Introduction
Chronic heart failure (CHF) (1) is a group of clinical syndromes caused
by changes in cardiac structure and function caused by various
reasons, leading to the reduction of left ventricular filling and
ejection fraction. It is the final stage of development of various
cardiovascular diseases and is also the main cause of death
(2). Heart failure (HF) refers to
cardiac circulatory disorder syndrome caused by failing to fully
discharge venous return volume out of the heart due to dysfunction
of cardiac systolic and/or diastolic function, resulting in blood
deposition in venous system and insufficient blood perfusion in
arterial system. Such disorder syndrome is mainly manifested as
pulmonary congestion and vena cava congestion (3). HF is not an independent disease, but
the final stage of the development of heart diseases, most of which
begin with left HF (4). Therefore,
it is of great significance to find the disease in time and control
and treat it to remission.
Studies have shown that patients with CHF have
pathophysiological changes such as myocardial electrical
remodeling, which can be characterized by cardiac rhythm.
Therefore, electrocardiogram (ECG) of patients with CHF may have
special ECG manifestations (5). Some
studies have shown that myocardial interstitial collagen deposition
in patients with CHF and arrhythmia can affect the maintenance of
ventricular structure and cardiac function (6). Previous studies have shown that type
III procollagen amino-terminal peptide (PIIINP) is a metabolic
product during myocardial collagen synthesis, which can better
reflect the index of collagen fiber formation in vivo
(7). Brain natriuretic peptide (BNP)
is mainly synthesized in ventricular myocytes and secreted by the
left ventricle. It flows back into the small vein to the
interventricular septum vein and enters the circulation through the
coronary sinus (8,9). Ventricular wall tension, pressure
overload, myocardial ischemia, necrosis and injury can stimulate
the synthesis and release of BNP. BNP is a sensitive index
reflecting ventricular function and load, and is widely used in
evaluating cardiac function (10).
Therefore, the purpose of this investigation was to
monitor the condition of patients with CHF and arrhythmia by
observing the changes of ECG indexes, and to study the relationship
between ECG indexes and serum PIIINP and BNP.
Patients and methods
General information
From December 2017 to December 2018, 101 patients
with HF were collected. Among them, 48 patients with HF and slow
arrhythmia were in group A, including 31 males and 16 females, with
an average age of 57.6±3.7 years and a course of disease of
1.75±0.07 years, while 53 cases of those with HF and non-slow
arrhythmia were in group B, including 33 males and 20 females, with
an average age of 59.2±4.1 years and course of disease of 1.89±0.09
years. Further data are shown in Table
I. There was no statistical significance between the two
groups.
 | Table I.General data. |
Table I.
General data.
| Factor | Group A (n=48) | Group B (n=53) | χ2/t | P-value |
|---|
| Sex |
|
| 1.958 | 0.1439 |
| Male | 31 | 33 |
|
|
|
Female | 16 | 20 |
|
|
| Age | 57.6±3.7 | 59.2±4.1 | 1.743 | 0.814 |
| Course of
disease | 1.75±0.07 | 1.89±0.09 | 0.5912 | 0.3541 |
| Coronary heart
disease | 23 | 24 | 1.740 | 0.4583 |
| Hypertension | 13 | 15 | 1.348 | 0.3674 |
| Rheumatic heart
disease | 8 | 5 | 1.181 | 0.4931 |
| Dilated
cardiomyopathy | 4 | 9 | 1.331 | 0.2405 |
| NYHA |
| Class
II | 14 | 16 | 0.4710 | 0.7813 |
| Class
III | 25 | 27 | 0.5188 | 0.5960 |
| Class
IV | 9 | 10 | 0.001 | 0.9995 |
| Lown class III | 24 | 24 | 2.782 | 0.5949 |
| Lown class IV | 17 | 18 | 7.509 | 0.0234 |
| Lown class V | 7 | 11 | 0.1053 | 0.9487 |
The study was approved by the Ethics Committee of
Yantai Yuhuangding Hospital (Yantai, China). Signed informed
consents were obtained from the patients and/or the guardians.
Exclusion and inclusion criteria
Inclusion criteria (1) were CHF B with arrhythmia confirmed by
ECG and echocardiography, and left ventricular ejection fraction
≤40% (11). Exclusion criteria were:
i) thyroid and lung diseases; ii) sick sinus syndrome patients;
iii) those who did not wish to be included in this study.
Methods and detection indexes
Specimen collection
Altogether 2–3 ml venous blood of all the selected
patients were taken on admission, and the next day on an empty
stomach, and the relevant biochemical indexes were checked.
BNP test
Fasting venous blood of patients was collected, 15%
EDTA was added into anticoagulation test tube, and centrifuged at
1,509.3 × g at 4°C for 10 min with an effective centrifugal radius
of 15 cm. The blood was detected by chemiluminescence using
Pulangpuzs-300 series automatic biochemical analyzer (Hitachi 7180
type).
PIIINP detection
Fasting venous blood of patients was collected, 15%
EDTA was added to anticoagulation test tube, centrifuged at 1,509.3
× g at 4°C for 10 min with an effective centrifugal radius of 15
cm, and the separated serum was stored in a low temperature
refrigerator at −20°C for later use. Balanced radioimmunoassay was
used for determination, and radioimmunoassay reagent was provided
by Biotechnology Center of Hunan Pharmaceutical Research
Institute.
Detection of ECG index changes in the
two groups
After admission, the ECG changes of the two groups
were observed, including heart rate, Q-T interval, P-R interval and
QRS wave group, and recorded.
Correlation between serum PIIINP, BNP
and NYHA classification of cardiac function (12)
Patients with different NYHA classification of
cardiac function were grouped, and the expression levels of PIIINP
and BNP in the patients were detected. Through Pearson correlation
factor analysis, the correlation between serum PIIINP, BNP and NYHA
classification of cardiac function was analyzed.
Correlation between ECG indexes and
PIIINP and BNP
Through Pearson correlation factor analysis, the
correlation between ECG indexes and PIIINP and BNP expression level
was analyzed.
ROC curve analysis (13)
The receiver operating characteristic curve (ROC)
was used to analyze whether serum PIIINP and BNP had diagnostic
value in CHF with arrhythmia.
Statistical methods
This study used SPSS18.0 software (Bizinsight
(Beijing) Information Technology Co., Ltd.) to carry out
statistical analysis on the data. GraphPad Prism 6 software was
used to draw the illustrations in this study. Chi-square test was
used to compare the counting data, and mean ± standard deviation to
express the measurement data. t-test was emplyed to analyze the two
groups, and variance analysis to compare the multiple groups, and
Pearson correlation analysis was used to analyze the relationship
between variables. P<0.05 was considered to indicate a
statistically significant difference.
Results
Levels of serum PIIINP and BNP of
patients in the two groups
The content of serum PIIINP and BNP of patients in
the two groups showed that the serum PIIINP and BNP in group A were
significantly higher than those in group B (P<0.05). The levels
of PIIINP and BNP in serum of NYHA patients with different cardiac
functions, and those in serum of patients with class III were
significantly higher than those of group II (P<0.05), while
significantly lower than those of group IV (P<0.05) (Fig. 1).
Changes of ECG indexes in the two
groups
The ECG indexes such as heart rate, Q-T interval,
P-R interval and QRS wave of patients in the two groups were
examined. The results revealed that the heart rate and Q-T interval
of group A were significantly higher than those of group B
(P<0.05), and the P-R interval and QES wave in group A were
significantly lower than those in group B (P<0.05) (Fig. 2).
Correlation analysis
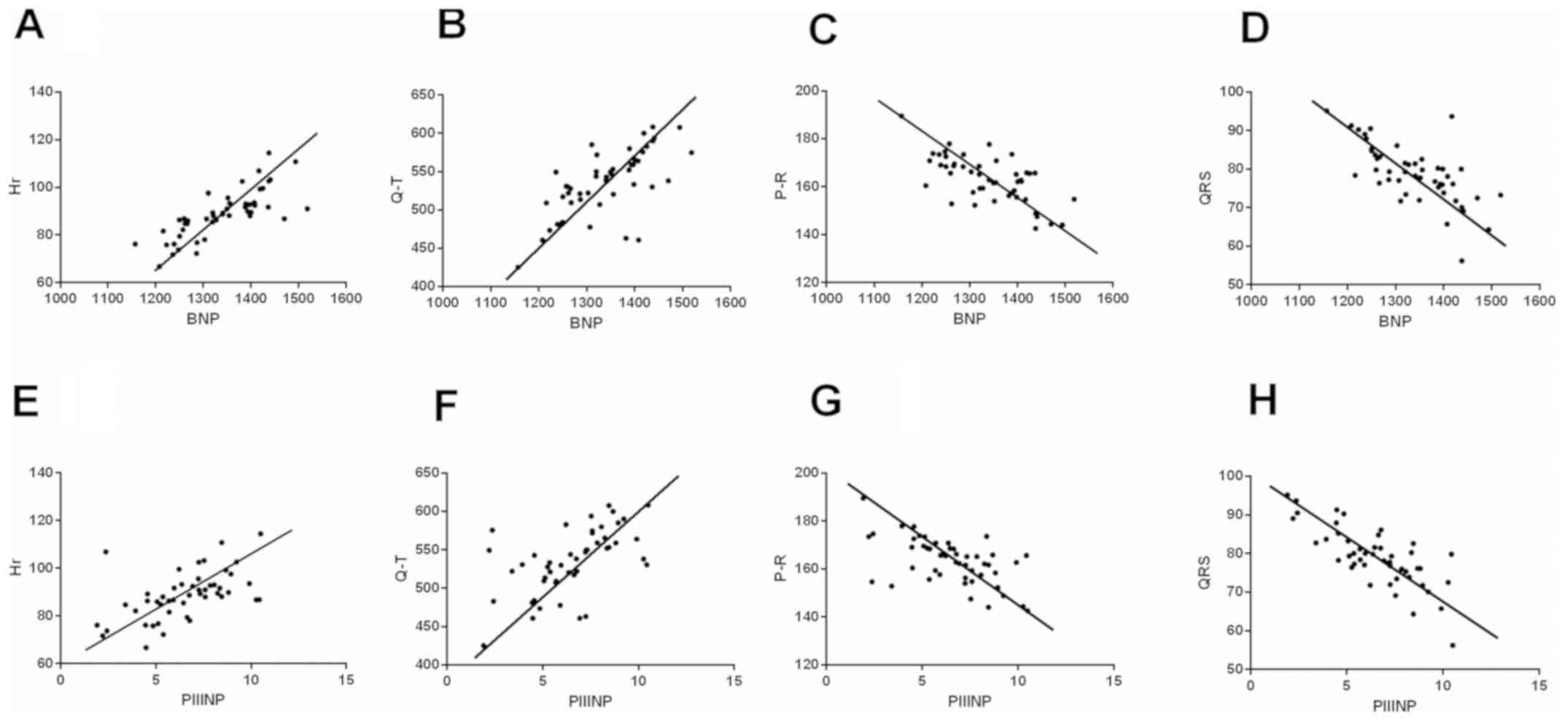
Pearson correlation analysis indicated that BNP was
correlated with Hr, G-T, P-R and QRS, positively correlated with Hr
and G-T (r=0.7749, r=0.6743), and was negatively correlated with
P-R and QRS (r=−0.6684, r=−0.6811). PIIINP was positively
correlated with Hr, G-T, P-R, and QRS (r=0.5509, r=0.5635), and was
negatively correlated with P-R and QRS (r=−0.5730, r=−0.7707). BNP,
PIIINP and NYHA had positive correlation (r=0.5804, r=0.5813)
(Figs. 3 and 4).
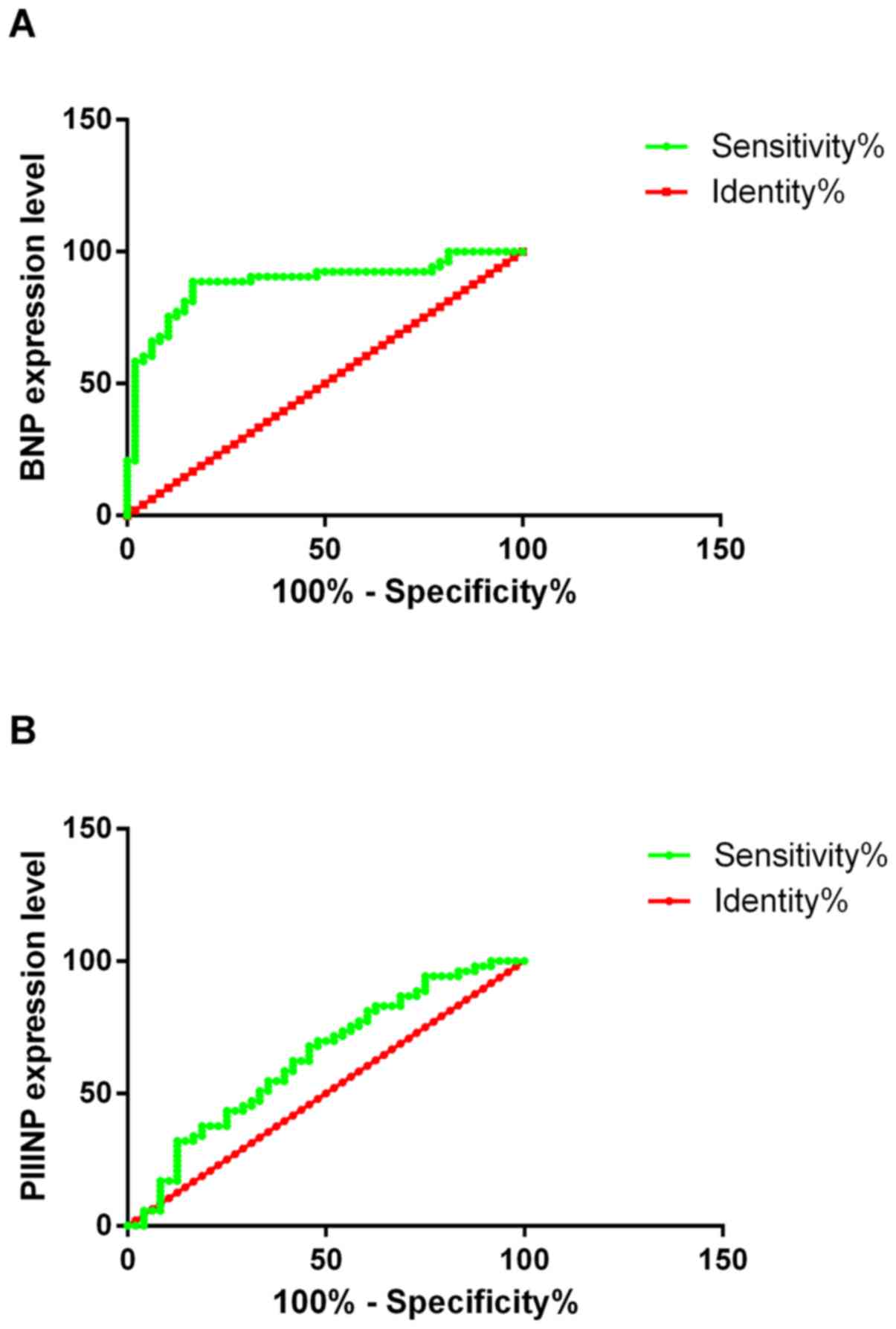
ROC curve analysis
ROC curve analysis represented that ACU of BNP in
diagnosing patients with CHF was 0.8829, the sensitivity was
69.51%, and the specificity was 81.61%; AUC of PIIINP in diagnosing
patients with CHF was 0.6340, the sensitivity was 73.64%, and the
specificity was 52.71%. (Table II
and Fig. 5).
 | Table II.ROC curve analysis. |
Table II.
ROC curve analysis.
| Indicators | AUC | SE | 95% CI | P-value |
|---|
| BNP | 0.8829 | 0.03548 | 0.8133–0.9524 | <0.001 |
| PIIINP | 0.6340 | 0.05561 | 0.5250–0.7431 | <0.001 |
Discussion
HF usually refers to the deterioration of myocardial
contractility, which leads to insufficient output to meet the needs
of collective metabolism, affecting the perfusion of organs and
tissues, and is often accompanied by passive hemorrhage of systemic
circulation and pulmonary circulation. CHF is mainly caused by
physiological changes, and the pathogenesis of ventricular
arrhythmia is mainly abnormal depolarization activity, increased
self-discipline and conduction reversion. When CHF progresses to
hypofilling function or ventricular pumping, or ventricular
tachycardia and ventricular arrhythmia is prematurely triggered,
leading to arrhythmia, and in serious cases, ventricular
fibrillation will even lead to death (14). Antiarrhythmic drugs are commonly used
in clinical treatment of CHF with ventricular arrhythmia, which can
effectively improve clinical symptoms and control arrhythmia, but
the treatment effect is slow.
Collagen in myocardial interstitium is mostly type
III collagen. Collagen, like other proteins, is transcribed into
mRNA in cells via DNA and then translated and expressed as
procollagen α peptide. The amino end and carboxyl end of
procollagen each have a non-collagen terminal peptide. After
hydroxylation, procollagen molecules form a triple helix, which is
secreted by cardiac fibroblasts after saccharification (15). Therefore, PIIINP can accurately
reflect the active process of collagen synthesis in cardiac tissue.
BNP is mainly produced in ventricles, and the release of BNP
increases with the increase of ventricular wall tension and load in
HF. At present, many studies have proved that BNP plays an
important role in the diagnosis and risk degree of HF (16,17). It
is also believed that BNP can be used as the mortality indicator of
patients with HF in hospital and at 6 months and one year after
discharge (18), but there is a lack
of research on arrhythmia (19).
This study found that the concentration of BNP in plasma of
ventricular arrhythmia group was significantly higher than that of
non-ventricular arrhythmia group, which might be due to the
increase of cardiac load caused by the change of hemodynamics
affected by ventricular arrhythmia.
ECG is a technique for recording changes in cardiac
electrical activity using an electrocardiograph. It is
non-invasive, convenient and inexpensive. It is the main detection
method for evaluating HF. This study revealed that common ECG
indicators were correlated with BNP and PIIINP proteins, which
suggested that BNP and PIIINP levels could be predicted. However,
ROC curve analysis of BNP and PIIINP in this study indicated that
BNP and PIIINP had diagnostic value for CHF, and could predict it
in advance in combination with ECG indexes.
In conclusion, ECG indicators were correlated with
BNP and PIIINP, and they showed diagnostic value for CHF. Using the
indexes to predict BNP and PIIINP levels was conducive to the
diagnosis of CHF.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YW wrote the manuscript, interpreted and analyzed
the data. XM designed the study and performed the experiments. YW
was responsible for the analysis and discussion of the data. Both
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Yantai Yuhuangding Hospital (Yantai, China). Patients who
participated in this research had complete clinical data. Signed
informed consents were obtained from the patients and/or the
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Morrissey RP, Czer L and Shah PK: Chronic
heart failure. Wiley Handbook of Current and Emerging Drug
Therapies. Am J Cardiovasc Drugs. 11:153–171. 2006. View Article : Google Scholar
|
|
2
|
Hunt SA, Baker DW, Chin MH, Cinquegrani
MP, Feldman AM, Francis GS, Ganiats TG, Goldstein S, Gregoratos G,
Jessup ML, et al American College of Cardiology/American Heart
Association, : ACC/AHA guidelines for the evaluation and management
of chronic heart failure in the adult: Executive summary. A report
of the American College of Cardiology/American Heart Association
Task Force on Practice Guidelines (Committee to revise the 1995
Guidelines for the Evaluation and Management of Heart Failure). J
Am Coll Cardiol. 38:2101–2113. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hunt SA, Abraham WT, Chin MH, Feldman AM,
Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K,
et al: ACC/AHA 2005 Guideline Update for the Diagnosis and
Management of Chronic Heart Failure in the Adult-Summary Article: A
Report of the American College of Cardiology/American Heart
Association Task Force on Practice Guidelines (Writing Committee to
Updat). J Am Coll Cardiol. 46:1116–1143. 2005. View Article : Google Scholar
|
|
4
|
Pocock SJ, Wang D, Pfeffer MA, Yusuf S,
McMurray JJ, Swedberg KB, Ostergren J, Michelson EL, Pieper KS and
Granger CB: Predictors of mortality and morbidity in patients with
chronic heart failure. Eur Heart J. 27:65–75. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hendry PB, Krisdinarti L and Erika M:
Scoring system based on electrocardiogram features to predict the
type of heart failure in patients with chronic heart failure.
Cardiol Res. 7:110–116. 2016. View
Article : Google Scholar : PubMed/NCBI
|
|
6
|
Petrovic D: Cytopathological basis of
heart failure - cardiomyocyte apoptosis, interstitial fibrosis and
inflammatory cell response. Folia Biol (Praha). 50:58–62.
2004.PubMed/NCBI
|
|
7
|
Lepojärvi ES, Piira OP, Pääkkö E,
Lammentausta E, Risteli J, Miettinen JA, Perkiömäki JS, Huikuri HV
and Junttila MJ: Serum PINP, PIIINP, galectin-3, and ST2 as
surrogates of myocardial fibrosis and echocardiographic left
venticular diastolic filling properties. Front Physiol. 6:2002015.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mukoyama M, Nakao K, Hosoda K, Suga S,
Saito Y, Ogawa Y, Shirakami G, Jougasaki M, Obata K and Yasue H:
Brain natriuretic peptide as a novel cardiac hormone in humans.
Evidence for an exquisite dual natriuretic peptide system, atrial
natriuretic peptide and brain natriuretic peptide. J Clin Invest.
87:1402–1412. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Anker SD, Coats AJ, Bonarjee VV, Caidahl
K, Lie RT, Nilsen DW, Sundsfjord JA and Dickstein K: Plasma brain
natriuretic peptide as an indicator of left ventricular systolic
function and long-term survival after acute myocardial infarction.
Circulation. 95:538–539. 1997.PubMed/NCBI
|
|
10
|
Nagaya N, Nishikimi T, Uematsu M, Satoh T,
Kyotani S, Sakamaki F, Kakishita M, Fukushima K, Okano Y, Nakanishi
N, et al: Plasma brain natriuretic peptide as a prognostic
indicator in patients with primary pulmonary hypertension. J
Cardiol. 37:110–111. 2001.(In Japanese). PubMed/NCBI
|
|
11
|
Degani R: Computerized electrocardiogram
diagnosis: Fuzzy approach. Methods Inf Med. 31:225–233. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nahler MPG: New York Heart Association
classification (NYHA). Dictionary of Pharmaceutical Medicine.
Springer; Vienna: pp. 121. 2009, View Article : Google Scholar
|
|
13
|
Wang Y, Xie B, Wan F, Xiao Q and Dai L:
Application of ROC curve analysis in evaluating the performance of
alien species potential distribution models. Biodiversity Sci.
15:365–372. 2007.(In Chinese). View Article : Google Scholar
|
|
14
|
Virk IS and Ip JR: The effect of cardiac
resynchronization on morbidity and mortality in heart failure.
Digest of the World Core Medical Journals 2005. https://doi.org/10.1111/j.1527-5299.2005.04176.xOctober
9–2008
|
|
15
|
Devereux RB and Reichek N:
Echocardiographic determination of left ventricular mass in man.
Anatomic validation of the method. Circulation. 55:613–618. 1977.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Droege ME, Mueller EW, Besl KM, Lemmink
JA, Kramer EA, Athota KP, Droege CA, Ernst NE, Keegan SP, Lutomski
DM, et al: Effect of a dalteparin prophylaxis protocol using
anti-factor Xa concentrations on venous thromboembolism in
high-risk trauma patients. J Trauma Acute Care Surg. 76:450–456.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Moe GW: BNP in the diagnosis and risk
stratification of heart failure. Heart Fail Monit. 4:116–122.
2005.PubMed/NCBI
|
|
18
|
Aldamiz-Echevarría Iraúrgui B, Muñiz J,
Rodríguez-Fernández JA, Vidán-Martínez L, Silva-César M,
Lamelo-Alfonsín F, Díaz-Díaz JL, Ramos-Polledo V and Castro-Beiras
A: Randomized controlled clinical trial of a home care unit
intervention to reduce readmission and death rates in patients
discharged from hospital following admission for heart failure. Rev
Esp Cardiol. 60:914–922. 2007.(In Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yonezawa E, Matsumoto K, Ueno K, Tachibana
M, Hashimoto H, Komamura K, Kamakura S, Miyatake K and Tanaka K:
Lack of interaction between amiodarone and mexiletine in cardiac
arrhythmia patients. J Clin Pharmacol. 42:342–346. 2002. View Article : Google Scholar : PubMed/NCBI
|