Introduction
Radiotherapy has an important role in the local
treatment of malignancies. The mechanism of radiotherapy is mainly
through the damage of deoxyribonucleic acid (DNA) inside the
malignant cells in the irradiation field. However, the rare
phenomenon of spontaneous regression in lesions distant from an
irradiation field has been reported and is called ‘abscopal
effect’. The abscopal effect was initially suggested by Mole
(1) in 1953. While the biological
mechanism of this effect has remained to be completely elucidated,
immunologic mechanisms are considered to mediate this effect. In
recent years, tumor immunity in combination with immune checkpoint
inhibitors (ICIs) has become of increasing interest in the abscopal
effect. However, this phenomenon is rarely encountered in clinical
practice, particularly for an abscopal effect to manifest itself
without pharmacologic immunomodulation (pure abscopal effect)
(2). The present study reported on
two cases with abscopal effects: One showed a pure abscopal effect
and the other occurred after resistance to immunotherapy. Fever of
unknown cause (FUC) was observed immediately after initiation of
radiotherapy in both cases. The relationship between this fever and
the abscopal effect was unclear, but radiotherapy does not normally
induce a systemic response. The symptoms at presentation, physical
exams and laboratory results are provided for each case in the
following section.
Case report
Case 1
A male patient aged 78 years was diagnosed with
pleomorphic sarcoma of the iliac bone (size, 8.1x12.1x15.5 cm) with
pelvic lymph node metastases and bilateral lung metastases at an
external hospital in June 2019, and the treatment options of
chemotherapy, radiotherapy and palliative care were considered.
However, taking into account the patient's age, the patient and his
family chose palliative care at our institution, and the patient
was referred to the department of palliative medicine of Tsukuba
Medical Center Hospital (Ibaraki, Japan) within the same month.
Palliative photon radiotherapy of 36 Gy in 12 fractions over 16
days was indicated for iliac pain control and fracture prevention.
The day after the start of radiotherapy, the patient complained of
fever without respiratory or urinary tract symptoms. Fever of up to
38˚C was observed twice a day during the irradiation period. This
fever broke spontaneously in 3 h after it started each time. Blood
tests indicated no characteristic findings other than a mild
inflammatory reaction and thrombocytopenia [C-reactive protein
(CRP), 7.07 mg/dl (normal range: ≤0.3 mg/dl); platelets,
5.6x104/µl (15-45x104/µl). Celecoxib was
prescribed for antipyretic and analgesic therapy but was
ineffective. The fever continued for 2 days after the end of
radiotherapy but then spontaneously resolved. After radiotherapy,
no additional treatment was given except for drugs for pain relief.
Pain improved gradually and the patient started to be able to walk
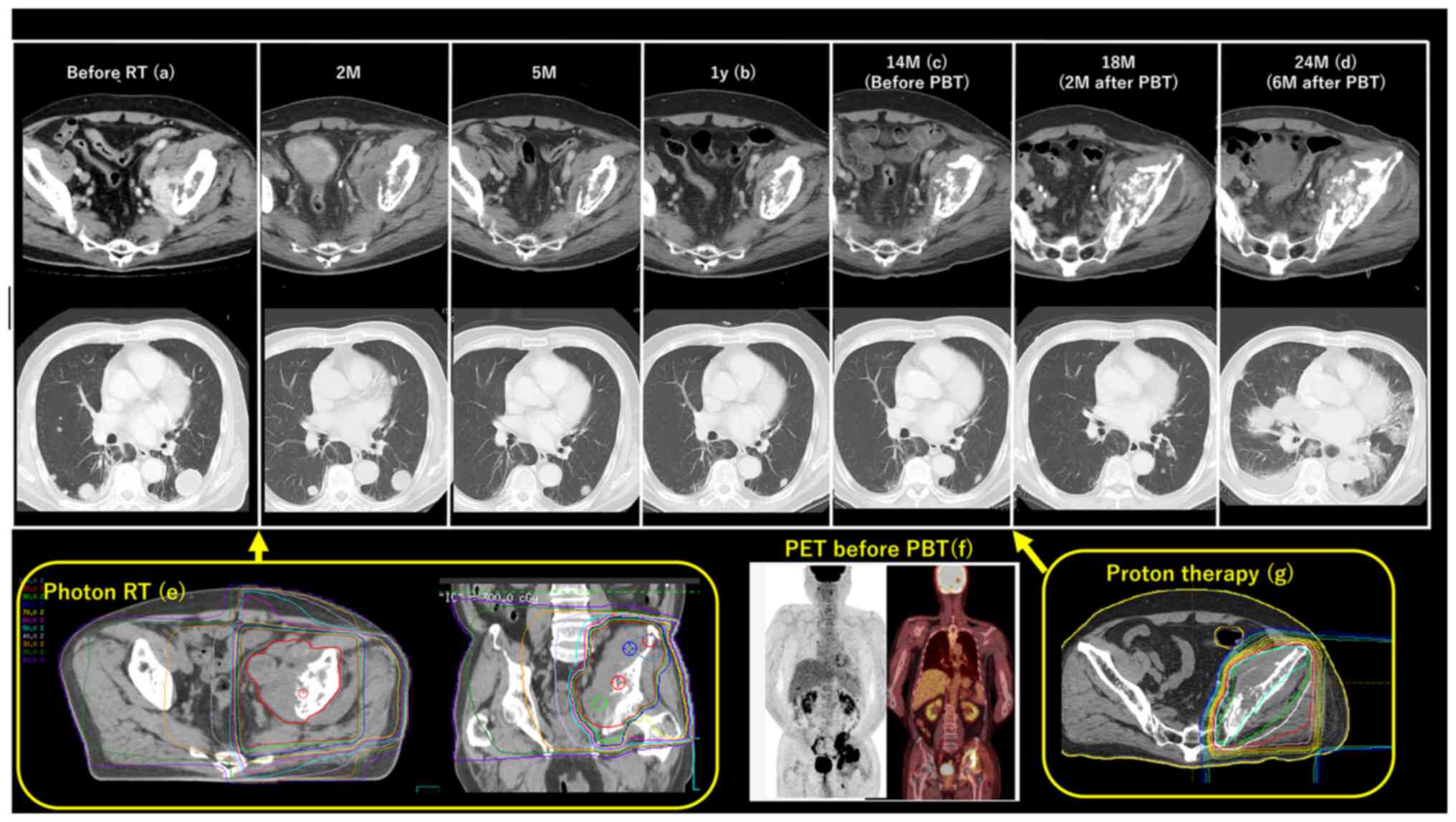
on his own 3 months after radiotherapy. Computed tomography (CT)
indicated significant shrinkage of the primary irradiated tumor and
lung metastases. At one year after radiotherapy, the primary tumor
size was 3.6x6x5.5 cm. However, 14 months after radiotherapy, the
patient complained of left coxalgia again and the iliac tumor had
slightly increased. At this time, the tumor size was 4.4x8x6 cm,
but lung metastases still remained small and
18fluorodeoxyglucose-positron emission tomography (PET)
indicated no accumulation except for the iliac tumor. Reirradiation
with photon radiotherapy was impossible because the alimentary
tract could not be avoided; therefore, proton therapy of 51 Gy in
17 fractions over 27 days was used for the iliac tumor. During this
course, there was no fever. Pain was slightly relieved, but the
tumor did not shrink at all. The tumor then rapidly increased in
size and lung metastases also progressed markedly. After proton
therapy, palliative care was offered and the patient died from lung
lymphangitis. The timeline, CT, PET images and the treatment fields
of photon and proton radiotherapy are presented in Fig. 1.
Case 2
A 59-year-old male patient was diagnosed with renal
cell cancer based on CT at the time of admission to Tsukuba Medical
Center Hospital (Ibaraki, Japan) due to capsular hemorrhage in
March 2016. After recovering from this hemorrhage, a close
examination for renal cell carcinoma (RCC) revealed metastasis to
renal hilum lymph nodes and lung metastases, and the clinical stage
was T3aN1M1. Nephrectomy was performed in 2016 and the pathological
results indicated clear cell carcinoma. Sunitinib was started one
month after nephrectomy, and lung and lymph node metastases
decreased. Sunitinib was continued for 10 months, then after the
lung metastases increased and right adrenal metastasis appeared,
treatment was switched to axitinib and the metastases shrank again.
However, severe chemical dehydration occurred 5 months after the
start of axitinib; therefore, nivolumab was started thereafter and
continued for 8 months, despite slight progression of lung and
adrenal metastases 2 months after the start of nivolumab. However,
nivolumab was then stopped due to severe immune-related adverse
events of pituitary insufficiency followed by infectious
endocarditis and severe ischemic enteritis. Subsequently, no
additional drug therapy was given and in the 8 months after
stopping nivolumab, right adrenal metastasis increased to 70x54 mm.
Other metastases remained small. At that time, the size of the lung
metastasis was 12.8x4.4 mm. Therefore, resection of the adrenal
metastasis was attempted; however, this proved to be impossible due
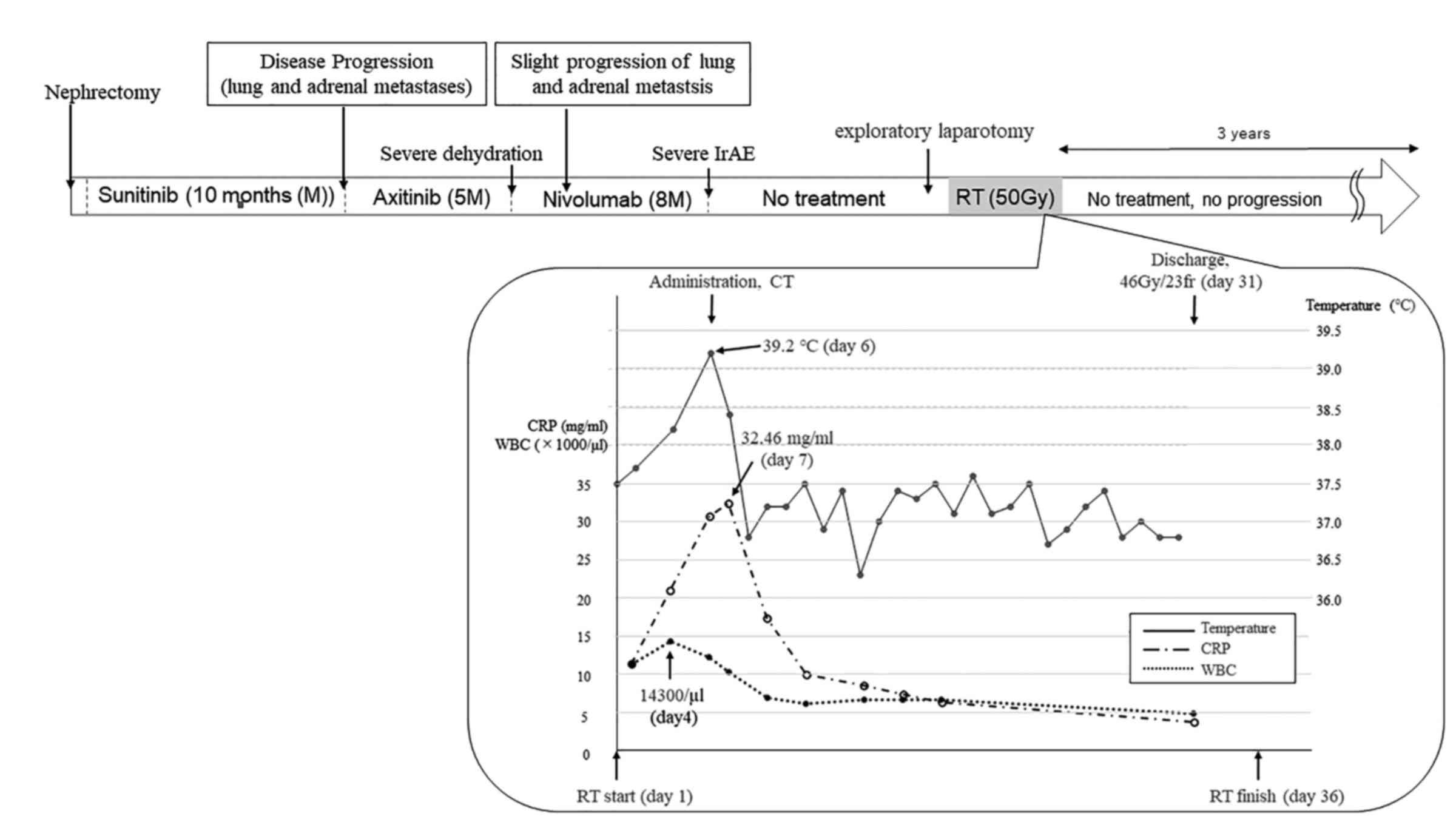
to strong adhesion. Radiotherapy was then considered and photon
radiotherapy of 50 Gy in 25 fractions over 36 days was delivered
with palliative intent. On the first day of the radiotherapy, the
patient had a fever of 37.5˚C after returning home from
radiotherapy. On the second day, blood tests were performed because
the fever persisted and a high inflammatory response was observed:
White blood cells (WBC), 14,300/µl (normal range: 3,100-8,400/µl);
and CRP, 11.38 mg/dl. The fever was not broken with oral aspirin
and the inflammatory reaction rapidly increased; the body
temperature reached 39.2˚C and CRP was 32.46 mg/dl. CT was
performed to search for the cause of inflammation on the 6th day,
but it could not be identified. At this time, the adrenal
metastasis increased to 97x69 mm and one of the lung metastases had
slightly increased to 13.6x4.8 mm, compared to 4 months earlier.
Urine tests and blood and urine cultures were all negative.
Therefore, it was considered that the inflammation was caused by
the tumor itself, and radiotherapy was continued despite the high
inflammatory response. The inflammatory reaction gradually
decreased spontaneously during the treatment period. The treatment
course of Case 2 is presented in Fig.
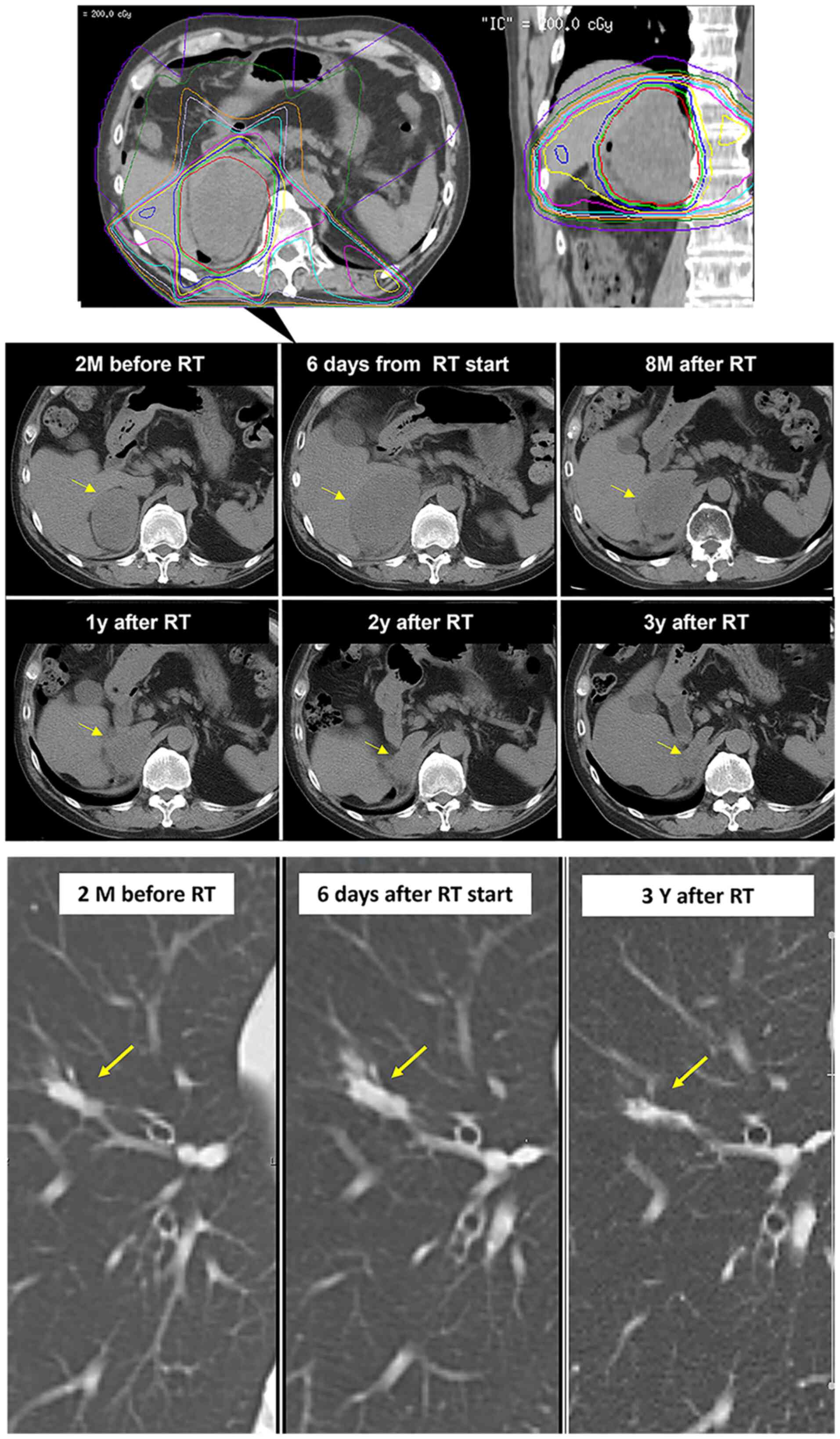
2. After radiotherapy, the adrenal metastasis shrunk gradually
and had reached a size of 35x25 mm by June 2022. The pulmonary
metastases also slightly shrank to 9.7x3.1 mm. The treatment field
and CT images of the lung and adrenal metastases until June 2022
are presented in Fig. 3.
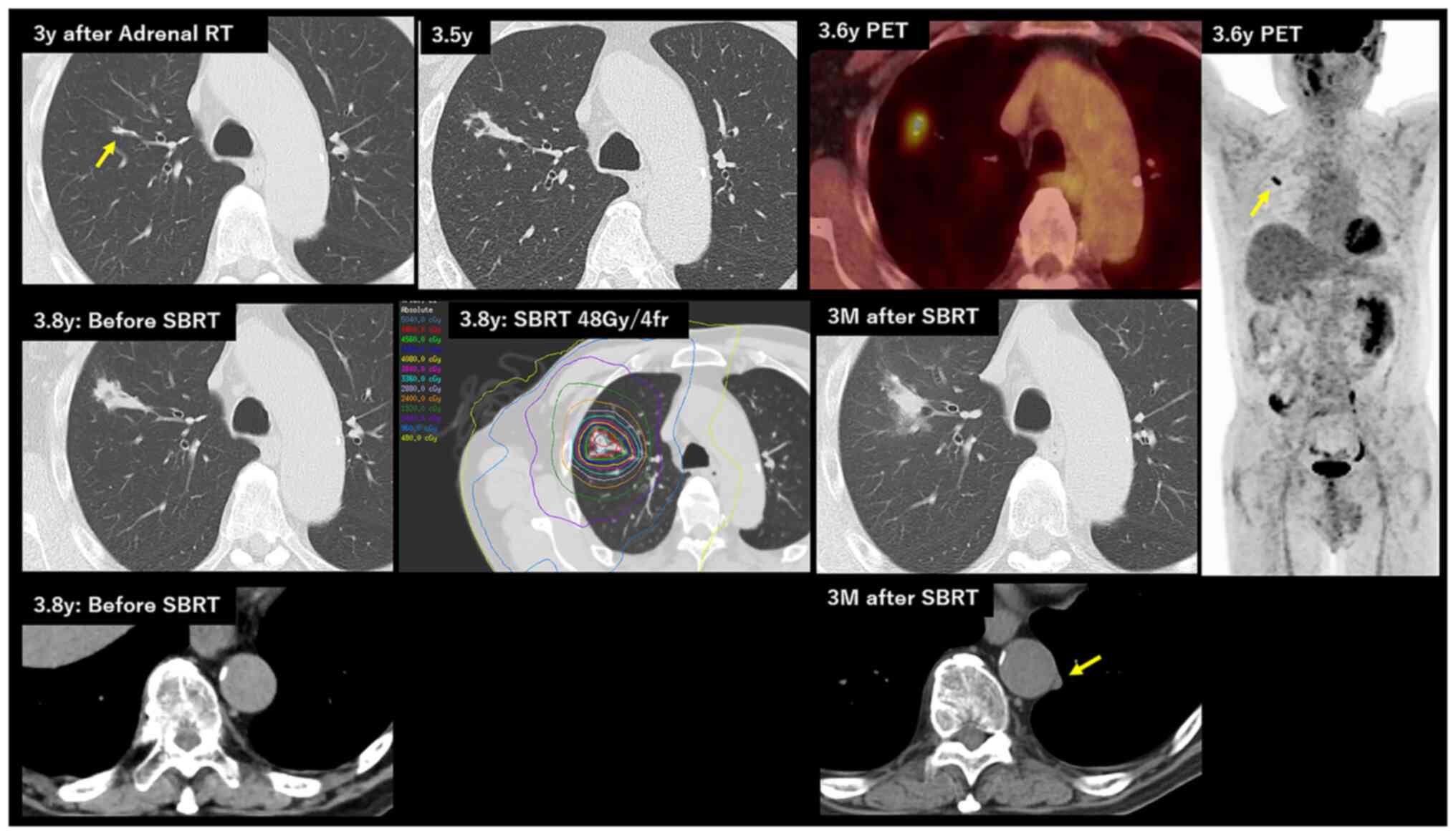
However, in December 2022, the lung metastasis
exhibited certain changes of calcification and dilatation of
downstream bronchus with endobronchial effusion. This finding
suggested secondary tracheal atresia, fungal infection or tumor
recurrence. However, blood tests were all negative for serum
beta-D-glucan (3),
Aspergillus antigen, Mycobacterium avium complex
antibody and the QuontiFeron test (4), which ruled out a fungal or
mycobacterium infection. After one month, the lung tumor had
continued to grow and PET accumulation was observed, so this change
of lung metastasis was diagnosed as recurrence. There was no PET
accumulation for adrenal metastasis. Bronchoscopy was not performed
due to hemorrhage risk. Considering oligo-progression and previous
adverse effects of tyrosine kinase inhibitor and ICI, stereotactic
body radiotherapy (SBRT) to the lung metastasis with a dose of 48
Gy in 4 fractions was performed in February 2023. This time, no
fever or CRP/WBC elevation was observed. After 3 months from the
SBRT, tumor consolidation was observed and ground glass opacity
around the tumor was enlarged. This change suggested tumor
progression, tumor hemorrhage or inflammation after SBRT. In
addition, new subpleural nodules were observed and lung atelectasis
or lung metastasis was considered for this nodule. The size of the
adrenal metastasis has remained unchanged since June 2022. This
patient will continue to be followed up. The CT and PET images and
treatment field of the lung are presented in Fig. 4.
Discussion and literature review
Abscopal effect has been reported in various
carcinomas. Siva et al (5)
suggested that this effect is transmitted by an acute inflammatory
cytokine cascade and the immune system. Ionizing radiation releases
cytokines, which elicit augmented tumor surveillance, inhibit tumor
growth and have direct tumoricidal properties (6). In addition, ionizing radiation
directly elicits innate immune recognition of a tumor: Dendritic
cells are activated by irradiated dying cells and antitumor T cells
are activated by the cross-presentation of tumor-derived antigens
presented to T cells (7).
In clinical practice, however, an abscopal effect of
radiotherapy alone is rare. In a literature review of abscopal
effects of radiotherapy, only 46 cases reported between 1969 and
2014 were retrieved (8). However,
the number of reports of abscopal effect in patients treated with a
combination of radiotherapy and ICI has increased (9-17).
In only one year, 2021, 21 case reports of abscopal effect promoted
after radiotherapy were yielded (15,18-37).
This is thought to be due to T-cell activation by a damage signal
from irradiated dying cells and upregulation of programmed death
receptor-1 and programmed cell death 1-ligand 1 (38,39),
and an ICI disarms immune escape mechanisms, and this may increase
the effects of the innate immune response activated by
radiotherapy. Grimaldi et al (40) reported an abscopal response in 52%
of patients with melanoma who received ipilimumab followed by
radiotherapy.
In the present study, two cases of abscopal effect
were reported. The most characteristic feature of the two cases is
that both patients had FUC soon after the start of radiotherapy.
Case 1, the patient with pleomorphic sarcoma, featured a pure
abscopal effect. In this case, a fever was observed during the
initial irradiation period, but since it was mild and there were no
signs of infection, not much attention was paid to it. By contrast,
the re-irradiation using proton therapy did not cause fever and no
abscopal effect was observed. Case 2, a patient with RCC, exhibited
an abscopal effect following radiotherapy after ICI. RCC frequently
has periods of disease quiescence; however, lung metastasis in this
case had an increasing trend at the start of radiotherapy;
therefore, it was expected to increase after radiotherapy to the
adrenal metastasis. In general, the prognosis of RCC after disease
progression during treatment with an ICI is poor. In a
retrospective analysis of 33 patients from 7 clinical trials,
Barata et al (41) found a
median progression-free survival (PFS) from initiation of molecular
targeted therapy after progression on an ICI of 6.4 months (95% CI:
4.4-8.4 months). Roviello et al (42) obtained a PFS of 5 and 3 months (95%
CI: 1-6 vs. 2-5; P=0.6) for patients who received active treatment
and best supportive care, respectively, after progression of
metastatic RCC while on nivolumab and cabozantinib. However, in
Case 2 of the present study, adrenal metastasis was well controlled
with a palliative dose and lung metastasis shrank over 3 years.
This may be due to enhanced immune response to nivolumab and the
strong inflammatory response observed during radiotherapy was also
related to immune response. After almost 4 years, the lung
metastasis recurred and SBRT was performed. This time, no
inflammatory response was observed, and the disease is suspected to
be progressing.
There was no evidence of a relationship between the
abscopal effect and fever during radiotherapy. However, the
abscopal effect is known to involve the activation of inflammatory
cytokines and these two phenomena are both so unusual that they may
not be coincidental. The two cases in the present study were
treated palliatively and detailed data are missing. However, given
that an inflammatory cytokine cascade is involved in the abscopal
effect, it may be concluded that FUC during radiotherapy may be a
hint to the abscopal effect, not by coincidence, although it is
frequently considered as a tumor fever without much of a
concern.
In conclusion, abscopal effect is rare and difficult
to predict. A total of 2 cases of abscopal effect with FUC during
radiotherapy were encountered at our institution. Awareness of FUC
during radiotherapy may offer the possibility of better patient
follow-up.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YO conducted photon radiotherapy on the 2 patients
and wrote a draft of the manuscript. MM and HS conducted proton
therapy on Case 1. MT and YO followed up Case 2. TH provided care
for Case 1. MK, KT and KK provided care for Case 2. All authors
contributed to manuscript revision, and have read and agreed to be
accountable for the content of the work. All authors have read and
approved the final manuscript. YO and MM checked and confirmed the
authenticity of all the raw data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent for the publication of this
manuscript, including case data and images, was obtained from each
patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mole RH: Whole body irradiation;
radiobiology or medicine? Br J Radiol. 26:234–241. 1953.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ellerin BE, Demandante CGN and Martins JT:
Pure abscopal effect of radiotherapy in a salivary gland carcinoma:
Case report, literature review, and a search for new approaches.
Cancer Radiother. 24:226–246. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Obayashi T, Yoshida M, Mori T, Goto H,
Yasuoka A, Iwasaki H, Teshima H, Kohno S, Horiuchi A, Ito A, et al:
Plasma (1-3)-beta-D-glucan mesurement in didagnosis of invasive
deep mycosis and fungal febrile episodes. Lancet. 345:17–20.
1995.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Mazurek GH and Villarino ME: CDC.
Guidelines for using the QuantiFERON-TB test for diagnosing latent
Mycobacterium tuberculosis infection. Centers for Disease Control
and Prevention. MMWR Recomm Rep. 52(RR-2):15–18. 2013.PubMed/NCBI
|
|
5
|
Siva S, MacManus MP, Martin RF and Martin
OA: Abscopal effects of radiation therapy: A clinical review for
the radiobiologist. Cancer Lett. 356:82–90. 2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kaminski JM, Shinohara E, Summers JB,
Niermann KJ, Morimoto A and Brousal J: The controversial abscopal
effect. Cancer Treat Rev. 31:159–172. 2005.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Obeid M, Tesniere A, Ghiringhelli F, Fimia
GM, Apetoh L, Perfettini JL, Castedo M, Mignot G, Panaretakis T,
Casares N, et al: Calreticulin exposure dictates the immunogenicity
of cancer cell death. Nat Med. 13:54–61. 2007.PubMed/NCBI View
Article : Google Scholar
|
|
8
|
Abuodeh Y, Venkat P and Kim S: Systematic
review of case reports on the abscopal effect. Curr Probl Cancer.
40:25–37. 2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Postow MA, Callahan MK, Barker CA, Yamada
Y, Yuan J, Kitano S, Mu Z, Rasalan T, Adamow M, Ritter E, et al:
Immunologic correlates of the abscopal effect in a patient with
melanoma. N Engl J Med. 366:925–931. 2012.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Golden EB, Demaria S, Schiff PB, Chachoua
A and Formenti SC: An abscopal response to radiation and ipilimumab
in a patient with metastatic non-small cell lung cancer. Cancer
Immunol Res. 1:365–372. 2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Hori K, Hirohashi Y, Aoyagi T, Taniguchi
N, Murakumo M, Miyata H, Torigoe T, Abe T, Shinohara N and Morita
K: Abscopal effect following nivolumab induction in a patient with
metastatic renal cell carcinoma-unique pathological features of the
primary specimen: A case report. Exp Ther Med. 19:1903–1907.
2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kuryk L, Moller AW and Jaderberg M:
Abscopal effect when combining oncolytic adenovirus and checkpoint
inhibitor in a humanized NOG mouse model of melanoma. J Med Virol.
91:1702–1706. 2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Nakajima N, Kano T, Oda K, Uchida T, Otaki
T, Nagao K, Shimizu Y, Kawakami M, Kim H, Nitta M, et al: Possible
abscopal effect after discontinuation of nivolumab in metastatic
renal cell carcinoma. IJU Case Rep. 3:215–218. 2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Oei AL, Korangath P, Mulka K, Helenius M,
Coulter JB, Stewart J, Velarde E, Crezee J, Simons B, Stalpers LJA,
et al: Enhancing the abscopal effect of radiation and immune
checkpoint inhibitor therapies with magnetic nanoparticle
hyperthermia in a model of metastatic breast cancer. Int J
Hyperthermia. 36(sup1):S47–S63. 2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Sezen D, Patel RR, Tang C, Onstad M,
Nagarajan P, Patel SP, Welsh JW and Lin LL: Immunotherapy combined
with high- and low-dose radiation to all sites leads to complete
clearance of disease in a patient with metastatic vaginal melanoma.
Gynecol Oncol. 161:645–652. 2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ishiyama Y, Takagi T, Yoshida K, Iizuka J,
Kakuta Y, Okumi M, Ishida H and Tanabe K: Possible abscopal effect
in urothelial carcinoma of the upper urinary tract after treatment
with immune checkpoint inhibitors. IJU Case Rep. 3:25–27.
2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Song HN, Jin H, Kim JH, Ha IB, Kang KM,
Choi HS, Jeong HJ, Kim MY, Kim HJ and Jeong BK: Abscopal effect of
radiotherapy enhanced with immune checkpoint inhibitors of triple
negative breast cancer in 4T1 mammary carcinoma model. Int J Mol
Sci. 22(10476)2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Damante MA, Huntoon KM, Palmer JD, Liebner
DA and Elder JB: A case of multiple synchronously diagnosed brain
metastases from alveolar soft part sarcoma without concurrent lung
involvement. Surg Neurol Int. 12(111)2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
D'Andrea MA and Reddy GK: Systemic effects
of radiation therapy-induced abscopal responses in patients with
advanced lung cancer. Oncology. 99:1–14. 2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Fiorica F, Belluomini L, Giuliani J,
Urbini B, Milella M, Frassoldati A, Pilotto S and Giorgi C:
Abscopal effect and resistance reversion in nivolumab-treated
non-small-cell lung cancer undergoing palliative radiotherapy: A
case report. Immunotherapy. 13:971–976. 2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Herrscher H, Sauer B, Truntzer P and
Robert C: Abscopal antitumor effect in a patient with melanoma and
coronavirus disease 2019. Eur J Cancer. 149:91–93. 2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Hotta T, Okuno T, Nakao M, Amano Y, Isobe
T and Tsubata Y: Reproducible abscopal effect in a patient with
lung cancer who underwent whole-brain irradiation and atezolizumab
administration. Thorac Cancer. 12:985–988. 2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Huynh LM, Bonebrake BT, DiMaio DJ, Baine
MJ and Teply BA: Development of bullous pemphigoid following
radiation therapy combined with nivolumab for renal cell carcinoma:
A case report of abscopal toxicities. Medicine (Baltimore).
100(e28199)2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Kim TH and Chang JS: Abscopal effect after
palliative five-fraction radiation therapy on bone and lymph node
metastases from luminal B breast cancer: A case report and clinical
implications for palliative radiation therapy. Radiat Oncol J.
39:139–144. 2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kondo T, Nakatsugawa M, Okubo M, Nakamura
H, Yunaiyama D, Wakiya M, Takeda A, Kikawada N, Kishida T, Someya
M, et al: Laryngeal cancer with lung metastases showing long-term
complete response and delayed immune-related adverse event after
nivolumab discontinuation. Ear Nose Throat J.
(1455613211031025)2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Mampuya WA, Bouchaab H, Schaefer N, Kinj
R, La Rosa S, Letovanec I, Ozsahin M, Bourhis J, Coukos G, Peters S
and Herrera FG: Abscopal effect in a patient with malignant pleural
mesothelioma treated with palliative radiotherapy and
pembrolizumab. Clin Transl Radiat Oncol. 27:85–88. 2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Mazzaschi G, Tommasi C, Pietri E, Corcione
L, De Giorgi A, Bini P and Bui S: Abscopal effect as part of
treatment of oligometastatic head and neck cancer: A case report.
Clin Case Rep. 9:1334–1338. 2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Moradi LA, Clark CA, Schneider CS, Deshane
AS and Dobelbower MC: Durable metastatic melanoma remission
following pembrolizumab and radiotherapy: A case report of
prophylactic immunosuppression in a patient with myasthenia gravis
and immune-mediated colitis. Front Immunol.
12(788499)2021.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Muto M, Nakata H, Ishigaki K, Tachibana S,
Yoshida M, Muto M, Yanagawa N and Okumura T: Successful treatment
of advanced gastric cancer with brain metastases through an
abscopal effect by radiation and immune checkpoint inhibitor
therapy. J Gastric Cancer. 21:319–324. 2021.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Ohmatsu K, Hashimoto Y, Kawanishi M, Ishii
Y, Kono S, Kuribayashi S, Ariizumi S and Karasawa K: Abscopal
complete regression of hepatocellular carcinoma with multiple
pleural metastases. Int Cancer Conf J. 10:54–58. 2021.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Piercey O, Tomaszewski JM and Smith K:
Intracranial response after extracranial radiation in a patient
with rapidly progressing metastatic melanoma. BMJ Case Rep.
14(e240921)2021.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Sakamoto T, Fujimoto N and Nakashima M:
One course of pembrolizumab after radiation therapy was very
effective against metastatic bladder cancer and Cr was confirmed: A
case report. Nihon Hinyokika Gakkai Zasshi. 112:220–223.
2021.PubMed/NCBI View Article : Google Scholar : (In Japanese).
|
|
33
|
Vilinovszki O, Andratschke N, Huellner M,
Curioni-Fontecedro A and Kroeze SGC: True abscopal effect in a
patient with metastatic non-small cell lung cancer. Radiat Oncol.
16(194)2021.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Wu M, Liu J, Seery S, Meng X and Yue J:
Cytoreductive nephrectomy promoted abscopal effect of camrelizumab
combined with radiotherapy for metastatic renal cell carcinoma: A
case report and review of the literature. Front Immunol.
12(646085)2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Yamaguchi T, Fushida S, Kinoshita J, Saito
H, Shimada M, Terai S, Moriyama H, Okamoto K, Nakamura K, Ninomiya
I and Inaki N: A case of primary malignant melanoma of the
esophagogastric junction with abscopal effect after nivolumab
administration. Surg Case Rep. 7(253)2021.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Zhang X, Zhang Y, Liu Y, Yang Y, Dong P,
He L and Zhou F: Stereotactic body radiotherapy-induced abscopal
effect twice after pembrolizumab failure in hereditary
leiomyomatosis and renal cell carcinoma: A case report with genetic
and immunologic analysis. Transl Androl Urol. 10:4304–4312.
2021.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Zhang YS, Zhang YH, Li XJ, Hu TC, Chen WZ,
Pan X, Chai HY and Ye YC: Bystander effect and abscopal effect in
recurrent thymic carcinoma treated with carbon-ion radiation
therapy: A case report. World J Clin Cases. 9:6538–6543.
2021.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Deng L, Liang H, Burnette B, Beckett M,
Darga T, Weichselbaum RR and Fu YX: Irradiation and anti-PD-L1
treatment synergistically promote antitumor immunity in mice. J
Clin Invest. 124:687–695. 2014.PubMed/NCBI View
Article : Google Scholar
|
|
39
|
Lauber K and Dunn L: Immunotherapy
mythbusters in head and neck cancer: The abscopal effect and
pseudoprogression. Am Soc Clin Oncol Educ Book. 39:352–363.
2019.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Grimaldi AM, Simeone E, Giannarelli D,
Muto P, Falivene S, Borzillo V, Giugliano FM, Sandomenico F,
Petrillo A, Curvietto M, et al: Abscopal effects of radiotherapy on
advanced melanoma patients who progressed after ipilimumab
immunotherapy. Oncoimmunology. 3(e28780)2014.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Barata PC, De Liano AG, Mendiratta P,
Crolley V, Szabados B, Morrison L, Wood L, Allman K, Tyler A,
Martin A, et al: The efficacy of VEGFR TKI therapy after
progression on immune combination therapy in metastatic renal cell
carcinoma. Br J Cancer. 119:160–163. 2018.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Roviello G, Gambale E, Giorgione R,
Santini D, Stellato M, Fornarini G, Rebuzzi SE, Basso U, Bimbatti
D, Doni L, et al: Effect of systemic therapies or best supportive
care after disease progression to both nivolumab and cabozantinib
in metastatic renal cell carcinoma: The Meet-Uro 19BEYOND study.
Cancer Med. 11:3084–3092. 2022.PubMed/NCBI View Article : Google Scholar
|