Introduction
The clavicle is one of the most commonly fractured
bones in the human body, accounting for 2.6-5% of all adult
fractures and 44% of injuries to the shoulder girdle (1). Nearly 80% of clavicle fractures occur
in the mid-shaft and the majority of these are displaced comminuted
fractures (2). For patients with
these fractures, nonunion rates following conservative treatment
may be as high as 15%, making them candidates for surgical
intervention (3,4).
Comminuted clavicle fractures with multiple
fragments or cortical splits pose a challenge for stable fixation
and early post-operative rehabilitation. Plate fixation is
frequently recommended for simple clavicle fractures; however, its
fixation strength is usually insufficient for comminuted clavicle
fractures. To achieve better stability, certain augmented supports,
including cerclage wirings and interfragmentary screws, are used in
combination with plate fixation (5,6).
Cerclage wires may be wrapped around the clavicle fracture above
and below the plate surface. Interfragmentary screws may be placed
separately or passed through the plate. Compared with cerclage
wirings, interfragmentary screws provide axial compressive force
and achieve absolute stability (7,8).
Clinical studies have revealed that augmented fixations produce
satisfactory surgical outcomes in patients (6,9).
However, there have been cases of implant failure and complications
after augmented fixation (10).
Therefore, the optimal augmented fixative remains controversial in
biomechanical contexts.
Finite element (FE) analysis is a powerful
biomechanical tool that allows for the control of various
parameters, including loading forces, fracture type and implants,
that would otherwise be difficult to assess in vivo or via
cadaveric experiments. FE analysis in clavicle fractures has been
used to study fixation stability, bone adaptation and for the
optimization of implant design (11-13).
The present study aimed to investigate the augmentations available
for plate fixation.
The purpose of the present study was to analyze the
biomechanical stability of clavicle plate fixation under the
following four augmentations: i) Cerclage wirings below the plate;
ii) cerclage wirings above the plate; iii) a single
interfragmentary screw; and iv) double interfragmentary screws. The
effects of these augmentations on fracture union and the degree of
bone and implant stress, model displacement and fracture
micro-motions were evaluated. The present study hypothesized that
double interfragmentary screw fixation provides greater stability
when compared with the other augmentations, enhancing the effect of
comminuted mid-shaft clavicle fracture treatment.
Materials and methods
Models of clavicle and surgery
simulation
The FE model was constructed using CT images of a
healthy male volunteer (age, 45 years; weight, 60 kg; height, 176
cm). The volunteer received a CT scan at Pudong New Area Peoples'
Hospital Affiliated to Shanghai University of Medicine and Health
Sciences due to shoulder periarthritis in October 2015. The
volunteer provided his written informed consent to the usage of his
images for model reconstruction and analysis. The modeled clavicle
consisted of cortical shell with a trabecular core. Isotropic
elastic properties corresponding to normal bone were assigned. The
elastic modulus was 1.0 GPa for cancellous bone and 17 GPa for
cortical bone. Furthermore, the Poisson's ratio was 0.3(13). The present study was approved by the
Ethics Committee of Pudong New Area Peoples' Hospital affiliated to
Shanghai University of Medicine and Health Sciences (Shanghai,
China; approval no. 2016-16).
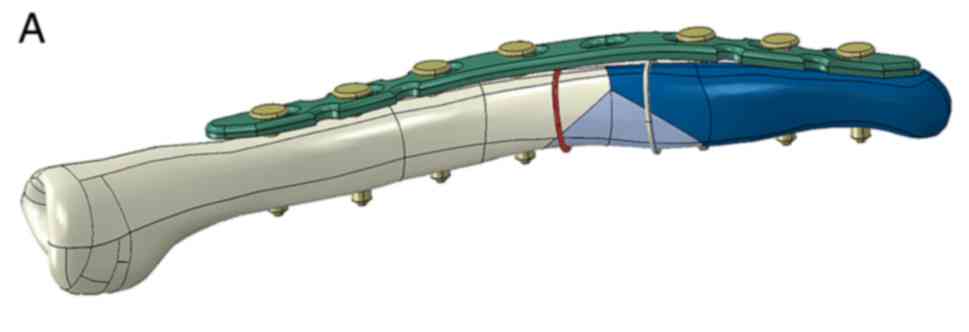
A type 15-B2 comminuted fracture was applied to the
model clavicle by partitioning a butterfly segment at the mid-shaft
(Fig. 1) in accordance with the AO
classification (14). The length,
width and height of the segment was 28, 15 and 10 mm, respectively.
The intrusion distance of the fragment into the fracture complex
was assumed to be 60%. The dimensions were adopted from a currently
unpublished clinical study, in which the CT images of 16 cases of
comminuted mid-shaft clavicle fractures were collected and the
basic characters of fragments were analyzed. There were 10 males
and 6 females, with a mean age of 38.8 (range, 24-58) years. They
received standard operative treatment at Pudong New Area Peoples'
Hospital Affiliated to Shanghai University of Medicine and Health
Sciences between August 2015 and May 2016 and provided written
informed consent for use of their data.
The implant consisted of a 3.5-mm locking
compressive plate (LCP; DePuy Synthes; Johnson & Johnson
Medical GmbH) containing 8 holes and was placed on the superior
surface of the clavicle. The internal and lateral parts of the
clavicle fracture were fixed using 4 and 3 screws, respectively.
The butterfly segment was fixed using four different augmentations
(Fig. 2): i) Double inner cerclage
wirings (DICW), which were wrapped around the segment only; ii)
double outer cerclage wirings (DOCW), which were wrapped around the
segment and the LCP; iii) a single 3.5-mm interfragmentary screw
(SIS), which was placed within the screw holes of the LCP; and iv)
double interfragmentary screws (DIS), which were inserted
perpendicularly into the plane of the fracture. The diameter of the
cerclage wirings was 1.0 mm and all implants were made from 316
low-vacuum-melting stainless steel with an elastic modulus of 186.4
GPa and a Poisson's ratio of 0.3(15).
Boolean operations were applied to the clavicle and
implants to reproduce the drilling and reaming employed during
clavicle fracture surgery (13).
Contact between bone and implant, and between bone fragments were
considered to be frictional. The coefficient of friction for the
bone-to-bone, bone-to-implant and implant-to-implant contacts were
0.46, 0.42 and 0.2, respectively (16).
Mesh convergence
The models were meshed using 4-node linear
tetrahedral element produced by Abaqus 6.13 (Dassault Systèmes SE).
The global and local mesh sizes of 1 and 0.6 mm resulted in a
<2% deviation of stress from a coarser mesh, as demonstrated by
a mesh convergence test. Therefore, the present study considered
the selected mesh sizes to be acceptable. The total number of
elements and nodes of the clavicle and four fixation models are
presented in Table I.
 | Table INumbers of nodes and elements in the
four fracture fixation models. |
Table I
Numbers of nodes and elements in the
four fracture fixation models.
| Item | DICW | DOCW | SIS | DIS |
|---|
| Nodes | 36,914 | 36,939 | 35,153 | 36,940 |
| Elements | 171,733 | 172,957 | 166,914 | 173,958 |
Boundary and loading conditions
A total of two loading cases were applied during the
present study: Cantilever bending and axial compression. A load of
100 N was applied in each case (17,18). The
forces were introduced on the acromial region, which started 15 mm
from the lateral end. The internal end of clavicle was fixed in all
degrees of freedom.
Data analysis
To calculate the model displacements along the
direction of loading forces, the axis of the clavicle shaft was
adjusted in line with the x-axis of the global coordinate system.
The axis of the clavicle shaft running through the midpoint of the
two ends of the clavicle was judged by eye. The y-axis adopted the
right-hand coordinate system. The z-axis was situated in the
frontal plane, vertical to the superior surface of the clavicle.
Model displacement was calculated by measuring the average
displacement of the acromial region. Fracture micro-motion was
defined as the change of fracture gap distance after load was
applied. The von Mises stress of fractures and implants of four
models were also recorded and analyzed. Statistical analysis was
performed in SPSS 16.0 software (SPSS Inc.) using an unpaired
t-test, with P<0.05 indicating statistically significant
differences.
Results
Von Mises stress
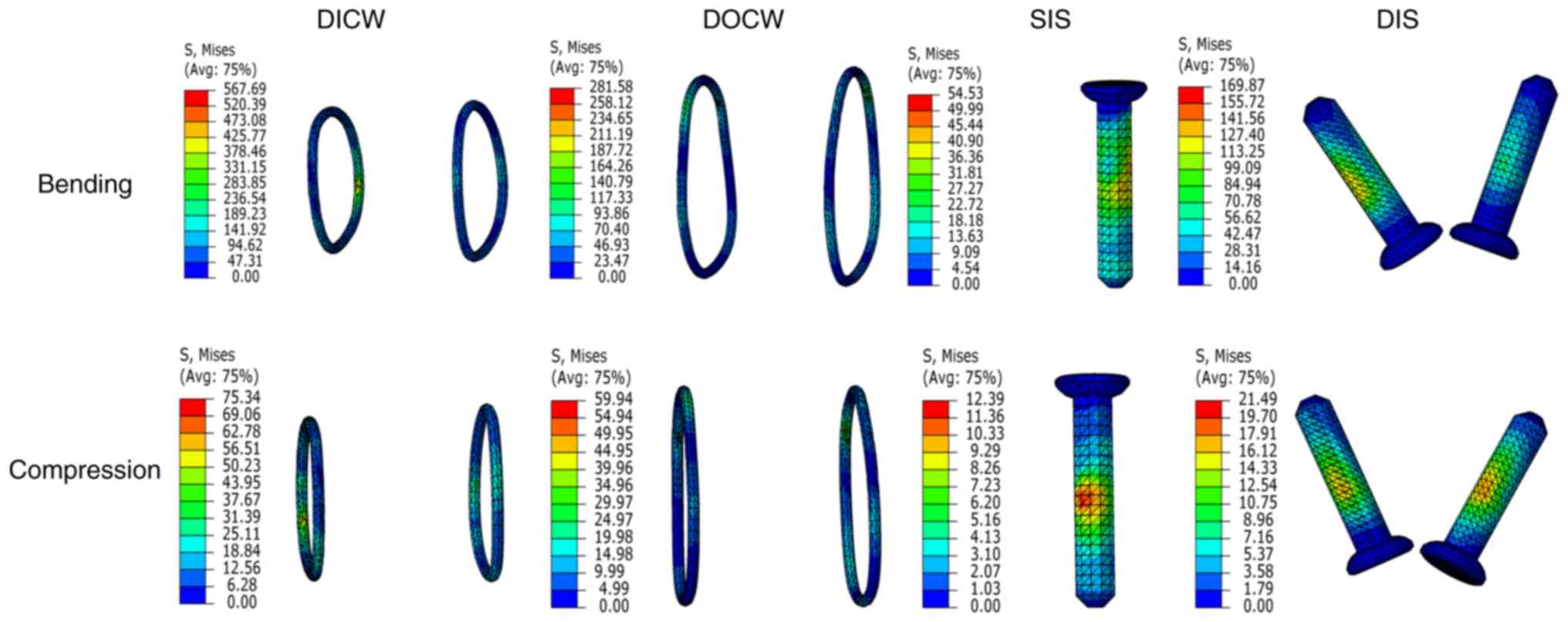
The stress distribution and maximum von Mises stress
of the four augmentations are presented in Figs. 3 and 4
and Table II. In general, stress as
a result of bending was higher than that caused by compression.
Under bending conditions, the DICW produced the highest stress
(567.69 MPa), followed by the DOCW (281.58 MPa). The stresses
applied to the DIS and SIS were 169.87 and 54.53 MPa, respectively.
Under compression, the maximum stresses of DICW, DOCW, DIS and SIS
were 75.34, 59.94, 21.49 and 12.39 MPa, respectively.
 | Table IIMaximum von Mises stress (MPa) of the
clavicle fracture model and implants under the four
augmentations. |
Table II
Maximum von Mises stress (MPa) of the
clavicle fracture model and implants under the four
augmentations.
| | Clavicle | Implant |
|---|
| Fixation method | Loading
condition | Internal part | Butterfly
segment | Lateral part | Plate | Interfragmentary
screw | Internal
ring/screw | Lateral
ring/screw |
|---|
| DICW | Bending | 141.52 | 523.20 | 450.60 | 348.28 | - | 567.69 | 186.43 |
| | Compression | 31.25 | 117.59 | 153.15 | 118.16 | - | 75.34 | 37.33 |
| DOCW | Bending | 115.59 | 192.15 | 74.04 | 506.64 | - | 262.67 | 281.58 |
| | Compression | 16.53 | 48.57 | 12.33 | 118.19 | - | 52.03 | 59.94 |
| SIS | Bending | 181.90 | 35.93 | 98.85 | 480.75 | 54.53 | - | - |
| | Compression | 32.02 | 4.81 | 13.18 | 117.99 | 12.39 | - | - |
| DIS | Bending | 107.31 | 31.92 | 26.02 | 269.40 | - | 169.87 | 74.25 |
| | Compression | 16.43 | 6.21 | 6.09 | 118.21 | - | 19.66 | 21.49 |
For the LCP, the maximum stress was concentrated at
the fracture site and internal 1/3 par under two loading
conditions. This was in agreement with previous biomechanical and
clinical reports (8-10,16) and maybe associated with the S-shape of
the plate. The stress of the LCP appeared to change when different
augmentations were applied during bending. The DOCW produced the
highest stress (506.64 MPa), which was 5, 47 and 31% higher than
that of SIS, DIS and DICW, respectively. However, the augmentations
produced similar stress to the LCP under compression.
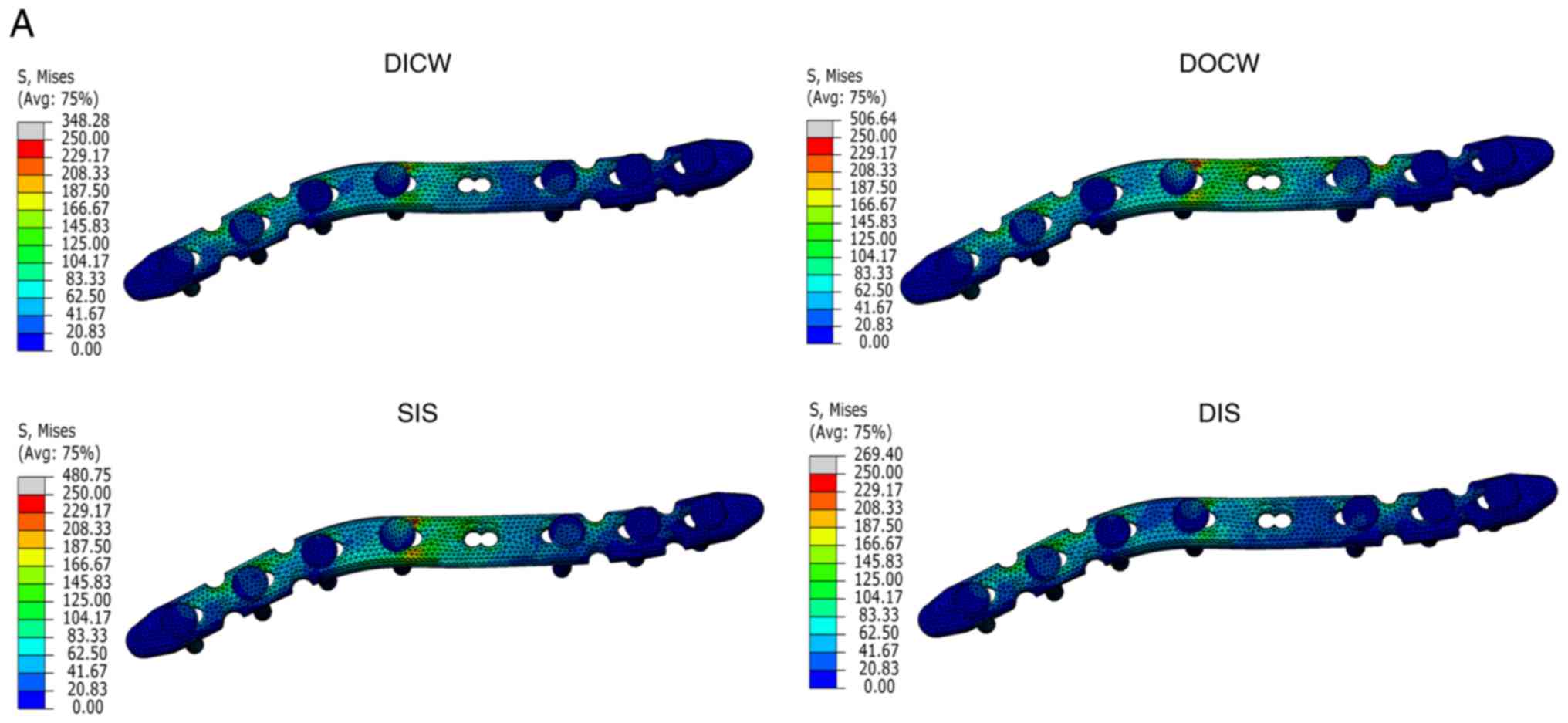
The von Mises stress distributions of the clavicle
fractures are presented in Fig. 5
and Table II. In each loading case,
the DICW produced the highest stress in the clavicle, particularly
at the contact area of wires and the butterfly segment. Bone
stresses under DOCW and SIS fixation were relatively lower, but the
internal and butterfly segments sustained considerable stress. Only
with the DIS alone, the bone stresses were within the normal range
of trabecular and cortical bone (19).
Fracture displacements
Acromial displacements and fracture micro-motion
distances are presented in Table
III. Under bending conditions, the greatest displacement was
observed in the DOCW fixation (2.59 mm) as compared with the SIS
(2.54 mm), DICW (2.31 mm) and DIS (2.24 mm; P<0.05). However,
their displacements under compression were similar. The DOCW
exhibited the highest micro-motions among the four supplements
(P<0.05), while the micro-motion of SIS, DIS and DICW was
similar.
 | Table IIIModel displacements and fracture
micro-motions (mm) under the four fixations. |
Table III
Model displacements and fracture
micro-motions (mm) under the four fixations.
| Fixation
method | Loading
condition | Acromial
displacement | Fracture
micro-motion |
|---|
| DICW | Bending | 2.31a | 0.17 |
| | Compression | 0.41 | 0.04 |
| DOCW | Bending | 2.59a | 0.24a |
| | Compression | 0.43 | 0.12a |
| SIS | Bending | 2.54a | 0.17 |
| | Compression | 0.42 | 0.04 |
| DIS | Bending | 2.24a | 0.15 |
| | Compression | 0.42 | 0.04 |
Discussion
The rigid internal fixation of clavicle fractures is
a necessary prerequisite for early post-rehabilitation and rapid
fracture union (20). The choice of
implant is critical for the treatment outcome of comminuted
clavicle fractures. To observe how an adequate fixation construct
should be established, an FE model of comminuted mid-shaft clavicle
fracture was developed in the present study from a 45-year-old male
with fixation by LCP and four augmentations. This model was
selected due to being representative of the majority of typical
comminuted and displaced multifragmentary fractures in adults
(average age, 43 years) (9). The
biomechanical performances of four augmented fixations were
assessed and compared in the present study. The results revealed
that the augmented fixations markedly altered the stability of
clavicle fracture fixation and may implicate fracture union.
Cerclage wiring is an efficient periosteal fixation
of fracture fragments for long bones, particularly the clavicle and
femur (5,21,22).
Although the risk of periosteal vascular strangulation is a
limitation that discourages surgeons to use cerclage wirings, one
study has demonstrated that they have no adverse effects on
cortical vascularity and produce satisfactory clinical outcomes
(23). However, the high tension and
small contact area of cerclage wiring fixation may result in the
local mechanical overload exceeding the strength of bone. When
cerclage wirings were wrapped around the clavicle in the present
study, high stresses were produced on bone and implants, exceeding
the yield strength of cortical bone. This may lead to a propensity
of bone necrosis and re-fracture. In addition, this result was
consistent with one previous clinical study (5). However, if cerclage wirings are placed
around the LCP, the plate may act as a support and the stress
placed upon bone tissue would markedly decrease. This was supported
by a study by Chen et al (6),
which demonstrated that 21 acute clavicle fractures treated with
DOCW fixations all healed uneventfully and without
complication.
Among the two cerclage wiring fixations, the results
of the present study indicated that the biomechanical stability of
DICW was greater than that of DOCW. This may be explained by the
‘loose-lock stability’ mechanism (21). ‘Loose-lock stability’ maybe divided
into two distinct phases: The loose-displace phase and the
lock-stable phase. In the first phase, fragments are allowed to
displace freely. However, with the increasing displacement of
fracture fragments, the wiring is tensioned and the segments are
subsequently stabilized, despite a certain degree of malalignment.
The DOCW may therefore exhibit larger fracture micro-motions, as
the cerclage would require to accommodate more room between the
plate and the clavicle.
Interfragmentary lag screw fixation is another
augmentation of plate osteosynthesis for comminuted clavicle
fractures. Depending on the size and geometry of fragments, one or
more screws maybe used to hold them. Biomechanical studies have
revealed that lag screw configurations are stiffer compared with
cerclage wiring or cable systems (7,8), which
was also supported by the FE results of the present study. Acromial
displacements of interfragmentary screw fixation were also smaller
than those of cerclage wirings. In clinical practice, lag screw
fixations exhibit more promising treatment results than cerclage
wirings (3,5). The results of the present study
indicated that the DIS should be preferably recommended over the
SIS in terms of lower stress magnitudes and better stability. This
is compatible with the aforementioned hypothesis.
The major surgical disadvantage of DIS is its double
drilling on the butterfly segment. Such a maneuver may induce the
risk of segment breakage and vascular damage. In view of this,
single lag screws are used. However, this compromises fixation
strength and a combination of lag screw, Kirshner pin, cerclage
wiring or plates may be required for the butterfly segment of a
clavicle fracture (24).
The position and orientation of the implant may
change the biomechanical environment of the fracture site. For the
interfragmentary lag screw, it may be placed either perpendicular
or oblique to the fracture plane. In most cases, the perpendicular
position is simple to place and provides nearly optimal function
(25). The present study indicated
that the DIS was more stable than the SIS, despite the SIS
providing more torque than the DIS. In addition, the screw of the
DIS was collinear to the principal stress direction under bending,
which may reinforce the strength of the fracture site. The results
indicated that, whether placed using the plate hole or
independently, the lag screw should be directed perpendicular to
the fracture plane.
The FE results of the present study demonstrated
that the augmented fixations may provide different construct
stabilities under different loading conditions. Under compression,
stress levels and acromial displacements were similar. However,
when bending, these levels varied greatly. This indicated that
augmented fixation may not effectively resist the bending force.
From biomechanical and anatomical perspectives, the major bending
force exerted on the clavicle originates from the gravity applied
to the affected upper limb. This suggests that suspension of the
affected limb after surgery is required. In addition, the
weight-bearing rehabilitation of the affected limb, or any practice
which may apply bending forces to the clavicle, should be
avoided.
The fracture micro-motion is not only a key
parameter of fixation stability, but also reflects the quality and
quantity of callus formations and fracture healing. Fracture
micro-motions between 0.15 and 1.0 mm have been determined to be
optimal for bone union, and hence, a certain amount of micro-motion
is required for healing (26). The
present study revealed that the fracture micro-motions in all
conditions were approximately within the suggested range,
indicating that bone regeneration or healing would have
resulted.
Despite the explicit qualitative and quantitative
results obtained, the present study has a clear limitation in that
no experimental test was performed to validate the results of FE.
However, it should be noted that the aim was to investigate the
clinical trends rather than absolute values. In this respect, the
lack of experimental validation is a justified limitation. In
addition, the reliability of the calculated results was further
guaranteed by the use of an FE model, which was developed using one
that was previously validated (10).
Furthermore, convergence tests were carefully performed to
guarantee the precision of FE analysis.
In conclusion, the SIS, DIS and DOCW may be used as
augmentations of LCP fixation for comminuted mid-shaft clavicle
fractures. The DIS featured improved fixation stability and lower
stress concentration when compared with those of other methods and
should be recommended for comminuted mid-shaft clavicle fracture.
The DICW may also be used to aid fracture reduction and plate
placement during surgery but should be avoided as a permanent
fixation.
Acknowledgements
We are grateful to Dr Kuan Wang from the
Rehabilitation Department of Yangzhi Rehabilitation Hospital,
Tongji University School of Medicine (Shanghai, China) for his help
and advice.
Funding
This study was supported by the general project of
Shanghai Municipal Health Bureau (grant no. 201840137).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MN, JM, WXN and FFZ designed the study and wrote the
first draft of the manuscript. SMSG and FFZ collected the data.
DWCW was responsible for finite element modeling. CYJL and MZ
participated in data analysis and interpretation and revision of
the manuscript. All authors have read and approved the final
version of the paper.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Pudong New Area Peoples' Hospital affiliated to Shanghai Health
University (approval no. 2016-16; Shanghai, China).
Consent for publication
The volunteer provided written informed consent for
the publication of his digital images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Postacchini F, Gumina S, De Santis P and
Albo F: Epidemiology of clavicle fractures. J Shoulder Elbow Surg.
11:452–456. 2002.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kulshrestha V, Roy T and Audige L:
Operative versus nonoperative management of displaced midshaft
clavicle fractures: A prospective cohort study. J Orthop Trauma.
25:31–38. 2011.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Shen WJ, Liu TJ and Shen YS: Plate
fixation of fresh displaced midshaft clavicle fractures. Injury.
30:497–500. 1999.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Canadian Orthopaedic Trauma Society.
Nonoperative treatment compared with plate fixation of displaced
midshaft clavicular fractures. A multicenter, randomized clinical
trial. J Bone Joint Surg Am. 89:1–10. 2007.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Shin SJ, Do NH and Jang KY: Risk factors
for postoperative complications of displaced clavicular midshaft
fractures. J Trauma Acute Care Surg. 72:1046–1050. 2012.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Chen CH, Chen JC, Wang C, Tien YC, Chang
JK and Hung SH: Semitubular plates for acutely displaced
midclavicular fractures: A retrospective study of 111 patients
followed for 2.5 to 6 years. J Orthop Trauma. 22:463–466.
2008.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Faraj AA, Naraen A and Twigg P: A
comparative study of wire fixation and screw fixation in
arthrodesis for the correction of hallux rigidus using an in vitro
biomechanical model. Foot Ankle Int. 28:89–91. 2007.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Matloub HS, Jensen PL, Sanger JR, Grunert
BK and Yousif NJ: Spiral fracture fixation techniques. A
biomechanical study. J Hand Surg [Br]. 18:515–519. 1993.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Smekal V, Oberladstaetter J, Struve P and
Krappinger D: Shaft fractures of the clavicle: Current concepts.
Arch Orthop Trauma Surg. 129:807–815. 2009.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Wijdicks FJ, Van der Meijden OA, Millett
PJ, Verleisdonk EJ and Houwert RM: Systematic review of the
complications of plate fixation of clavicle fractures. Arch Orthop
Trauma Surg. 132:617–625. 2012.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Favre P, Kloen P, Helfet DL and Werner CM:
Superior versus anteroinferior plating of the clavicle: A finite
element study. J Orthop Trauma. 25:661–665. 2011.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Huang TL, Chen WC, Lin KJ, Tsai CL, Lin KP
and Wei HW: Conceptual finite element study for comparison among
superior, anterior, and spiral clavicle plate fixations for
midshaft clavicle fracture. Med Eng Phys. 38:1070–1075.
2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Ni M, Niu W, Wong DW, Zeng W, Mei J and
Zhang M: Finite element analysis of locking plate and two types of
intramedullary nails for treating mid-shaft clavicle fractures.
Injury. 47:1618–1623. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Marsh JL, Slongo TF, Agel J, Broderick JS,
Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B,
et al: Fracture and dislocation classification compendium - 2007:
Orthopaedic Trauma Association classification, database and
outcomes committee. J Orthop Trauma. 21:S1–S133. 2007.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Cronskär M, Rasmussen J and Tinnsten M:
Combined finite element and multibody musculoskeletal investigation
of a fractured clavicle with reconstruction plate. Comput Methods
Biomech Biomed Engin. 18:740–748. 2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Goffin JM, Pankaj P and Simpson AH: The
importance of lag screw position for the stabilization of
trochanteric fractures with a sliding hip screw: A subject-specific
finite element study. J Orthop Res. 31:596–600. 2013.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Iannolo M, Werner FW, Sutton LG, Serell SM
and VanValkenburg SM: Forces across the middle of the intact
clavicle during shoulder motion. J Shoulder Elbow Surg.
19:1013–1017. 2010.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Scepi M, Faure JP, Ridoux N, Kamina P and
Richer JP: A three-dimensional model of the shoulder girdle. Forces
developed in deltoid and supraspinatus muscles during abduction.
Surg Radiol Anat. 26:290–296. 2004.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Bayraktar HH, Morgan EF, Niebur GL, Morris
GE, Wong EK and Keaveny TM: Comparison of the elastic and yield
properties of human femoral trabecular and cortical bone tissue. J
Biomech. 37:27–35. 2004.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Asadollahi S, Hau RC, Page RS, Richardson
M and Edwards ER: Complications associated with operative fixation
of acute midshaft clavicle fractures. Injury. 47:1248–1252.
2016.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Perren SM, Fernandez Dell'Oca A, Lenz M
and Windolf M: Cerclage, evolution and potential of a Cinderella
technology. An overview with reference to periprosthetic fractures.
Acta Chir Orthop Traumatol Cech. 78:190–199. 2011.PubMed/NCBI
|
|
22
|
Lenz M, Lehmann W and Wähnert D:
Periprosthetic fracture fixation in osteoporotic bone. Injury 47
(Suppl 2). S44–S50. 2016.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Kirby BM and Wilson JW: Effect of
circumferential bands on cortical vascularity and viability. J
Orthop Res. 9:174–179. 1991.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Misaghi A, Doan J, Bastrom T and Pennock
AT: Biomechanical Evaluation of Plate Versus Lag Screw Only
Fixation of Distal Fibula Fractures. J Foot Ankle Surg. 54:896–899.
2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Baumgart FW, Cordey J, Morikawa K, Perren
SM, Rahn BA, Schavan R and Snyder S: AO/ASIF self-tapping screws
(STS). Injury 24 (Suppl 1). S1–S17. 1993.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Jagodzinski M and Krettek C: Effect of
mechanical stability on fracture healing - an update. Injury. 38
(Suppl 1):S3–S10. 2007.PubMed/NCBI View Article : Google Scholar
|