Introduction
The research regarding intraocular tamponade
products is one of the most challenging and interesting areas in
ophthalmology; it began more than a century ago. In the early
1960s, Dr Paul Cibis began to inject silicon oil in vitro to
animals, in order to provide a permanent support to the retina, but
the anatomical and functional outcomes were not the expected ones
(1-3).
In The Netherlands, Zivojnović popularized the technique and
contributed greatly to its use (4).
In 1992, the Silicone Oil Study, a prospective, multicenter,
randomized, controlled clinical trial showed that silicone oil was
superior to SF6 and equivalent to the perfluorocarbon gas in the
treatment of vitreoretinal proliferation. Following these studies,
the USA Food and Drug Administration (FDA) approval for its use as
a tamponade product in 1994 triggered marketing and use worldwide
(5-9).
The first indications of silicone oil use were:
Ocular trauma, severe proliferative diabetic retinopathy,
complicated retinal detachment caused by proliferative retinopathy
or viral retinitis and giant retinal tears, due to the silicone oil
ability to displace aqueous humor from the retinal surface maintain
the application of the neurosensory retina to the retinal pigment
epithelium (10).
At present, new indications for silicone oil use are
possible, such as chronic and persistent macular hole, chronic
uveitis with hypotony, retinal detachment due to macular hole in
myopic eyes, and colobomatous retinal detachment (11,12). A
great advantage of the silicone oil is that it provides support
over a long period of time until retinal recovery occurs.
In the case of retinal detachment, silicone oil is
usually removed after 3-6 months, because it is thought that it is
enough for the eye to recover with minimal risk for the development
of proliferative vitreoretinopathy (13).
In addition, in patients who travel by air, in
children and elderly patients (who cannot maintain a correct
postoperative position), silicone oil is a first choice (14).
Retinal detachment surgery is a relative emergency
surgery meaning that patients undergo this surgery within 24-48 h
after the onset of vision loss. Furthermore, surgery is the only
possible remedy in the event of retinal detachment. Different
interventions exist and the choice is made according to the
characteristics of the patient's pathology.
The objectives of the surgery sought in retinal
detachment are: To heal or plug the tear in the retina, to puncture
the liquid present between the two retinal layers, to re-approach
the neuroepithelium of the pigment epithelium in order to
reconstitute the anatomically and physiologically normal retina,
and to create an adhesive scar between the retina and the fundus of
the eye, in order to stabilize the retina and prevent recurrence
(15,16).
Silicone oil is injected at the end of the surgical
procedure, when membrane dissection has already been performed, all
lesions are sealed and released from the traction forces. Air-fluid
exchange occurs and between 3-4 cm³ of silicone oil of 1,000 or
5,000 centistokes is injected (17).
In the postoperative period, the patient should be
placed in ventral decubitus, in order to avoid the contact of
silicone oil with the cornea and the posterior face of the
intraocular lens (18).
Large population-based studies of retinal detachment
have an annual incidence of about 1 in 10.000, and a family
aggregation study estimated a 3% lifetime risk at 85.2 years
(19). White and Asian populations
have similar rates, with a lower incidence among individuals of
African descent (20,21). The average age of presentation is
approximately 60 years, the sexes being equally affected.
Due to the fact that the surgery for retinal
detachment involves retrobulbar anesthesia and to the potential
complications induced by the surgery and silicone oil, patients
were screened for other associated disease and treatment options
(22-29).
However, post-operatory complications of the
silicone oil tamponade also occur. The use of silicone oils has no
short- or medium-term side effects. Patients should be monitored
regularly. They are usually seen several times in the first months,
then 3-4 times a year, as long as silicone oil persists in the
eye.
Early complications include: i) Post-operatory
ocular inflammation that is almost constant. It is related to
severe trauma and initial pathology. However, silicone oil,
especially heavy silicone oil, is considered pro-inflammatory.
Serum anti-silicon antibodies were found in 35.7% of patients with
silicone tamponade, and up to 83% of those with intraocular
silicone oil (30). ii) Variation
of intraocular pressure pertains to early postoperative ocular
hypertension which is often evident after silicone oil tamponade.
It is related to immediate post-operatory inflammation and, more
rarely, to excessive filling, which requires a partial discharge of
silicone oil present. Chronic ocular hypertonia may occur,
especially in the case of prolonged tamponade. This may be related
to decompensation of pre-existing hypertension, prolonged steroid
prescription, chronic trabeculitis through trabecular adhesions, or
migration of silicon microemulsion particles into trabecular
meshwork (31,32).
Medium- or long-term complications include: i)
Refraction disorders: Due to its refractive index, silicone oil
tamponade causes a change in the patient's refraction. Silicone is
responsible for a hypermetropic of 3-7 diopters in phakic eyes and
a myopia of 5 diopters in aphakic eyes. It is not just a
complication, but rather a disorder that will last only during the
intraocular presence of silicone (30). ii) The appearance of cataracts is a
frequent complication after silicone oil tamponade. The contact
between the silicone bubbles and the posterior capsule of the lens
prevents the diffusion of nutrients and leads to the development of
a posterior subcapsular cataract. After silicone oil tamponade
62.5% of patients develop cataracts up to 3 months, while the
incidence is 100% over 6 years (33). iii) Emulsification is the second
most common complication associated with silicone oil tamponade. It
is defined as the fragmentation of a single silicone bubble in more
bubbles of different diameters. Emulsification changes the silicone
tamponade power resulting in a decrease in its ability to block
dehiscence. Silicone microbubbles may be able to migrate to the
anterior chamber and to the trabecular meshwork, and can cause
edema keratopathy or intraocular hypertension (8). Some authors observed emulsification 2
weeks after injection. Previous findings showed that, the average
emulsification time of silicone 1,000 was 13.2 months (5-24
months), which was significantly higher than the average tamponade
time (34,35). iv) Contact of silicone oil with
corneal endothelium can cause corneal decompensation and band
keratopathy. Complications are secondary to the migration of
silicone oil into the anterior chamber, resulting in discontinuity
of endothelial metabolism and precipitation of calcium salts
(36).
Literature reported an incidence of keratopathy of
up to 30% of patients after 6 months of treatment (37,38).
Thus, the aim of the present study was to evaluate
the loss of corneal endothelial cells in patients undergoing
complex retinal detachment, which required internal tamponade with
silicone oil of 1,000 centistokes.
Materials and methods
Ethics approval and patient
consent
The present study is a retrospective,
interventional, comparative assessment with consecutive enrolment
of patients diagnosed with rhegmatogenous or tractional retinal
detachment requiring surgery. All subjects provided written
informed consent to be subjected to ocular surgery for retinal
detachment, prior to enrolment. Ethics Committee (number 401)
approval was obtained from ‘Dr. Carol Davila’ Central Military
University Emergency Hospital Bucharest and was conducted in
accordance with the Declaration of Helsinki and with the
International Standard of Good Clinical Practice (ICH-GCP E6 Step
4).
Patients
A total of 20 patients (7 males,13 females, aged
54-70 years) diagnosed with rhegmatogenous or traction retinal
detachment that requires as a method of treatment posterior
vitrectomy adjusted with silicone oil endotamponade, were selected
from the Department of Ophthalmology of the ‘Dr. Carol Davila’
Central Military Emergency University Hospital in Bucharest.
The inclusion criterion was the diagnosis of
rhegmatogenous or tractional retinal detachment requiring surgery.
The exclusion criteria included any coexisting corneal or retinal
disease, history of eye trauma or any other eye intervention
performed in the past other than cataract.
The patients were divided into 2 groups: Group 1 (9
females, 3 males, aged, aged 54-70 years) included subjects who had
a natural lens in the operated eye and group 2 (4 females, 4 males,
aged 58-69 years) included those who were pseudophakic in the eye
where the surgery was performed.
Methods
Non-contact corneal specular microscopy was used to
measure the following parameters: Mean endothelial cell density
(MCD), average cell area (AVG), coefficient of variation in cell
size (CV), percentage of hexagonal cells (HEX) and corneal
thickness (CT) at baseline representing surgery and then 3 months
after the surgery was completed. Of the several measurements, the
one that showed maximum counted endothelial cells was chosen. As a
control method, the patient's other unoperated eye was used.
Surgery was performed under retrobulbar anesthesia
by the same surgeon for all the patients. After topical
disinfection with povidone-iodine, a sterile field and lid speculum
were applied. The surgery consisted of: 25 gauge total posterior
vitrectomy, locating the retinal hole/holes and performing a laser
blockage around the hole and once the retinal attachment was
obtained the air exchange was changed to silicone oil of 1,000
centistoke.
Preoperatively and 3 months postoperatively,
bilateral corneal specular microscopy was performed in all the
patients to count endothelial cells, coefficient of variation,
central cell area, percentage of hexagonal cells and corneal
thickness.
Patients were subsequently discharged after
confirmation of retinal attachment and then re-evaluated after
three months, using corneal specular microscopy; the results were
recorded.
All determinations of the studied values were
performed using similar working techniques. For the processing and
systematization of the data, the Excel program of the Microsoft
Office 365 suite was used. The graphical representations, as well
as the statistical analysis of the data were performed using the
same program, together with ‘add-ins’, such as WinStat and XL-stat.
For the calculation of the statistical significance of the obtained
results, online support was provided by Professor Richard
Lowry-Vassar College Poughkeepsie (Poughkeepsie, NY, USA), through
the link www.vassarstats.net.
Statistical analysis
In order to establish the relationships between
various values of the analyzed coefficients, the average values
were calculated, as well as the mean ± standard deviation or
standard error of Student's test (t-test), and its statistical
significance was represented by P-values. The statistical
significance of the results was interpreted according to the value
of the coefficient p: P>0.05 indicated the results were not
statistically significant; for P-values between 0.05 and 0.001 the
results were considered highly statistically significant, while
P-values <0.001 were considered very highly statistically
significant.
Results
Patients
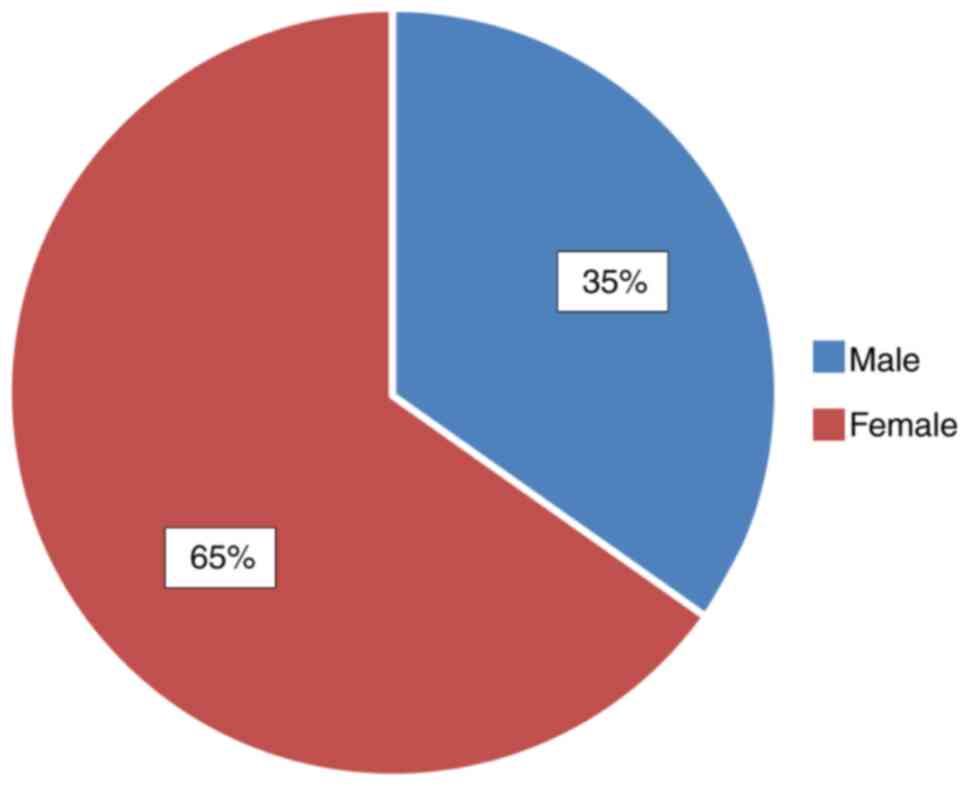
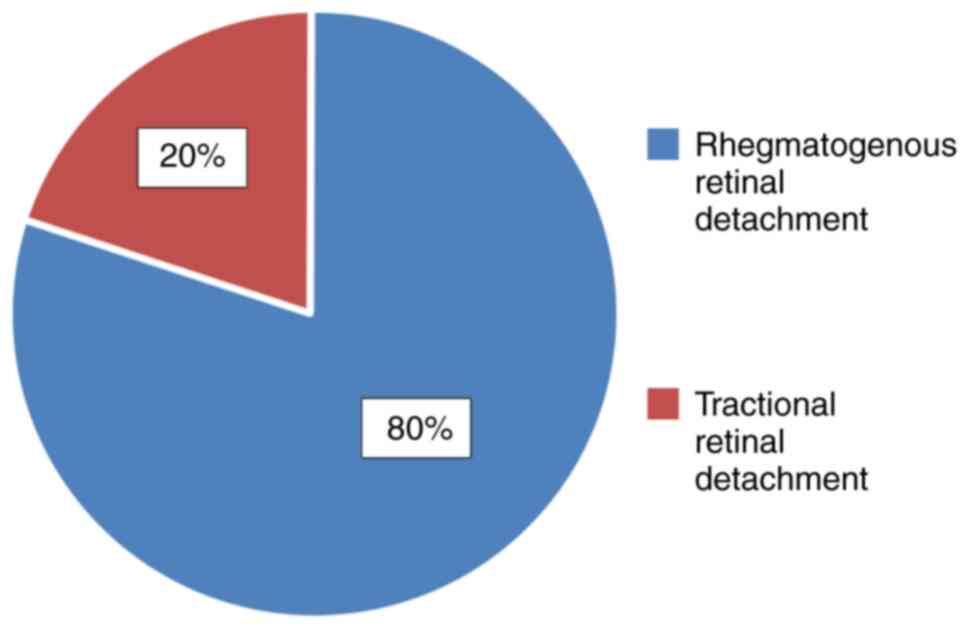
Patient demographic data are presented in Fig. 1. Patient surgical indications were
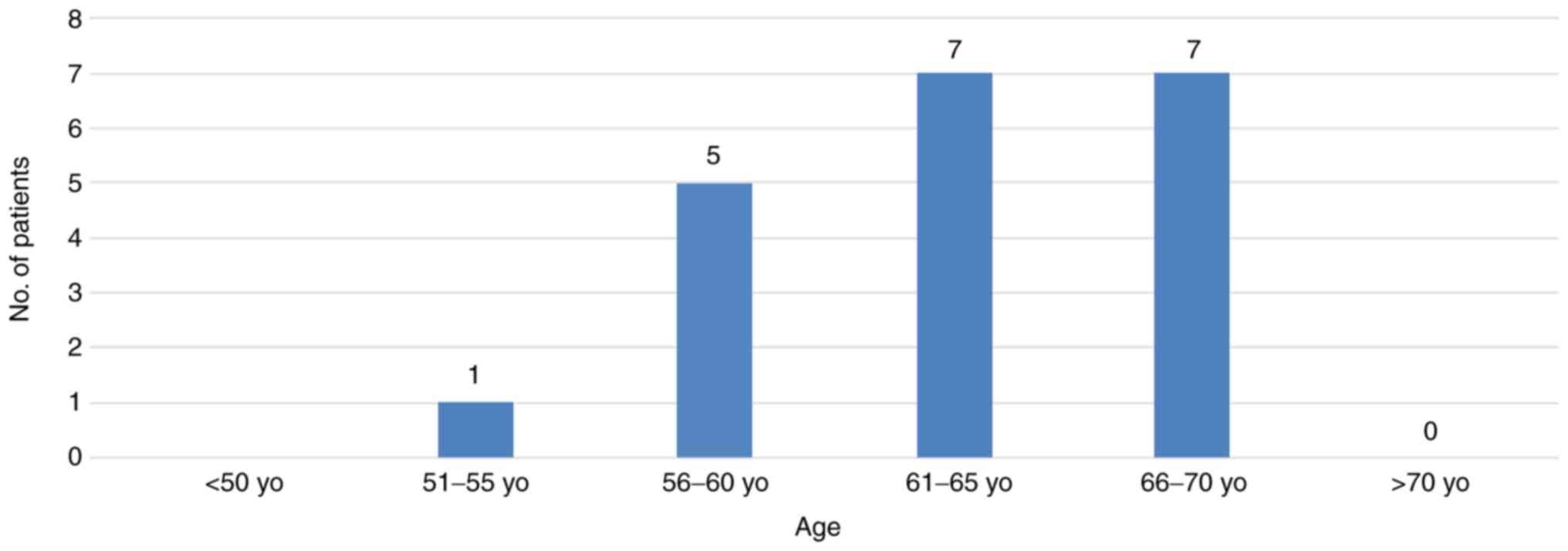
rhegmatogenous and tractional retinal detachment (Fig. 2). Patient distribution according to
age is presented in Fig. 3.
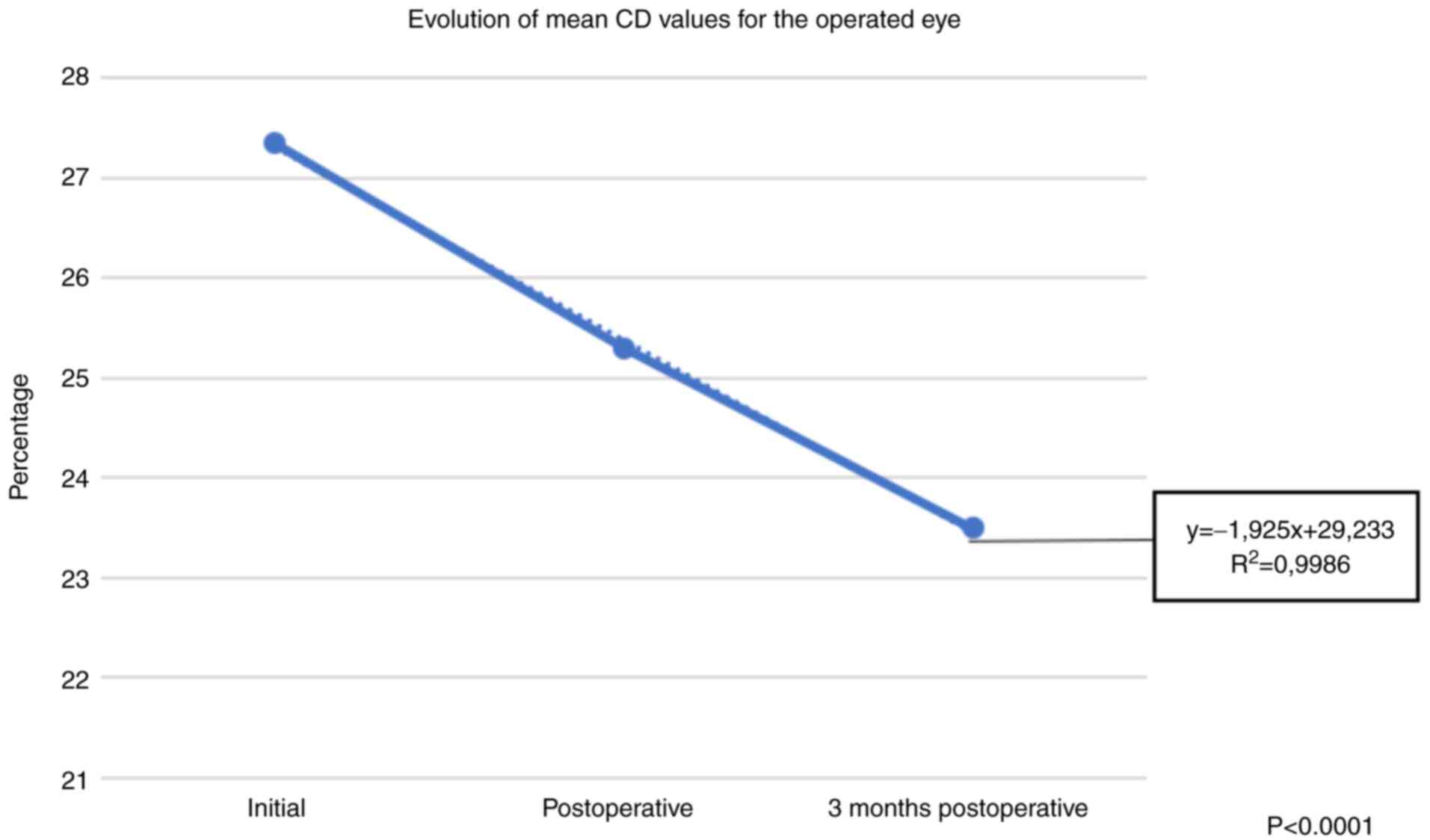
Various parameters
MCD, CV, AVG, HEX and CT values of all groups at
baseline, postoperative and three months postoperatively are shown
in Fig. 4, Fig. 5, Fig.
6, Fig. 7 and Fig. 8. For the parameters MCD, AVG, CV,
HEX a linear decrease was observed both immediately postoperatively
(MCD with 1.22%, AVG with 12.05%, CV with 7.50%, HEX with 4.19%)
(Table I) and after 3 months (MCD
with 3.61%, AVG with 14.04%, CV with 14.08%, HEX with 7.78%)
(Table II).
 | Table IComparison between the postoperative
values of the analyzed parameters for all patients. |
Table I
Comparison between the postoperative
values of the analyzed parameters for all patients.
| Variables | Operated eye | Non-operated
eye |
|---|
| MCD average
postoperative | 2,171.95
(-1.22%) | 2,525.6 |
| Standard
deviation | 564.92 | 466.69 |
| Standard error | 163.851 |
| 95% CI |
21.9507-685.3493 |
| T-test | 2.158 |
| P-value | 0.04a |
| CV average
postoperative | 25.3 (-7.5%) | 28.2 |
| Standard
deviation | 6.197580173 | 4.843552415 |
| Standard error | 1.759 |
| 95% CI | -0.6606-6.4606 |
| T-test | 1.649 |
| P-value | 0.1 |
| AVG average
postoperative | 403.75
(-12.5%) | 418.3 |
| Standard
deviation | 118.5752398 | 125.7756336 |
| Standard error | 38.652 |
| 95% CI |
-63.6970-92.7970 |
| T-test | 0.376 |
| P-value | 0.7 |
| HEX average
postoperative | 65.25 (-4.19%) | 69.15 |
| Standard
deviation | 6.08173495 | 4.475209492 |
| Standard error | 1.688 |
| 95% CI | 0.4820-7.3180 |
| T-test | 2.31 |
| P-value | 0.03a |
| CT average
postoperative | 572.95 | 567.8 |
| Standard
deviation | 59.23721381
(+2.52%) | 66.45720427 |
| Standard error | 19.907 |
| 95% CI |
-45.4492-35.1492 |
| T-test | -0.259 |
| P-value | 0.8 |
 | Table IIComparison between the 3 months
postoperative values of the analyzed parameters for all
patients. |
Table II
Comparison between the 3 months
postoperative values of the analyzed parameters for all
patients.
| Variables | Operated eye | Non-operated
eye |
|---|
| MCD average 3
months postoperative | 2,119.55
(-3.61%) | 2,478.6 |
| Standard
deviation | 587.5921609 | 455.2281186 |
| Standard error | 166.207 |
| 95% CI |
22.5810-695.5190 |
| T-test | 2.16 |
| P-value | 0.04a |
| CV average 3 months
postoperative | 23.5 (-14.08%) | 28.5 |
| Standard
deviation | 5.599107072 | 4.82182538 |
| Standard error | 1.652 |
| 95% CI | -0.3448-6.3448 |
| T-test | 1.816 |
| P-value | 0.07a |
| AVG average 3
months postoperative | 394.6
(-14.04%) | 418 |
| Standard
deviation | 116.9621306 | 125.8046104 |
| Standard error | 38.41 |
| 95% CI |
-54.3575-101.1575 |
| T-test | 0.609 |
| P-value | 0.5 |
| HEX average 3
months postoperative | 62.8 (-7.78%) | 68.65 |
| Standard
deviation | 6.257795139 | 4.901785389 |
| Standard error | 1.777 |
| 95% CI | 2.2517-9.4483 |
| T-test | 3.291 |
| P-value | 0.002a |
| CT average 3 months
postoperative | 582.6 (+4.25%) | 575.85 |
| Standard
deviation | 60.75063786 | 65.25049808 |
| Standard error | 19.935 |
| 95% CI |
-47.068-33.3068 |
| T-test | -0.339 |
| P value | 0.74 |
For the CT parameter, a slight increase was observed
both immediately postoperatively (with 2.52%) (Table I) and after 3 months (with 4.25 %)
(Table II).
Postoperatively, a statistically significant
decrease in the parameters MCD (P=0.04) and HEX (P=0.03) (Table I) was identified. A linear decrease
in the other parameters (CV, AVG) was evident, but these were
statistically insignificant (Table
I).
After 3 months postoperatively, a statistically
significant decrease was observed at the following analyzed
parameters: MCD (P=0.04), HEX (P=0.002) (Table II). The remaining parameters also
had a linear decrease (AVG, CV), but were statistically
insignificant. Furthermore, after 3 months postoperatively, the CT
parameter had a slight increase (Table
II).
Comparison of values of the analyzed
parameters depending on the lens
Prior to retinal detachment surgery, pseudophakic
patients had a greater decrease in MCD, AVG, CV, HEX parameters
(Table III, Table IV, Table V, Table
VI and Table VII) in
comparison with those who had their own lens and underwent the same
surgery for retinal detachment. The decrease was observed both
immediately postoperatively and after 3 months postoperatively, but
this decrease was statistically insignificant. In all patients, the
presence of a slight constant postoperative inflammation and
increased intraocular pressure immediately postoperatively was
observed.
 | Table IIIComparison between the values of the
analyzed parameters, depending on the type of lens. |
Table III
Comparison between the values of the
analyzed parameters, depending on the type of lens.
| | Non-operated
eye | Operated eye |
|---|
| Variable | Phakic | PFK-CP | Phakic | PFK-CP |
|---|
| MCD average
postoperative | 2,309.33 | 1,965.87 | 2,517.83 | 2,537.2 |
| Standard
deviation | 494.86 | 599.77 | 515.21 | 382.27 |
| Standard error | 245.61 | 213.62 |
| 95% CI | -844.14
to-246.48 | -394.34 to
-480.25 |
| T-test | -1.39 | 0.09 |
| P-value | 0.18 | 0.93 |
| MCD average 3
months postoperative | 2,239.08 | 1,940.25 | 2,461.41 | 2,504.37 |
| Standard
deviation | 554.69 | 589.96 | 498.87 | 379.02 |
| Standard error | 259.56 | 208.14 |
| 95% CI | -844.14 to
-246.48 | -394.34 to
-480.25 |
| T-test | -1.15 | 0.21 |
| P-value | 0.26 | 0.84 |
 | Table IVComparison between the values of the
analyzed parameters, depending on the type of lens. |
Table IV
Comparison between the values of the
analyzed parameters, depending on the type of lens.
| | Non-operated
eye | Operated eye |
|---|
| Variables | Phakic | PFK-CP | Phakic | PFK-CP |
|---|
| CV average
postoperative | 27.41 | 22.12 | 28.5 | 27.75 |
| Standard
deviation | 6.31 | 4.39 | 5.61 | 3.34 |
| Standard error | 2.57 | 2.21 |
| 95% CI | -10.71 to
-0.12 | -5.40 to -3.90 |
| T-test | -2.05 | -0.33 |
| P-value | 0.05a | 0.74 |
| CV average 3 months
postoperative | 24.25 | 22.37 | 28.83 | 28 |
| Standard
deviation | 6.64 | 3.15 | 5.01 | 4.47 |
| Standard error | 2.53 | 2.19 |
| 95% CI | -7.2 to-3.45 | -5.44 to-3.77 |
| T-test | -0.73 | -0.38 |
| P-value | 0.47 | 0.71 |
 | Table VComparison between the values of the
analyzed parameters, depending on the type of lens. |
Table V
Comparison between the values of the
analyzed parameters, depending on the type of lens.
| | Non-operated
eye | Operated eye |
|---|
| Variables | Phakic | PFK-CP | Phakic | PFK-CP |
|---|
| AVG average
postoperative | 414.16 | 388.12 | 428 | 403.75 |
| Standard
deviation | 142.68 | 64.85 | 150.86 | 71.1 |
| Standard error | 54.15 | 57.5 |
| 95% CI | -139.81 to
-87.73 | -145.07 to
-96.57 |
| T-test | 0.48 | -0.42 |
| P-value | 0.60 | 0.67 |
| AVG average 3
months postoperative | 401.08 | 384.87 | 428.75 | 401.87 |
| Standard
deviation | 141.8 | 62.28 | 150.44 | 71.99 |
| Standard error | 53.61 | 57.45 |
| 95% CI | -128.84 to
-96.43 | -147.59 to
-93.84 |
| T-test | -0.3 | -0.46 |
| P-value | 0.76 | 0.64 |
 | Table VIComparison between the values of the
analyzed parameters (HEX), depending on the type of lens. |
Table VI
Comparison between the values of the
analyzed parameters (HEX), depending on the type of lens.
| | Non-operated
eye | Operated eye |
|---|
| Variables | Phakic | PFK-CP | Phakic | PFK-CP |
|---|
| HEX average
postoperative | 66.25 | 63.75 | 69.67 | 68.37 |
| Standard
deviation | 4.88 | 7.27 | 3.19 | 5.81 |
| Standard error | 2.70 | 2.01 |
| 95% CI | -8.18 to -3.18 | -5.51 to -2.93 |
| T-test | 0.92 | -0.64 |
| P-value | 0.36 | 0.52 |
| HEX average 3
months postoperative | 63.75 | 61.37 | 65.58 | 67.25 |
| Standard
deviation | 3.58 | 8.67 | 3.09 | 6.51 |
| Standard error | 2.78 | 2.15 |
| 95% CI | -8.21 to -3.46 | -6.86 to -2.2 |
| T-test | -0.85 | -1.08 |
| P-value | 0.4 | 0.29 |
 | Table VIIComparison between the values of the
analyzed parameters (CT), depending on the type of lens. |
Table VII
Comparison between the values of the
analyzed parameters (CT), depending on the type of lens.
| | Non-operated
eye | Operated eye |
|---|
| Variables | Phakic | PFK-CP | Phakic | PFK-CP |
|---|
| CT average
postoperative | 578.41 | 564.75 | 571.91 | 561.62 |
| Standard
deviation | 45.59 | 74.44 | 46.8 | 87.69 |
| Standard error | 26.71 | 30.03 |
| 95% CI | -69.79 to
-42.45 | -73.39 to
-52.81 |
| T-test | -0.51 | -0.34 |
| P value | 0.61 | 0.73 |
| CT average 3 months
postoperative | 587.91 | 574.62 | 579.66 | 570.12 |
| Standard
deviation | 44.21 | 78.67 | 47.94 | 84.51 |
| Standard error | 27.39 | 29.51 |
| 95% CI | -70.83 to
-44.25 | -71.55 to
-52.47 |
| T-test | -0.48 | -0.32 |
| P-value | 0.63 | 0.75 |
Discussion
The direct effect of silicone oil on the corneal
endothelium in direct touch (39-41)
has been studied before, but there are very few studies showing the
effect of silicone oil in the vitreous cavity of phakic and
pseudophakic eyes on endothelium. Consequently, in the present
study, the changes that may occur in the corneal endothelium
following retinal detachment surgery adjusted with silicone oil in
phakic or pseudophakic patients were examined.
In the present study, we found a significant loss of
endothelial cells, as demonstrated by the decrease in MCD, CV, AVG
and HEX parameters. During the follow-up period, there were no
significant complications caused by the use of silicone oil, except
for a slight ocular inflammation, present almost constantly in all
operated patients.
In 2014, Goezinne et al (42) who studied five groups of patients
showed that the highest loss in MCD at postoperative 12 months was
observed in aphakic eyes (39.2%), followed by pseudophakic eyes
(19.2%) that underwent cataract surgery during the follow-up
period. The eyes that were pseudophakic at the beginning of the
study showed an MCD loss of 4.6%. In any case, phakic eyes showed
no significant difference. The silicone oil tamponade eyes in the
present study included both phakic and pseudophakic eyes, in which
a statistically significant reduction (3.61%) in MCD at 3 months
postoperatively was found, compared with baseline.
In 2017, Shaheer et al (43) who studied two groups of patients
reported that MCD was decreased in both the groups showing a cell
loss of 30.48±25.78 in phakic patients group and 77.52±40.03 in
pseudophakic patients group, but the decrease in the endothelial
cell count was statistically insignificant. Findings of the present
study demonstrate statistically significant reduction on MCD both
in the phakic and pseudophakic groups.
Silicone oils are powerful tools when used wisely
and within the limits of their use. These are often recommended in
cases of severe detachment of the retina in patients at high risk
of experiencing intraoperative complications. Regular monitoring of
these patients is therefore essential, especially when prolonged
tamponade is required.
In the present study, we have found a linear
decrease in all parameters followed (MCD, AVG, CV, HEX), both
immediately postoperatively and after 3 months postoperatively.
The decrease was not statistically significant at
all. At MCD, it was statistically significant both immediately
postoperatively (P=0.04) and after 3 months postoperatively
(P=0.04). For HEX, we also observed a statistically significant
decrease immediately postoperatively (P=0.03), and a statistically
significant high after 3 months (P=0.002). There was also a greater
decrease in patients previously operated on for cataracts; thus,
the irido-crystalline diaphragm provides protection against the
decrease in the number of endothelial cells during retinal
detachment surgery (44).
The study has some limitations. First of all, the
low number of patients on whom it was performed. In addition, the
duration of the surgery was not measured, which also contributes to
the decrease in the number of endothelial cells. Another limitation
is the low number of pseudophakic patients included in the study.
In conclusion, posterior vitrectomy with internal silicone oil
tamponade causes a decrease in the number of endothelial cells.
Other factors, such as fluid turbulence, phototoxicity, changes in
temperature and pH can also affect the corneal endothelium
(45). Further studies are needed
to demonstrate potential side effects on the anterior ocular
segment of interventions in the posterior ocular segment.
Acknowledgements
Professional editing, linguistic and technical
assistance performed by Irina Radu, Individual Service Provider,
certified translator in Medicine and Pharmacy (certificate
credentials: Series E no. 0048).
Funding
Funding: No funding was received.
Availability of data and materials
All data and materials supporting the results of the
present study are available in the published article.
Authors' contributions
CCC and OM conceived and designed the study and were
responsible for the interpretation and acquisition of the data.
CCC, OM and SN assessed the authenticity of all data. SN and OM
provided scientific advice. SIP, HF, CR were involved in the design
of the study, analysis of the data, and revised the manuscript. DM,
SS, SN, OLK were also involved in the conception and drafting of
the study and revised the manuscript. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Local Ethics
Committee of ‘Dr. Carol Davila’ Central University Military
Emergency Universal Hospital, Bucharest (no. 401) and was conducted
in accordance with the Declaration of Helsinki and with the
International Standard of Good Clinical Practice (ICH-GCP E6 Step
4). All subjects expressed their informed consent in writing.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Authors' information
Dr Corina Cristina Coman (Cernat) is a PhD student
at the Department of Ophthalmology of ‘Victor Babes’ University of
Medicine and Pharmacy in Timisoara, Romania.
References
|
1
|
Lucke KH, Forester MH and Laqua H:
Long-term results of vitrectomy and silicone oil in 500 cases of
complicated retinal detachments. Am J Ophthalmol. 104:624–633.
1987.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Sell CH, McCuen BW II, Landers MB III and
Machemer R: Long-term results of successful vitrectomy with
silicone oil for advanced proliferative vitreoretinopathy. Am J
Ophthalmol. 103:24–28. 1987.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Azen SP, Scott IU, Flynn HW Jr, Lai MY,
Topping TM, Benati L, Trask DK and Rogus LA: Silicone oil in the
repair of complex retinal detachments. A prospective observational
multicentric study. Opthalmology. 105:1587–1597. 1998.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Zivojnović R: Silicone oil in
vitreoretinal surgery. Springer Netherlands, 1987.
doi:10.1007/978-94-009-3321-7.
|
|
5
|
Stone W Jr: Alloplasty in surgery of the
eye. N Engl J Med. 258:486–490. 1958.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Cibis PA, Becker B, Okun E and Canaan S:
The use of liquid silicone in retinal detachment surgery. Arch
Ophthalmol. 68:590–599. 1962.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ryan JS: Silicone oils: Physicochemical
properties. In: Retina. vol. 3, Elsevier Mosby, 4th edition,
pp2191-2210, 2006.
|
|
8
|
Vitrectomy with silicone oil or sulfur
hexafluoride gas in eyes with severe vitreoretinopathy: Results of
a randomized clinical trial. Silicone study report 1. Arch
Ophthalmol. 110:770–779. 1992.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Vitrectomy with silicone oil or
perfluoropropane gas in eyes with severe proliferative
vitreoretinopathy: Results of a randomized clinical trial. Silicone
study report 2. Arch Ophthalmol. 110:780–792. 1992.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Foster WJ: Vitreous substitutes. Expert
Rev Ophthalmol. 3:211–218. 2008.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Nadal J, Verdaguer P and Canut MI:
Treatment of retinal detachment secondary to macular hole in high
myopia: Vitrectomy with dissection of the inner limiting membrane
to the edge of the staphyloma and long-term tamponade. Retina.
32:1525–1530. 2012.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Wei Y, Li Y and Chen F: Vitrectomy
treatment of retinal detachments related to choroidal coloboma
involving the disk. Retina. 34:1091–1095. 2014.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Unlü N, Kocaoğlan H, Acar MA, Sargin M,
Aslan BS and Duman S: Outcome of complex retinal detachment surgery
after silicone oil removal. Int Ophthalmol. 25:33–36.
2004.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kapur R, Birnbaum AD, Goldstein DA,
Tessler HH, Shapiro MJ, Ulanski LJ and Blair MP: Treating
uveitis-associated hypotony with pars plana vitrectomy and silicone
oil injection. Retina. 30:140–145. 2010.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Wilkinson C: Interventions for
asymptomatic retinal breaks and lattice degeneration for preventing
retinal detachment. Cochrane Database Syst Rev.
(CD003170)2001.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Saw SM, Gazzard G, Wagle AM, Lim J and Au
Eong KG: An evidence-based analysis of surgical interventions for
uncomplicated rhegmatogenous retinal detachment. Acta Ophthalmol
Scand. 84:606–612. 2006.PubMed/NCBI View Article : Google Scholar
|
|
17
|
García-Arumí J, Martínez-Castillo V,
Boixadera A, Blasco H, Marticorena J, Zapata MÁ, Macià C, Badal J,
Distéfano L, Rafart JM, et al: Rhegmatogenous retinal detachment
treatment guidelines. Arch Soc Esp Oftalmol. 88:11–35.
2013.PubMed/NCBI View Article : Google Scholar : (In English,
Spanish).
|
|
18
|
Ryan SJ: Retina @a ed., vol III. CD ROM,
Mosby, USA. 2004:653–670. 2004.
|
|
19
|
Polkinghorne PJ and Craig JP: Northern New
Zealand rhegmatogenous retinal detachment study: Epidemiology and
risk factors. Clin Exp Ophthalmol. 32:159–163. 2004.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wong TY, Tielsch JM and Schein OD: Racial
difference in the incidence of retinal detachment in Singapore.
Arch Ophthalmol. 117:379–383. 1999.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Peters AL: Retinal detachment in black
South Africans. S Afr Med J. 85:158–159. 1995.PubMed/NCBI
|
|
22
|
Preda MA, Popa G, Karancsi OL, Musat O,
Popescu SI, Munteanu M and Popa Z: Effectiveness of subconjunctival
bevacizumab associated with a laser-based procedure in the
treatment of neovascular glaucoma. Farmacia. 66:621–626. 2018.
|
|
23
|
Boruga O, Bălăşoiu AT, Giuri S, Munteanu
M, Stanca HT, Iovanescu G and Preda MA: Caruncular late-onset
junctional nevus: Apropos of an anatomo-clinical observation. Rom J
Morphol Embryol. 58:1461–1464. 2017.PubMed/NCBI
|
|
24
|
Balica NC, Poenaru M, Preda MA, Boia RE,
Burlacu ON, Horhat ID, Mogoanță CA, Vlăescu AN, Baderca F, Jifcu EM
and Sarău CA: Primary tonsillar tuberculosis-case report. Rom J
Morphol Embryol. 60:267–271. 2019.PubMed/NCBI
|
|
25
|
Stanca HT, Munteanu M, Jianu DC, Motoc
AGM, Jecan CR, Tăbăcaru B, Stanca S and Preda MA: Femtosecond-LASIK
outcomes using the VisuMax®-MEL® 80 platform
for mixed astigmatism refractive surgery. Rom J Morphol Embryol.
59:277–283. 2018.PubMed/NCBI
|
|
26
|
Stanca HT, Suvac E, Munteanu M, Jianu DC,
Motoc AGM, Roşca GC and Boruga O: Giant cell arteritis with
arteritic anterior ischemic optic neuropathy. Rom J Morphol
Embryol. 58:281–285. 2017.PubMed/NCBI
|
|
27
|
Preda MA, Karancsi OL, Munteanu M and
Stanca HT: Clinical outcomes of micropulse transscleral
cyclophotocoagulation in refractory glaucoma-18 months follow-up.
Lasers Med Sci. 35:1487–1491. 2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Stanca HT, Munteanu M, Jianu DC, Motoc
AGM, Tăbăcaru B, Stanca S, Ungureanu E, Boruga VM and Preda MA: New
perspectives in the use of laser diode transscleral
cyclophotocoagulation. A prospective single center observational
cohort study. Rom J Morphol Embryol. 59:869–887. 2018.PubMed/NCBI
|
|
29
|
Balica NC, Poenaru M, Doroş CI, Baderca F,
Preda MA, Iovan VC, Stanca HT, Busuioc CJ, Oprişcan IC and Boruga
O: The management of the oropharyngeal anterior wall cancer. Rom J
Morphol Embryol. 59:113–119. 2018.PubMed/NCBI
|
|
30
|
Duan A, She H and Qi Y: Complications
after heavy silicone oil tamponade in complicated retinal
detachment. Retina. 31:547–552. 2011.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Han DP, Lewis H, Lambrou FH Jr, Mieler WF
and Hartz A: Mechanisms of intraocular pressure elevation after
pars plana vitrectomy. Ophthalmology. 96:1357–1362. 1989.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Muether PS, Hoerster R, Kirchhof B and
Fauser S: Course of intraocular pressure after vitreoretinal
surgery: Is early postoperative intraocular pressure elevation
predictable? Retina. 31:1545–1552. 2011.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Barać J, Katusić D, Ivancić D, Sisljagić V
and Bradvica M: Effect of intraocular silicone oil on ocular
tissue. Coll Antropol. 29 (Suppl 1):S51–S54. 2005.PubMed/NCBI
|
|
34
|
Kleinberg TT, Tzekov RT, Stein L, Ravi N
and Kaushal S: Vitreous substitutes: A comprehensive review. Surv
Ophthalmol. 56:300–323. 2011.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Caramoy A, Kearns VR, Chan YK, Hagedorn N,
Poole RJ, Wong D, Fauser S, Kugler W, Kirchhof B and Williams RL:
Development of emulsification resistant heavier-than-water
tamponades using high molecular weight silicone oil polymers. J
Biomater Appl. 30:212–220. 2015.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Light DJ: Silicone oil emulsification in
the anterior chamber after vitreoretinal surgery. Optometry.
77:446–449. 2006.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Bennett SR and Abrams GW: Band keratopathy
from emulsified silicone oil. Arch Ophthalmol.
108(1387)1990.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Azuara-Blanco A, Dua HS and Pillai CT:
Pseudo-endothelial dystrophy associated with emulsified silicone
oil. Cornea. 18:493–494. 1999.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Kertes PJ and Peyman GA: Complications of
silicone oil use. In: Vitreoretinal Surgical Techniques. Peyman GA,
Meffert SA, Conway MD and Chou F (eds). Dunitz, London, pp200-203,
2006.
|
|
40
|
Sternberg P Jr, Hatchell DL, Foulks GN and
Landers MB III: The effect of silicone oil on the cornea. Arch
Ophthalmol. 103:90–94. 1985.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Pang MP, Peyman GA and Kao GW: Early
anterior segment complications after silicone oil injection. Can J
Ophthalmol. 21:271–275. 1986.PubMed/NCBI
|
|
42
|
Goezinne F, Nuijts RM, Liem AT, Lundqvist
IJ, Berendschot TJ, Cals DW, Hendrikse F and La Heij EC: Corneal
endothelial cell density after vitrectomy with silicone oil for
complex retinal detachments. Retina. 34:228–236. 2014.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Shaheer M, Khan AA, Ahmed N, Mahju TM and
Rasheed U: Corneal endothelial cell loss after vitrectomy with
silicone oil tamponade in phakic versus pseudophakic patients with
rhegmatogenous retinal detachment. Pak J Ophthalmol. 33:137–141.
2017.
|
|
44
|
Goyal JI, Panda A and Angra SK: Corneal
endothelial changes following pars plana lensectomy. Indian J
Ophthalmol. 39:25–27. 1991.PubMed/NCBI
|
|
45
|
Kwon JW, Cho KJ, Kim HK, Lee JK, Gore PK,
McCartney MD and Chuck RS: Analyses of factors affecting
endothelial cell density in an eye bank corneal donor database.
Cornea. 35:1206–1210. 2016.PubMed/NCBI View Article : Google Scholar
|