL-8, high-sensitivity C-reactive protein (hs-CRP) and
tumor necrosis factor (TNF)-α were measured by ELISA using human
IL-1 ELISA kit (cat. no. KHC0011; Thermo Fisher Scientific, Inc.,
Waltham, MA, USA), IL-8 ELISA kit (cat. no. BMS204-3; Thermo Fisher
Scientific, Inc.), human hs-CRP ELISA kit (cat. no. HK369; Hycult
Biotech, Uden, Netherlands) and human TNF-α ELISA kit (cat. no.
KHC3011; Thermo Fisher Scientific, Inc.) according to
manufacturer's instructions.
Statistical analysis
SPSS 19.0 (IBM Corp., Armonk, NY, USA) software was
used for all statistical analyses. Measurement data were expressed
as the mean ± standard deviation, and the Student's t-test was used
for comparisons between the two groups. Count data were expressed
as a rate and analyzed using the χ2 test. P<0.05 was
considered to indicate a statistically significant difference.
Results
Comparison of clinical data
The general clinical data were compared between the
two groups. As presented in Table I,
no significant differences in sex, mean age, average age, body mass
index, weight and presence of LNM were identified between the two
groups (P>0.05). In addition, no significant differences in
anesthesia time and surgical time were noted between the two groups
(P>0.05), indicating that compared with general anesthesia,
combined epidural and general anesthesia did not increase the
anesthesia time and surgical time.
 | Table I.Comparison of general characteristics
between the observation and control groups. |
Table I.
Comparison of general characteristics
between the observation and control groups.
| Item | Control (n=53) | Observation
(n=54) | P-value |
|---|
| Sex |
|
| 0.357 |
| Male | 35 (66%) | 37 |
|
|
Female | 18 (34%) | 17 |
|
| Age (years) |
|
| 0.331 |
|
Range | 27–74 | 30–75 |
|
|
Median | 47.2 | 47.5 |
|
|
Average | 49.3±12.6 | 48.6±11.9 |
|
| BMI
(kg/m2) | 20.34±1.23 | 20.22±1.31 | 0.323 |
| Weight (kg) | 61.22±5.76 | 63.13±7.33 | 0.191 |
| LNM (cases) |
|
| 0.146 |
| Yes | 22 | 25 |
|
| No | 31 | 29 |
|
| Anesthesia time
(min) | 277.91±28.36 | 286.43±31.93 | 0.237 |
| Surgical time
(min) | 211.72±44.34 | 205.02±52.22 | 0.212 |
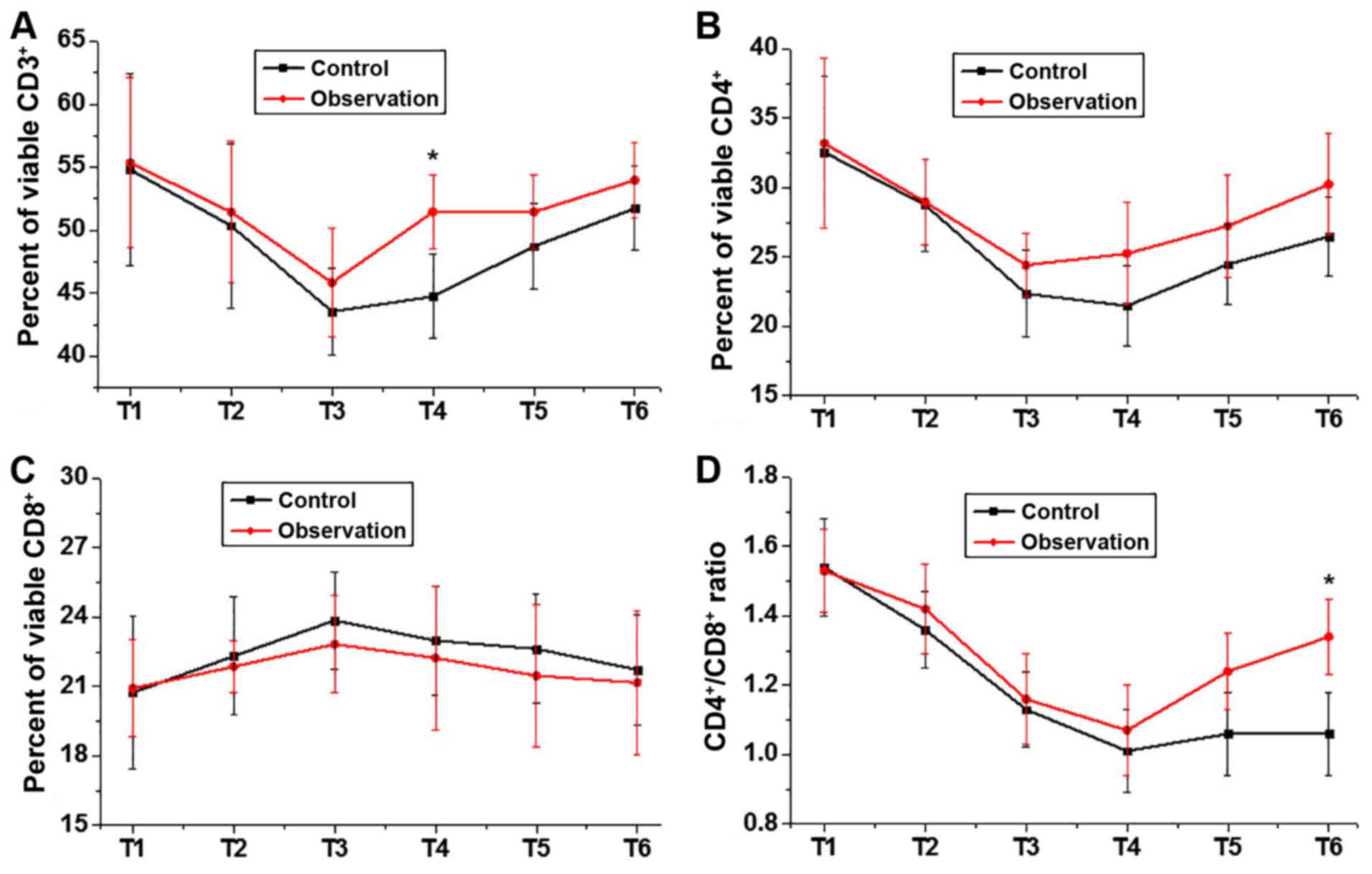
Comparison of percentages of viable
T-lymphocyte subsets between the two groups at different
time-points
The percentages of viable T-lymphocyte subsets,
including CD3+, CD4+ and CD8+
cells, were measured by flow cytometry, and the
CD4+/CD8+ ratio was calculated. As presented
in Fig. 1, no significant
differences in the percentage of viable CD3+,
CD4+ and CD8+ cells, or the
CD4+/CD8+ ratio were identified between the
two groups prior to anesthesia. The percentage of CD3+
and CD4+ cells, as well as the
CD4+/CD8+ ratio, were decreased during
surgery and increased after surgery in the two groups. By contrast,
the percentage of CD8+ cells was increased during
surgery and decreased after surgery. Although most differences were
not statistically significant, the percentages of CD3+
and CD4+ cells and the CD4+/CD8+
ratio were slightly higher, while percentage of CD8+
cells was slightly lower in observation group compared with that
that in the control group. Significant differences were observed
between two groups in percentage of viable CD3+ at T4
and in CD4+/CD8+ ratio at T6.
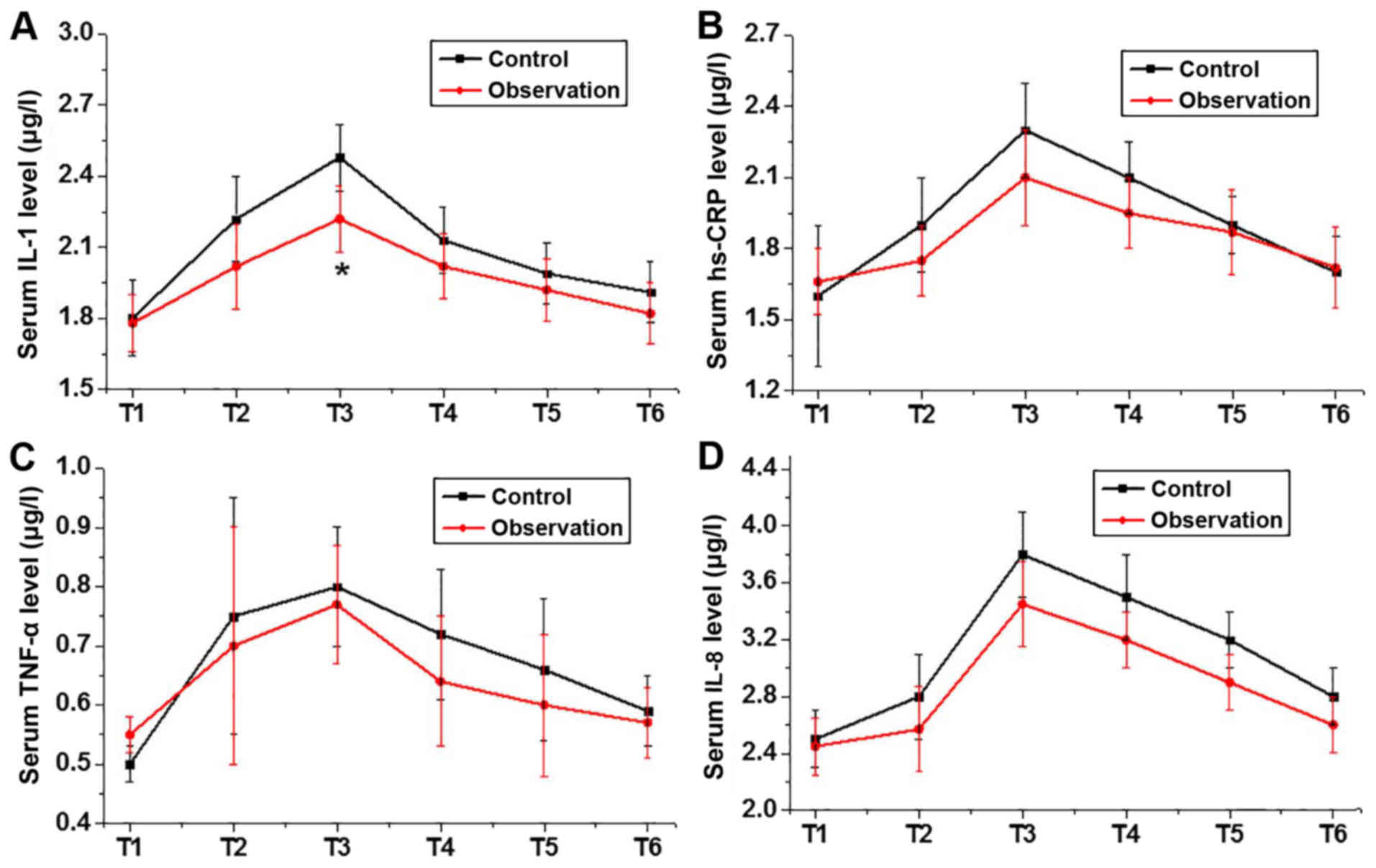
Comparison of inflammatory cytokines
between the two groups
ELISA was used to determine the levels of the
pro-inflammatory cytokines IL-1, IL-8, hs-CRP and TNF-α at
different time-points. As presented in Fig. 2, no significant differences in the
serum levels of IL-1, IL-8, hs-CRP and TNF-α were identified
between the two groups prior to anesthesia. The serum levels of
IL-1, IL-8, hs-CRP and TNF-α were increased during the surgery and
decreased after the surgery in each of the two groups. Although
most differences were not statistically significant, the serum
levels of IL-1, IL-8 and hs-CRP in the observation group were
slightly lower than those in the control group.
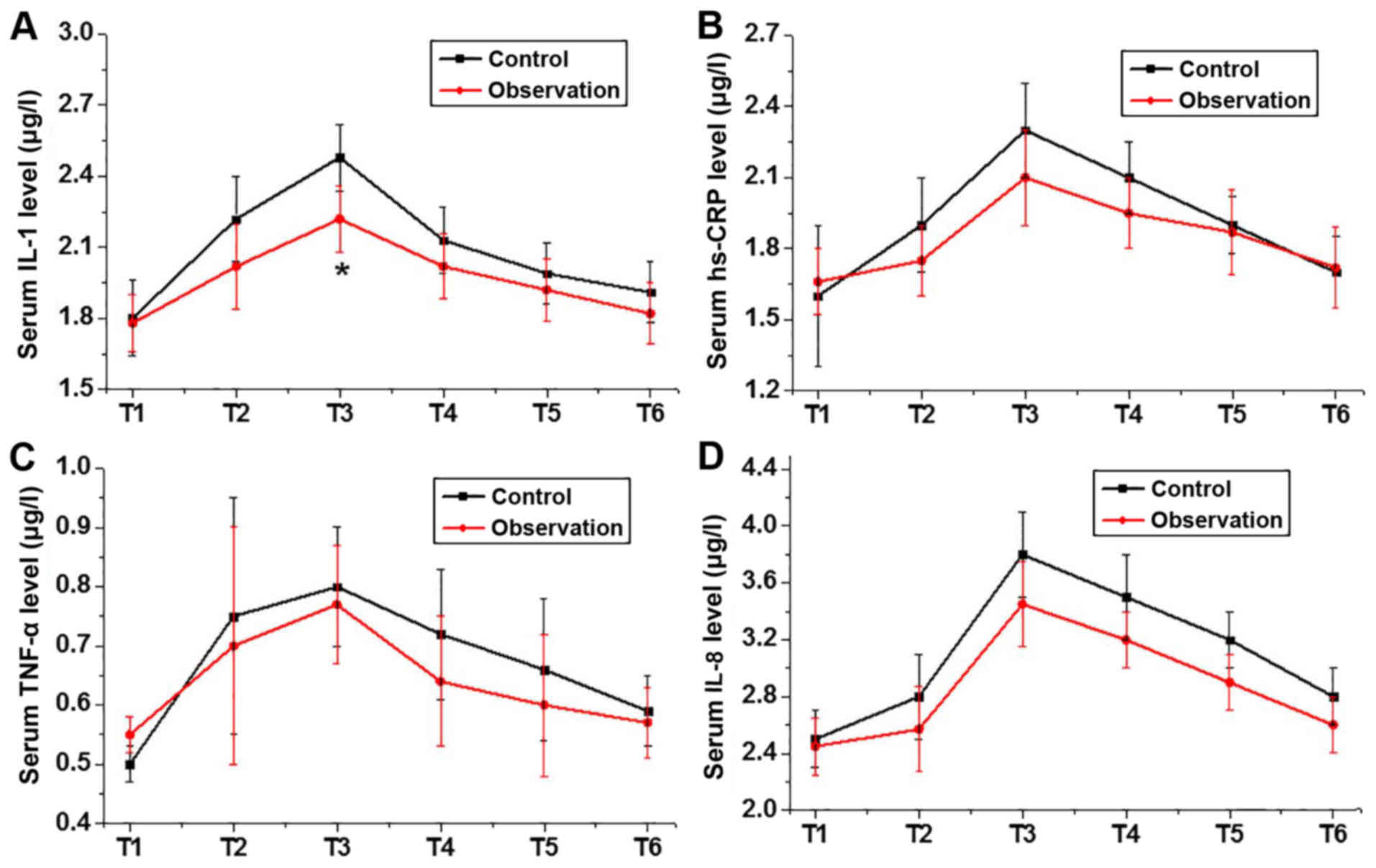 | Figure 2.Comparison of inflammatory cytokines
between the two groups. Serum levels of (A) IL-1, (B) hs-CRP, (C)
TNF-α and (D) IL-8. The serum levels of IL-1, IL-8 and hs-CRP in
the observation group were slightly lower than those in the control
group at each time-point. Significant differences were observed
between two groups in serum levels of IL-1 at T3. Time-points: T2,
immediately prior to anesthesia; T2, 2 h after the beginning of the
surgery; T3, immediately after the surgery; T4, 24 h after surgery;
T5, 48 h after surgery; T6, 72 h after surgery. *P<0.05 vs.
control group. IL, interleukin; hs-CRP, high-sensitivity C-reactive
protein; TNF, tumor necrosis factor. |
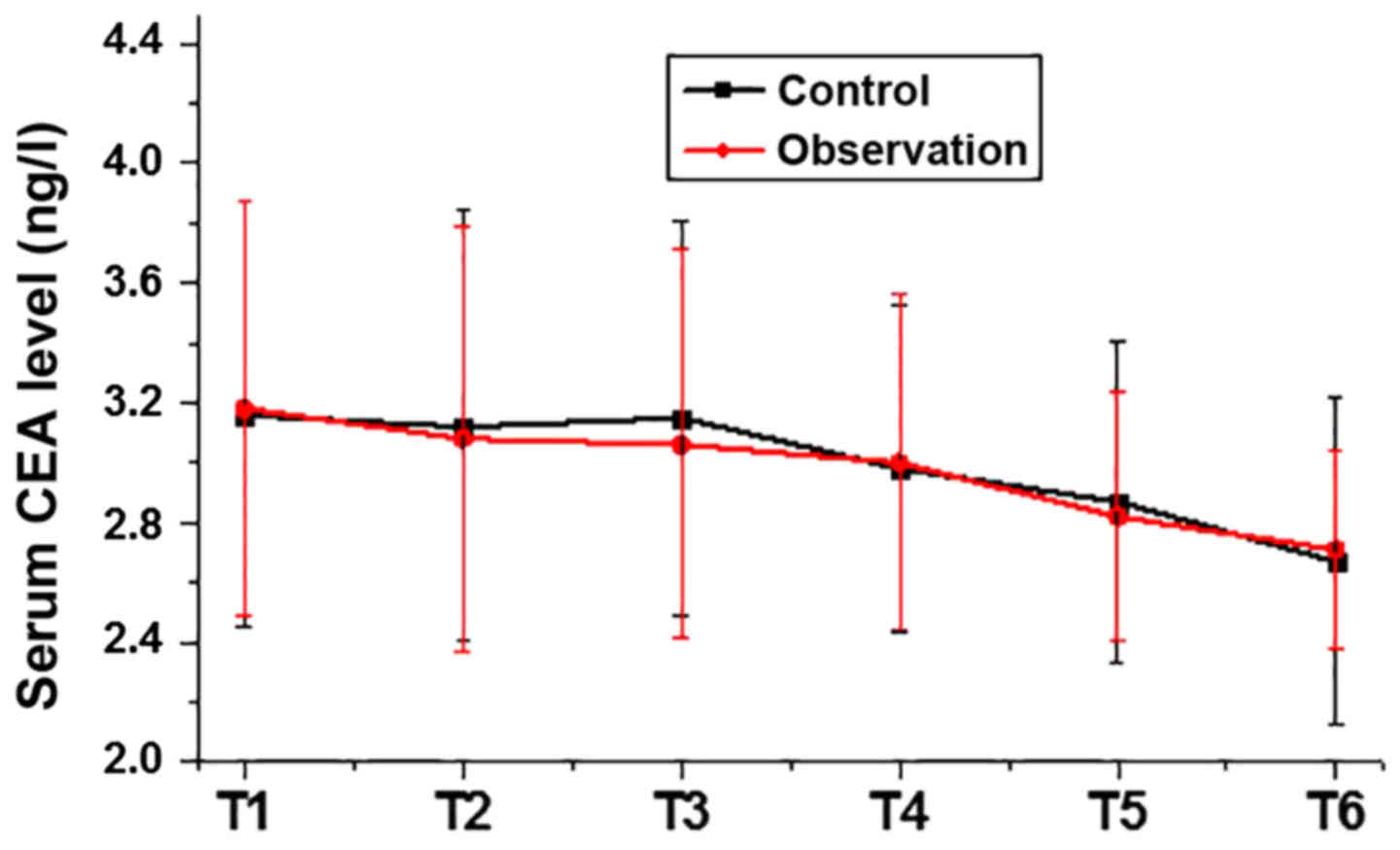
Comparison of serum levels of CEA
between the two groups
CEA has been widely used in the diagnosis of various
types of malignancies. As presented in Fig. 3, no significant differences in the
serum levels of CEA were identified between the two groups prior to
anesthesia. The serum levels of CEA were slightly decreased after
surgery in each of the groups. No significant differences in the
serum levels of CEA were identified between the observation group
and the control group. A clear decreasing trend was observed in
both groups.
Comparison of adverse reactions
between the two groups
The incidence of adverse reactions within 3 days
after the operation was recorded and compared between the two
groups. As presented in Table II,
no significant differences in the incidence of hypoxemia and
delayed recovery were identified between the two groups. By
contrast, the incidence of nausea and vomiting, as well as
post-operative agitation were significantly lower in the
observation group than those in the control group (P<0.05).
 | Table II.Comparison of adverse reactions
between the observation and control groups. |
Table II.
Comparison of adverse reactions
between the observation and control groups.
| Adverse event | Observation (n=54)
(%) | Control (n=53)
(%) | χ2 | P-value |
|---|
| Nausea and
vomiting | 1 (1.9) | 5 (9.4) | 1.323 | 0.041 |
| Hypoxemia | 1 (1.9) | 3 (5.7) | 0.277 | 0.21 |
| Post-operative
agitation | 0 | 6 (11.3) | 4.427 | 0.035 |
| Delayed
recovery | 2 (3.7) | 4 (7.5) | 0.198 | 0.171 |
Discussion
Gastric cancer is a type of malignancy that
originates from the lining of the stomach and poses a serious
threat to the health and life of humans (10). In recent years, the incidence of
gastric cancer has exhibited an increasing trend, possibly due to
changes in lifestyle and diet. At present, gastric cancer is
considered to be one of the most common malignancies worldwide. In
China, the incidence rate of gastric cancer ranks third among all
types of malignancies in females and is only lower than that of
lung cancer and breast cancer; in males it ranks second followign
lung cancer (11). Men are generally
more vulnerable to gastric cancer than women (12). In the present study, male patients
accounted for 67.3% of all cases and only 35 patients (32.7%) were
females.
Cancer patients usually have an impaired immune
function (13). During surgical
preparation and operation, stress reactions caused by incisions and
anesthetics, including opioids, may further inhibit immune function
(14). Percentages of viable
T-lymphocyte subsets are usually employed to refelect immune
function. The CD3 T-cell co-receptor mediates the activation of
T-helper cells (CD4+ naïve T cells) and cytotoxic T
cells (CD8+ naïve T cells) (15). The CD4+/CD8+
ratio in the peripheral blood of normal healthy adults is
approximately 2:1, and a reduced CD4+/CD8+
ratio indicates morbidities associated with immunodeficiency or
autoimmunity (16). In the present
study, the percentage of CD3+ and CD4+ cells,
as well as the CD4+/CD8+ ratio, were
decreased during surgery. By contrast, the percentage of
CD8+ cells was increased, which indicated a reduced
immune function caused by the surgical operation and anesthetics.
The possible explanation is that trauma and anesthetics may promote
the secretion of catechol and adrenaline, which may inhibit
T-lymphocyte immune function. After treatment, the percentage of
CD3+ and CD4+ cells, and the
CD4+/CD8+ ratio were increased, while the
percentage of CD8+ cells was decreased. In addition,
although no significant differences were identified at most
time-points, the percentage of CD3+ and CD4+,
and the CD4+/CD8+ ratio in observation group
were higher, while the percentage of CD8+ was lower than
that in control group. This is due to the fact that the cerebral
cortex limbic system may be inhibited by general anesthesia, so
that central conduction is nociceptively stimulated, leading to an
obvious stress response and a reduced cellular immune function
(17). By contrast, epidural
anesthesia has no significant effects on the sensitivity of the
immune response. Therefore, nerve impulses caused by traumatic
stimulation may be effectively inhibited.
Stress responses mediated by anesthesia may lead to
changes in the synthesis and secretion of catechins, which in turn
stimulate the secretion of inflammatory cytokines and cause
inflammatory reactions (18). IL-1
and IL-8 are two pro-inflammatory factors involved in the
development of vairous human diseases (19). As a major acute-phase reactant,
levels of CRP reflect the severity of the inflammatory response
(20). As another pro-inflammatory
factor, the levels of TNF-α reflect the severity of the
inflammatory response and immune function (21). In the present study, the serum levels
of IL-1, IL-8, hs-CRP and TNF-α were increased during the surgery,
which indicated the presence of an inflammatory reponse caused by
surigical trauma and anesthetics. After the sugery, the serum
levels of IL-1, IL-8, hs-CRP and TNF-α were decreased again.
Although no significant differences were observed in most cases,
the serum levels of IL-1, IL-8 and hs-CRP in the observation group
were lower than those in the control group. These results suggest
that compared with general anesthesia, combined epidural and
general anesthesia inhibits the inflammatory response. This may
possibly be explained by the reduced stress response and less
adverse effects of epidural anesthesia on the entire body. However,
it's known that particular levels of inflammatory reposes promote
wounding healing (22). Therefore,
the fine regulation of surgical inflammation remains to be further
investigated and discussed.
Serum CEA has been widely used to predict the
recurrence of gastric cancer after treatment, and high levels of
serum CEA indicate a high risk of post-operative recurrence
(23). In the present study, no
significant differences were identified in the serum levels of CEA
between the observation group and the control group at different
time-points after surgery, indicating that combined epidural and
general anesthesia is not superior to general anesthesia in
inhibiting post-operative recurrence of gastric cancer. However,
compared with patients treated with general anesthesia, combined
epidural and general anesthesia significantly inhibited the
occurrence of nausea and vomiting, as well as post-operative
agitation, although no significant differences in the incidence of
hypoxemia and delayed recovery were identified between the two
groups. Therefore, future studies by our group will focus on the
reduction of the incidence of hypoxemia and delayed recovery. The
present study did not include the analysis of post-operative
analgesia. Patients in the control group were treated with
intravenous analgesia by infusion of sufentanil for post-operative
analgesia, while patients in the observation group received
ropivacaine combined with sufentanil at a lower dose. The different
types of post-operative analgesia may affect inflammation in
patients. Further study will investigate the effects of
post-operative analgesia modes on inflammatory responses.
In conclusion, compared with general anesthesia,
combined epidural and general anesthesia inhibits the inflammatory
response, improves immune function and inhibits the occurrence of
certain post-operative adverse events in patients with EGC that
underwent tumor resection.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LZ designed the experiments. WL and LW performed
experiments. MZ analyzed the data. LZ drafted the manuscript. The
final version of the manuscript has been read and approved by all
authors, and each author believes that the manuscript represents
honest work.
Ethics approval and consent to
participate
The Ethics Committee of General Hospital of Daqing
Oil Field of Heilongjiang approved the present study and all
patients provided written informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Yasunaga H, Horiguchi H, Kuwabara K,
Matsuda S, Fushimi K, Hashimoto H and Ayanian JZ: Outcomes after
laparoscopic or open distal gastrectomy for early-stage gastric
cancer: A propensity-matched analysis. Ann Surg. 257:640–646. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Choi WJ, Baek S, Joo EY, Yoon SH, Kim E,
Hong B, Hwang JH and Kim YK: Comparison of the effect of spinal
anesthesia and general anesthesia on 5-year tumor recurrence rates
after transurethral resection of bladder tumors. Oncotarget.
8:87667–87674. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Mahle WT, Matthews E, Kanter KR, Kogon BE,
Hamrick SE and Strickland MJ: Inflammatory response after neonatal
cardiac surgery and its relationship to clinical outcomes. Ann
Thorac Surg. 97:950–956. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Martelli D, Yao ST, Mancera J, McKinley MJ
and McAllen RM: Reflex control of inflammation by the splanchnic
anti-inflammatory pathway is sustained and independent of
anesthesia. Am J Physiol Regul Integr Comp Physiol.
307:R1085–R1091. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Thomas SN, Vokali E, Lund AW, Hubbell JA
and Swartz MA: Targeting the tumor-draining lymph node with
adjuvanted nanoparticles reshapes the anti-tumor immune response.
Biomaterials. 35:814–824. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cheng YC, Cheng XB, Li XJ, Wang FZ and Li
ZK: Combined general and regional anesthesia and effects on immune
function in patients with benign ovarian tumors treated by
laparoscopic therapy. Int J Clin Exp Med. 6:716–719.
2013.PubMed/NCBI
|
|
7
|
Zhang T, Fan Y, Liu K and Wang Y: Effects
of different general anaesthetic techniques on immune responses in
patients undergoing surgery for tongue cancer. Anaesth Intensive
Care. 42:220–227. 2014.PubMed/NCBI
|
|
8
|
Japanese Gastric Cancer Association, .
Japanese classification of gastric carcinoma-2nd english edition.
Gastric Cancer. 1:10–24. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Abe N, Mori T, Takeuchi H, Yoshida T, Ohki
A, Ueki H, Yanagida O, Masaki T, Sugiyama M and Atomi Y:
Laparoscopic lymph node dissection after endoscopic submucosal
dissection: A novel and minimally invasive approach to treating
early-stage gastric cancer. Am J Surg. 190:496–503. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Karimi P, Islami F, Anandasabapathy S,
Freedman ND and Kamangar F: Gastric cancer: Descriptive
epidemiology, risk factors, screening and prevention. Cancer
Epidemiol Biomarkers Prev. 23:700–713. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chen W, Zheng R, Zhang S, Zhao P, Zeng H,
Zou X and He J: Annual report on status of cancer in China, 2010.
Chin J Cancer Res. 26:48–58. 2014.PubMed/NCBI
|
|
12
|
Rugge M, Fassan M and Graham DY:
Epidemiology of gastric cancer. Springer International Publishing
Switzerland; Gastric Cancer. pp. 23–34. 2015, View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Brandacher G, Winkler C, Schroecksnadel K,
Margreiter R and Fuchs D: Antitumoral activity of interferon-gamma
involved in impaired immune function in cancer patients. Curr Drug
Metab. 7:599–612. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sprung J, Scavonetto F, Yeoh TY, Kramer
JM, Karnes RJ, Eisenach JH, Schroeder DR and Weingarten TN:
Outcomes after radical prostatectomy for cancer: A comparison
between general anesthesia and epidural anesthesia with fentanyl
analgesia: A matched cohort study. Anesth Analg. 119:859–866. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Birnbaum ME, Berry R, Hsiao YS, Chen Z,
Shingu-Vazquez MA, Yu X, Waghray D, Fischer S, McCluskey J,
Rossjohn J, et al: Molecular architecture of the αβ T cell
receptor-CD3 complex. Proc Natl Acad Sci USA. 111:17576–17581.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Luz Correa B, Ornaghi AP, Cerutti Muller
G, Engroff P, Pestana Lopes R, Gomes da Silva Filho I, Bosch JA,
Bonorino C and Bauer ME: The inverted CD4:CD8 ratio is associated
with cytomegalovirus, poor cognitive and functional states in older
adults. Neuroimmunomodulation. 21:206–212. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hung MH, Chan KC, Liu YJ, Hsu HH, Chen KC,
Cheng YJ and Chen JS: Nonintubated thoracoscopic lobectomy for lung
cancer using epidural anesthesia and intercostal blockade: A
retrospective cohort study of 238 cases. Medicine (Baltimore).
94:e7272015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Li B, Li Y, Tian S, Wang HX, Wu H, Zhang A
and Gao C: Anti-inflammatory effects of perioperative
dexmedetomidine administered as an adjunct to general anesthesia: A
meta-analysis. Sci Rep. 5:123422015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Dinarello CA: The IL-1 family and
inflammatory diseases. Clin Exp Rheumatol. 20 Suppl 27:S1–S13.
2002.PubMed/NCBI
|
|
20
|
Karadeniz M, Duran M, Akyel A, Yarlıoğlueş
M, Öcek AH, Çelik İE, Kılıç A, Yalcin AA, Ergün G and Murat SN:
High sensitive CRP level is associated with intermediate and high
syntax score in patients with acute coronary syndrome. Int Heart J.
56:377–380. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Murdaca G, Spanò F, Contatore M, Guastalla
A, Penza E, Magnani O and Puppo F: Infection risk associated with
anti-TNF-α agents: A review. Expert Opin Drug Saf. 14:571–582.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hunt TK, Knighton DR, Thakral KK, Goodson
WH III and Andrews WS: Studies on inflammation and wound healing:
Angiogenesis and collagen synthesis stimulated in vivo by resident
and activated wound macrophages. Surgery. 96:48–54. 1984.PubMed/NCBI
|
|
23
|
Takahashi Y, Takeuchi T, Sakamoto J, Touge
T, Mai M, Ohkura H, Kodaira S, Okajima K and Nakazato H; Tumor
Marker Committee, . The usefulness of CEA and/or CA19-9 in
monitoring for recurrence in gastric cancer patients: A prospective
clinical study. Gastric Cancer. 6:142–145. 2003. View Article : Google Scholar : PubMed/NCBI
|