Introduction
Infertility is estimated to affect ~186 million
individuals worldwide with a prevalence of 9-13% among women, which
results in various social, psychological and economic issues
(1-4).
In general, numerous factors are responsible for female
infertility, and fallopian tube obstruction is an important cause,
accounting for ~35% of anatomical factor-induced infertility
(5,6). Hysterosalpingography (HSG) is a
common and valuable X-ray test for the uterus and fallopian tubes
that assists in checking the patency of the fallopian tubes, the
site of obstruction and the morphology of the uterine cavity
(7,8). Beyond the diagnostic value, HSG also
has a potential therapeutic implication for infertile female
patients, since contrast medium is injected to flush the uterus and
fallopian tubes of the patient, which improves the tubal patency
and is beneficial for pregnancy (9,10).
Oil-based and water-based contrast media are two
options for HSG. The oil-based contrast medium has a high
viscosity, which enhances the flushing and dilation of the
fallopian tubes, while the water-based contrast medium has a low
viscosity and is absorbed quickly with a short stay in the pelvic
cavity, which places a minimal influence on the patients (11). A number of previous studies have
explored the effect of these two contrast media during HSG on
improving fertility, and hypothesized that an oil-based contrast
medium may be superior to a water-based contrast medium; however,
the improved fertility-enhancing effect of oil-based contrast
medium has not been widely accepted yet (9,12-24).
For example, one randomized controlled trial (RCT), including
patients with primary and secondary infertility, has highlighted
that the oil-based contrast medium for HSG increases the ongoing
pregnancy rate, number of clinical pregnancies and number of live
births, as well as reduces the time to pregnancy compared with the
water-based contrast medium (23).
Another non-RCT study has indicated that the pregnancy rate is
increased using the water-based contrast medium compared with the
oil-based contrast medium in patients receiving HSG (22); however, this opposing finding may
be due to the study having only enrolled patients with secondary
infertility. Another study reported that the cumulative pregnancy
rate is not influenced by using oil-based or water-based contrast
medium in patients receiving HSG with primary or secondary
infertility (19). A few previous
meta-analyses have explored the optimal contrast medium for
improving pregnancy in patients receiving HSG (25,26).
However, these two meta-analyses used only RCTs and omitted the
influence of non-RCTs. Additionally, some updated clinical studies
regarding the fertility-enhancing effect in patients receiving HSG
should be taken into account (23,24).
Apart from the aforementioned study, a recently published
meta-analysis also concluded that an oil-based contrast medium
exhibits an improved fertility-enhancing effect compared with a
water-based contrast medium in patients receiving HSG (27). However, all studies used in this
meta-analysis were RCTs, thereby not taking into account the effect
of non-RCTs. In addition, whether the fertility-enhancing effect of
oil-based and water-based contrast media would be affected by the
follow-up duration was not reported. Furthermore, only 4,739
patients were included in this meta-analysis, and a large-scale
meta-analysis is required to improve the statistical power
(27).
Therefore, the present meta-analysis comprehensively
screened both RCTs and non-RCTs and slightly increased the number
of patients with the aim of comparing the fertility-enhancing
effect between the oil-based and water-based contrast media in
patients receiving HSG.
Materials and methods
Search strategy
The present meta-analysis was conducted according to
the Preferred Reporting Items for Systematic Review and
Meta-Analysis guidelines (28).
Studies that assessed the fertility enhancement between oil-based
and water-based contrast media during HSG were screened in Web of
Science (WOS) (https://clarivate.com/products/webofscience/), PubMed
(https://pubmed.ncbi.nlm.nih.gov/),
Excerpta Medica Database (EMBASE) (https://elh.nhs.wales/databases/databases/embase-excerpta-medica1/),
Cochrane (https://www.cochranelibrary.com/), China National
Knowledge Infrastructure (CNKI) (https://en.cnki.com.cn/), Wanfang Data (https://www.wanfangdata.com.cn/index.html) and China
Science and Technology Journal Database (CQVIP; http://csi1.cqvip.com/productor/pro_zk.shtml) up to
November 10, 2022 and there was no cut off for studies published
earlier than any given year. The following medical subject headings
and keywords were used for study searching:
‘Hysterosalpingography’, ‘HSG’, ‘hysterosalpingo contrast
sonography’, ‘tubal patency test’, ‘laparoscopy’, ‘oil’,
‘ethiodol’, ‘lipiodol’, ‘poppy’, ‘water’, ‘iotrolan’, ‘iodipamide’,
‘iohexol’, ‘diatrizoate’ and ‘aqueous’. Additionally, the
references of the included studies were also screened as
aforementioned.
Study selection
Two researchers worked independently to complete the
study screening. First, the studies were screened based on a
previously designed information extraction form (25). Second, the title and the abstract
were evaluated according to the inclusion and exclusion criteria
described later. Third, the studies considered acceptable for
inclusion were downloaded, and the full texts were read. Next, the
data of the included studies were extracted, and their references
were also examined as aforementioned. A cross-discussion or
consultation with a 3rd investigator was held if there was a
disagreement.
The inclusion criteria were as follows: i) RCT or
non-RCT study (such as a cohort study or case-control study); ii)
patients ≥18 years old; iii) patients underwent HSG with oil-based
or water-based contrast medium; and iv) studies had ≥1 outcome
concerned (including clinical pregnancy, ongoing pregnancy, live
birth, miscarriage, or ectopic pregnancy) in the present study. The
exclusion criteria were as follows: i) Other study types (such as a
systematic review or meta-analysis); ii) duplicated study; and iii)
incomplete or inconsistent data.
Data extraction
Two researchers worked independently to complete the
data extraction. The extracted data contained the names of the
authors, publication year, study type, study location, sample size,
follow-up duration, method of tube flushing, contrast medium and
outcome (clinical pregnancy, ongoing pregnancy, live birth,
miscarriage or ectopic pregnancy). A cross-discussion or
consultation with a 3rd investigator was held if there was a
disagreement.
Quality assessment
The bias risk of RCTs was evaluated using the
Cochrane Collaboration risk of bias tool, and involved selection,
performance, detection, attrition and reporting bias amongst others
(29). The bias risk of non-RCTs
was evaluated using the Newcastle-Ottawa Scale criteria, and
involved selection, comparability and outcome. A total score
#x003C;4 was considered as high risk of bias; the total score
ranging 4-6 was considered as moderate risk of bias; the total
score ranging from 7-9 was considered as low risk of bias (30).
Statistical analysis
Stata software (version 14.0; StataCorp LP) was used
for statistical analysis. Relative risks (RRs) and 95% confidence
intervals (CIs) were presented for outcome assessment. Since none
of the studies selected for this analysis have any relation with
each other, the random effects model was utilized for all analyses
regardless of the I2 value or P-value. It should be
mentioned that I2 ≤50.0% and P≥0.10 referred to low
heterogeneity. I2 >50% and P#x003C;0.01 referred to
high heterogeneity. Publication bias was analyzed using Egger's and
Begg's tests. Sensitivity analysis was carried out for the
evaluation of data robustness and stability. Briefly, the RR and
95% CI calculations were performed again after sequentially
omitting each study, then the results were compared with the
previous data analysis and no statistically significant changes
were considered to indicate low sensitivity to any study omission
and robust results. P#x003C;0.05 was considered to indicate a
statistically significant difference.
Results
Study screening procedure
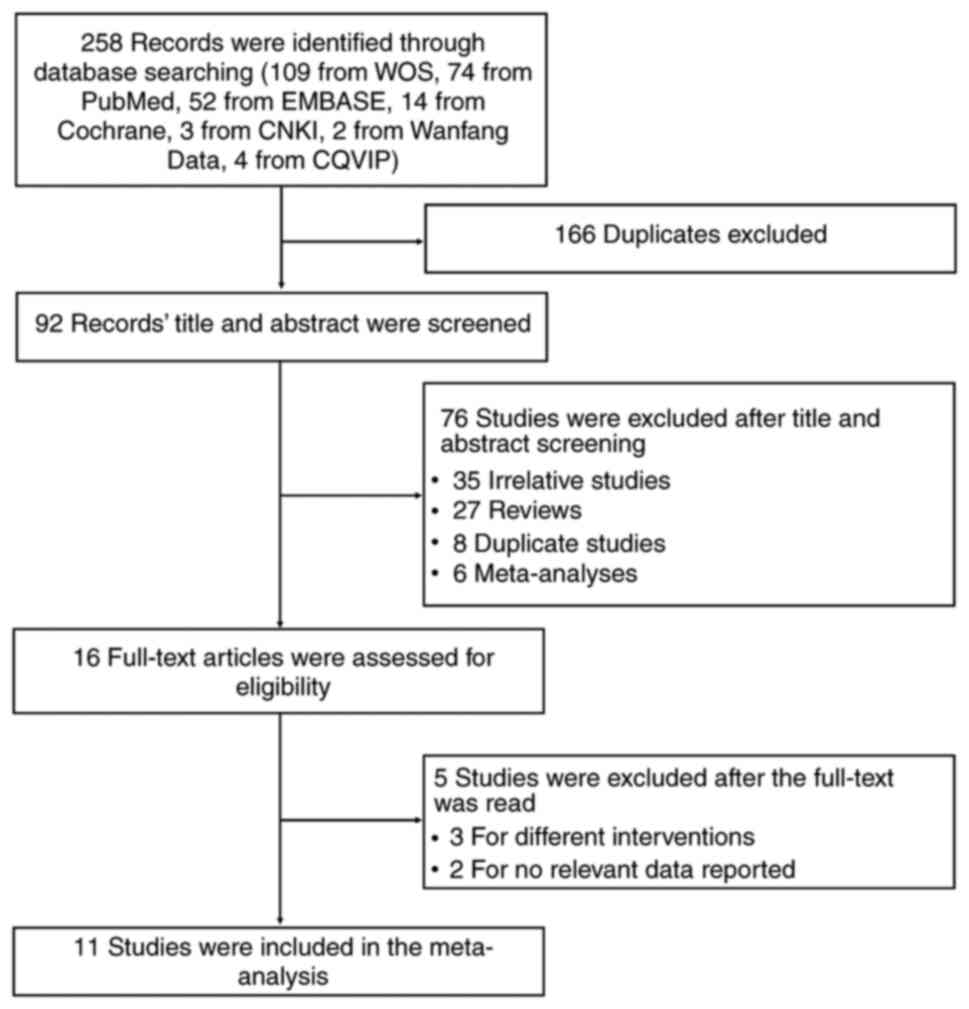
Initially, 258 records were identified through
database screening, including 109 records from WOS, 74 records from
PubMed, 52 records from EMBASE, 14 records from Cochrane, 3 records
from CNKI, 2 records from Wanfang Data and 4 records from CQVIP.
Subsequently, 166 duplicates were excluded, and the remaining 92
records were screened by title and abstract. Subsequently, 76
records were excluded, including 35 irrelevant studies, 27 reviews,
8 duplicated studies and 6 meta-analyses. The remaining 16
full-text articles were then assessed for eligibility, during which
5 records were further excluded after the full-text was read,
including 3 records for different interventions and 2 records for
lacking relevant data. Finally, 11 studies were selected to be
included in the present meta-analysis (Fig. 1).
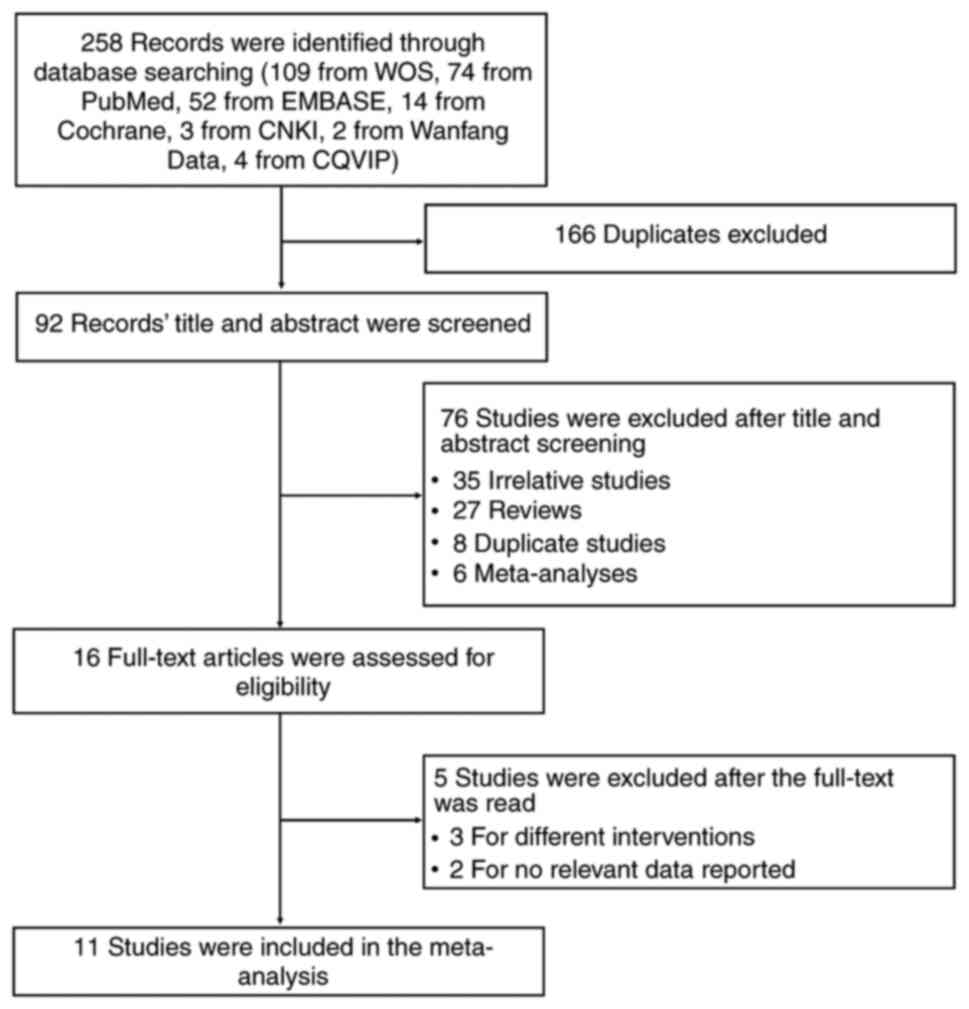 | Figure 1Study flow chart. A total of 258
records were identified through database searching, including 109
from WOS, 74 from PubMed, 52 from EMBASE, 14 from Cochrane, 3 from
CNKI, 2 from Wanfang Data, and 4 from CQVIP. After that, 166
duplicates were excluded. The title and abstract of 92 records were
screened, and 76 studies were further excluded, including 35
irrelevant studies, 27 reviews, 8 duplicate studies and 6
meta-analyses. Subsequently, 16 full-text articles were assessed
for eligibility, and 5 studies were excluded after full-text was
read, including 3 for different interventions and 2 for no relevant
data reported. Ultimately, 11 studies were included in the
meta-analysis. CNKI, China National Knowledge Infrastructure;
CQVIP, China Science and Technology Journal Database; EMBASE,
Excerpta Medica Database; WOS, Web of Science. |
Features of the included studies
The screened studies included eight RCTs (14-19,21,23)
and three non-RCTs (20,22,24).
Regarding the locations of the studies, the eight RCTs were
conducted in USA, The Netherlands, Denmark and China, whereas the
three non-RCTs were all conducted in China. The publication year of
the selected studies ranged from 1986 to 2022; specifically, four
studies were published before 2000, including Alper et al
(14), de Boer et al
(15), Rasmussen et al
(16) and Lindequist et al
(17); three studies were
published between 2000 and 2010, including Spring et al
(18), Steiner et al
(19) and Qiu (20); and four studies were published
after 2010, including Dreyer et al (21), Wang et al (22), Zhang et al (23) and Lu et al (24). A total of 5,292 patients were
included in the present study, including 2,462 patients receiving
oil-based contrast medium and 2,830 patients receiving water-based
contrast medium during HSG. The majority of the studies included
patients with primary and patients with secondary infertility;
however, this information was unclear in two of the studies, and
one study included only patients with secondary infertility.
Regarding endometriosis, six studies did not report this
information and three studies excluded patients with endometriosis;
however, 24.8 and 18.6% of patients had a history of endometriosis
in the other two studies. The specific features of the included
studies are listed in Table I.
 | Table IDetails of the included studies. |
Table I
Details of the included studies.
| | Sample size, n | | Contrast
medium | Type of
patient | |
|---|
| First author,
year | Study type | Study location | Oil | Water | Follow-up duration,
months | Method of tubal
flushing | Oil | Water | Primary or
secondary infertility | Endometriosis | Outcome | (Refs.) |
|---|
| Alper et al,
1986 | RCT | USA | 58 | 73 | 6 | HSG | Lipiodol | Reno-M-60 | Unclear | Unclear | Clinical
pregnancy | (14) |
| de Boer et
al, 1988 | RCT | The
Netherlands | 87 | 88 | 6 | HSG | Ethiodol | Lopamidol | Both types | Unclear | Clinical
pregnancy | (15) |
| Rasmussen et
al, 1991 | RCT | Denmark | 98 | 300 | 10 | HSG | Lipiodol | Iohexol, ioxaglate
or diatrizoate | Both types | Unclear | Clinical pregnancy
and live birth | (16) |
| Lindequist et
al, 1994 | RCT | Denmark | 121 | 121 | 9 | HSG | Lipiodol | Iotrolan | Both types | Unclear | Clinical
pregnancy | (17) |
| Spring et
al, 2000 | RCT | USA | 273 | 260 | 12 | HSG | Ethiodol | Sinografin | Both types | Unclear | Clinical pregnancy,
live birth, miscarriage and ectopic pregnancy | (18) |
| Steiner et
al, 2003 | RCT | USA | 28 | 25 | 18 | HSG | Ethiodol | Sinografin | Both types | A total of 24.8% of
patients had a history of endometriosis | Clinical
pregnancy | (19) |
| Qiu, 2005 | Non-RCT | China | 132 | 283 | 6 | HSG | Iodinate oil | Iohexol | Unclear | Unclear | Clinical
pregnancy | (20) |
| Dreyer et
al, 2017 | RCT | The
Netherlands | 557 | 562 | 6 | HSG | Lipiodol | Telebrix
Hystero | Both types | Excluded patients
with endometriosis | Clinical pregnancy,
ongoing pregnancy, live birth, miscarriage and ectopic
pregnancy | (21) |
| Wang et al,
2021 | Non-RCT | China | 100 | 100 | 6 | HSG | Iodinate oil | Iohexol | Secondary
infertility | Excluded patients
with endometriosis | Clinical
pregnancy | (22) |
| Zhang et al,
2022 | RCT | China | 508 | 518 | 6 | HSG | Ethiodized
poppyseed oil | Iohexol (300
mg/ml), iopromide (300 mg/ml) or ioversol (320 mg/ml) | Both types | Excluded patients
with endometriosis | Clinical pregnancy,
ongoing pregnancy, live birth and miscarriage | (23) |
| Lu et al,
2022 | Non-RCT | China | 500 | 500 | 36 | HSG | Ethiodized poppy
seed oil | Ioversol | Both types | A total of 18.6% of
patients had a history of endometriosis | Clinical
pregnancy | (24) |
Quality assessments
Regarding selection bias, 5 RCTs were ranked as low
risk of random sequence generation; thus, 62.5% (5/8) of the RCTs
presented sufficient methods of random sequence generation.
Meanwhile, 1 RCT was ranked as low risk of allocation concealment;
thus,12.5% (1/8) of the studies disclosed adequate methods of
allocation concealment. Since blind trials were impossible owing to
the nature of the interventions, the risk of performance bias was
scored as unclear. Considering that the fertility outcome was
objective, a non-blinded design would not influence the outcome
assessment; thus, the risk of detection bias was low in all
studies. There were three RCTs at high risk of allocation
concealment (19), incomplete
outcome data (14) and other
sources of bias (18) (Table II). In the three non-RCTs, the
total score of the assessment of the risk of bias ranged from 7 to
9, which indicated a low risk of bias (Table III). Briefly, Qiu (20) lacked a definition for the controls
and an adequate follow-up, resulting in a total score of 7. Wang
et al (22) had a score of
1 for the risk of comparability owing to a lack of control for
confounders, resulting in a total score of 8. Lu et al
(24) had reduced bias compared
with other two non-RCTs with a total score of 9.
 | Table IIAssessment of the risk of bias among
the eight randomized controlled trials. |
Table II
Assessment of the risk of bias among
the eight randomized controlled trials.
| First author,
year | Random sequence
generation (selection bias) | Allocation
concealment (selection bias) | Blinding of
participants and personnel (performance bias) | Blinding of outcome
assessment (detection bias) | Incomplete outcome
data (attrition bias) | Selective reporting
(reporting bias) | Other sources of
bias (other bias) | (Refs.) |
|---|
| Alper et al,
1986 | Low risk | Unclear | Unclear | Low risk | High risk | Unclear | Unclear | (14) |
| de Boer et
al, 1988 | Unclear | Unclear | Unclear | Low risk | Low risk | Unclear | Low risk | (15) |
| Rasmussen et
al, 1991 | Unclear | Unclear | Unclear | Low risk | Unclear | Unclear | Unclear | (16) |
| Lindequist et
al, 1994 | Unclear | Unclear | Unclear | Low risk | Unclear | Unclear | Low risk | (17) |
| Spring et
al, 2000 | Low risk | Unclear | Unclear | Low risk | Low risk | Low risk | High risk | (18) |
| Steiner et
al, 2003 | Low risk | High risk | Unclear | Low risk | Low risk | Unclear | Low risk | (19) |
| Dreyer et
al, 2017 | Low risk | Low risk | Unclear | Low risk | Low risk | Low risk | Low risk | (21) |
| Zhang et al,
2022 | Low risk | Unclear | Unclear | Low risk | Low risk | Unclear | Low risk | (23) |
 | Table IIIAssessment of the risk of bias among
the three non-randomized controlled trials. |
Table III
Assessment of the risk of bias among
the three non-randomized controlled trials.
| | Selection | Comparability | Outcome | |
|---|
| First author,
year | Adequate definition
of cases | Representativeness
of the cases | Selection of
controls | Definition of
controls | Cohorts on the
basis of the design or analysis controlled for confounders | Assessment of
outcome | Was follow-up long
enough | Adequacy of
follow-up | Total
scorea | (Refs.) |
|---|
| Qiu, 2005 | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 7 | (20) |
| Wang et al,
2021 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | (22) |
| Lu et al,
2022 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | (24) |
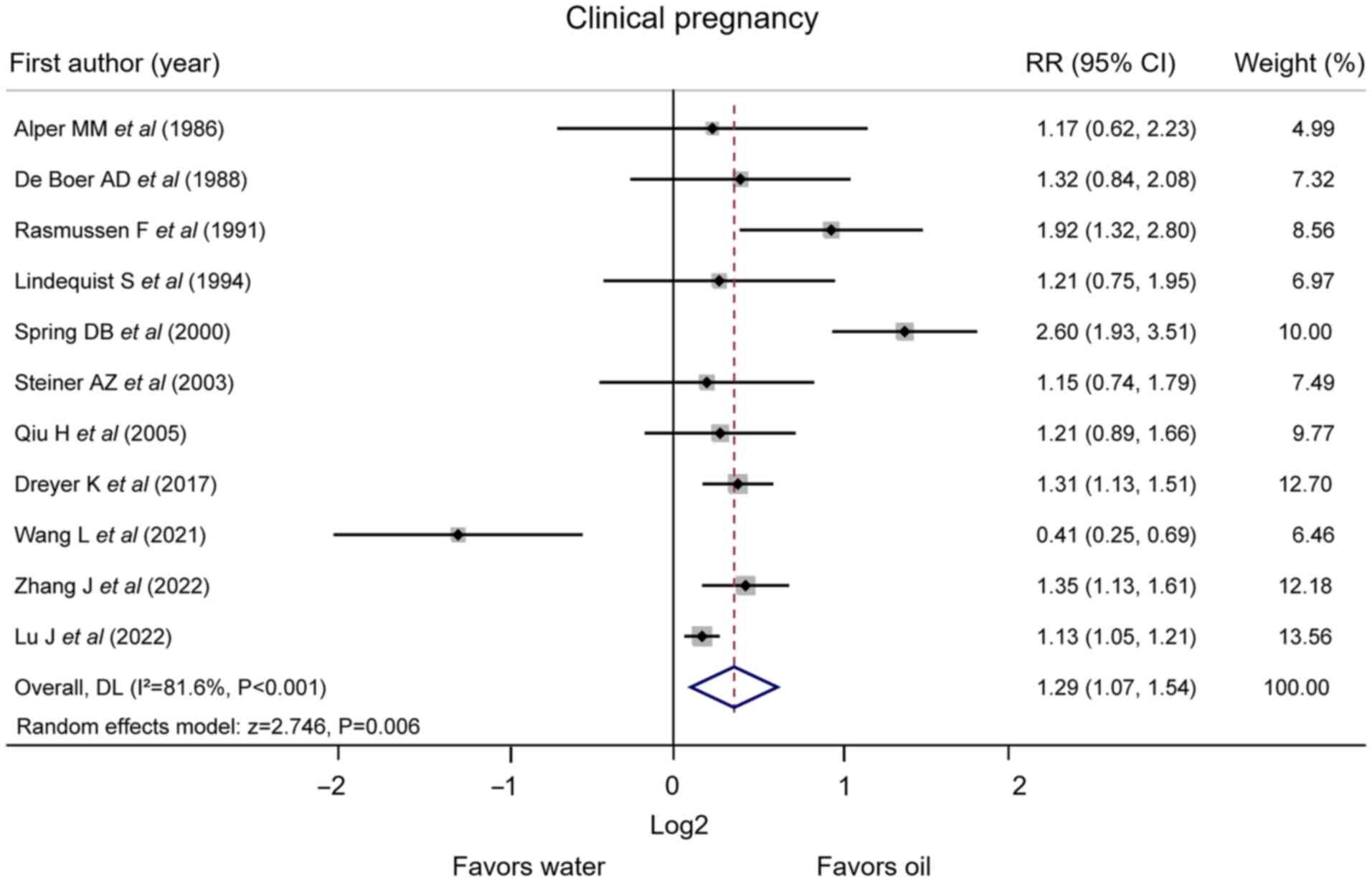
Clinical pregnancy
All 11 studies reported clinical pregnancy. The
pooled analysis revealed that the oil-based contrast medium
increased the rate of clinical pregnancy compared with the
water-based contrast medium [RR (95% CI), 1.29 (1.07, 1.54);
P=0.006]. Heterogeneity existed among the studies
(I2=81.6%; P#x003C;0.001; Fig. 2).
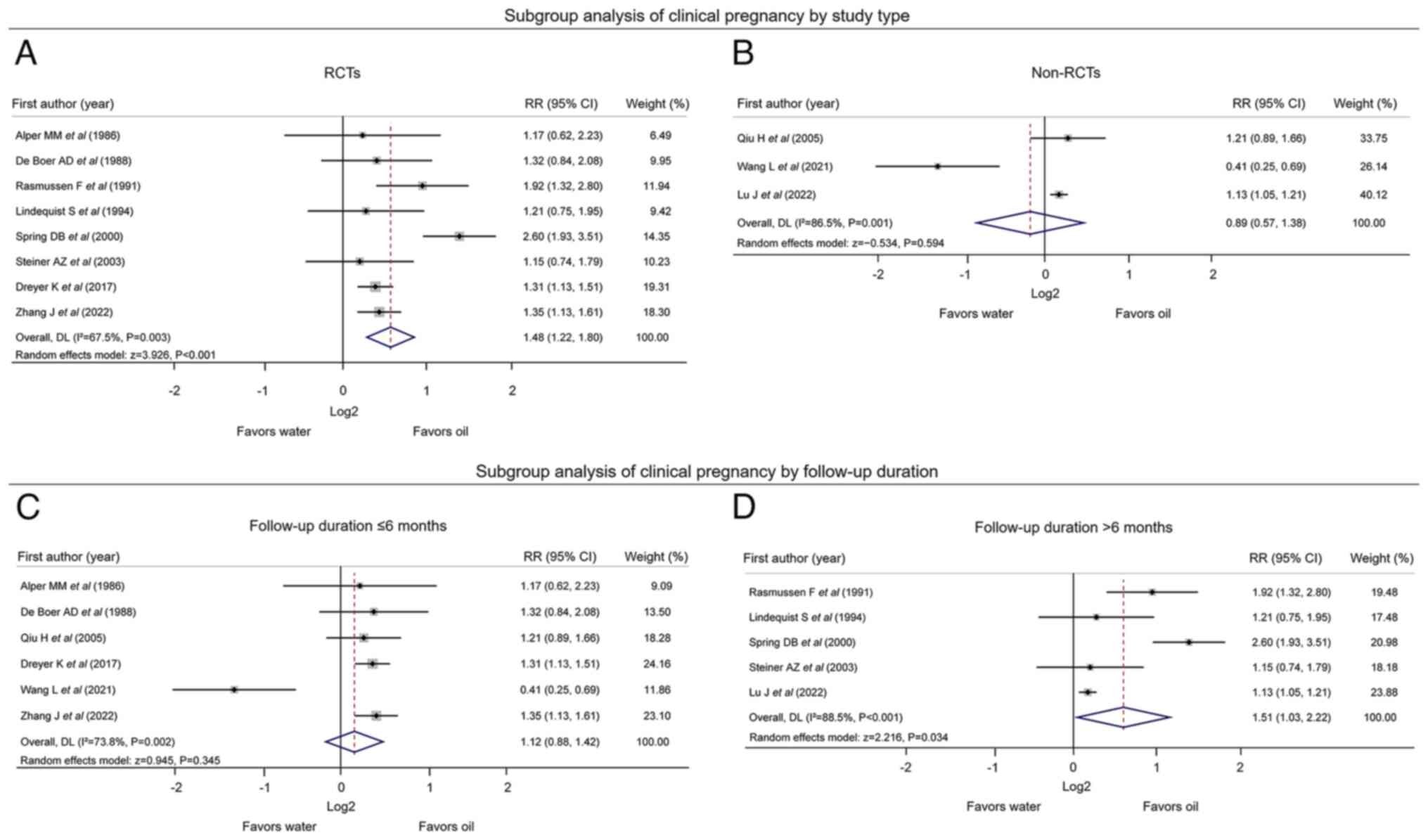
Subgroup analyses were carried out based on the
study type. The pooled analysis of the eight RCTs revealed that the
rate of clinical pregnancy was increased following the use of
oil-based contrast medium compared with water-based contrast medium
during HSG [RR (95% CI), 1.48 (1.22, 1.80); P#x003C;0.001];
heterogeneity existed among these studies (I2=67.5%;
P=0.003) (Fig. 3A). Pooled
analysis of the three non-RCTs suggested that the rate of clinical
pregnancy was not different between patients receiving oil-based
contrast medium and patients receiving water-based contrast medium
for HSG [RR (95% CI), 0.89 (0.57, 1.38); P=0.594]; there was
heterogeneity among these studies (I2=86.5%; P=0.001)
(Fig. 3B). The pooled analysis of
six studies with a follow-up duration ≤6 months revealed that the
rate of clinical pregnancy was not affected by using oil-based or
water-based contrast medium [RR (95% CI), 1.12 (0.88, 1.42);
P=0.345]; heterogeneity existed among these studies
(I2=73.8%; P=0.002) (Fig.
3C). Pooled analysis of five studies with a follow-up duration
>6 months indicated that the rate of clinical pregnancy was
increased using oil-based contrast medium compared with water-based
contrast medium during HSG [RR (95% CI), 1.51 (1.03, 2.22);
P=0.034]; heterogeneity existed among the studies
(I2=88.5%; P#x003C;0.001) (Fig. 3D).
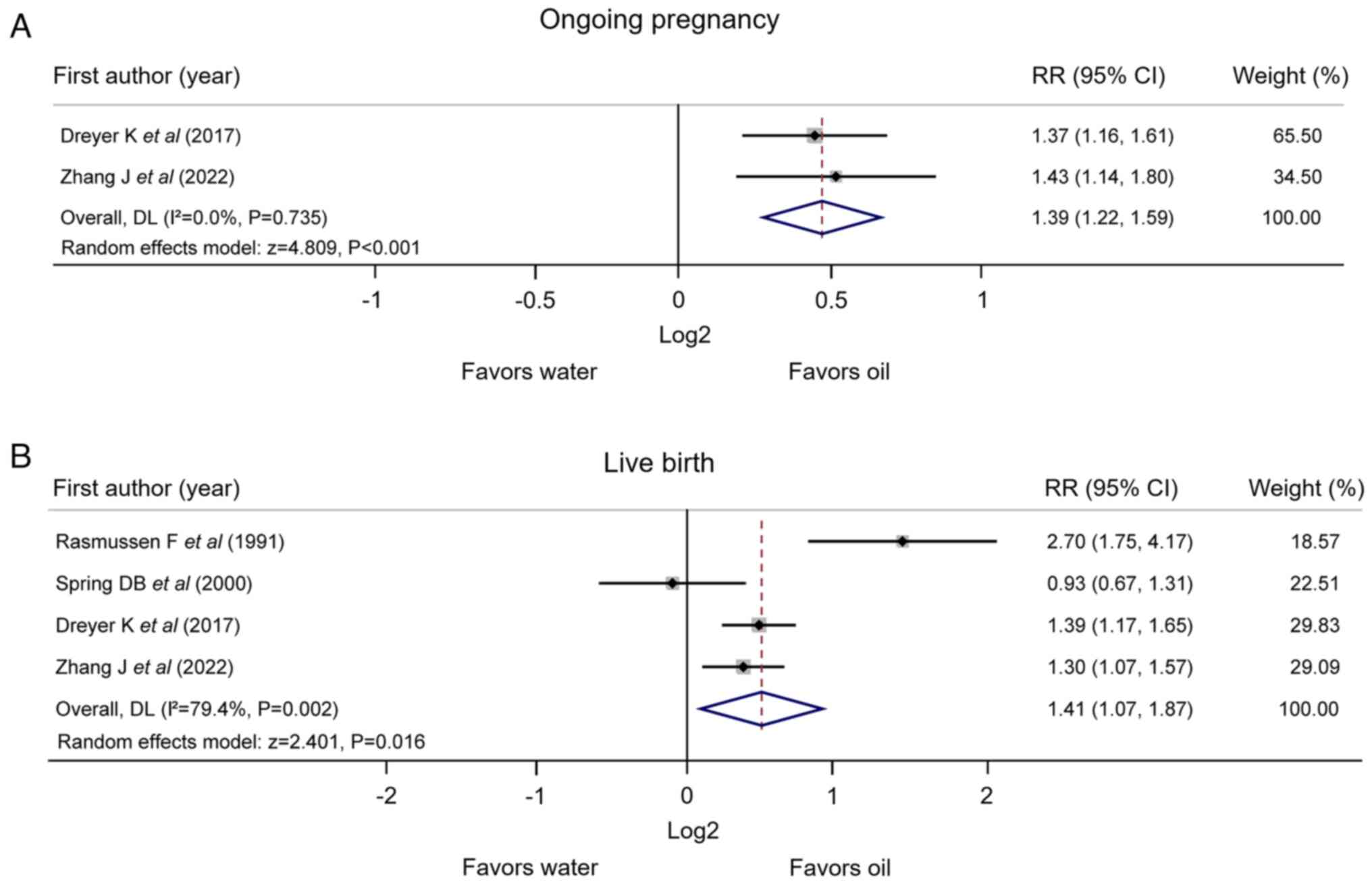
Ongoing pregnancy and live birth
There were two studies that reported ongoing
pregnancy. The pooled analysis suggested that the rate of ongoing
pregnancy was enhanced by the oil-based contrast medium compared
with the water-based contrast medium during HSG [RR (95% CI), 1.39
(1.22, 1.59); P#x003C;0.001]; heterogeneity did not exist between
the two studies (I2=0.0%; P=0.735) (Fig. 4A). In addition, four studies
reported live birth, and the pooled analysis indicated that the
rate of live birth was increased using oil-based contrast medium
compared with water-based contrast medium [RR (95% CI), 1.41 (1.07,
1.87); P=0.016]; there was heterogeneity among the studies
(I2=79.4%; P=0.002; Fig.
4B).
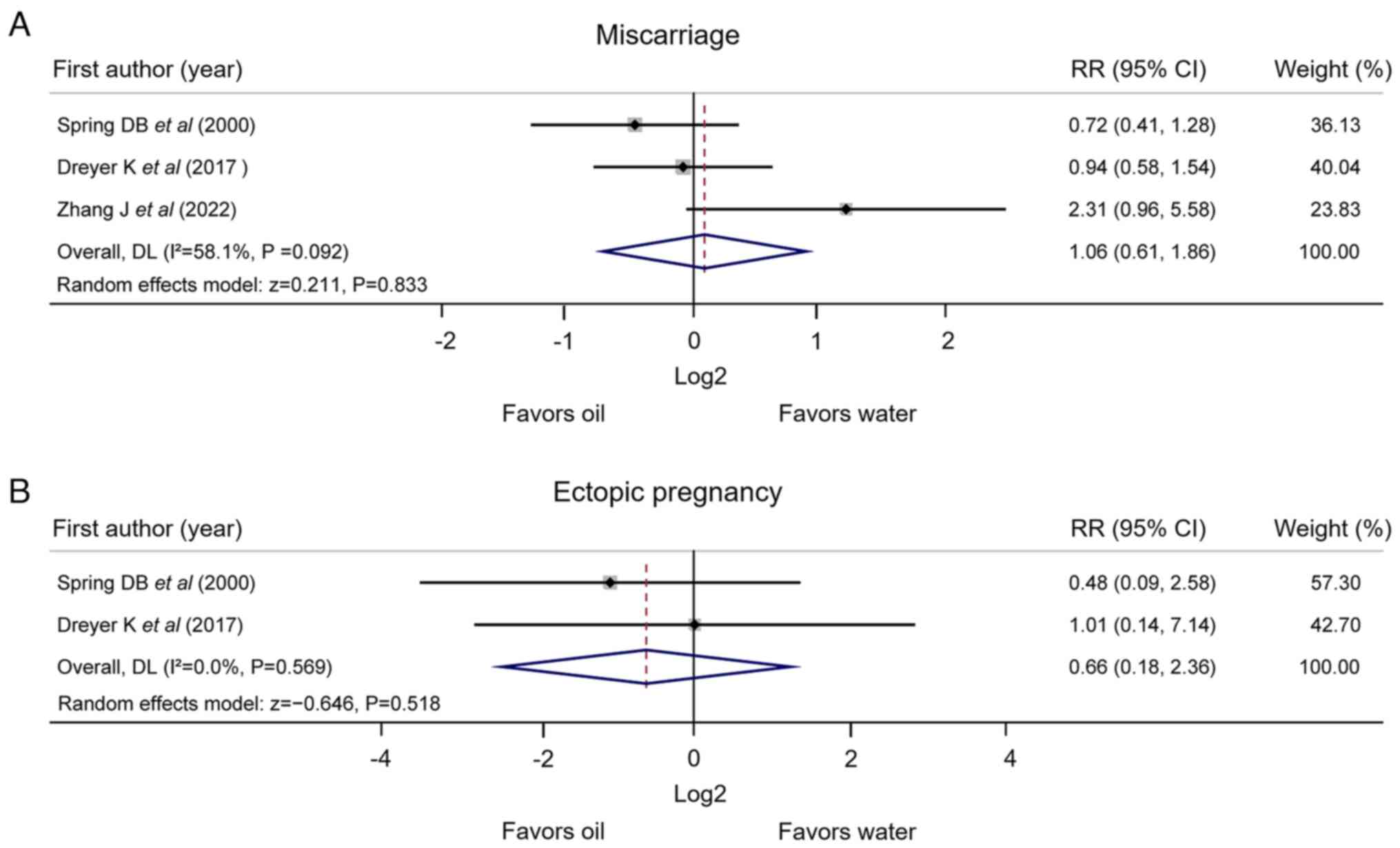
Miscarriage and ectopic pregnancy
There were three studies that reported miscarriage;
however, the pooled analysis revealed that the rate of miscarriage
was not affected by using oil-based or water-based contrast medium
[RR (95% CI), 1.06 (0.61, 1.86); P=0.833]; there was no
heterogeneity among the studies (I2=58.1%; P=0.092)
(Fig. 5A). Furthermore, two
studies reported ectopic pregnancy. The pooled analysis revealed
that the rate of ectopic pregnancy was not affected by using
oil-based or water-based contrast medium [RR (95% CI), 0.66 (0.18,
2.36); P=0.518]; there was no heterogeneity between the two studies
(I2=0.0%; P=0.569) (Fig.
5B).
Publication bias and sensitivity
analysis
Begg's and Egger's tests were carried out to
estimate the potential publication bias, and the results suggested
that no publication bias for clinical pregnancy, ongoing pregnancy,
live birth, miscarriage and ectopic pregnancy existed (all
P>0.05) (Table IV). In
addition, sensitivity analysis was conducted, and it was
demonstrated that omitting Dreyer et al (21) or Zhang et al (23) would affect the RR of the rate of
live birth. Furthermore, the RR of clinical pregnancy, ongoing
pregnancy, miscarriage and ectopic pregnancy did not change by
omitting any single study, which indicated the stability of the
present meta-analysis (Table
V).
 | Table IVPublication bias. |
Table IV
Publication bias.
| Outcomes | Number of included
studies | P-value (Begg's
test) | P-value (Egger's
test) |
|---|
| Clinical
pregnancy | 11 | 0.276 | 0.530 |
| Ongoing
pregnancy | 2 | 1.000 | 1.000 |
| Live birth | 4 | 1.000 | 0.709 |
| Miscarriage | 3 | 1.000 | 0.381 |
| Ectopic
pregnancy | 2 | 1.000 | 1.000 |
 | Table VSensitivity analysis for omitted
studies. |
Table V
Sensitivity analysis for omitted
studies.
| A, Clinical
pregnancy |
|---|
| First author,
year | Relative risk (95%
CI) | (Refs.) |
|---|
| Alper et al,
1986 | 1.291 (1.071,
1.555) | (14) |
| de Boer et
al, 1988 | 1.281 (1.060,
1.549) | (15) |
| Rasmussen et
al, 1991 | 1.239 (1.032,
1.489) | (16) |
| Lindequist et
al, 1994 | 1.290 (1.067,
1.559) | (17) |
| Spring et
al, 2000 | 1.202 (1.037,
1.393) | (18) |
| Steiner et
al, 2003 | 1.296 (1.071,
1.567) | (19) |
| Qiu, 2005 | 1.291 (1.062,
1.570) | (20) |
| Dreyer et
al, 2017 | 1.274 (1.023,
1.586) | (21) |
| Wang et al,
2021 | 1.387 (1.183,
1.626) | (22) |
| Zhang et al,
2022 | 1.272 (1.034,
1.565) | (23) |
| Lu et al,
2022 | 1.299 (1.039,
1.624) | (24) |
| Combined | 1.285 (1.075,
1.537) | |
| B, Ongoing
pregnancy |
| First author,
year | Relative risk (95%
CI) | (Refs.) |
| Dreyer et
al, 2017 | 1.435 (1.142,
1.803) | (21) |
| Zhang et al,
2022 | 1.366 (1.158,
1.613) | (23) |
| Combined | 1.390 (1.215,
1.589) | |
| C, Live birth |
| First author,
year | Relative risk (95%
CI) | (Refs.) |
| Rasmussen et
al, 1991 | 1.250 (1.039,
1.503) | (16) |
| Spring et
al, 2000 | 1.576 (1.174,
2.115) | (18) |
| Dreyer et
al, 2017 | 1.449 (0.893,
2.352) | (21) |
| Zhang et al,
2022 | 1.486 (0.928,
2.381) | (23) |
| Combined | 1.410 (1.065,
1.867) | |
| D, Miscarriage |
| First author,
year | Relative risk (95%
CI) | (Refs.) |
| Spring et
al, 2000 | 1.196 (0.784,
1.824) | (18) |
| Dreyer et
al, 2017 | 1.064 (0.669,
1.690) | (21) |
| Zhang et al,
2022 | 0.844 (0.582,
1.225) | (23) |
| Combined | 1.062 (0.607,
1.856) | |
| E, Ectopic
pregnancy |
| First author,
year | Relative risk (95%
CI) | (Refs.) |
| Spring et
al, 2000 | 1.009 (0.143,
7.138) | (18) |
| Dreyer et
al, 2017 | 0.476 (0.088,
2.578) | (21) |
| Combined | 0.656 (0.183,
2.356) | |
Discussion
The oil-based contrast medium has the benefit of
increasing the rate of clinical pregnancy in patients receiving
HSG; however, it has not been widely accepted and incorporated into
clinical practice (14-24).
For example, a previous study demonstrated that the clinical
pregnancy rate was unchanged between patients receiving oil-based
and water-based contrast media for HSG (14); however, this study did not indicate
the infertility status (primary or secondary) of the patients.
Another study reported that the use of oil-based contrast medium
enhances clinical pregnancy compared with the water-based contrast
medium during HSG in patients with primary infertility as well as
in patients with secondary infertility (16). However, a recent study demonstrated
that the water-based contrast medium improves the pregnancy rate
compared with the oil-based contrast medium in patients with
secondary infertility; this opposing finding may be attributable to
the fact that all included patients had secondary infertility
(22). The present meta-analysis
reviewed 11 studies (including 8 RCTs and 3 non-RCTs), and revealed
that the rate of clinical pregnancy was increased by using an
oil-based contrast medium compared with a water-based contrast
medium in patients receiving HSG; in addition, this finding was
further confirmed in the subgroup analysis conducted in RCTs and
studies with a follow-up duration >6 months. The potential
reasons for this outcome could be as follows: i) The oil-based
contrast medium regulates the dendritic cells and regulatory T cell
profiles and it could be incorporated by dendritic cells, thus
altering the immune environment in the peritoneal cavity, which
further improves the fertility (31); ii) the slow absorption speed of the
oil-based contrast medium enhances the suppression of macrophage
phagocytosis and adherence, which further reduces sperm
phagocytosis and increases clinical pregnancy (32); and iii) the oil-based contrast
medium removes mucus plugs from the fallopian tubes, which improves
tubal patency and is beneficial for clinical pregnancy (33-35).
The oil-based contrast medium increased rate of clinical pregnancy
compared with the water-based contrast medium in studies with a
follow-up duration >6 months, which indicated that the
pregnancy-enhancing effect of the oil-based contrast medium was
improved over 6 months. Notably, heterogeneity in the rate of
clinical pregnancy existed among the 11 studies analyzed. Although
sensitivity analysis disclosed that no single study affected the
pooled analysis of clinical pregnancy, further studies are required
to verify these findings.
Apart from clinical pregnancy, the present
meta-analysis also explored the efficacy of using an oil-based or a
water-based contrast medium for improving ongoing pregnancy and
live birth in patients receiving HSG. It was revealed that the
rates of ongoing pregnancy and live birth were enhanced using an
oil-based contrast medium compared with a water-based contrast
medium in patients receiving HSG. It can be speculated that the
oil-based contrast medium may be helpful for enhancing the
receptivity of the endometrium, which is beneficial for embryo
development and implantation (34,36,37),
ultimately leading to the improvement of ongoing pregnancy and live
birth. However, heterogeneity in live birth rates existed among the
four studies analyzed, and sensitivity analysis indicated that
after omitting Dreyer et al (21) or Zhang et al (23), the results of live birth would be
affected. However, considering the number of studies that reported
ongoing pregnancy and live birth were relatively few compared with
the total number of studies analyzed, the reliability and
generalization of these findings should be verified by further
large-scale studies.
Miscarriage and ectopic pregnancy are two major
concerns in pregnant patients, and these two issues may occur after
HSG (18,21,23,38,39).
The present study revealed that miscarriage and ectopic pregnancy
did not differ after HSG with the oil-based or water-based contrast
medium. The potential reason behind this may be that the major
causes of miscarriage and ectopic pregnancy are chromosomal
abnormalities, uterus abnormalities and hormonal problems, rather
than the administration of contrast media (38,39).
Thus, miscarriage and ectopic pregnancy were not affected by using
oil-based or water-based contrast medium during HSG.
A recently published meta-analysis has demonstrated
that using an oil-based contrast medium improves the pregnancy and
live birth rates compared with a water-based contrast medium,
whereas miscarriage and ectopic pregnancy are not affected by
either an oil-based or a water-based contrast medium in patients
receiving HSG (27). The present
meta-analysis slightly increased the number of patients and
screened both RCTs and non-RCTs, aiming to provide a comprehensive
view of the fertility-enhancing effect of oil-based and water-based
contrast media during HSG. In accordance with the aforementioned
meta-analysis (27), it was also
revealed in the present study that the fertility-enhancing effect
was increased using an oil-based contrast medium compared with a
water-based contrast medium during HSG, whereas miscarriage and
ectopic pregnancy remained unchanged between the two contrast
media. The present meta-analysis also revealed that in studies with
a follow-up duration >6 months, the fertility-enhancing effect
was increased using an oil-based contrast medium compared with a
water-based contrast medium during HSG.
The majority of the studies used in the present
meta-analysis did not include information on endometriosis.
However, two of the studies reported 24.8% (19) and 18.6% (24) of patients with a history of
endometriosis. In addition, three studies indicated that patients
with fallopian tube disease, including endometriosis, were excluded
(21-23).
Furthermore, the majority of the studies contained patients with
primary and secondary infertility (15-19,21,23,24);
however, two studies did not clearly report whether the patients
had primary or secondary infertility (14,20),
and one study included only patients with secondary infertility
(22). Although whether patients
have primary or secondary infertility may unavoidably affect the
results of the present meta-analysis, the majority of the included
studies did not distinguish patients based on the type of
infertility. Thus, the present study could not analyze the results
based on whether the patients had primary or secondary infertility,
and further studies that focus on the specific type of patients
should be conducted.
A number of limitations of the present study should
be noted: i) The number of studies that reported ongoing pregnancy
and live birth was small, thus, more large-scale studies are
required to validate these findings; ii) sensitivity analysis
revealed that omitting Dreyer et al (21) or Zhang et al (23) would affect the pooled analysis
finding of rates of live births; thus, more updated studies are
required to validate this finding; iii) there were three studies at
high risk of selection, attrition or other bias, which may
interfere with the results; and iv) the findings of the present
meta-analysis require further verification with real-world
clinical-setting studies.
The present meta-analysis concluded that using an
oil-based contrast medium increases the rates of clinical
pregnancy, ongoing pregnancy and live birth compared with a
water-based contrast medium in patients receiving HSG, indicating
the oil-based contrast medium for HSG may exert a superior
fertility-enhancing effect.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JL contributed to the study conception and design.
JC and SL performed data acquisition, analysis and interpretation.
JL and JC confirm the authenticity of all raw data. All authors
have read and approved the final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Inhorn MC and Patrizio P: Infertility
around the globe: New thinking on gender, reproductive technologies
and global movements in the 21st century. Hum Reprod Update.
21:411–426. 2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Boivin J, Bunting L, Collins JA and Nygren
KG: International estimates of infertility prevalence and
treatment-seeking: Potential need and demand for infertility
medical care. Hum Reprod. 22:1506–1512. 2007.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Datta J, Palmer MJ, Tanton C, Gibson LJ,
Jones KG, Macdowall W, Glasier A, Sonnenberg P, Field N, Mercer CH,
et al: Prevalence of infertility and help seeking among 15 000
women and men. Hum Reprod. 31:2108–2118. 2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Carson SA and Kallen AN: Diagnosis and
management of infertility: A review. JAMA. 326:65–76.
2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Abrao MS, Muzii L and Marana R: Anatomical
causes of female infertility and their management. Int J Gynaecol
Obstet. 123 (Suppl 2):S18–S24. 2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Grigovich M, Kacharia VS, Bharwani N,
Hemingway A, Mijatovic V and Rodgers SK: Evaluating fallopian tube
patency: What the radiologist needs to know. Radiographics.
41:1876–18961. 2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Baramki TA: Hysterosalpingography. Fertil
Steril. 83:1595–1606. 2005.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zafarani F, Ghaffari F, Ahmadi F,
Soleimani Mehranjani M and Shahrzad G: Hysterosalpingography in the
assessment of proximal tubal pathology: A review of congenital and
acquired abnormalities. Br J Radiol. 94(20201386)2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Li H, Ren Y, Yan J, Huang M, Zheng B, Luo
X, Huang S and Cai S: Fertility outcome and safety of ethiodized
poppy seed oil for hysterosalpingography in 1,053 infertile
patients: A real-world study. Front Med (Lausanne).
9(804494)2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Roest I, Hajiyavand AM, Bongers MY,
Mijatovic V, Mol BWJ, Koks CAM and Dearn KD: What is the
fertility-enhancing effect of tubal flushing? A hypothesis article.
J Obstet Gynaecol. 42:1619–1625. 2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Burks HR and Hansen KR: Oil or water-based
contrast for hysterosalpingography? Fertil Steril. 114:75–76.
2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Liang G, Zhu Q, He X, Wang X, Jiang L, Zhu
C, Xie L, Qian Z and Zhang J: Effects of oil-soluble versus
water-soluble contrast media at hysterosalpingography on pregnancy
outcomes in women with a low risk of tubal disease: Study protocol
for a randomised controlled trial. BMJ Open.
10(e039166)2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
van Rijswijk J, van Welie N, Dreyer K,
Pham CT, Verhoeve HR, Hoek A, de Bruin JP, Nap AW, van Hooff MHA,
Goddijn M, et al: Tubal flushing with oil-based or water-based
contrast at hysterosalpingography for infertility: Long-term
reproductive outcomes of a randomized trial. Fertil Steril.
114:155–162. 2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Alper MM, Garner PR, Spence JE and
Quarrington AM: Pregnancy rates after hysterosalpingography with
oil- and water-soluble contrast media. Obstet Gynecol. 68:6–9.
1986.PubMed/NCBI
|
|
15
|
de Boer AD, Vemer HM, Willemsen WN and
Sanders FB: Oil or aqueous contrast media for
hysterosalpingography: A prospective, randomized, clinical study.
Eur J Obstet Gynecol Reprod Biol. 28:65–68. 1988.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Rasmussen F, Lindequist S, Larsen C and
Justesen P: Therapeutic effect of hysterosalpingography: Oil-versus
water-soluble contrast media-a randomized prospective study.
Radiology. 179:75–78. 1991.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Lindequist S, Rasmussen F and Larsen C:
Use of iotrolan versus ethiodized poppy-seed oil in
hysterosalpingography. Radiology. 191:513–517. 1994.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Spring DB, Barkan HE and Pruyn SC:
Potential therapeutic effects of contrast materials in
hysterosalpingography: A prospective randomized clinical trial.
Kaiser permanente infertility work group. Radiology. 214:53–57.
2000.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Steiner AZ, Meyer WR, Clark RL and
Hartmann KE: Oil-soluble contrast during hysterosalpingography in
women with proven tubal patency. Obstet Gynecol. 101:109–113.
2003.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Qiu HX: Clinical observation of 283 cases
of hysterosalpingography using nonionic contrast media. Chongqing
Med J. 34:796–798. 2005.
|
|
21
|
Dreyer K, van Rijswijk J, Mijatovic V,
Goddijn M, Verhoeve HR, van Rooij IAJ, Hoek A, Bourdrez P, Nap AW,
Rijnsaardt-Lukassen HGM, et al: Oil-based or water-based contrast
for hysterosalpingography in infertile women. N Engl J Med.
376:2043–2052. 2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Wang LY, Du WF and Zhang QH: Explore the
clinical effect of iodized water and Lipiodol in the diagnosis and
treatment of secondary infertility in hysterosalpingography. J
Nongken Med. 43:29–31. 2021.
|
|
23
|
Zhang J, Lan W, Wang Y, Chen K, Zhang G,
Yang W, Chen H, Xu W, Ma J, Qin W, et al: Ethiodized poppyseed
oil-based contrast medium is superior to water-based contrast
medium during hysterosalpingography regarding image quality
improvement and fertility enhancement: A multicentric, randomized
and controlled trial. EClinicalMedicine. 46(101363)2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Lu J, Qi D and Xu W: Fertility-enhancing
effect of oil-based contrast agents during hysterosalpingography
and the variation of this effect within a 3-year follow-up period
in infertile patients. Front Med (Lausanne).
9(948945)2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Wang R, van Welie N, van Rijswijk J,
Johnson NP, Norman RJ, Dreyer K, Mijatovic V and Mol BW:
Effectiveness on fertility outcome of tubal flushing with different
contrast media: Systematic review and network meta-analysis.
Ultrasound Obstet Gynecol. 54:172–181. 2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Fang F, Bai Y, Zhang Y and Faramand A:
Oil-based versus water-based contrast for hysterosalpingography in
infertile women: A systematic review and meta-analysis of
randomized controlled trials. Fertil Steril. 110:153–160.e3.
2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Tsui S and Sofy AA: A meta-analysis of
fertility and adverse outcomes in oil- and water-based contrast for
hysterosalpingography. Turk J Obstet Gynecol. 20:64–73.
2023.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Moher D, Liberati A, Tetzlaff J and Altman
DG: PRISMA Group. Preferred reporting items for systematic reviews
and meta-analyses: The PRISMA statement. PLoS Med.
6(e1000097)2009.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Lundh A and Gøtzsche PC: Recommendations
by cochrane review groups for assessment of the risk of bias in
studies. BMC Med Res Methodol. 8(22)2008.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Wells GA, Shea B, O'Connell D, et al: The
Newcastle-Ottawa Scale (NOS) for assessing the quality of
nonrandomized studies in meta-analyses. The Ottawa Hospital.
|
|
31
|
Izumi G, Koga K, Takamura M, Bo W, Nagai
M, Miyashita M, Harada M, Hirata T, Hirota Y, Yoshino O, et al:
Oil-soluble contrast medium (OSCM) for hysterosalpingography
modulates dendritic cell and regulatory T cell profiles in the
peritoneal cavity: A possible mechanism by which OSCM enhances
fertility. J Immunol. 198:4277–4284. 2017.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Johnson JV, Montoya IA and Olive DL:
Ethiodol oil contrast medium inhibits macrophage phagocytosis and
adherence by altering membrane electronegativity and
microviscosity. Fertil Steril. 58:511–517. 1992.PubMed/NCBI View Article : Google Scholar
|
|
33
|
van Welie N, Dreyer K, van Rijswijk J,
Verhoeve HR, Goddijn M, Nap AW, Smeenk JMJ, Traas MAF,
Rijnsaardt-Lukassen HGM, van Dongen AJCM, et al: Treatment effect
of oil-based contrast is related to experienced pain at HSG: A
post-hoc analysis of the randomised H2Oil study. Hum Reprod.
34:2391–2398. 2019.PubMed/NCBI View Article : Google Scholar
|
|
34
|
van Welie N, Rosielle K, Dreyer K, van
Rijswijk J, Lambalk CB, van Geloven N, Mijatovic V, Mol BWJ and van
Eekelen R: H2Oil Study Group. How long does the fertility-enhancing
effect of hysterosalpingography with oil-based contrast last?
Reprod Biomed Online. 41:1038–1044. 2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Wang R, Watson A, Johnson N, Cheung K,
Fitzgerald C, Mol BWJ and Mohiyiddeen L: Tubal flushing for
subfertility. Cochrane Database Syst Rev.
10(CD003718)2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Harris EA, Stephens KK and Winuthayanon W:
Extracellular vesicles and the oviduct function. Int J Mol Sci.
21(8280)2020.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Court KA, Dare AJ, Weston-Webb M, Hadden
WE, Sim RG and Johnson NP: Establishment of lipiodol as a fertility
treatment-prospective study of the complete innovative treatment
data set. Aust N Z J Obstet Gynaecol. 54:13–19. 2014.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Quenby S, Gallos ID, Dhillon-Smith RK,
Podesek M, Stephenson MD, Fisher J, Brosens JJ, Brewin J, Ramhorst
R, Lucas ES, et al: Miscarriage matters: The epidemiological,
physical, psychological, and economic costs of early pregnancy
loss. Lancet. 397:1658–1667. 2021.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Tonick S and Conageski C: Ectopic
pregnancy. Obstet Gynecol Clin North Am. 49:537–549.
2022.PubMed/NCBI View Article : Google Scholar
|