Introduction
Tuberculosis (TB) is a relatively common disease in
developing countries, including China and India (1,2). TB
spondylitis is considered to be a serious type of TB disease. The
incidence of spinal TB is increasing, with the spine being affected
in an estimated 50% of cases with musculoskeletal involvement
(3,4). Previous studies have reported that
surgical treatment is an important strategy for the treatment of
spinal TB.
Regarding the surgical removal of spinal TB, bone
grafting fusion is an important step in surgical therapy, which may
improve spinal stability, allow for recovery of the spinal cord
function and reduce the time to recovery for patients (5). The safety and efficacy of internal
fixation for the treatment of spinal TB have been recognized by the
majority of clinicians, and this treatment has an important role in
stabilizing the decreased kyphotic deformity, reducing spinal cord
compression. Hibbs (6) and Albee
(7) reported on the posterior
interbody fusion for spinal TB, also known as Pott's disease, as
early as 1911. Anterior radical debridement and non-instrumented
fusion have been described by Ito et al (8) in 1934, followed by Hodgson and Stock
(9) in 1956. Combined anterior and
posterior fusion has been described by Mukhtar et al
(10) in 2003. In 2013, Kumar et
al (11) reported on posterior
interbody fusion for selected cases of thoracolumbar spinal TB
without anterior instrumentation and without anterior or posterior
bone grafting.
The aim of the present study was to analyze the
clinical and radiological outcomes of active thoracolumbar spinal
TB treated by application of transforaminal-lumbar interbody fusion
(TLIF) technology combined with lesion clearance and chemotherapy
via catheter (TCLC). The study was performed on 26 patients with
active thoracolumbar spinal TB who underwent TCLC. The present
study assessed the changes of the Cobb angle, erythrocyte
sedimentation rate (ESR) and C-reactive protein (CRP) levels, the
functional and radiological outcomes, and the fusion status of
patients with spinal TB treated by using TCLC.
Patients and methods
Patients
The present prospective study included 26 patients
diagnosed with TB spondylitis involving the thoracic spine and
lumbar spine. Permission from the Ethics Committee of Hong Hui
Hospital (Xi'an, China) and written informed consent was obtained
from the patients prior to the study commencing. The Patients
underwent a TLIF procedure (unilateral decompression laminectomy,
drainage of abscess and posterior pedicle screw implementation).
Various patients with active TB spondylitis and with neurological
involvement were included in the study, and the procedures were
performed between October 2010 and October 2013. The pre-operative
kyphosis angle ranged from 5 to 50°. Patients with severe and
highly severe kyphosis (>50°), those with late-onset paraplegia
of healed disease with thoracic spine a bony internal gibbus, and
those with multi-segmental disease with destruction of >2
vertebral bodies were excluded.
The cohort comprised 17 men and 9 women, and their
mean age was 45 years (range, 19–69 years). Neurological assessment
was performed using Frankel grading (12); three patients were rated as Frankel
grade B, six were of grade C and seven were of grade D. A total of
10 patients without any neurological deficits were assigned a
Frankel grade E. For each of the patients, pre-operative
anteroposterior and standing radiographs of the spine were
recorded, and computed tomography (CT) scans, magnetic resonance
imaging and hematological investigations, including complete blood
cell count, ESR and CRP, were performed.
Surgical procedure
Under general anesthesia, patients were positioned
in the prone position on the spinal table. The position of the
affected vertebrae was confirmed using fluoroscopy. The involved
segment was exposed via a midline posterior approach. Screws were
temporarily connected by a rod on one side to avoid instability
during decompression. Hemi-zygapophysial joints or bilateral
zygapophysial joints were made at the involved segment while
retaining the lamina as much as possible. Granulation tissue was
debrided and the abscess, if present, was drained through the
inter-transverse space. Pedicle screws were connected by rods and
compression was applied to correct the kyphosis through a
zygapophysial joint bone graft or lamina bone graft. An
intra-operative biopsy was obtained and sent for histopathological
examination. To maintain the stability of the spine and to
facilitate post-operative vertebral fusion, an intervertebral bone
graft from the ilium was placed. Prior to this, a 0.7-mm epidural
catheter was implanted in the lesion. The kyphosis was corrected as
much as possible by applying compression between the screws prior
to tightening them to the rods.
Post-operative treatment and
rehabilitation
After the operation, patients were treated with 0.1
g isonicotinic acid hydrazide (INH) daily via injection through the
catheter. The mean duration of follow-up for the retention of
catheter was 2.2 months (range 2–4 months); four-drug chemotherapy
(25 mg/ml isoniazid, 15 mg/ml rifamycin sodium, 25 mg/ml
streptomycin, 20 mg/ml acetazolamide; each administered orally) was
continued for 3 months following catheter removal, followed by a
two-drug regimen (INH and rifampicin) for a further period of 8
months.
Mobilization was started in ambulatory patients on
the second post-operative day, and physiotherapy and sickbed
mobilization was started in non-ambulatory patients. Post-operative
bracing was continued for a minimum period of 3 months following
surgery in all patients. The disease was considered healed when
clinical evaluation indicated no spinal tenderness or spasm,
hematological parameters returned to near normal levels and spinal
fusion was evident on follow-up radiographs. Radiographically,
fusion was considered to be complete when a bony bridge with
trabeculation equal in density to the adjacent vertebrae was
present, radiolucent zones were absent and no abnormal mobility
(<5° of movement) was observed at the fused segment on
post-operative flexion-extension radiographs. These criteria were
previously described by Schofferman et al (13) and Kim et al (14).
Statistical analysis
All calculations were performed using SPSS 17.0
(SPSS, Inc., Chicago, IL, USA). Results were presented as mean ±
standard deviation. Comparisons between the three groups were
performed using an unpaired t-test and one-way analysis of variance
followed by a Levene test. P<0.05 was considered to indicate a
statistically significant result.
Results
Pre-operative patient
characteristics
The present study comprised 26 patients diagnosed
with TB spondylitis involving the thoracic spine and lumbar spine.
Patients with active TB spondylitis and with neurological
involvement were included in the study. The pre-operative kyphosis
angle ranged from 5 to 50°. The cohort comprised 17 men and 9
women, and their mean age was 45 years (range, 19–69 years). The
mean duration of follow-up was 14.1 months (range, 9–24 months).
The locations of the lesions were distributed as follows: A total
of 3 cases of lumbar 2–3, 8 cases of lumbar 3–4, 12 cases of lumbar
4–5 and 7 cases of lumbar 5-sacral 1 involvement. Of the 19 cases
with paravertebral abscesses, 9 had psoas abscesses. The
demographic and clinical characteristics of the patients are
presented in Table I.
 | Table I.Demographic and clinical
characteristics of patients (n=26). |
Table I.
Demographic and clinical
characteristics of patients (n=26).
| Variables | Value |
|---|
| Mean age (range,
19–69 years) | 45.4±10.5 |
| Gender | 17 |
| Male |
|
|
Female | 9 |
| Occupation |
|
|
Farmer | 21 |
|
Othera–c | 5 |
| Educational
level |
|
| Basic
school education | 18 |
| Higher
school education | 8 |
| Duration of TB
(months) | 14.1±3.9 |
| Other body sites
infected |
|
| Thoracolumbar
spine | 24 |
|
Otherd,e | 2 |
Surgery and outcomes
In the present study, the mean duration of the
operation was 130 min (range, 112–170 min), the mean
intra-operative blood loss was 550 ml (range, 470–820 ml) and the
mean duration of hospital stay was 7 days (range, 5–10 days). Data
on the pre- and post-operative ESR and CRP are presented in
Table II. The number of patients
with normal ESR before operation was 4, CRP was 6, while the number
of patients with normal ESR after operation was 6, CRP was 10 in
the first month. All patients with neurological deficits exhibited
an improvement in Frankel grading post-operatively (Table III). The mean pre-operative
kyphosis angle was 32.4° (range, 5–50°). The angle of kyphosis was
reduced to a mean of 7.2° in the immediate post-operative period
(range, 0–12°), and the difference was statistically significant
(P<0.005).
 | Table II.Amount of patients with normal ESR
and CRP levels prior to surgery and at various post-OP stages. |
Table II.
Amount of patients with normal ESR
and CRP levels prior to surgery and at various post-OP stages.
| Time-point | ESR | CRP |
|---|
| Pre-OP Post-OP
(months) | 4 (15.3) | 6
(23.1) |
| 1 | 6 (23.1) | 10 (38.5) |
| 3 | 15 (57.7) | 16 (61.5) |
| 6 | 26 (100) | 26 (100) |
 | Table III.Post-operative Frankel grading
(n). |
Table III.
Post-operative Frankel grading
(n).
|
| Frankel grade
(post-operative) |
|---|
|
|
|
|---|
| Pre-Operative
Frankel grade | A | B | C | D | E |
|---|
| A | 0 | 0 | 0 | 0 | 0 |
| B | 0 | 0 | 0 | 2 | 1 |
| C | 0 | 0 | 0 | 2 | 4 |
| D | 0 | 0 | 0 | 2 | 5 |
| E | 0 | 0 | 0 | 0 | 10 |
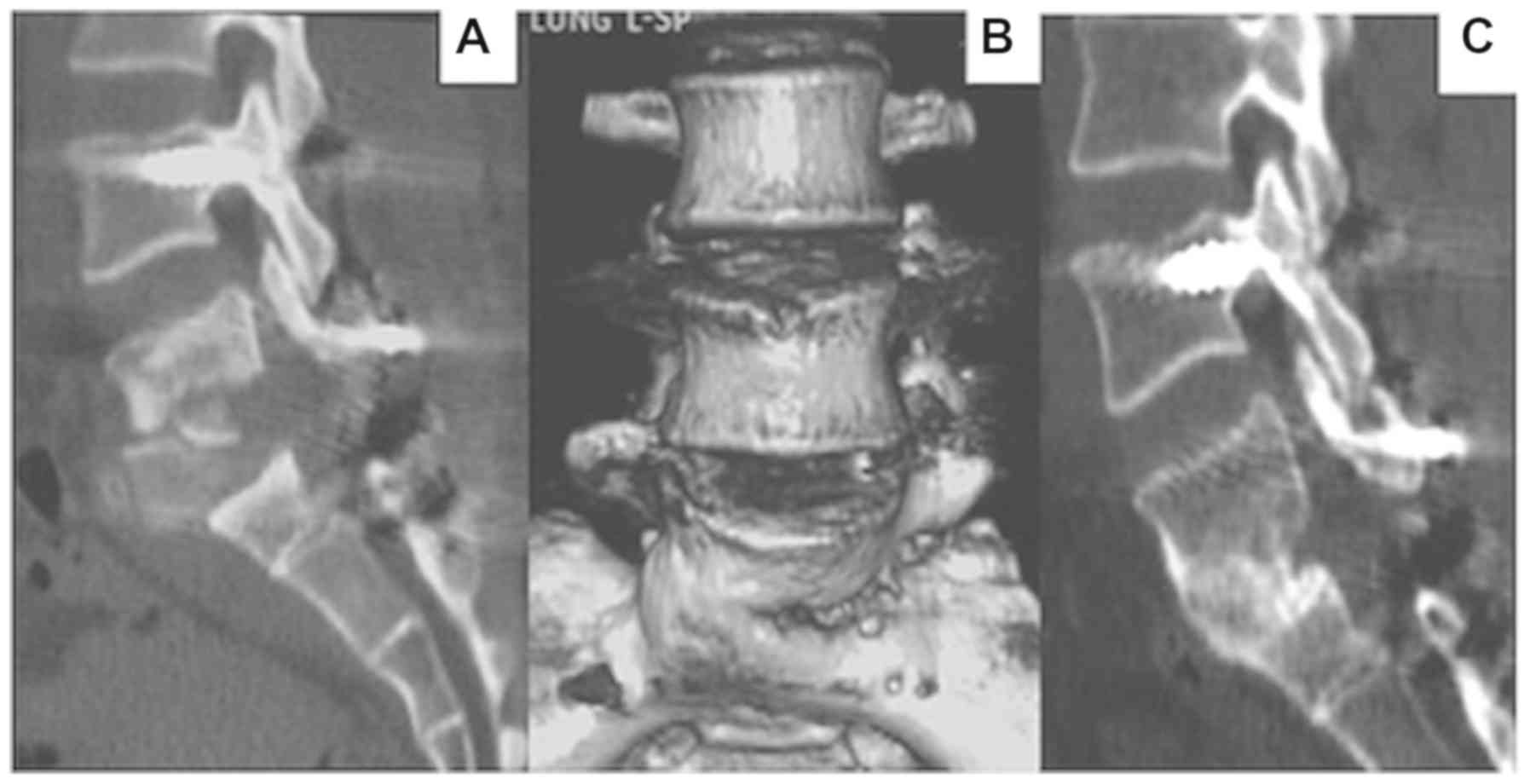
Follow-up results
At the time of the final follow-up, the mean
kyphotic Cobb angle at presentation, after surgery and at the final
follow-up were 22.7±9.8, 9.8±7.3 and 10.3±8.8°, respectively, with
an average correction of 13.1±5.4° after surgery, and a loss of
correction of 1.8±1.0° at the final follow-up (Table IV). The rate of correction and loss
of correction were 56.6 and 8.3%, respectively. Complications were
minor in nature and included delayed wound healing in 1 patient and
sinus formation in 1 patient. No major complications were reported.
The anterior vertebral lesions healed through bony fusion, which
was completed between 6 and 7 months post-operatively (Figs. 1 and 2).
 | Table IV.Kyphotic Cobb angle at presentation
following surgery. |
Table IV.
Kyphotic Cobb angle at presentation
following surgery.
| Time | 1 | 2 | 3 | Mean |
|---|
| Kyphotic Cobb
angle | 22.7±9.8° | 9.8±7.3° | 10.3±8.8° | 13.1±5.4° |
Discussion
In recent years, multiple treatments have been
proposed for spinal TB, but most clinicians perform isolated
anterior lesion clearance or posterior fixation fusion. Certain
studies have described the application of isolated anterior
instrumented fusion with good results (15,16).
According to certain studies, single anterior debridement and bone
grafting are frequently unsatisfactory in correcting kyphosis
deformity or preventing its progression (17–19).
However, others have reported good outcomes for posterior fusion.
Studies including that by Güven et al (20) used CT- or ultrasound-guided
percutaneous catheter drainage (PCD) to treat TB with abscess
formation (21–23). Based on the results of long-term
observation, PCD is a safe, effective, minimally invasive treatment
method with advantages for abscess treatment, but it does not
resolve complications including deformity, severe nerve dysfunction
or spinal instability. However, local chemotherapy for TB infection
is effective, as it acts directly on the lesions. This is
particularly useful for TB patients after surgery, as they are
likely to present with post-operative scarring around lesions and a
limited local blood supply due to destruction of blood vessels
during surgery, which may lead to reduced concentrations of
systemic drugs and reduce the effectiveness of systemic TB drugs.
Furthermore, the anterior approach may damage the spinal segment
and the diaphragm. Soares Do Brito et al (24) have reported a higher incidence of
complications arising from single anterior fusion compared with
those associated with individual post-fusion (25–29).
McDonnell et al (30) have
reported higher complication rates for single-event anterior and
posterior fusions compared with multi-stage anterior and posterior
fusions. They obtained an incidence of major complications of 11%
and an incidence of minor complications of 24%. Simultaneous
multi-level spinal TB surgery has become popular due to its
satisfactory clinical outcomes (31,32); the
disadvantages of combined anterior and posterior approaches include
bleeding, long operation time and complications associated with the
anterior approach (33,34).
For the treatment of spinal TB, posterior
debridement, intervertebral bone graft fusion and internal fixation
compared with anterior and posterior surgery has the following
advantages: i) The anatomic approach is a simple operation with
little trauma, while anterior surgery requires a wide exposure, and
a combined anterior and posterior approach further increases the
surgical trauma. ii) Posterior surgery avoids thoracotomy and
abdominal surgery, and reduces trauma to the lungs and abdominal
cavity viscera, with a consequently low incidence of complications.
iii) Posterior osteotomy using a pedicle screw rod system fixation
of the spinal column provides superior deformity correction with a
sustained effect, allowing the vertebral lamina bone graft to reach
360°. iv) Combined with fixation of the diseased vertebrae, this
approach reduces the internal fixation and fusion range, avoiding
excessive loss of spinal movement units and associated
complications.
Certain experts have raised concerns regarding
posterior surgery alone for TB, mainly for the following reasons:
i) Posterior surgery may destroy the originally normal posterior
column structure, potentially aggravating spinal instability
(35–37) and ii) The presence of anterior foci
indicates the risk of spreading to the rear of the spine (38). In the present study, these
disadvantages were avoided by selecting an appropriate operation
scheme: i) Since the posterior approach cannot completely clear the
lesion in all cases and dissemination is possible, a catheter was
inserted during surgery for local chemotherapy, through which
anti-TB drugs were directly administered; thereby, sufficient drug
supply to the site of the lesion was guaranteed and ii) TLIF
technology was used to gain access from a unilateral intervertebral
foramen, avoiding bilateral decompression as far as possible and
reducing the destruction of the posterior column.
The present study indicated that the TLIF approach
is sufficient in adults with spinal TB for the following reasons:
i) Effective chemotherapy via catheter is provided to sterilize the
vertebral body lesions without the requirement for excessive
anterior debridement or fusion; ii) Complications associated with
anterior approaches to the thoracolumbar spine may be avoided; iii)
TLIF technology may stabilize the vertebral column and is conducive
to vertebral fusion and stability and iv) Inter-body bone grafting
promotes interbody fusion, permitting patients to undertake early
rehabilitation.
However, the present study had certain deficiencies.
The amount of data obtained to support that TCLC was insufficient.
In addition, the follow-up duration was relatively short. A future
prospective study with long-term follow-up of patients treated with
a posterior approach, including abscess clearance, bone fusion and
internal fixation for the treatment of complex thoracic and lumbar
spinal TB is required to provide further evidence-based
outcomes.
In conclusion, the present study indicated that
application of TCLC for the treatment of spinal TB provides
satisfactory healing of the lesions. During surgery, TB lesions
were removed as far as possible. After the operation, local
chemotherapy with INH via catheter was essential for the successful
treatment of TB.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Natural
Science Foundation of Shaanxi Province, China (grant no.
2017JM8054).
Availability of data and materials
The data and materials used in the present study are
available upon reasonable request from the corresponding
author.
Authors' contribution
DL and LS participated in the study design, data
analysis and manuscript drafting. YM and YH were mainly responsible
for the patient treatment, data interpretation and revision of the
manuscript. DH collected the information of the participants of
this study. SJ and XH were involved in part of the patient
treatment and data analysis.
Ethics approval and consent to
participate
Ethics approval was obtained from the Ethics
Committee of Hong Hui Hospital (Xi'an, China) and all participants
provided written informed consent prior to the study.
Patient consent for publication
All the patients were informed and agreed with the
publication.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
TB
|
tuberculosis
|
|
ESR
|
erythrocyte sedimentation rate
|
|
CRP
|
C-reactive protein
|
|
TLIF
|
transforaminal-lumbar interbody
fusion
|
|
CT
|
computed tomography
|
|
INH
|
isonicotinic acid hydrazide
|
|
PCD
|
percutaneous catheter drainage
|
References
|
1
|
China Tuberculosis Control Collaboration,
. The effect of tuberculosis control in China. Lancet. 364:417–422.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Padmapriyadarsini C, Shobana M, Lakshmi M,
Beena T and Swaminathan S: Undernutrition & tuberculosis in
India: Situation analysis & the way forward. Indian J Med Res.
144:11–20. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zhang HQ, Tang MX and Wang YX: Using
multiple special formed titanium mesh cages to treat spinal
tuberculosis via posterior approach only. Orthop J Chin.
22:1353–1358. 2014.(In Chinese).
|
|
4
|
Rivas-Garcia A, Sarria-Estrada S,
Torrents-Odin C, Casas-Gomila L and Franquet E: Imaging findings of
Pott's disease. Eur Spine J. 22 (Suppl 4):S567–S578. 2013.
View Article : Google Scholar
|
|
5
|
Moon MS: Development in the management of
tuberculosis of the spine. Curr Orthop. 20:132–140. 2006.
View Article : Google Scholar
|
|
6
|
Hibbs RA: An operation for Pott's disease
of the spine. J Am Med Assoc. 59:433–436. 1912. View Article : Google Scholar
|
|
7
|
Albee FH: Transplantation of a portion of
the tibia into the spine for Pott's disease: A preliminary report
1911. Clin Orthop Relat Res. 460:14–16. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ito H, tsuchiya J and Asami G: A new
radical operation for Pott's disease. Report of ten cases. J Bone
Joint Surg. 16:499–515. 1934.
|
|
9
|
Hodgson AR and Stock FE: Anterior spinal
fusion a preliminary communication on the radical treatment of
Pott's disease and Pott's paraplegia. Br J Surg. 44:266–275. 1956.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mukhtar AM, Farghaly MM and Ahmed SH:
Surgical treatment of thoracic and lumbar tuberculosis by anterior
interbody fusion and posterior instrumentation. Med Princ Pract.
12:92–96. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kumar MN, Joseph B and Manur R: Isolated
posterior instrumentation for selected cases of thoracol-umbar
spinal tuberculosis without anterior instrumentation and without
anterior or posterior bone grafting. Eur Spine J. 22:624–632. 2013.
View Article : Google Scholar
|
|
12
|
Li S1, Li Z, Hua W, Wang K, Li S, Zhang Y,
Ye Z, Shao Z, Wu X and Yang C: Clinical outcome and surgical
strategies for late post-traumatic kyphosis after failed
thoracolumbar fracture operation: Case report and literature
review. Medicine (Baltimore). 96:e87702017. View Article : Google Scholar
|
|
13
|
Schofferman J, Slosar P, Reynolds J,
Goldthwaite N and Koestler M: A prospective randomized comparison
of 270 degree fusions to 360 degree fusions (circumferential
fusions). Spine (Phila Pa 1976). 26:E207–E212. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kim KT, Lee SH, Lee YH, Bae SC and Suk KS:
Clinical outcomes of 3 fusion methods through the posterior
approach in the lumbar spine. Spine (Phila Pa 1976). 31:1351–1357.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Benli IT, Acaroğlu E, Akalin S, Kiş M,
Duman E and Un A: Anterior radical debridement and anterior
instrumentation in tuberculosis spondylitis. Eur Spine J.
12:224–234. 2003.PubMed/NCBI
|
|
16
|
Jin D, Qu D, Chen J and Zhang H: One-stage
anterior interbody autografting and instrumentation in primary
surgical management of thoracolumbar spinal tuberculosis. Eur Spine
J. 13:114–121. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Pang X, Shen X, Wu P, Luo C, Xu Z and Wang
X: Thoracolumbar spinal tuberculosis with psoas abscesses treated
by one-stage posterior transforaminal lumbar debridement, interbody
fusion, posterior instrumentation, and postural drainage. Arch
Orthop Trauma Surg. 133:765–772. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhang HQ, Lin MZ, Shen KY, Ge L, Li JS,
Tang MX, Wu JH and Liu JY: Surgical management for multilevel
noncontiguous thoracic spinal tuberculosis by single-stage
posterior transforaminal thoracic debridement, limited
decompression, interbody fusion, and posterior instrumentation
(modified TTIF). Arch Orthop Trauma Surg. 132:751–757. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Singh K, Vaccaro AR, Kim J, Lorenz EP, Lim
TH and An HS: Biomechanical comparison of cervical spine
reconstructive techniques after a multilevel corpectomy of the
cervical spine. Spine (Phila Pa 1976). 28:2352–2358. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Güven O, Kumano K, Yalçin S, Karahan M and
Tsuji S: A single stage posterior approach and rigid fixation for
preventing kyphosis in the treatment of spinal tuberculosis. Spine
(Phila Pa 1976). 19:1039–1043. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Pombo F, Martín-Egaña R, Cela A, Díaz JL,
Linares-Mondéjar P and Freire M: Percutaneous catheter drainage of
tuberculous psoas abscesses. Acta Radiol. 34:366–368. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gupta S, Suri S, Gulati M and Singh P:
Ilio-psoas abscesses: Percutaneous drainage under image guidance.
Clin Radiol. 52:704–707. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Dinç H, Ahmetoğlu A, Baykal S, Sari A,
Sayil O and Gümele HR: Image-guided percutaneous drainage of
tuberculous iliopsoas and spondylodiskitic abscesses: midterm
results. Radiology. 225:353–358. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Soares Do Brito J, Tirado A and Fernandes
P: Surgical treatment of spinal tuberculosis complicated with
extensive abscess. Iowa Orthop J. 34:129–136. 2014.
|
|
25
|
Soares do Brito J, Batista N, Tirado A and
Fernandes P: Surgical treatment of spinal tuberculosis: An
orthopedic service experience. Acta Med Port. 26:349–356. 2013.(In
Portuguese).
|
|
26
|
Shi JD, Wang Q and Wang ZL: Primary issues
in the selection of surgical procedures for thoracic and lumbar
spinal tuberculosis. Orthop Surg. 6:259–268. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Garg B, Kandwal P, Nagaraja UB, Goswami A
and Jayaswal A: Anterior versus posterior procedure for surgical
treatment of thoracolumbar tuberculosis: A retrospective analysis.
Indian J Orthop. 46:165–170. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Pola E, Rossi B, Nasto LA, Colangelo D and
Logroscino CA: Surgical treatment of tuberculous spondylodiscitis.
Eur Rev Med Pharmacol Sci. 16 (Suppl 2):S79–S85. 2012.
|
|
29
|
Ma YZ, Cui X, Li HW, Chen X, Cai XJ and
Bai YB: Outcomes of anterior and posterior instrumentation under
different surgical procedures for treating thoracic and lumbar
spinal tuberculosis in adults. Int Orthop. 36:299–305. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
McDonnell MF, Glassman SD, Dimar JR II,
Puno RM and Johnson JR: Perioperative complications of anterior
procedures on the spine. J Bone Joint Surg Am. 78:839–847. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Qureshi MA, Khalique AB, Afzal W, Pasha IF
and Aebi M: Surgical management of contiguous multilevel
thoracolumbar tuberculous spondylitis. Eur Spine J. 22 (Suppl
4):S618–S623. 2013. View Article : Google Scholar
|
|
32
|
Zhang HQ, Guo CF, Xiao XG, Long WR, Deng
ZS and Chen J: One-stage surgical management for multilevel
tuberculous spondylitis of the upper thoracic region by anterior
decompression, strut autografting, posterior instrumentation, and
fusion. J Spinal Disord Tech. 20:263–267. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Zeng H, Shen X, Luo C, Xu Z, Zhang Y, Liu
Z and Wang X: Comparison of three surgical approaches for
cervicothoracic spinal tuberculosis: A retrospective case-control
study. J Orthop Surg Res. 10:1002015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Zeng H, Wang X, Pang X, Luo C, Zhang P,
Peng W, Wu P and Xu Z: Posterior only versus combined posterior and
anterior approaches in surgical management of lumbosacral
tuberculosis with paraspinal abscess in adults. Eur J Trauma Emerg
Surg. 40:607–616. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Güzey FK, Emel E, Bas NS, Hacisalihoglu S,
Seyithanoglu MH, Karacor SE, Ozkan N, Alatas I and Sel B: Thoracic
and lumbar tuberculous spondylitis treated by posterior
debridement, graft placement, and instrumentation: A retrospective
analysis in 19 cases. J Neurosurg Spine. 3:450–458. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Jain AK: Tuberculosis of the spine: A
fresh look at an old disease. J Bone Joint Surg Br. 92:905–913.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Tuli SM: Tuberculosis of the spine: A
historical review. Clin Orthop Relat Res. 460:29–38.
2007.PubMed/NCBI
|
|
38
|
Int Veld BA, Rettig TCD, de Heij N, de
Vries J, Wolfs JFC and Arts MP: Maintaining endotracheal tube cuff
pressure at 20 mmHg during anterior cervical spine surgery to
prevent dysphagia: A double-blind randomized controlled trial. Eur
Spine J. Oct 25–2018.(Epub ahead of print).
|