Introduction
The inferior vena cava (IVC) is the largest single
vein in the human body, and is responsible for collecting venous
blood from the abdomen, pelvic organs and lower extremities
(1). Because of the complexity of
its development during the embryonic stage, IVC can have a variety
of anatomical variations in adulthood (2,3).
Double IVC is a relatively rare congenital malformation, with a
reported incidence of 0.2-3% worldwide (4). Although congenital double IVC is
asymptomatic in the majority of cases and it is occasionally found
during imaging examination, intraoperative examination or autopsy,
this venous malformation may have important implications during
surgery and for interventional radiotherapy (1,5-26).
Aljabri et al (27)
reported that fatal and uncontrollable bleeding occurred in 10% of
the patients when IVC anomalies were not identified preoperatively.
The presence of double IVC can complicate surgery for aortic
aneurysm (28). It is important
for urologists to evaluate whether the kidney donor has double IVC
during the procedure of kidney harvesting, which can prevent
vascular injury and complications (29). In addition, patients with double
IVC have a high tendency for thromboembolic events (6). The IVC malformations are associated
with 5% of deep vein thrombosis cases due to slow blood flow
(30). It is crucial to confirm
whether double IVC is present for patients requiring the placement
of an IVC filter, and venography should be performed to rule out
vascular variation for patient with planned IVC filter placement
(31). If double IVC is found, the
filter should be implanted in both IVCs respectively or a common
IVC which is formed by the confluence of the left IVC (LIVC) and
right IVC (RIVC), and failure to do so maybe lead to the pulmonary
embolism (32). To the best of the
authors' knowledge, coexistence of a retroperitoneal tumor with
double IVC is rarely reported. In the present report, a case of a
retroperitoneal lymphoma with double IVC is documented, following
which its embryological, clinical and radiological significance is
discussed.
Case report
A 52-year-old male patient of Chinese ethnicity
visited the Urology Department of Yichang Central People's Hospital
with a retroperitoneal tumor in March 2022, which was discovered
unexpectedly during a routine health screen by abdominal
ultrasound. The patient was asymptomatic and previously healthy.
The patient was assessed using an abdominal computed tomography
(CT) for further diagnosis, which revealed a retroperitoneal
neoplastic space-occupying lesion measuring 116x83 mm. Furthermore,
CT urography was performed using 64-slice spiral CT. The diagnosis
was as follows: Right retroperitoneal neoplasm surrounding the
right renal artery and vein, abdominal aorta (AA) and RIVC, unclear
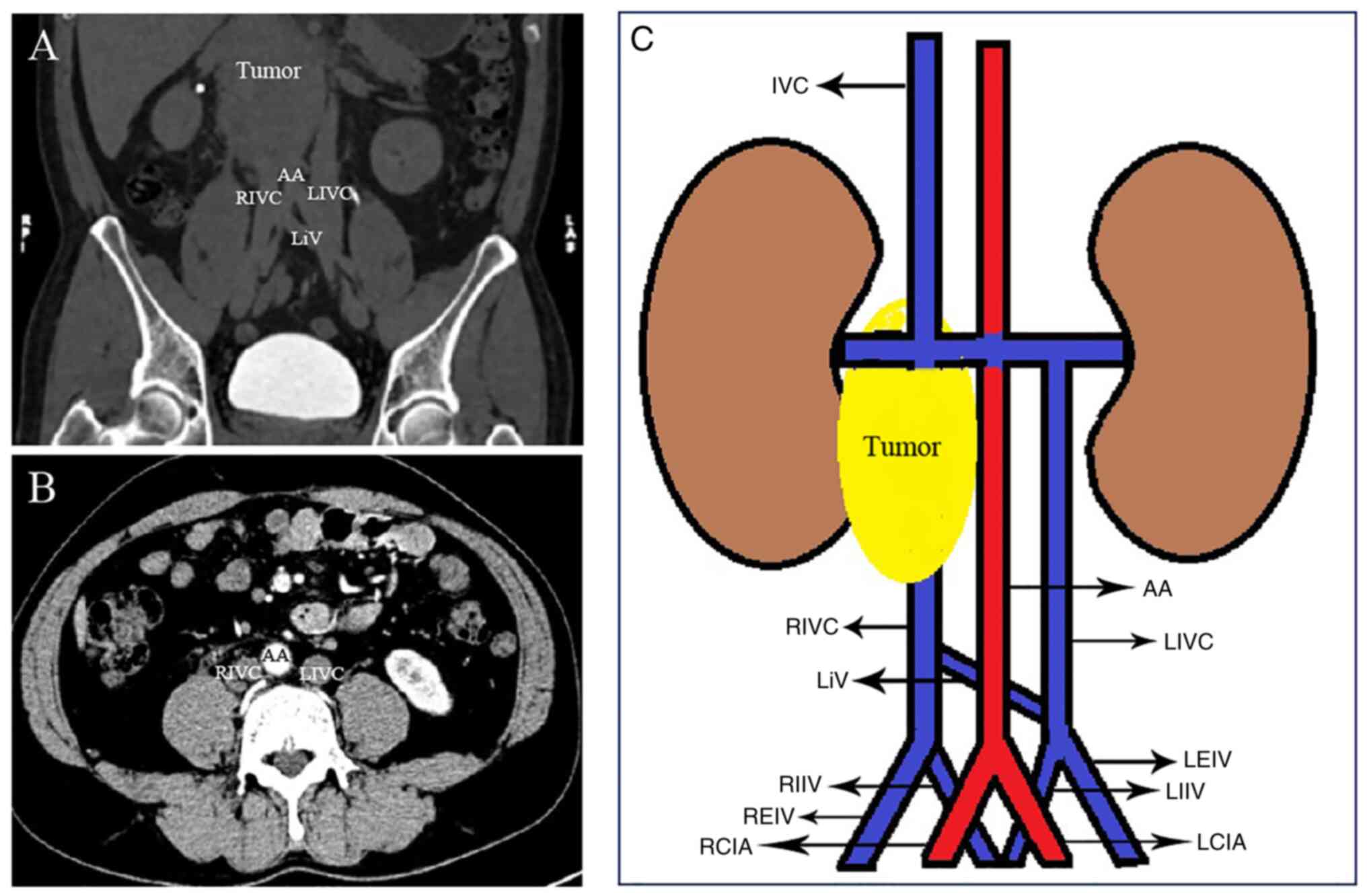
boundary with the psoas muscle and double IVC (Fig. 1A and C). CT data were collected in the
non-enhancement phase, arterial phase and venous phase. The data
were then imported into the three-dimensional (3D) reconstruction
software (3D visualization image processing software for medical
diagnosis, version number: DX3D/V1.4.0. Anhui King Star Digital
S&T Co., Ltd.) to establish a 3D visualization model of the
abdominal organ tissues and the vascular system to study the
overall structure of the double IVC and its relationship with the
retroperitoneal tumor. A percutaneous puncture biopsy of the
retroperitoneal tumor was then performed. The biopsy tissue of the
retroperitoneal tumor was fixed using 10% formalin at 4˚C for 24 h,
rinsed with tap water and dehydrated in an ascending series of
ethanol followed by xylene. The specimens were then infiltrated and
embedded in paraffin, before being affixed to glass slides after
sectioning (5 µm). Finally, the specimens were subjected to heating
at 37˚C for 12 h, and hematoxylin-eosin staining at 30˚C for 5 min
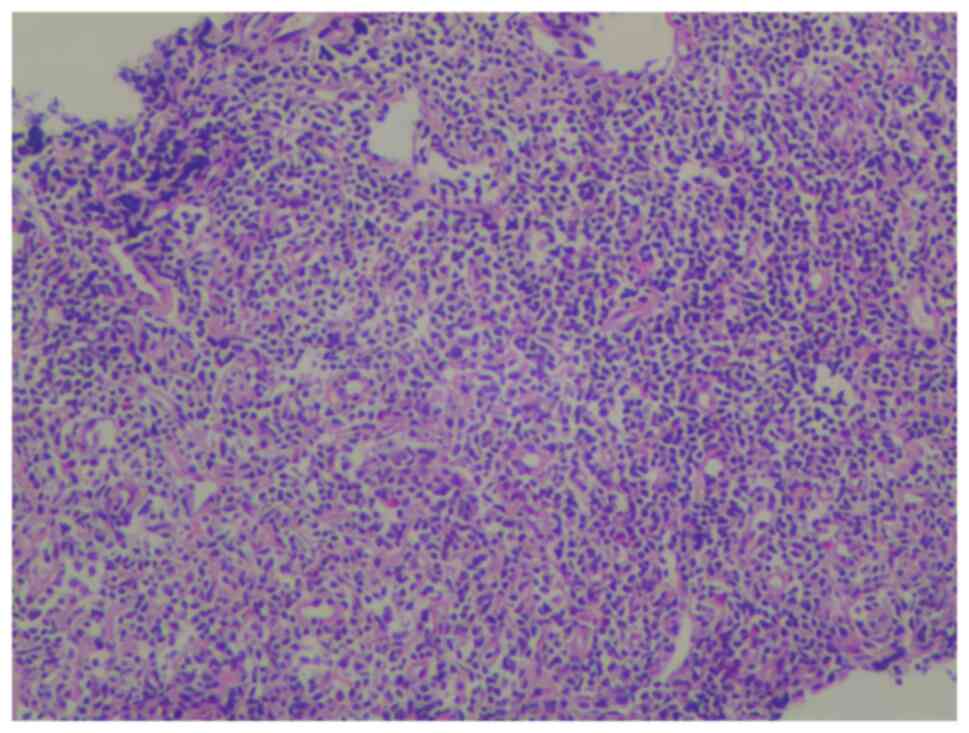
and 3 min respectively. The tumor was then identified to be a
lymphoma using light microscopy. The histopathological images
showed that fibrous connective tissue was infiltrated by numerous
small, round and blue cells (Fig.
2). The patient was transferred to the Hematology Department of
Yichang Central People's Hospital in April 2022 for chemotherapy
according to lymphoma management guidelines (33). He received 4 cycles of ABVD
(doxorubicin, bleomycin, vinblastine, dacarbazine) chemotherapy,
following which the size of the tumor was reduced by 3 cm after
chemotherapy during the patient's 6 months follow-up.
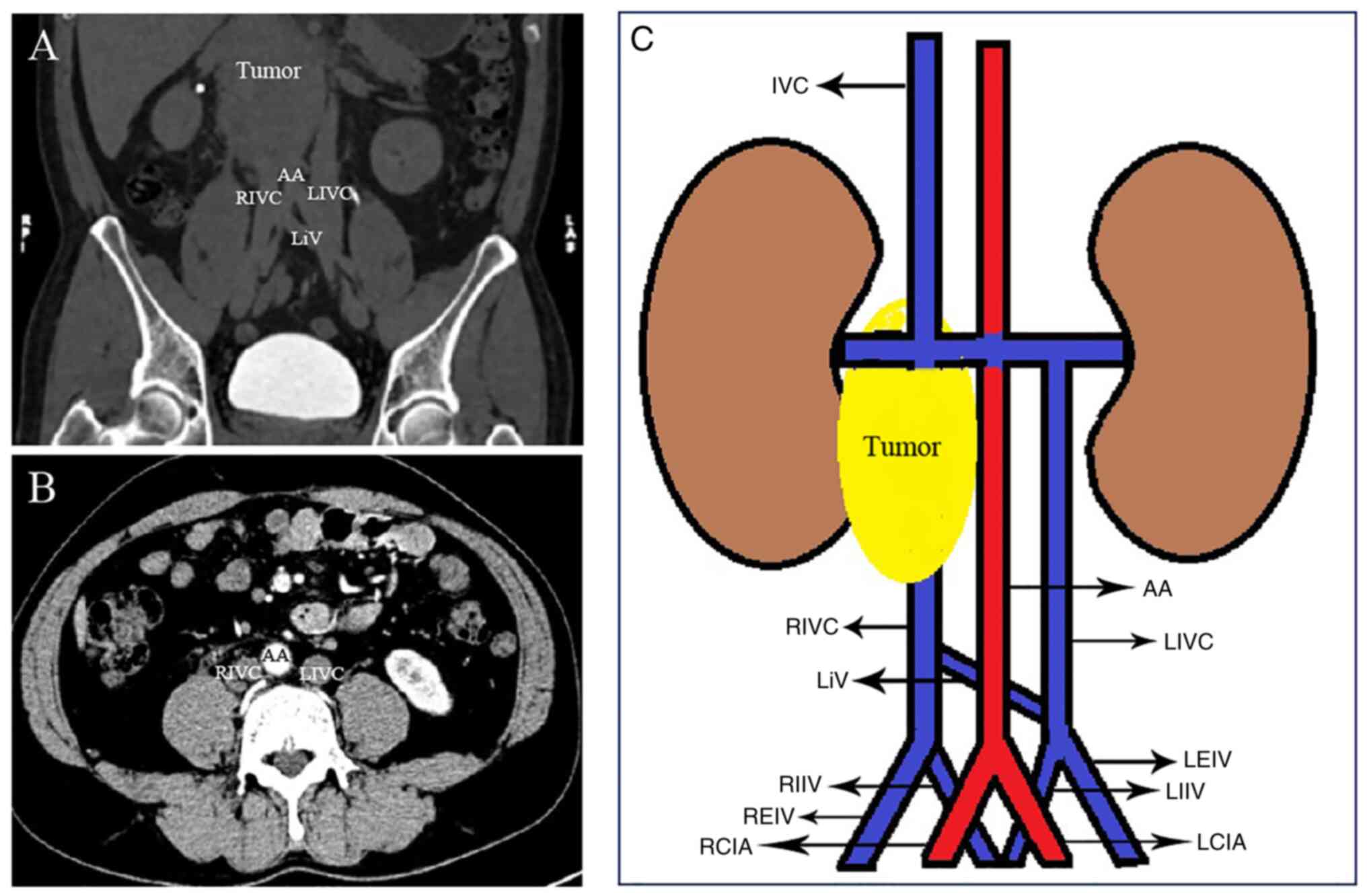 | Figure 1Images of the retroperitoneal lymphoma
and double IVC in a 52-year-old male patient. (A) Coronal CT scan
showing the double IVC and the retroperitoneal tumor. (B) Axial CT
scan showing the double IVC. (C) Schematic showing the double IVC
and the retroperitoneal tumor, with the left IVC ending in the left
renal vein. AA, abdominal aorta; RCIA, right common iliac artery;
LCIA, left common iliac artery; IVC, inferior vena cava; RIVC,
right inferior vena cava; REIV, right external iliac vein; RIIV,
right internal iliac vein; LIVC, left inferior vena cava; LEIV,
left external iliac vein; LIIV, left internal iliac vein; LiV,
interiliac vein. |
Abdominal CT showed two rounded structures on both
sides of the AA, which were considered to be the bilateral IVC
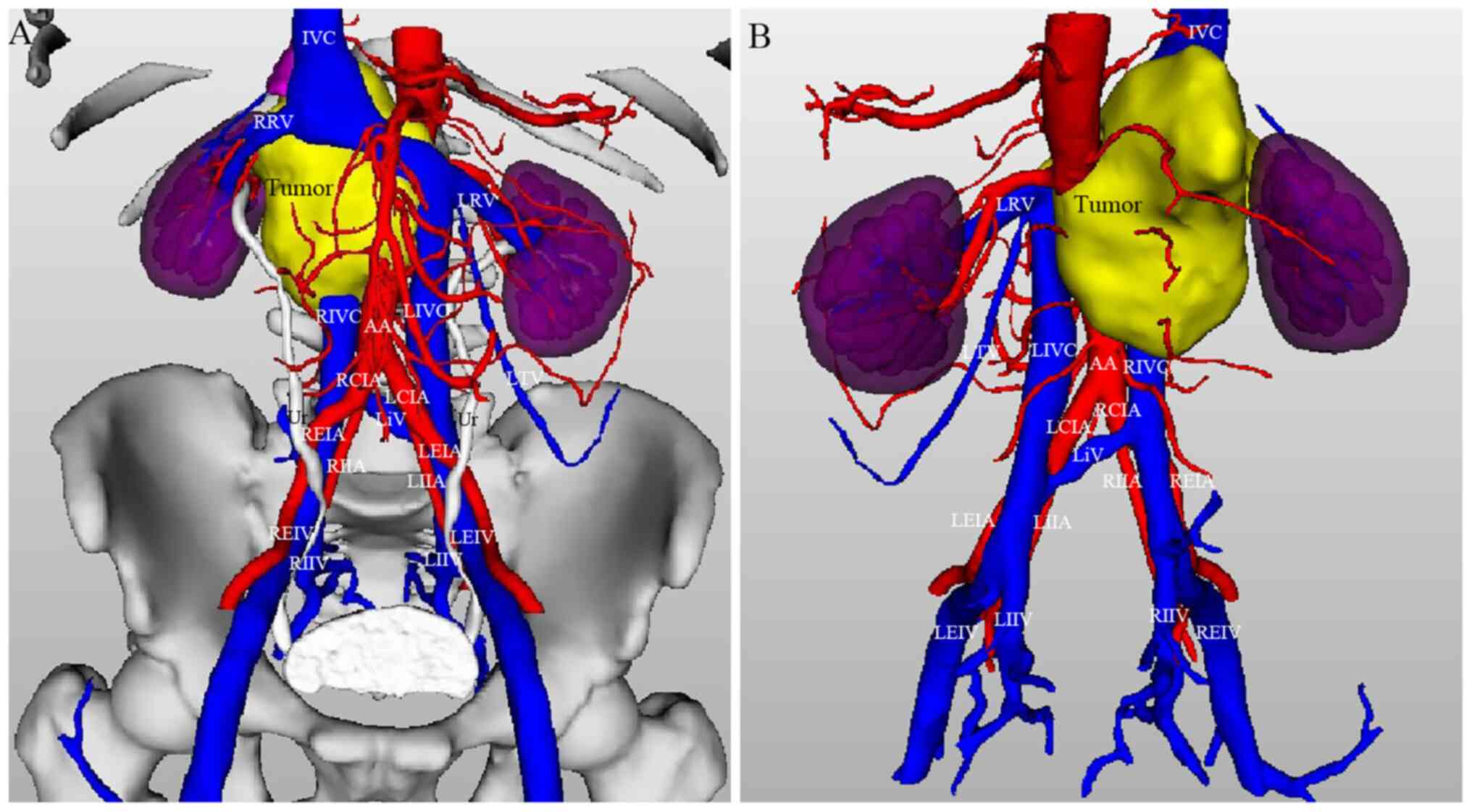
(Fig. 1B). 3D reconstruction
showed the bilateral IVC ascending along either side of the AA,
where the two vessels had a similar diameter. In front of the left
sacroiliac joint, the LIVC appeared to be formed by the confluence
of the left internal iliac vein and the external iliac vein. Behind
the left common iliac artery, the LIVC rose along the left-side AA
to the level of the second lumbar vertebra, ending at the left
renal vein (LRV), which crossed anteriorly to the aorta in a normal
manner to join the RIVC at an angle of 61˚ (Fig. 3A). The lengths of the LIVC and LRV
were 127.8 and 76.7 mm, respectively, whereas the length of the LRV
that crosses anteriorly to the aorta was 43.4 mm. The initial
caliber of the LRV and left testicular vein was 9.6 and 2.8 mm,
respectively, where the blood flows into the LRV (Fig. 3). In front of the right sacroiliac
joint, the RIVC was formed by the confluence of the right internal
iliac vein and external iliac vein. Behind the right common iliac
artery, the RIVC rose along the right side of the AA and joined the
LRV to form a common IVC. The right renal vein had a length of 46.9
mm and a caliber of 5.6 mm, which flowed into the common IVC. The
length of the RIVC was 142.7 mm, whereas the calibers of the LIVC
and RIVC were 14.6 and 14.0 mm, respectively. The caliber of the
common IVC was 18.6 mm (Fig. 3A).
The retroperitoneal tumor was 116.8x83.9x50.3 mm in size, which
tightly enveloped and compressed the RIVC, AA and right renal
artery, in addition to pressing the right psoas muscle and
bilateral renal veins and the RIVC wrapped (where the tumor was
compressing the IVC) was 66.2 mm in length. From the beginning of
the common IVC to the level of the RIVC at the right kidney lower
pole, no blood supply could be found in the IVC of the wrapped
segment. The interiliac vein connecting the LIVC and RIVC had a
length of 37.8 mm and a caliber of 6.4 mm. The interiliac vein was
located in front of the left sacroiliac joint, crossed posterior to
the right common iliac artery, oblique from the lower left to the
upper right and joined the RIVC in front of the fifth lumbar
vertebra (Fig. 3). According to
the classification method of IVC proposed by Chen et al
(8), the present case involved a
double IVC with interiliac vein, which was type 2b from the
LIVC.
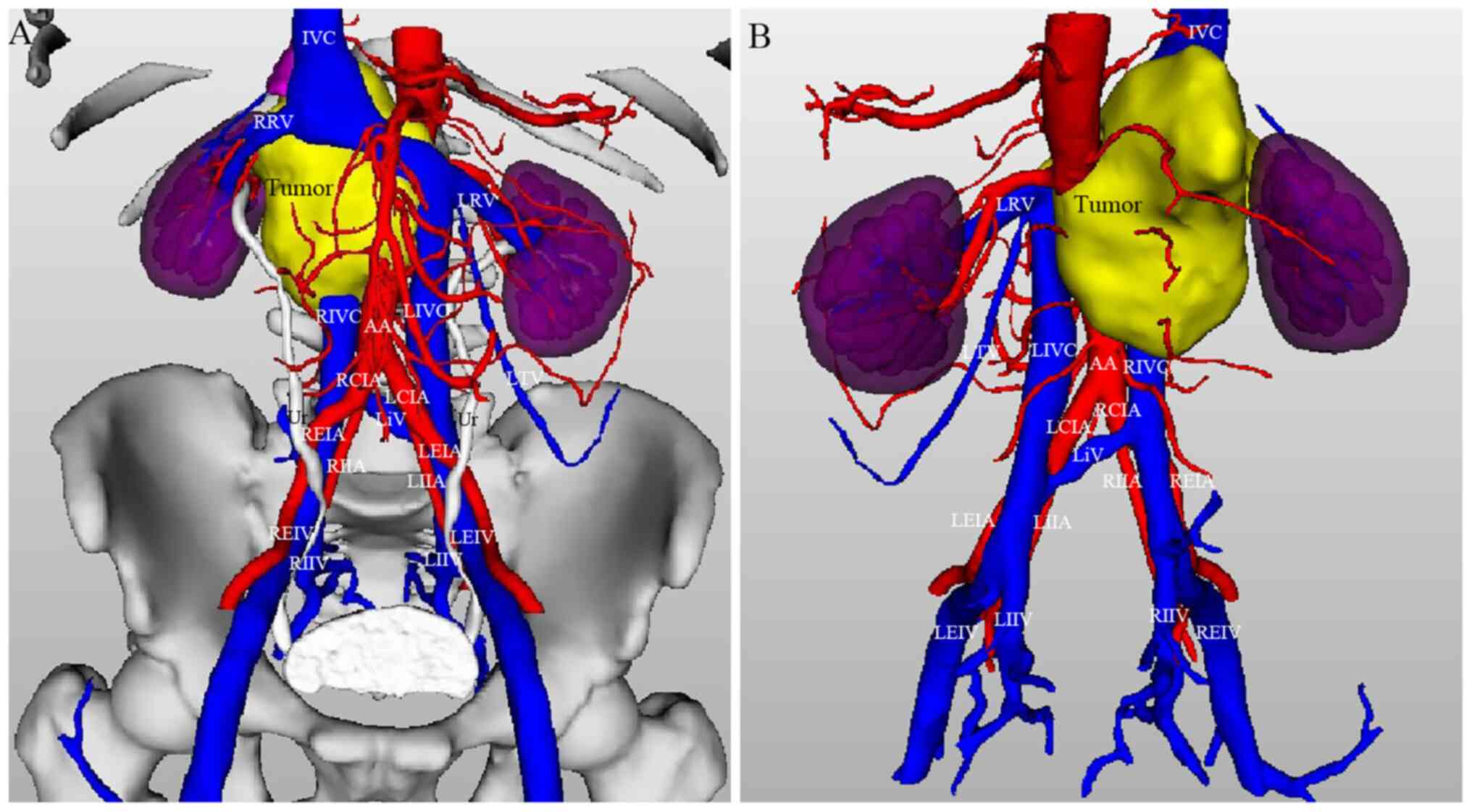 | Figure 3Three-dimensional reconstruction model
of the double inferior vena cava and the retroperitoneal tumor
based on CT data. (A) Front view. (B) Posterior view. AA, abdominal
aorta; RCIA, right common iliac artery; REIA, right external iliac
artery; RIIA, right internal iliac artery; LCIA, left common iliac
artery; LEIA, left external iliac artery; LIIA, left internal iliac
artery; IVC, inferior vena cava; RIVC, right inferior vena cava;
REIV, right external iliac vein; RIIV, right internal iliac vein;
LIVC, left inferior vena cava; LEIV, left external iliac vein;
LIIV, left internal iliac vein; LiV, interiliac vein; RRV, right
renal vein; LRV, left renal vein; LTV, left testicular vein; Ur,
ureter. |
In the present study, the 3D visualization model was
used as a novel diagnostic method. Compared with the 2D CT images,
the 3D visualization model provided a stereoscopic and additional
detail to the anatomical hierarchy, which was more appropriate
compared with that 2D images used in usual clinical practice to
meet the patient's clinical requirements. Therefore, these
diagnostic procedures were approved by The Ethics Committees of
Yichang Central People's Hospital. Written informed consent was
obtained from the patient for the participation in the study and
publication of this case report.
The literature was then searched. The databases used
were https://www.tsgyun.com/official/index.html (wisdom
cloud library) and PubMed. The search terms included inferior vena
cava, double inferior vena cava, retroperitoneal tumor, anatomical
variations, congenital malformation, right inferior vena cava, left
inferior vena cava, interiliac vein, three-dimensional
visualization model and three-dimensional reconstruction. The
inclusion criteria of selecting papers for Table I were double inferior vena cava,
baseline characteristics such as sex, age, department in which
double inferior vena cava was found, double inferior vena cava
diameter, interiliac vein, diagnostic methods, primary symptoms,
population and ethnicity and the number of items ≥7 among the 9
items. The exclusion criteria for selecting papers for Table I were minors (<16 years old),
article size is less than one page and article is too old (over 30
years).
 | Table IA review of double inferior vena cava
cases reported to 2022. |
Table I
A review of double inferior vena cava
cases reported to 2022.
| First author,
year | Sex | Age, years | Department | RIVC and LIVC
caliber, mm | Interiliac vein | Diagnostic
methods | Primary
presentation/Symptoms |
Population/Ethnicity | (Refs.) |
|---|
| Yoshimura et
al, 2022 | Male | 85 | Department of
Anatomy | RIVC, 11; LIVC,
7 | Yes | Dissection | NA | Japan/Asian | (5) |
| Shaheen et al,
2022 | Male | 62 | Department of
Anatomy | RIVC, 16; LIVC,
16 | Yes | Dissection | NA | Saudi
Arabia/Caucasian | (5) |
| Waśniewska et
al, 2020 | Female | 42 | Department of
Radiology and Diagnostic Imaging | RIVC, 15; LIVC,
13 | No | Imaging examination
(ultrasonography, CT angiography) | Abdominal pain | Poland/Caucasian | (6) |
| Klinkhachorn et
al, 2020 | Male | 66 | Department of
Anatomy | RIVC, 16; LIVC,
26 | No | Dissection | NA | USA/Caucasian | (7) |
| Chen et al,
2012 | Female | 84 | Department of
Anatomy | RIVC, 20; LIVC,
9 | Yes | Dissection | NA | Japan/Asian | (8) |
| Matsuoka et
al, 2018 | Female | 53 | Gynecologic
Surgery | NA | No | Imaging examination
(CT) | Advanced ovarian
cancer | Japan/Asian | (9) |
| Matsuoka et
al, 2018 | Female | 51 | Gynecologic
Surgery | NA | Yes | Imaging examination
(CT) | Advanced ovarian
cancer | Japan/Asian | (9) |
| Onoda et al,
2018 | Male | 74 | Cardiovascular
Surgery | NA | No | Imaging examination
(CT) | Abdominal aortic
aneurysm | Japan/Asian | (10) |
| Wang et al,
2014 | Male | 32 | Vascular
Surgery | RIVC, 25; LIVC,
7 | No | Imaging examination
(venogram) | Pain and swelling
of the right lower extremity | China/Asian | (11) |
| Pilichowska et
al, 2020 | Female | 25 | Department of
Transplantation | NA | No | During the organ
procurement procedure | Intracranial
hemorrhage |
Poland/Caucasian | (12) |
| Ito and Ikeda,
2018 | Female | 81 | Department of
Anatomy | RIVC, 15; LIVC,
10 | Yes | Dissection | NA | Japan/Asian | (13) |
| Coco et al,
2016 | Female | 42 | Department of
Radiology | NA | No | Imaging examination
(CT) | Right abdominal
pain |
Italy/Caucasian | (14) |
| Chaijaroonkhanarak
et al, 2017 | Female | 45 | Department of
Anatomy | RIVC, 14; LIVC,
7 | Yes | Dissection | NA | Thailand/Asian | (15) |
| Jiang et al,
2011 | Male | 16 | Department of
Endocrinology | NA | Yes | Imaging examination
(CT, vasography) | Headaches and
dizziness | China/Asian | (16) |
| Nakatani et
al, 2004 | Male | 40 | Department of
Urology | NA | No | Imaging examination
(CT, venography) | NA | Japan/Asian | (17) |
| Nakatani et
al, 2004 | Female | 44 | Department of
Urology | NA | No | Imaging examination
(CT, renal angiography) | NA | Japan/Asian | (17) |
| Kumar et al,
2008 | Female | 62 | Department of
Urology | NA | No | Imaging examination
(CT) | Left flank
pain |
India/Caucasian | (18) |
| Yano et al,
2000 | Male | 70 | Department of
Anatomy | RIVC, 15; LIVC,
13 | Yes | Dissection | NA | Japan/Asian | (19) |
| Yano et al,
2000 | Male | 86 | Department of
Anatomy | RIVC, 15; LIVC,
10 | No | Dissection | NA | Japan/Asian | (19) |
| Fronek et
al, 2006 | Female | 37 | Renal Transplant
Unit | NA | No | Imaging examination
(angiography, CT) | NA | UK/Caucasian | (20) |
| Kumar et al,
2016 | Female | 70 | Cardiac Center | NA | No | Imaging examination
(CT, angiography) examination (CT, angiography) | Dyspnea and chest
pain |
India/Caucasian | (21) |
| Furutani et
al, 2020 | Female | 66 | Gastroenterological
Surgery | NA | Yes | Imaging examination
(CT, angiography) | Rectal cancer and
lung metastasis | Japan/Asian | (22) |
| Habuchi et
al, 1993 | Male | 77 | Department of
Urology | NA | No | Imaging examination
(CT, phlebography) | Asymptomatic gross
hematuria | Japan/Asian | (23) |
| Mao et al,
2015 | Male | 63 | Department of
Urology | RIVC, NA; LIVC,
13 | No | Intraoperative
examination | Intermittent gross
hematuria | China/Asian | (24) |
| Yamaguchi et
al, 2021 | Male | 60 | Department of
Urology | NA | No | CT, intraoperative
examination | Left scrotal
enlargement | Japan/Asian | (25) |
| Gomes et al,
2020 | Female | 45 | Department of
Gynecology | NA | Yes | Intraoperative
examination | NA |
Portugal/Caucasian | (26) |
Discussion
Lucas (34)
reported the first case of congenital IVC duplication in 1916. IVC
malformations are rare, with the most common type being double IVC,
occurring mainly due to abnormalities during embryonic development
(25). The venous system
originates from three symmetrically paired veins, namely the
cardinal veins, umbilical veins and vitelline veins, all of which
are formed during weeks 1-4 of embryonic development (26). In addition, the IVC develops from
four of the following different embryonic sources: The posterior
cardinal vein, right subcardinal vein, right supracardinal vein and
the right vitelline vein (35).
Embryonic development of the IVC is a complex process, involving
the formation, anastomosis, regression and replacement of the major
embryonic veins (24). The normal
IVC consists of the following four parts: Hepatic, renal,
suprarenal and infrarenal segments. The hepatic segment was
considered to be derived from the vitelline vein (36). By contrast, the suprarenal and
infrarenal segments are developed from the right subcardinal vein
and right supracardinal vein, respectively (35). The renal segment originates from
the right suprasubcardinal anastomosis (36). Left supracardinal vein regression
disappears during embryonic development, whereas the right
supracardinal vein is retained and develops to form a unilateral
right normal infrarenal segment of the IVC (37). Double IVC is caused by the
persistence of the bilateral supracardinal veins (37,38).
Our case was a type 2b from the LIVC, and the
incidence of type 2b in abnormal IVC has been reported to be 38.5%,
where IVC with iliac vein accounts for 67.9% of the total number of
cases of IVC abnormalities (8).
The majority of cases of duplicated IVC are
asymptomatic (Table I), the
diagnosis of which is typically made with CT angiography or MRI. In
addition, venography may be used to identify this abnormality.
However, there are certain limitations in CT examination. Sousa
Gomes et al (26)
previously reported that a double IVC was found during
gynecological surgery, but preoperative CT failed to diagnose this
anomaly. In addition, a number of studies have shown that the
incidence of double IVC reported based on CT is 0.3-1%, because one
of the double IVC may be too narrow, below the scope of detection
to be detected with CT (36). It
may sometimes be difficult to use CT to distinguish between venous
anomalies and lymphadenopathy, where the two circular structures,
one on each side of the aorta, may be misinterpreted as
retroperitoneal lymphadenopathy (39). Therefore, in the present report,
based on the patient's CT data, a 3D model was reconstructed using
3D visualization software, which enabled multistage fusion
visualization of the retroperitoneal tumor, blood vessels and organ
tissues. Previous reports on double IVC occasionally use 3D
reconstruction images (14,25).
The present report utilized a 3D reconstruction model of the
retroperitoneal lymphoma with double IVC, which to the best of our
knowledge, has not been reported previously. Compared with
two-dimensional CT images, the 3D reconstruction model can not only
potentially provide an understanding of the anatomical structure of
each organ and tissue more intuitively, but can also accurately
reflect the positional relationship between the double IVC, AA and
tumor by employing freely rotating 3D images.
When a malformation of the IVC is involved in
radiology, interventional therapy or surgery, knowledge of double
IVC and other vascular variants can be used to minimize the risk of
intraoperative bleeding, misdiagnosis or life-threatening
complications (9,11,16,22,26).
A previous study showed that misdiagnosis of a double IVC caused
surgical confusion between the LIVC and the left gonadal vein,
resulting in the severing of the LIVC during radical
nephroureterectomy (24). Because
the left gonadal vein develops from the left subcardinal vein, the
LIVC runs along the medial side of the left gonadal vein, which
increases the risk of misidentification between the left gonadal
vein and LIVC (25). To avoid such
misdiagnosis, operators are advised to probe the distal vein during
the operation to confirm the type of vein.
In addition, since the interiliac vein crosses
anterior to the lumbar and sacral regions, it is of particularly
high importance to avoid severe bleeding caused by injury to the
interiliac vein during anterior lumbar interbody fusion, anterior
sacral and retroperitoneal lymphadenectomy (9,40).
Injury to the interiliac vein has been reported to cause serious
hemorrhage during gynecological oncology surgery (26). There was an interiliac vein in the
present case, where the RIVC was completely blocked by the
retroperitoneal lymphoma. However, the RIVC drained into the LIVC
through shunting of the interiliac vein and the patient did not
develop edema of the right lower limb. Although the patient with
lymphoma did not undergo surgery, they were transferred to the
Hematology Department for chemotherapy. However, for patients who
require surgical treatment, it is important to determine the
surgical approach, scope and plans, and to ensure surgical safety
according to the 3D visualization technology.
The limitation of the present report is that the
patient did not undergo surgical treatment. Therefore, the surgical
plan and precautions formulated according to the 3D reconstruction
model could not be intuitively verified during surgery.
In conclusion, the present report documented a rare
case of a retroperitoneal lymphoma with double IVC. The condition
was accidentally discovered by CT. A 3D visualization model was
established using 3D reconstruction software based on CT data,
which was used to accurately reveal the anatomical details of the
double IVC and its surrounding tissue structure. The present case
suggested the importance of the recognition of IVC abnormalities.
In clinical practice, it is critical to perform preoperative
evaluation and preparation for IVC variation, which could be
associated with surgery outcomes. This variation in IVC may have
important clinical implications. It is of the utmost importance for
surgeons, interventional radiologists and clinicians to understand
the abnormalities in the anatomical features and to avoid
misdiagnosis and reduce the occurrence of severe intraoperative
complications.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
WL and LY made substantial contributions to the
design of the study, collected clinical information, and drafted
the manuscript, ZD and JX conceived the paper's objective and
collected the patient's data. ZL and LZ analyzed the data and
performed the literature search. WL and ZD confirm the authenticity
of all the raw data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The present case report was approved by the Ethics
Committees of Yichang Central People's Hospital (approval no.
18/16.10.2021). Written informed consent was obtained from the
patient.
Patient consent for publication
The patient provided written informed consent for
the publication of the information.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Shaheen S, Alyahya KI, Fouhil AFE, Salama
EEA, Atteya M, Elshaer F and Darwish H: An extremely rare complete
bilateral duplication of inferior vena cava in a male cadaver:
Anatomy, embryology and clinical relevance. Folia Morphol (Warsz).
81:247–253. 2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Banerjee A, Maharana S, Kumar IA and
Jhansi P: Duplication of the inferior vena cava-report of a rare
congenital variation. IJAV. 5:141–143. 2012.
|
|
3
|
Petik B: Inferior vena cava anomalies and
variations: Imaging and rare clinical findings. Insights Imaging.
6:613–639. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Babaian RJ and Johnson DE: Major venous
anomalies complicating retroperitoneal surgery. South Med J.
72:1254–1258. 1979.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Yoshimura S, Yamamoto K, Fujimura S,
Kawata S, Shimada K, Omotehara T and Itoh M: A case of double
inferior vena cava with the connection to sacral venous plexus.
Anat Sci Int. 97:143–146. 2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Waśniewska A, Ruzik K, Olewnik Ł,
Stefańczyk L and Polguj M: Unusual coexistence of double inferior
vena cava with nutcracker syndrome-a case report and review of the
literature. J Int Med Res. 48(300060520904520)2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Klinkhachorn PS, Ritz BK, Umstot SI,
Skrzat J and Zdilla MJ: Duplication of the inferior vena cava:
Evidence of a novel type IV. Folia Cracov. 60:5–13. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Chen HY, Emura S, Nagasaki S and Kubo K:
Double inferior vena cava with interiliac vein: A case report and
literature review. Okajimas Folia Anat Jpn. 88:147–151.
2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Matsuoka A, Tate S, Nishikimi K and Shozu
M: Retroperitoneal lymphadenectomy for ovarian cancer with double
inferior vena cava. Gynecol Oncol. 148:632–633. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Onoda K, Shomura Y and Komada T: Double
inferior vena cava with azygos continuation and retroaortic left
renal vein associated with juxtarenal abdominal aortic aneurysm
surgery. Ann Vasc Dis. 11:123–126. 2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Wang X, Chen Z and Cai Q:
Catheter-directed thrombolysis for double inferior vena cava with
deep venous thrombosis: A case report and literature review.
Phlebology. 29:480–483. 2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Pilichowska E, Ostrowski P, Kotowski MJ,
Tejchman K, Ostrowska-Clark K, Ostrowski M and Sieńko J:
Transplantation of a kidney with duplicated ureter harvested from a
donor with vascular anomaly in the form of double inferior vena
cava: A Case Report. Transplant Proc. 52:2533–2535. 2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Ito T and Ikeda Y: A case of double
inferior vena cava with renal, ovarian and iliac vein variation.
Anat Sci Int. 93:139–143. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Coco D, Cecchini S, Leanza S, Viola M,
Ricci S and Campagnacci R: Inferior vena cava duplication:
Incidental case in a young woman. Case Rep Radiol.
2016(3071873)2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Chaijaroonkhanarak W, Pannangrong W,
Welbat JU, Namking M, Khamanarong K and Prachaney P: Double
inferior vena cava with three shunts: A rare anomaly with important
implications for surgeons. Folia Morphol (Warsz). 76:307–311.
2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Jiang Y, Duan L, Lu L, Zhao WG, Zeng ZP,
Li HZ and Zhang XB: Rare case of reninoma with double inferior vena
cava. Clin Exp Hypertens. 33:325–327. 2011.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Nakatani T, Kim T, Naganuma T, Uchida J,
Takemoto Y and Sugimura K: Kidney transplants from living related
donors having double inferior vena cava. Urol Int. 72:358–360.
2004.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kumar S, Panigrahy B, Ravimohan SM, Pandya
S, Mandal AK and Singh SK: Rare case of renal cell carcinoma with
double inferior vena cava with venous thrombosis. Urology.
72:461.e7–e10. 2008.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Yano R, Hayakawa D, Emura S, Chen H, Ozawa
Y, Taguchi H and Shoumura S: Two cases of the double inferior venae
cavae. Okajimas Folia Anat Jpn. 77:133–136. 2000.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Fronek JP, Morsy MA, Singh U, Chemla E and
Chang RW: Retroperitoneoscopic live donor nephrectomy in a patient
with a double inferior vena cava. J Laparoendosc Adv Surg Tech A.
16:378–380. 2006.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Vasanth Kumar A, Anirudh Kumar A, Hussain
A and Sameeraja V: An uncommon encounter during temporary pacemaker
implantation-A double inferior vena cava. Indian Heart J. 68 (Suppl
2):S216–S217. 2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Furutani A, Yoshida S, Yoshida T, Nishi M,
Yamagishi T, Goto H, Otsubo D, Yamane H, Matsumoto T, Fujino Y and
Tominaga M: A case of laparoscopic anterior resection for rectal
cancer with duplication of the inferior vena cava using
preoperative 3D computed tomography angiography. J Surg Case Rep.
2020(rjaa223)2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Habuchi T, Okagaki T, Arai K and Miyakawa
M: Renal cell carcinoma extending into left side of double inferior
vena cava. Urology. 41:181–184. 1993.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Mao YQ, Zhu SX and Zhang W: The iatrogenic
injury of double vena cava due to misdiagnosis during the radical
nephroureterectomy and cystectomy. World J Surg Oncol.
13(41)2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Yamaguchi A, Negoro H, Kojo K, Ikeda A,
Kimura T, Kandori S, Hoshi A, Kojima T, Kawai K and Nishiyama H:
Retroperitoneal lymph node dissection for testicular cancer in a
patient with a double inferior vena cava. IJU Case Rep. 4:86–88.
2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Sousa Gomes M, Pardal C, Monteiro C and
Serrano P: Double inferior vena cava in gynaecological oncology
surgery. BMJ Case Rep. 13(e240361)2020.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Aljabri B, MacDonald PS, Satin R, Stein
LS, Obrand DI and Steinmetz OK: Incidence of major venous and renal
anomalies relevant to aortoiliac surgery as demonstrated by
computed tomography. Ann Vasc Surg. 15:615–618. 2001.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Shammas NW, Rachwan RJ, Daher G and
Dargham BB: Double inferior vena cava and its implications during
endovascular and surgical interventions: A word of caution. J
Invasive Cardiol. 29:51–53. 2017.PubMed/NCBI
|
|
29
|
Eldefrawy A, Arianayagam M, Kanagarajah P,
Acosta K and Manoharan M: Anomalies of the inferior vena cava and
renal veins and implications for renal surgery. Cent European J
Urol. 64:4–8. 2011.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Sitwala PS, Ladia VM, Brahmbhatt PB, Jain
V and Bajaj K: Inferior vena cava anomaly: A risk for deep vein
thrombosis. N Am J Med Sci. 6:601–603. 2014.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Sartori MT, Zampieri P, Andres AL,
Prandoni P, Motta R and Miotto D: Double vena cava filter insertion
in congenital duplicated inferior vena cava: A case report and
literature review. Haematologica. 91 (Suppl
6)(ECR30)2006.PubMed/NCBI
|
|
32
|
Vo NJ, Wieseler KW, Burdick TR, Goswami
GK, Vaidya SS and Andrews RT: The use of paired optionally
retrievable günther tulip filters in trauma patients with
anatomical variants. Semin Intervent Radiol. 24:20–28.
2007.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Hoppe RT, Advani RH, Ai WZ, Ambinder RF,
Armand P, Bello CM, Benitez CM, Bierman PJ, Boughan KM, Dabaja B,
et al: Hodgkin lymphoma, version 2.2020, NCCN clinical practice
guidelines in oncology. J Natl Compr Canc Netw. 18:755–781.
2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Lucas MF: A case of double inferior vena
cava. J Anat. 51(Pt 1). 69–70. 1916.PubMed/NCBI
|
|
35
|
Yagel S, Kivilevitch Z, Cohen SM, Valsky
DV, Messing B, Shen O and Achiron R: The fetal venous system, part
I: Normal embryology, anatomy, hemodynamics, ultrasound evaluation
and Doppler investigation. Ultrasound Obstet Gynecol. 35:741–750.
2010.PubMed/NCBI View
Article : Google Scholar
|
|
36
|
Mayo J, Gray R, St Louis E, Grosman H,
McLoughlin M and Wise D: Anomalies of the inferior vena cava. AJR
Am J Roentgenol. 140:339–345. 1983.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Mathews R, Smith PA, Fishman EK and
Marshall FF: Anomalies of the inferior vena cava and renal veins:
Embryologic and surgical considerations. Urology. 53:873–880.
1999.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Bass JE, Redwine MD, Kramer LA, Huynh PT
and Harris JH Jr: Spectrum of congenital anomalies of the inferior
vena cava: Cross-sectional imaging findings. Radiographics.
20:639–652. 2000.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Tisnado J, Amendola MA, Vines FS and
Beachley MC: Computed tomography of double inferior vena cava: The
‘double cava’ sign. Comput Tomogr. 3:195–199. 1979.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Inamasu J and Guiot BH: Laparoscopic
anterior lumbar interbody fusion: A review of outcome studies.
Minim Invasive Neurosurg. 48:340–347. 2005.PubMed/NCBI View Article : Google Scholar
|